Introduction
Prostate cancer is expected to account for 21% of
total new malignancies developing among men in USA during
2020(1). Several factors associated
with increasing age, ethnicity, family history, genetic and
hormonal influences, increase the probability of being diagnosed
with carcinoma of the prostate gland (2). The presence of this malignancy can
reduce the life expectancy and also compromise the quality of life
of the patients due to sexual dysfunction, urinary incontinence and
bowel problems. The improvements in early disease detection and
treatment have reduced the mortality rate for prostate carcinoma by
52% since 1993 and have achieved a 5-year survival rate for
all-stage disease of 98% (1).
External-beam radiotherapy is extensively applied for the effective
management of prostate cancer (2).
At present, prostate irradiation is usually performed with the
modern techniques of intensity-modulated radiation therapy (IMRT)
and volumetric modulated arc therapy (VMAT). These modern
approaches enable the delivery of high cumulative radiation doses
to the tumor site using high-energy X-ray beams generated by a
linear accelerator. Both IMRT and VMAT improve the quality of the
patient's treatment plan and the sparing of the adjacent normal
structures compared to conventional irradiation (3,4). A
meta-analysis comparing the two aforementioned modulated techniques
revealed that VMAT may be considered as the preferred approach to
prostate cancer treatment due to its superior delivery efficiency
(5).
VMAT is usually delivered with 6-MV photons in most
radiation oncology centers (6). The
use of 10-MV X-rays for arc therapy of prostate carcinoma has also
been proposed (7-10).
Pasler et al (7)
demonstrated that the effect of beam energy on the target coverage
and organ at risk (OAR) sparing is not significant. Different
results were reported by other studies (8-10).
Kleiner and Podgorsak (8) found
that the use of 10-MV instead of 6-MV X-rays was associated with
better conformity and sparing of the critical organs. Stanley et
al (9) observed a faster dose
fall-off with 10-MV photon beams. Mattes et al (10) also reported that the increase of
photon beam energy resulted in dosimetric benefits. However, none
of those studies discussed the issue of radiation-induced
carcinogenesis due to the heavy irradiation of surrounding
tissues.
The purpose of the present study was to examine the
effect of 6-MV and 10-MV photon beam energies on the VMAT plan
quality for prostate cancer, as well as on the relevant risk of
secondary cancer induction.
Materials and methods
Prostate cancer patients
A total of 11 consecutive patients with newly
diagnosed low-risk prostate cancer, who underwent external-beam
radiation therapy at the Department of Radiotherapy and Oncology of
the University Hospital of Iraklion between July and December 2019,
were studied. All patients had ultrasound-guided transrectal
biopsy-proven clinical T1-T2aN0M0 disease with Gleason score
3+3/grade 1 and prostate-specific antigen <10 ng/ml. None of the
participants had been subjected to transurethral resection and/or
hormone therapy prior to irradiation. Patients with hip implants
were excluded from the study. The patients had been subjected to a
planning computed tomography (CT) examination with a comfortably
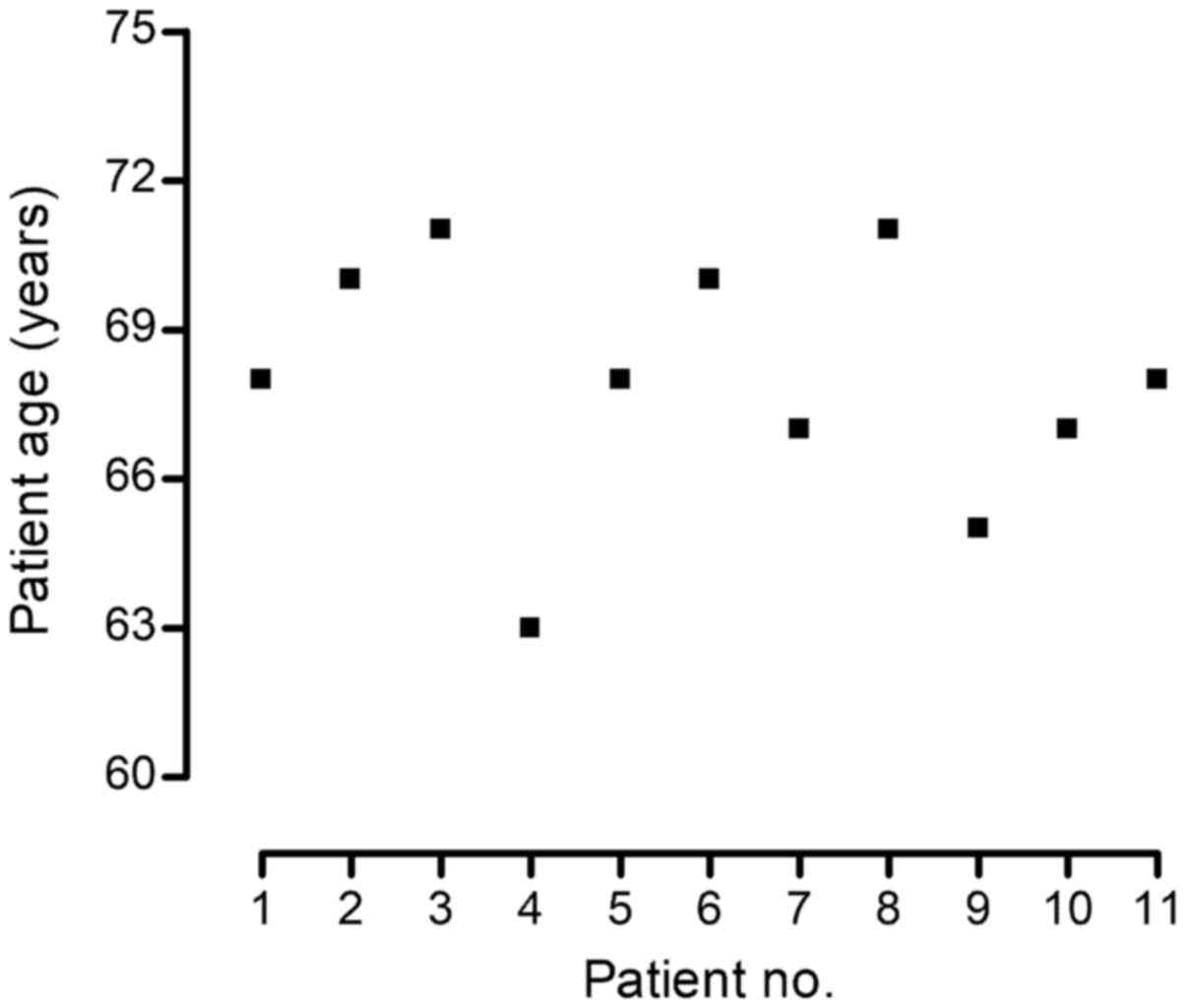
full urinary bladder and an empty rectum. The age of each study
participant is presented in Fig. 1.
The mean patient's age ± one standard deviation (SD) was 68.0±2.5
years.
Contouring and treatment planning
The treatment planning process was carried out with
the Monaco system, version 5.11.03 (Elekta Instrument AB). The CT
images of the study participants were transferred to the
aforementioned system. The rectum, urinary bladder, and right and
left femoral heads were manually delineated and were considered as
the OARs. A radiation oncologist was responsible for the contouring
of the structures of interest on CT scans. The rectal boundaries
were drawn from the anus to the rectosigmoid flexure. The clinical
target volume (CTV) coincided with the manually delineated prostate
gland. The planning target volume (PTV) was calculated as the CTV
with a margin of 0.5-0.8 cm in all directions, except posteriorly,
where a margin of 0.4 cm was applied (11). Moderate hypofractionated irradiation
was used for the treatment of low-risk prostate cancer patients, as
suggested in the literature (11,12).
All patients were prescribed to receive 70 Gy to the PTV in 28
fractions using VMAT on a newly installed medical linear
accelerator (Elekta Instrument AB) emitting 6-MV and 10-MV
photons.
For each study participant, two VMAT plans with 6-MV
and 10-MV X-rays were generated. The applied VMAT technique
consisted of two full arcs with the same isocenter in clockwise and
counterclockwise directions. The beam delivery was continuous over
each arc. The beam was modulated by dynamic multileaf collimation,
variable dose rate and speed of gantry rotation. The dose
calculations of the VMAT plans were made using a Monte Carlo
algorithm. The dose constraints for the PTV and OARs were based on
previous reports (11,13) and they are presented in Table I. Cumulative dose-volume histograms
(DVHs) of the aforementioned structures were employed to determine
the relevant Vi, defined as the percentage of the target
or OAR volume absorbing a radiation dose equal to i Gy. The normal
tissue integral dose (NTID) was also calculated as the product of
the average dose to a region, including normal tissues minus PTV,
and the volume of this region. The number of monitor units (MU) was
recorded for each plan.
 | Table IDose constraints for PTV and organs at
risk. |
Table I
Dose constraints for PTV and organs at
risk.
| Structure | Constraint |
|---|
| PTV | V70
≥98% |
| | Dmax ≤74.9
Gy |
| Bladder | V74
≤25% |
| | V69
≤35% |
| | V64
≤50% |
| Rectum | V74
≤15% |
| | V69
≤20% |
| | V64
≤25% |
| | V59
≤35% |
| Femoral heads | V45
<10% |
Radiation-induced bladder and rectal
cancer risks
Radiotherapy for prostate cancer may increase the
risk of development of radiation-induced malignancies to the
adjacent bladder and rectum (14).
These secondary cancer risks were estimated in the present study.
The DVHs of rectum and bladder derived from each VMAT plan
demonstrated that these organs receive an inhomogeneous dose
distribution. Parts of these OARs are exposed to primary radiation
and, therefore, they receive high doses, similar to the dose
delivered to the target. For radiation doses up to ~2 Gy, the risk
of radiation carcinogenesis is linearly related to the absorbed
dose (15). The extrapolation of
the linear-no-threshold model to high therapeutic doses is
currently in dispute (15,16). Schneider et al (17) previously introduced the concept of
the organ equivalent dose (OED), which considers the inhomogeneous
dose distribution of partially in-field organs from radiotherapy.
The non-linear mechanistic model is based on the use of the OED.
The model parameters were defined by data obtained from Japanese
A-bomb and Hodgkin cohorts for doses similar to radiation therapy
(17).
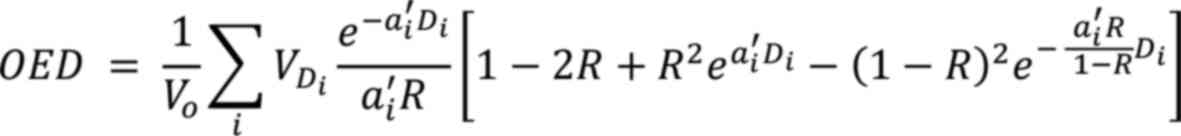
Differential DVHs were employed to compute the OED
of bladder and rectum from all VMAT plans with 6-MV or 10-MV
photons with the formula:
where Vo is the overall organ volume as
measured from CT scans, VDi is the organ volume
receiving a radiation dose of Di, and R is the organ-dependent
repopulation parameter. The cell-kill parameter was calculated as
follows:
where α and β are the linear quadratic model factors
and n is the number of fractions delivered during the whole
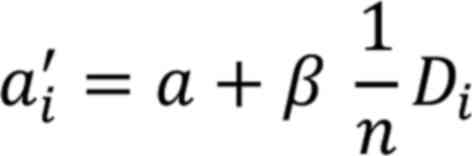
radiotherapy course. The excess absolute risk (EAR) for developing
bladder or rectal malignancies due to VMAT for prostate cancer was
estimated using the following equation:
where βEAR is the slope of the
dose-response curve in the low-dose region for individuals in
Western countries, agee is the patient's age at
the time of irradiation, agea is the attained age
of the patient and γe, γa are
the age-modifying factors (17).
The parameters R, α, β, βEAR,
γe and γa for the bladder and
rectum were derived from the literature (17,18)
and they are summarized in Table
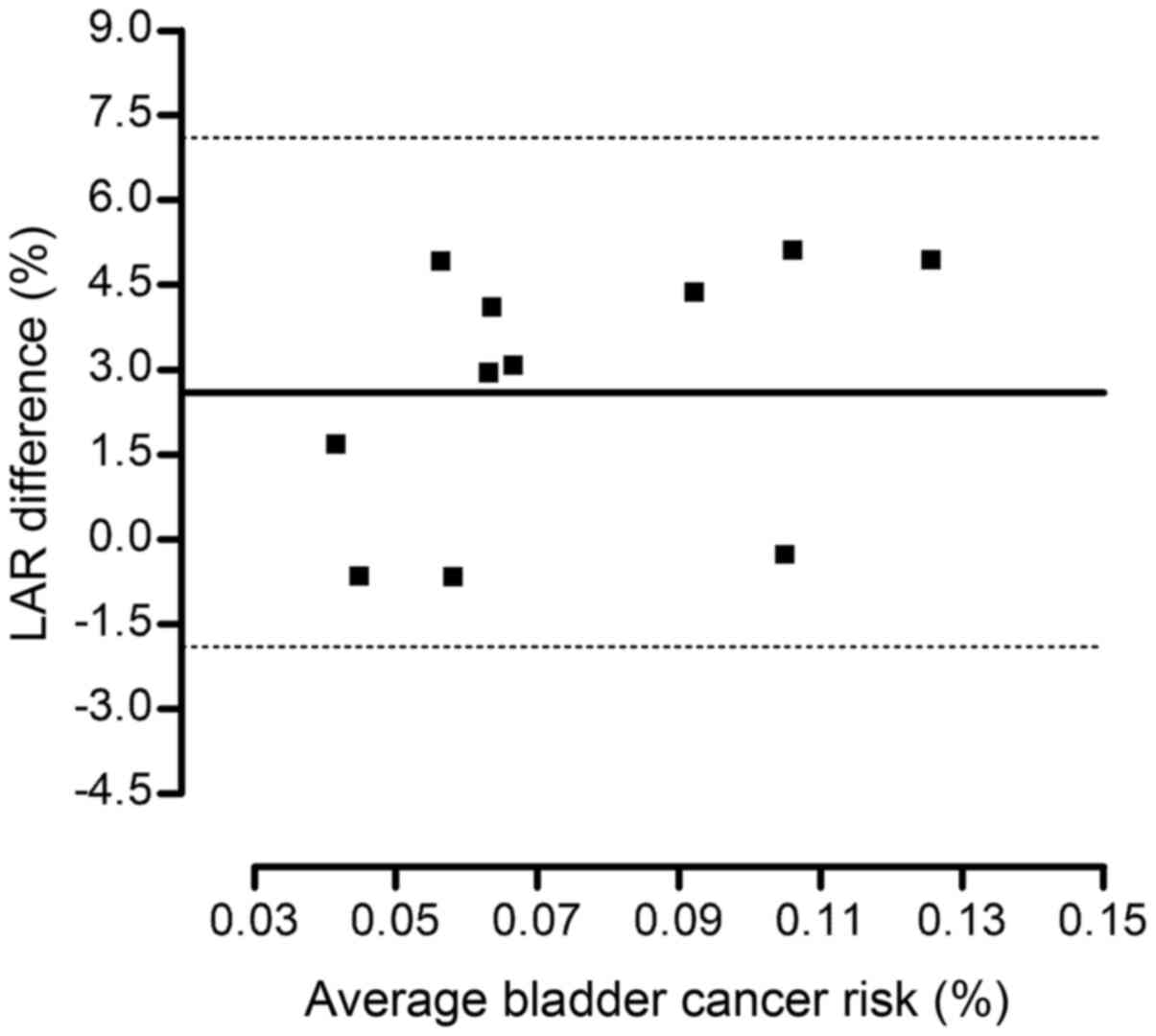
II. The lifetime attributable risk (LAR) was calculated by
summing the EAR values over an attained age from a latent period of
cancer induction of 5 years after radiotherapy to a final attained
age of 80 years. The LAR was calculated using the formula:
 | Table IIOrgan-specific risk parameters of the
mechanistic model. |
Table II
Organ-specific risk parameters of the
mechanistic model.
| Parameters | Bladder | Rectum |
|---|
| R | 0.06 | 0.56 |
|
α(Gy-1) | 0.219 | 0.033 |
| α/β(Gy) | 3.0 | 3.0 |
| γe | -0.024 | -0.056 |
| γa | 2.38 | 6.9 |
| βEAR
(/104 PY Gy) | 3.8 | 0.73 |
where the quantity
S(agea)/S(agee)
refers to the probability of a male patient to survive from
agee to agea according to the
most recent United States life tables (19).
Bland-Altman analysis
The agreement of the lifetime risks for developing
bladder or rectal malignancies due to VMAT plans with 6-MV photons
with those from arc therapy based on the use of 10-MV X-rays was
assessed using Bland-Altman analysis. This statistical test is
widely used for the determination of the exact levels of agreement
along with the respective confidence intervals between the two
experimental methods. Bland-Altman analysis was made using the
software package GraphPad Prism v.4.0 (GraphPad Software, Inc.).
For each patient, the percentage difference between the
organ-specific LARs estimated with the low and high photon energy
was plotted against the mean LAR value. The mean percentage
difference associated with bladder or rectal cancer risk was
calculated. The 95% limits of agreement are presented as the mean
difference ±1.96 SD of the differences.
Results
Parameters derived from VMAT
plans
The mean values of the parameters associated with
the target site and critical organs, as derived from the treatment
plans of all patients, are summarized in Table III. The analysis of the DVHs
revealed that the femoral heads were not exposed to doses up to 45
Gy (V45=0%) irrespective of the X-ray beam energy used.
Moreover, no volume of the bladder or rectum received a radiation
dose >74 Gy for all VMAT plans (V74=0%). The
difference between the mean Vi of the parameters of the
urinary bladder and rectum, as determined by the VMAT plans with
6-MV and 10-MV photons, varied between 1.4 and 3.4%. The
corresponding difference for the mean V70 of the PTV and
the mean NTID was found to be 0.2 and 2.7%, respectively. Prostate
irradiation with the high photon energy resulted in a mean MU
reduction of 11.8% compared to arc therapy using low-energy
X-rays.
 | Table IIIMean value of each planning parameter
± one SD calculated from VMAT plans with 6-MV and 10-MV
photons. |
Table III
Mean value of each planning parameter
± one SD calculated from VMAT plans with 6-MV and 10-MV
photons.
| | Mean parameter
value (±SD) |
|---|
| Parameters | 6-MV VMAT | 10-MV VMAT |
|---|
| PTV | | |
|
V70
(%) | 98.6±0.4 | 98.8±0.3 |
| Bladder | | |
|
V74
(%) | 0.0 | 0.0 |
|
V69
(%) | 9.4±5.0 | 9.6±5.1 |
|
V64
(%) | 13.9±6.9 | 14.3±7.1 |
| Rectum | | |
|
V74
(%) | 0.0 | 0.0 |
|
V69
(%) | 6.9±2.5 | 7.0±2.3 |
|
V64
(%) | 12.8±4.3 | 13.2±4.3 |
|
V59
(%) | 17.4±5.5 | 18.0±5.6 |
| Femoral heads | | |
|
V45
(%) | 0.0 | 0.0 |
| Delivery time | | |
|
Monitor
units | 605.2±43.2 | 537.6±34.4 |
| Normal tissues | | |
|
NTID
(Gy/l) | 126.1±18.5 | 122.7±17.7 |
Radiation-induced bladder and rectal
cancer risks
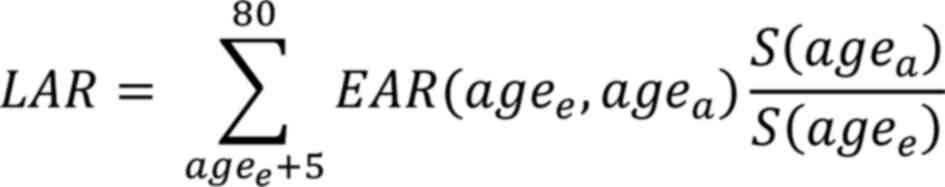
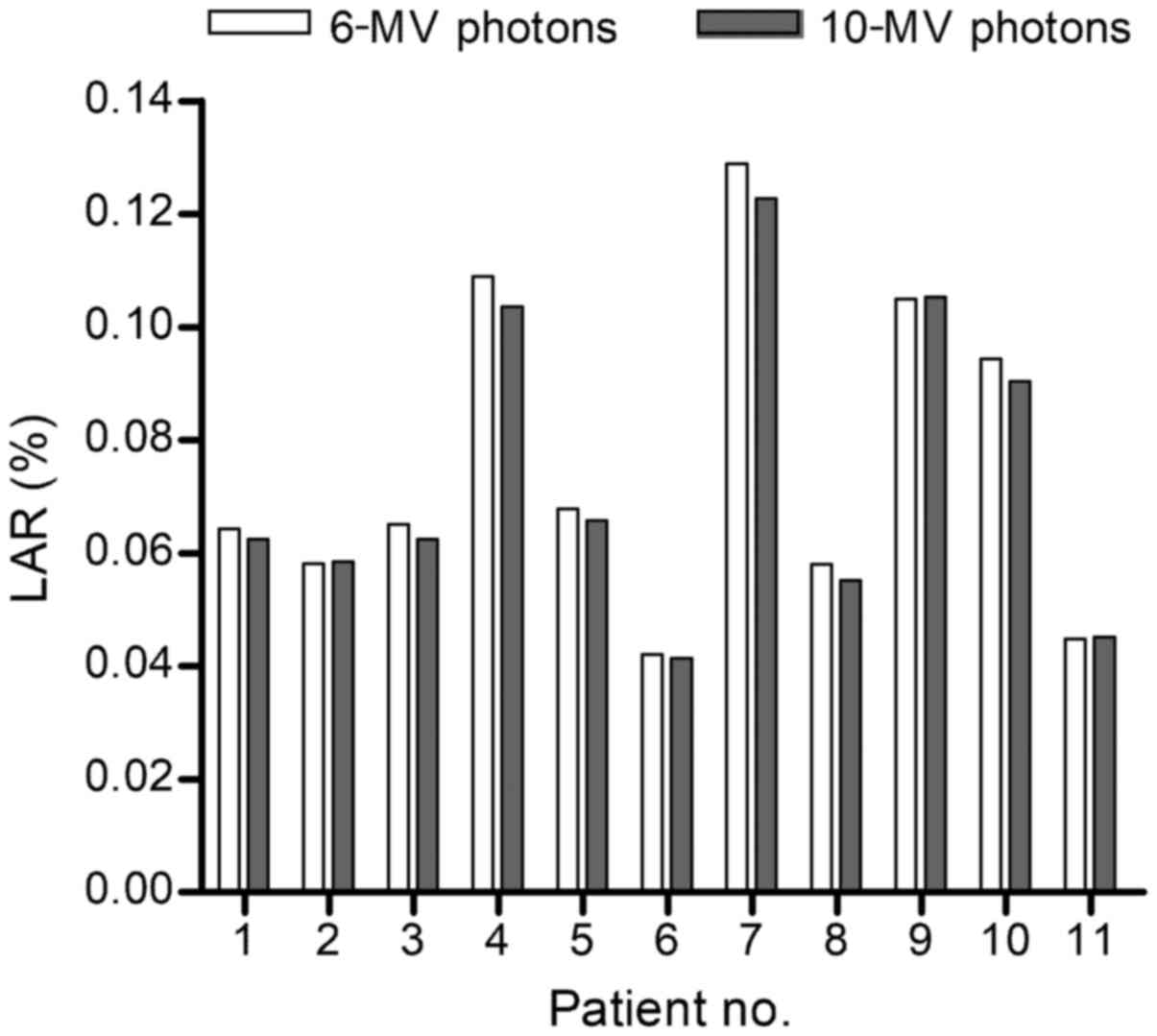
The mean OED of bladder and rectum from the 6-MV
VMAT plans of all patients was 0.65±0.18 and 8.69±0.48 Gy,
respectively. The corresponding OED due to treatment with a higher
photon energy was 0.63±0.16 and 8.63±0.50 Gy. The LAR for bladder
cancer induction from VMAT with 6-MV photons varied between 0.042
and 0.129%, whereas the use of 10-MV X-rays led to LARs of
0.041-0.123% (Fig. 2). The LAR
range for developing secondary rectal malignancies due to VMAT with
the low and high photon energy was 0.048-0.153 and 0.047-0.150%,
respectively (Fig. 3).
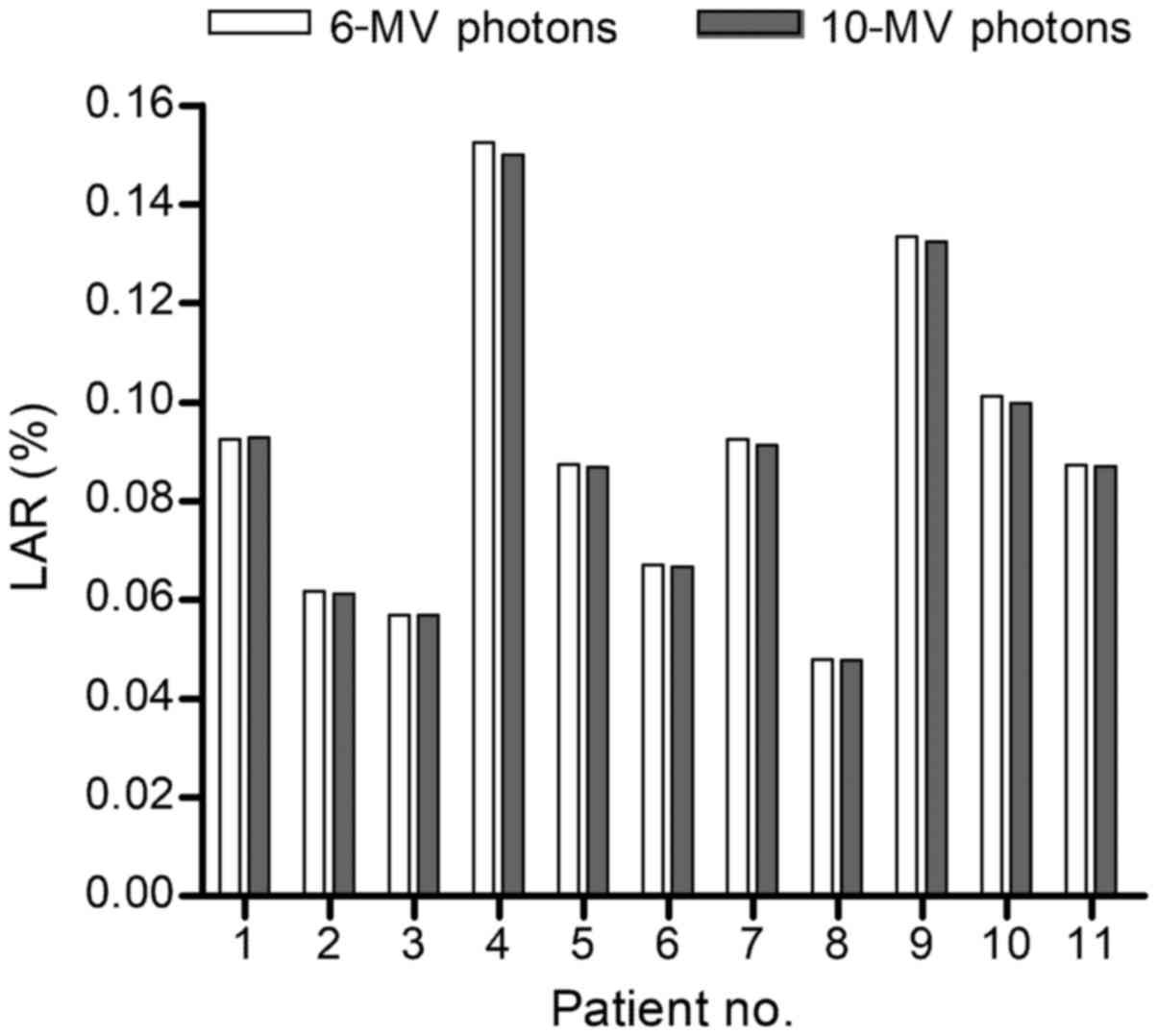
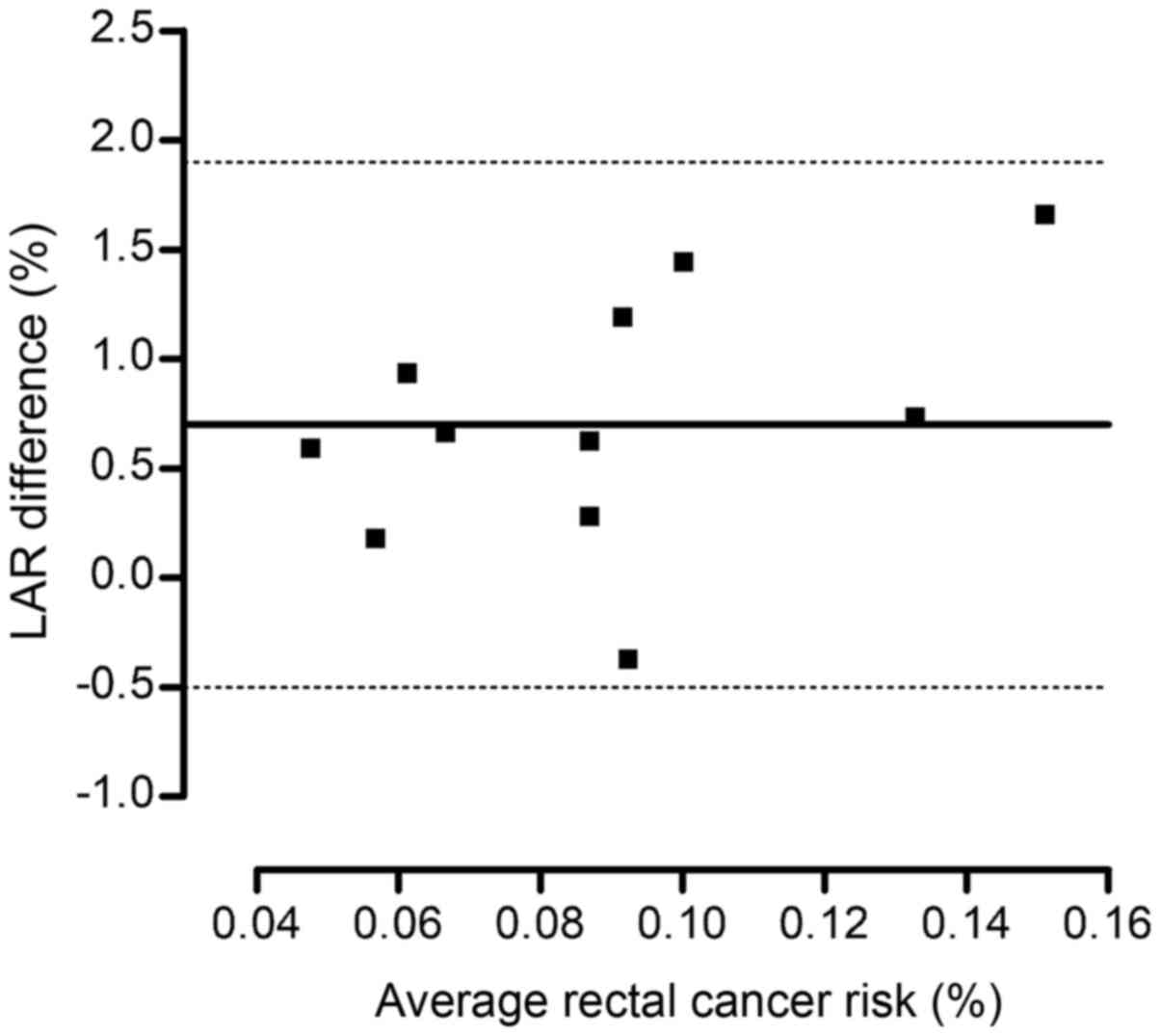
Based on the Bland-Altman analysis, the mean
percentage difference of the probability for developing bladder
malignancies from VMAT plans created with 6-MV and 10-MV photons
was 2.6±2.3% (Fig. 4). The 95%
limits of agreement were equal to-1.9 and 7.1% (Fig. 4). The corresponding mean difference
for the second rectal cancer risk was found to be 0.7±0.6%, with
limits of agreement of -0.5 and 1.9% (Fig. 5).
Discussion
In the present study, the effect of 6-MV and 10-MV
photons on the VMAT plans for prostate cancer and on the
probability for developing secondary bladder or rectal malignancies
were investigated. No attempts were made to use higher photon beam
energies for treatment planning. It is well known that there is no
neutron contamination when medical linear accelerators operate at
6-MV. The neutron production is also minimal for treatment with
10-MV X-rays (20). By contrast,
the contribution of the neutron dose to the total dose of critical
organs becomes significant when radiation therapy is delivered with
15-MV or 18 MV photon beams (20).
The DVH parameters of the two plans of each patient
satisfied the previously published dose constraints (11,13).
The differences in the mean values of the parameters related to
PTV, OARs and surrounding normal tissues, as defined by the plans
with 6-MV and 10-MV photon energies, were found to be rather small.
The aforementioned minor discrepancies are consistent with the
results of previous reports on IMRT (21) and VMAT (7) for prostate cancer. In the present
study, the only noteworthy discrepancy between the plans generated
with the two different photon energies was observed for the
treatment delivery time. The mean value of the MUs calculated for
10-MV VMAT plans was by 11.8% lower compared with that associated
with 6-MV treatment.
The lifetime risk for radiotherapy-induced bladder
malignancies varied between 0.041 and 0.129% by the patient under
investigation and the photon energy used for VMAT of prostate
cancer. The corresponding probability for developing secondary
rectal malignancies was 0.047-0.153%. The lifetime risks of
carcinogenesis were estimated from a patient group with a mean age
of 68 years subjected to hypofractionated VMAT for prostate
carcinoma up to a dose of 70 Gy. Limited information has been
published on the probability of developing secondary malignancies
from prostate irradiation using hypofractionation schedules
(13,22). The cancer risks of the present study
are consistent with those of a previous report on hypofractionated
treatment with 6-MV photons at the ages of 60 and 70 years
(13), reporting lifetime bladder
and rectal cancer risks of 0.06-0.18% and 0.07-0.20%, respectively.
Stokkevag et al (22)
provided a wide range of bladder and rectal cancer risks of
0.01-0.80% for 60-year-old patients receiving 67.5 Gy to the
prostate and simultaneously 60 Gy to the seminal vesicles in 25
fractions with 6-MV VMAT. Their estimates were obtained with a
linear-plateau association and a bell-shaped competition model.
Bladder and rectal cancer risks from standard fractionated IMRT and
VMAT for prostate carcinoma have also been reported (18,23,24).
These theoretical risks were estimated for total tumor doses of
75.6-78.0 Gy in daily fractions of 1.8-2.0 Gy. Murray et al
(18) and Fontenot et al
(23) did not report lifetime risks
of carcinogenesis. Sanchez-Nietto et al (24) reported lifetime probabilities of
0.4-0.5% from IMRT and VMAT for a prostate cancer patient aged 60
years.
The Bland-Altman statistical test revealed that the
bladder cancer risk associated with arc therapy using the low
photon energy may be up to 7.1% higher or 1.9% lower than the
respective risk value from irradiation with the high energy of
X-rays in 95% of the cases. The 95% limits of agreement for the
rectal cancer risk were -0.5 and 1.9%. These narrow limits clearly
indicate that the differences between the VMAT plans created with
6-MV and 10-MV photons in the assessment of the second cancer risks
are minor.
The cancer risk assessments in the present study
were carried out for the bladder and rectum, which are partly
exposed to primary radiation during VMAT for prostate cancer. The
use of data from treatment planning systems for out-of-field organ
dose calculations is not recommended (25). Different approaches, based either on
direct measurements using physical phantoms (26,27) or
on Monte Carlo simulations (28),
may be applied for assessing the out-of-field organ doses and the
relevant probabilities of carcinogenesis. The relatively small
sample of patients with low-risk prostate carcinoma should be
considered as a limitation of the present study. It should be noted
that this study provided lifetime bladder and rectal cancer risk
estimates derived from the use of a non-linear mechanistic model
introduced by Schneider et al (17). The model-based risk predictions may
contain several uncertainties. These uncertainties are associated
with the definition of the organ-specific parameters of the
mechanistic model. The use of the absolute values of the
model-based cancer risk predictions in clinical practice must be
viewed with caution. The PTV of the study participants included
only the prostate gland. Further studies are required to examine
the effect of beam energy on the probability of carcinogenesis in
prostate cancer patients irradiated at sites encompassing the
seminal vesicles and/or pelvic lymph nodes (7,29).
In conclusion, the VMAT plans for low-risk prostate
cancer patients generated with 6-MV or 10-MV photons were
clinically equivalent in respect to target volume coverage and
normal tissue sparing. The differences between the probabilities
for developing secondary bladder and rectal malignancies due to
pelvic VMAT with the low and high energy X-rays were found to be
minimal. Therefore, the selection of the 10-MV photons may be
considered as the optimal choice for prostate cancer treatment due
to the reduction of the treatment time.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
MM and JD designed the study. SK performed the
target and OAR contouring on CT scans. MM and JD were responsible
for treatment planning process and second cancer risk assessments.
All the authors have read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of the University Hospital of Iraklion.
Patient consent for publication
Not applicable.
Competing interests
All the authors declare that they have no competing
interests.
References
|
1
|
Siegel RA, Miller KD and Jemal A: Cancer
statistics, 2020. CA Cancer J Clin. 70:7–30. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Perez CA, Michalski JM and Zelefsky MJ:
Low-risk prostate cancer. In: Perez & Brady's Principles and
Practice of Tadiation Oncology. Halperin EC, Wazer DE, Perez CA and
Brady LW (eds). Wolters Kluwer, Philadelphia, pp1560-1601,
2019.
|
|
3
|
Wolff D, Stieler F, Welzel G, Lorenz F,
Abo-Madyan Y, Mai S, Herskind C, Polednik M, Steil V, Wenz F and
Lohr F: Volumetric modulated arc therapy (VMAT) vs. Serial
tomotherapy, step-and-shoot IMRT and 3D-conformal RT for treatment
of prostate cancer. Radiother Oncol. 93:226–233. 2009.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Palma D, Vollans E, James K, Nakano S,
Moiseenko V, Shaffer R, McKenzie M, Morris J and Otto K: Volumetric
modulated arc therapy for delivery of prostate radiotherapy:
Comparison with intensity-modulated radiotherapy and
three-dimensional conformal radiotherapy. Int J Radiat Oncol Biol
Phys. 72:996–1001. 2008.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Ren W, Sun C, Lu N, Xu Y, Han F, Liu YP
and Dai J: Dosimetric comparison of intensity-modulated
radiotherapy and volumetric-modulated arc radiotherapy in patients
with prostate cancer: A meta-analysis. J Appl Clin Med Phys.
17:254–262. 2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Cosset JM, Nassf M, Saidi R, Pugnaire J,
Ben Abdennebi A and Noel A: Which photon energy for
intensity-modulated radiotherapy and volumetric-modulated arc
therapy in 2019? Cancer Radiother. 23:58–61. 2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Pasler M, Georg D, Wirtz H and Lutterbach
J: Effect of photon-beam energy on VMAT and IMRT treatment plan
quality and dosimetric accuracy for advanced prostate cancer.
Strahlenther Onkol. 187:792–798. 2011.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Kleiner H and Podgorsak MB: The dosimetric
significance of using 10-MV photons for volumetric modulated arc
therapy for post-prostatectomy irradiation of the prostate bed.
Radiol Oncol. 50:232–237. 2016.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Stanley DN, Popp T, Ha CS, Swanson GP, Eng
TY, Papanikolaou N and Gutierez AN: Dosimetric effect of photon
beam energy on volumetric modulated arc therapy treatment plan
quality due to body habitus in advanced prostate cancer. Pract
Radiat Oncol. 5:e625–e633. 2015.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Mattes MD, Tai C, Lee A, Ashamalla H and
Ikoro NC: The dosimetric effects of photon energy on the quality of
prostate volumetric modulated arc therapy. Pract Radiat Oncol.
4:e39–e44. 2014.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Lee WR, Dignam JJ, Amin MB, Bruner DW, Lo
D, Swanson GP, Shah AB, D'Souza DP, Michalski JM, Dayes IS, et al:
Randomized phase III noninferiority study comparing two
radiotherapy fractionation schedules in patients with low-risk
prostate cancer. J Clin Oncol. 34:2325–2332. 2016.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Morgan SC, Hoffman K, Loblaw DA,
Buyyounouski MK, Patton C, Barocas D, Bentzen S, Chang M,
Efstathiou J, Greany P, et al: Hypofractionated radiation therapy
for localized prostate cancer: Executive summary of an ASTRO, ASCO,
and AUA evidence-based guideline. J Urol. 201:528–534.
2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Mazonakis M, Kachris S and Damilakis J:
Secondary bladder and rectal cancer risk estimates following
standard fractionated and moderately hypofractionated VMAT for
prostate carcinoma. Med Phys. 47:2805–2813. 2020.PubMed/NCBI View
Article : Google Scholar
|
|
14
|
Wallis CJ, Mahar AL, Choo R, Herschom S,
Kodama RT, Shah PS, Danjoux C, Narod SA and Nam RK: Second
malignancies after radiotherapy for prostate cancer: Systematic
review and meta-analysis. BMJ. 352(i851)2016.PubMed/NCBI View
Article : Google Scholar
|
|
15
|
Dasu A and Toma-Dasu I: Models for the
risk of secondary cancer from radiation therapy. Phys Med.
42:232–238. 2017.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Mazonakis M and Damilakis J: Cancer risk
after radiotherapy for benign diseases. Phys Med. 42:285–291.
2017.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Schneider U, Sumila M and Robotka J:
Site-specific dose-response relationships for cancer induction from
the combined Japanese A-bomb and Hodgkin cohorts for doses relevant
to radiotherapy. Theor Biol Med Model. 8(27)2011.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Murray LJ, Thompson CM, Lilley J, Cosgrove
V, Franks K, Sebag-Montefiore D and Henry AM: Radiation-induced
second primary cancer risks from modern external beam radiotherapy
for early prostate cancer: Impact of stereotactic ablative
radiotherapy (SABR), volumetric modulated arc therapy (VMAT) and
flattening filter free (FFF) radiotherapy. Phys Med Biol.
60:1237–1257. 2015.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Arias E: United States life tables, 2017.
Natl Vital Stat Rep. 68:1–66. 2019.PubMed/NCBI
|
|
20
|
Kry SF, Salehpour M, Followill DS, Stovall
M, Kuban DA, White RA and Rosen II: The calculated risk of fatal
secondary malignancies from intensity-modulated radiation therapy.
Int J Radiat Oncol Biol Phys. 62:1195–1203. 2005.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Pirzkall A, Carol MP, Pickett B, Xia P,
Roach M III and Verhey LJ: The effect of beam energy and number of
fields on photon-based IMRT for deep-seated targets. Int J Radiat
Oncol Biol Phys. 53:434–442. 2002.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Stokkevag CH, Engeseth GM, Hysing LB,
Ytre-Hauge KS, Ekanger C and Muren LP: Risk of radiation-induced
secondary rectal and bladder cancer following radiotherapy of
prostate cancer. Acta Oncol. 54:1317–1325. 2015.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Fontenot JD, Lee AK and Newhauser WD: Risk
of secondary malignant neoplasms from proton therapy and intensity
modulated X-ray therapy for early-stage prostate cancer. Int J
Radiat Oncol Biol Phys. 74:616–622. 2009.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Sanchez-Nietto B, Romero-Exposito M,
Terron JA, Irazola L, Garcia Hernandez MT, Mateos JC, Rosello J,
Planes D, Paiusco M and Sanchez-Doblado F: External phοton
radiation treatment for prostate cancer: Uncomplicated and
cancer-free probability assessment of 36 plans. Phys Med. 66:88–96.
2019.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Kry SF, Bednarz B, Howell RM, Dauer L,
Followill D, Klein E, Paganetti H, Wang B, Wuu CS and George Xu X:
AAPM TG-158: Measurement and calculation of doses outside the
treated volume from external-beam radiation therapy. Med Phys.
44:e391–e429. 2017.PubMed/NCBI View
Article : Google Scholar
|
|
26
|
Mazonakis M, Damilakis J, Varveris H,
Theoharopoulos N and Gourtsoyiannis N: A method of estimating fetal
dose during brain radiation therapy. Int J Radiat Oncol Biol Phys.
44:455–459. 1999.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Mazonakis M, Damilakis J, Varveris H and
Gourtsoyiannis N: Therapeutic external irradiation in women of
reproductive age: Risk estimation of hereditary effects. Br J
Radiol. 77:847–850. 2004.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Bednarz B, Athar B and Xu XG: A
comparative study on the risk of second primary cancers in
out-of-field organs associated with radiotherapy of localized
prostate carcinoma using Monte Carlo-based accelerator and patient
models. Med Phys. 37:1987–1994. 2010.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Bahtiyar N, Onaran I, Aydemir B, Batykara
O, Toplan S, Agaoglu FY and Akyolcu MC: Monitoring of platelet
function parameters and microRNA expression levels in patients with
prostate cancer treated with volumetric modulated arc radiotherapy.
Oncol Lett. 16:4745–4753. 2018.PubMed/NCBI View Article : Google Scholar
|