Introduction
Disseminated intravascular coagulation (DIC) is a
well-known hemostatic complication of solid tumors. It is usually
identified at the time of presentation and can sometimes cause
excessive bleeding or thromboembolic complication. In comparison,
primary angiosarcoma of the breast (PASB) is a malignant primary
endothelial neoplasm of mammary parenchyma that is not associated
with radiation exposure. The median age of patients at diagnosis is
40 years, compared with a median age of 70 years for the secondary
angiosarcoma (1). Adem et al
(2) reported that angiosarcoma
accounts for one-fourth of all breast sarcomas, excluding
metaplastic carcinomas and phyllodes tumors. D'Angelo et al
(3) performed a retrospective
analysis of 119 patients with metastatic angiosarcoma, 24% of which
had radiation-associated angiosarcoma. The most frequent primary
sites were the chest wall/breast (37.31%), viscera (22%), and
head/neck (20%). The median overall survival of patients with
metastatic angiosarcoma with origin at all sites was 12.1 months.
Even if DIC is a common complication associated with angiosarcomas
and often interferes with patients' chemotherapy (4), there have been few case reports on
anticoagulant therapies for DIC associated with angiosarcoma
because angiosarcoma is rare. In the current study, we present a
rare case of a PASB with DIC that was controllable by a
self-subcutaneous injection of unfractionated heparin calcium
(UFH).
Case report
In November 2019, a 47-year-old woman with a breast
tumor and multiple lung and bone metastases was referred to our
hospital for further diagnosis and treatment. She had consulted a
nearby hospital complaining of swelling of the left breast in July
2018. Imaging examinations revealed a giant mass in her breast.
Core needle biopsy was performed, resulting in the histological
diagnosis of hemangioma. Lumpectomy was performed in September
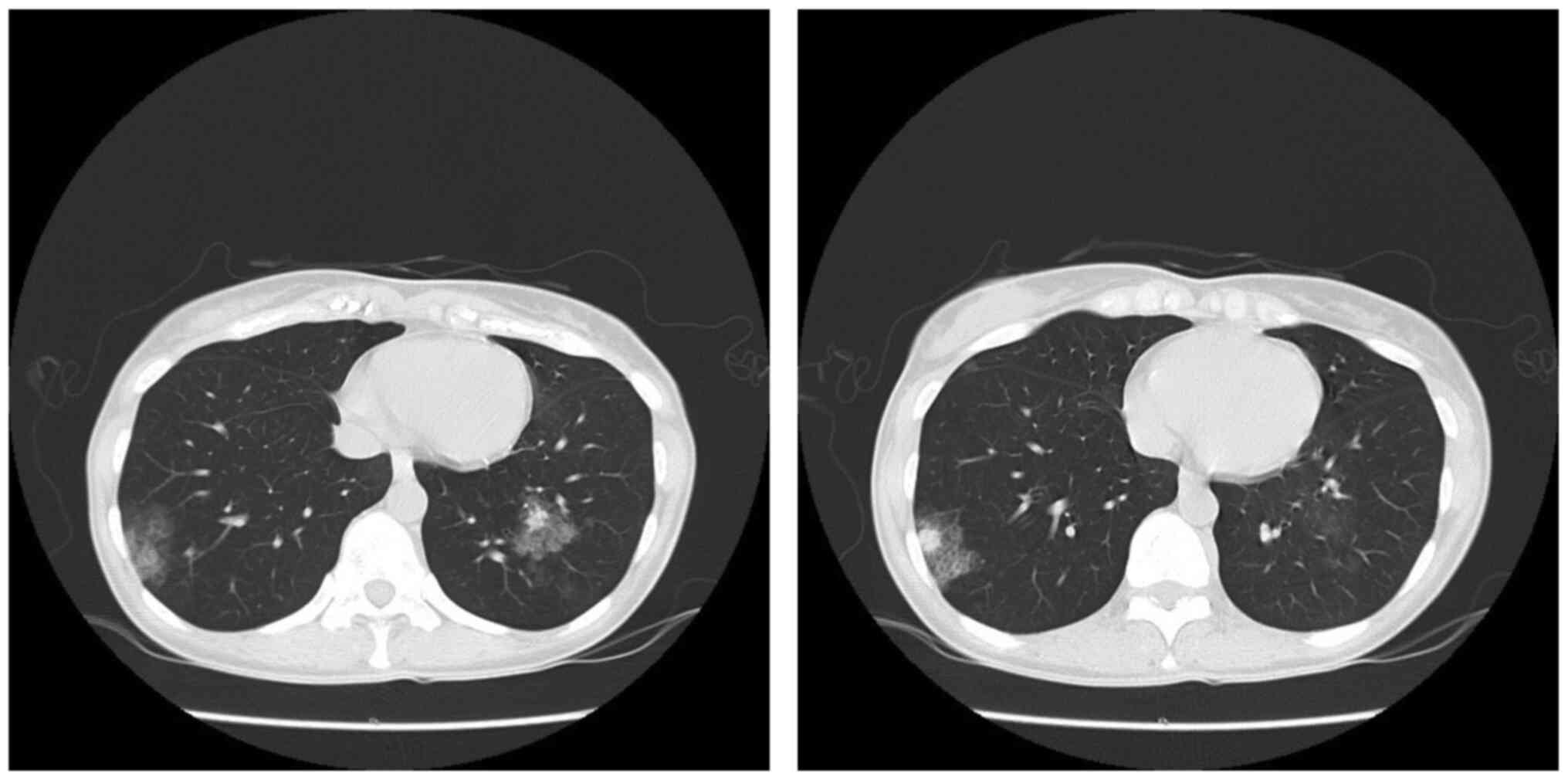
2018. In August 2019, her left nipple became swollen, and computed
tomography (CT) revealed bilateral multiple lung and bone
metastases (Fig. 1). At this point,
a malignant tumor was suspected and she was transferred to our
hospital.
She was admitted to our hospital in November 2019.
Upon admission, a red mass that was 3 cm in diameter was observed
on the left nipple during physical examination. Whole body magnetic
resonance imaging revealed multiple bone metastases in the
vertebra, sternum, ilium, bilateral humeri, and bilateral femurs.
Laboratory tests yielded the following results (Table I): White blood
cells=4.67x109/l, hemoglobin=11.3 g/dl, platelet
count=79x109/l [normal range (NR):
158-348x109/l], total bilirubin=0.6 mg/dl, aspartate
aminotransferase=17 U/l, alanine aminotransferase=9 U/l, lactate
dehydrogenase=323 U/l (NR: 124-222 U/l), blood urea nitrogen=15
mg/dl, creatinine=0.64 mg/dl, prothrombin time-international
normalized ratio (PT-INR)=1.12, activated partial thromboplastin
time (APTT)=31.8 sec, fibrinogen=127 mg/dl (NR: 200-400 mg/dl),
fibrinogen/fibrin degradation product=297.9 µg/ml (NR <5.0
µg/ml), and D-dimer=112.9 µg/ml (NR <1.0 µg/ml). Her laboratory
data met the diagnostic criteria (6 points) for DIC from the
Japanese Society on Thrombosis and Hemostasis (5). However, there were no signs of deep
vein thrombosis or pulmonary embolism, or signs of bleeding
tendency such as subcutaneous bleeding or mucosal bleeding.
 | Table ISummary of laboratory data. |
Table I
Summary of laboratory data.
| Parameter | Normal range | 1st Admission | 2nd Admission |
|---|
| Complete blood
count | | | |
|
White blood
cells (x109/l) | 3.30-8.60 | 4.67 | 3.35 |
|
Hemoglobin
(g/dl) | 11.6-14.8 | 11.3 | 9.3 |
|
Platelets
(x109/l) | 158-348 | 79 | 52 |
| Biochemistry | | | |
|
Aspartate
aminotransferase (U/l) | 13-30 | 17 | 23 |
|
Alanine
aminotransferase (U/l) | 7-23 | 9 | 22 |
|
Lactate
dehydrogenase (U/l) | 124-222 | 323 | 433 |
|
Total
bilirubin (mg/dl) | 0.4-1.5 | 0.6 | 0.4 |
|
Blood urea
nitrogen (mg/dl) | 8.0-20.0 | 15.0 | 12.0 |
|
Creatinine
(mg/dl) | 0.47-0.79 | 0.64 | 0.51 |
|
Total
protein (g/dl) | 6.6-8.1 | 7.9 | 6.7 |
|
C-reactive
protein (mg/dl) | <0.14 | 0.14 | 0.09 |
| Coagulation | | | |
|
PT-INR | 0.85-1.20 | 1.12 | 1.22 |
|
APTT
(sec) | 24.0-39.0 | 31.8 | 30.9 |
|
AT-3
(%) | 75-130 | 100 | 100 |
|
Fibrinogen
(mg/dl) | 200-400 | 127 | 84 |
|
FDP
(µg/ml) | <5.0 | 297.9 | No data |
|
D-dimer
(µg/ml) | <1.0 | 112.9 | 215.8 |
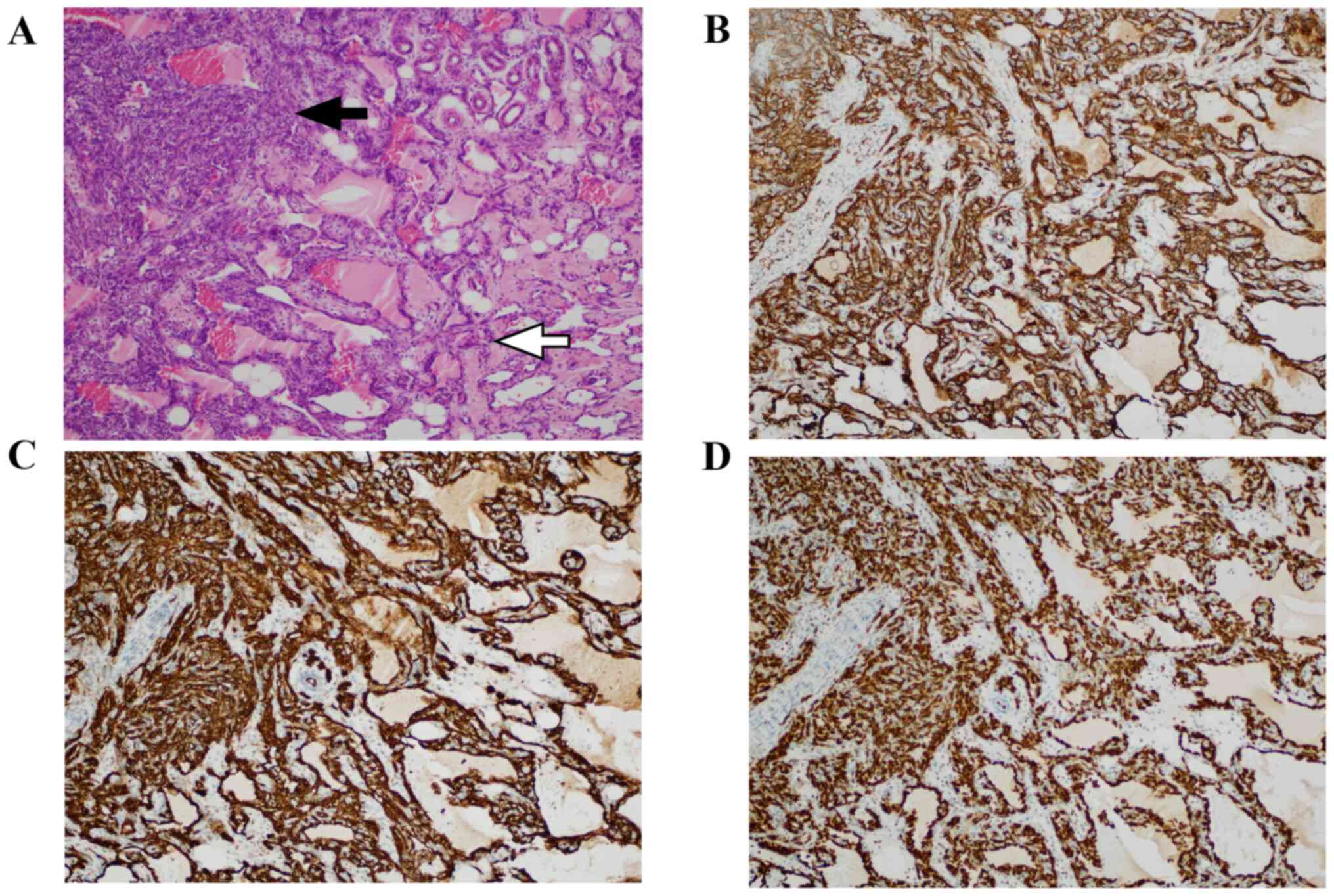
Re-examination of the resected left breast tumor by
our hospital pathologists resulted in the diagnosis of high-grade
angiosarcoma, as the mass was mainly composed of atypically
anastomosing vessels that spread invasively, and dense solid foci
containing oval or spindle cells with nuclear enlargement and
hyperchromasia (Fig. 2). Tumor
cells were immunohistochemically positive for cluster of
differentiation (CD)34, CD31, and erythroblast
transformation-specific [ETS]-related gene (ERG). The
immunohistochemistry was performed using monoclonal antibodies for
CD34 (clone QBEnd/10, cat. no. 518-102418, Roche), CD31 (clone
JC70, cat. no. 518-103231, Roche), and ERG (clone EPR3864, cat. no.
518-110819, Roche). The immunostaining was performed using a
Ventana BenchMark ULTRA IHC/ISH Staining Module®.
Antigen retrieval was performed by placing tissue sections in ULTRA
CC1 buffer (pH 9.0) for the optimum amount of time (32-64 min).
Subsequently, slides were incubated at 37˚C for varying amounts of
time: 8 min for CD34, 32 min for CD31, and 24 min for ERG. The
OptiVIEW DAB Detection Kit (Ventana Medical Systems, Inc.) was used
to detect the mouse IgG, mouse IgM, and rabbit primary antibodies.
Slides were then counterstained with hematoxylin.
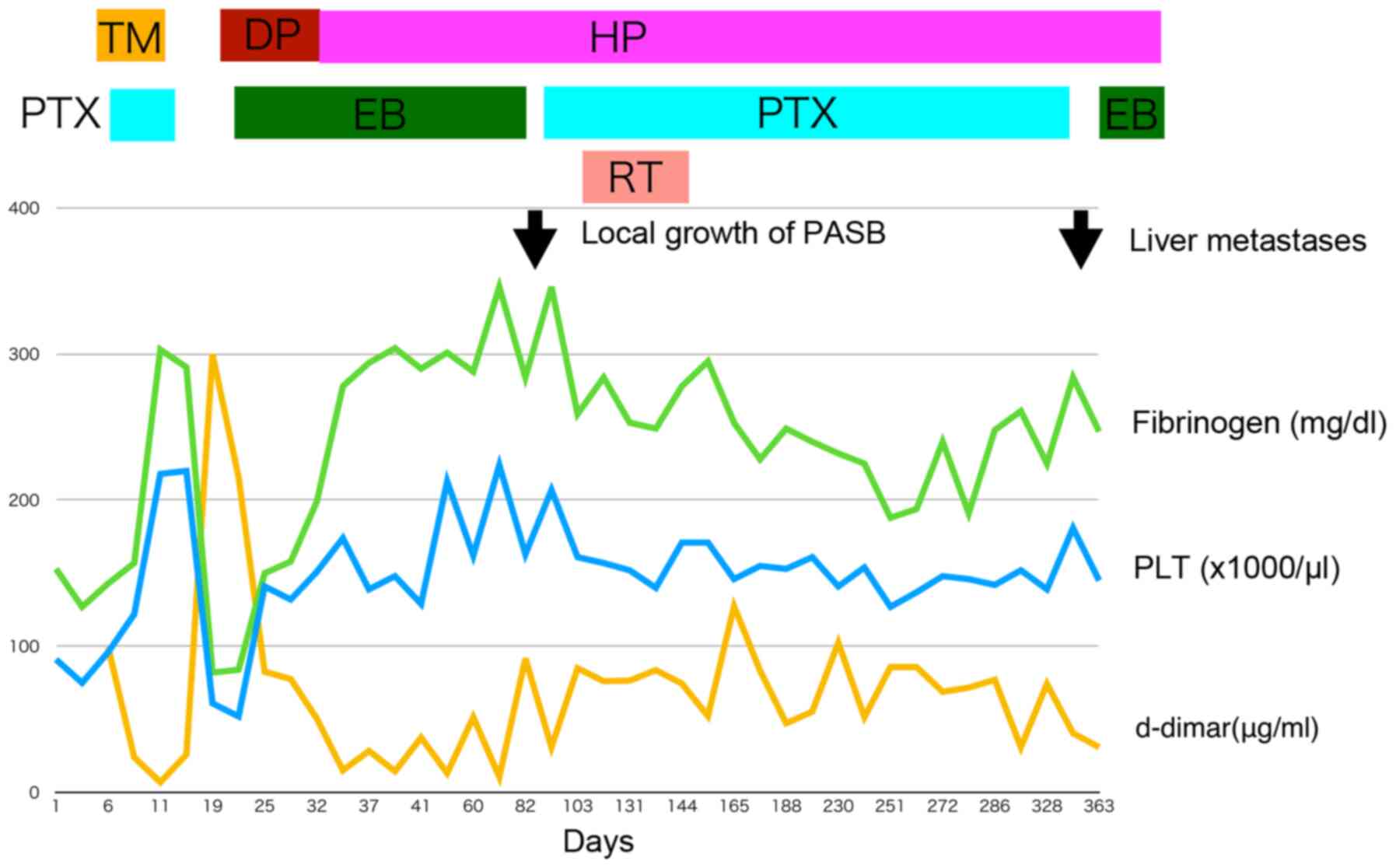
Thrombomodulin-α (380 U/kg) was started on the day
of admission and lasted for 7 days. Weekly PTX infusion (100
mg/m2) was started on the second day. Her hemostasis
test improved and she was discharged 13 days after admission.
However, she was hospitalized a second time 3 days after discharge
because her DIC relapsed.
On her second admission, hemostasis tests yielded
the following results: Platelet count=52x109/l,
PT-INR=1.22, APTT=30.9 sec, fibrinogen=84 mg/dl, and D-dimer=215.8
µg/ml. At this point, we decided that angiosarcoma activity and DIC
were uncontrollable by mono-chemotherapy of PTX. Therefore, to
control DIC, danaparoid sodium (1,250 units, every 12 h) was
infused for 13 days, and chemotherapy was switched from PTX to
eribulin mesylate (1.4 mg/m2; infusions performed on
days 1 and 8, of every 21-day cycle). After treatment with
danaparoid sodium was started, her DIC had improved. For outpatient
treatment, infusion of danaparoid sodium was switched to
self-subcutaneous injection of UFH (5,000 units, once every 12 h).
After this anticoagulant change, her DIC remained controllable, and
eribulin mesylate was continued for 2 months (Fig. 3).
CT in February 2020 revealed an increase in the left
breast mass, whereas lung metastatic lesions became reduced.
Eribulin mesylate was stopped and chemoradiotherapy was performed,
which consisted of intensity-modulated radiotherapy (total 60 Gy/30
fraction) and concurrent weekly PTX infusions (63
mg/m2), as well as self-subcutaneous injections of UFH.
PTX was re-started because a previous report suggested that
chemoradiotherapy with taxane and maintenance chemotherapy in
cutaneous angiosarcoma were efficacious (6), but there have been no reports of
eribulin mesylate with radiotherapy.
After the radiotherapy, PTX (63 mg/m2;
infusions performed on days 1, 8, and 15 of every 28-day cycle) was
continued as a maintenance therapy for 6 months. In November 2020,
multiple liver metastases were diagnosed by follow-up CT, but her
DIC remained stable, and PTX was replaced by eribulin mesylate (1.1
mg/m2; infusions performed on days 1, day 8, of every
21-day cycle) again. At the time of reporting, the patient has been
continuing the self-subcutaneous injections of UFH as well as
eribulin mesylate infusions. No adverse events associated with UFH
use have been observed. Her PASB remained in stable disease,
whereas DIC became controllable.
Discussion
DIC is a common complication associated with
angiosarcoma and often interferes with a patient's chemotherapy.
Farid et al (4)
retrospectively reviewed case records of 42 patients diagnosed with
angiosarcoma at Mount Sinai Hospital, wherein 7 patients (17%) met
clinical criteria for DIC. In their report, all patients who
received systemic antineoplastic therapy with resultant disease
response or stability had their DIC resolved in tandem with
clinical improvement. DIC also recurred at the time of disease
progression in all cases. Only a few case reports mention
anticoagulant therapies for DIC associated with angiosarcoma. Honda
et al (7) reported the first
case of a patient having primary cardiac angiosarcoma with
coexisting DIC who was successfully treated with nab-PTX. This
patient's DIC, treated with transfusion of fresh-frozen plasma and
recombinant thrombomodulin-α (used for 6 days), improved shortly
after the initiation of chemotherapy. Rosen et al (8) reported a case of hepatic angiosarcoma
with a primary focus on the management of the patient's DIC. In
their report, the patient's DIC became controlled after initial
treatment with unfractionated heparin and subsequent enoxaparin
treatment.
In our study, the patient's DIC improved through
chemotherapy with PTX and recombinant thrombomodulin-α. However, it
re-exacerbated soon after recombinant thrombomodulin-α was
completed. As a second treatment for DIC, danaparoid sodium was
used and her DIC improved again. To switch from inpatient treatment
to outpatient treatment, infusion of danaparoid sodium was switched
to self-subcutaneous injections of UFH. This UFH resulted in
long-term stabilization of DIC (>13 months) and made the
continuity of chemotherapy and chemoradiotherapy possible as an
outpatient treatment.
Based on the degree of fibrinolytic activation,
there are diverse subtypes in DIC, such as
suppressed-fibrinolytic-type, balanced-fibrinolytic-type, and
enhanced-fibrinolytic-type (9). Our
patient's laboratory findings, that was measured under the
treatment of UFT, showed a marked elevation in both
thrombin-antithrombin complex (more than 120.0 ng/ml: NR<4
ng/ml) and plasmin-α 2 plasmin complex (8.5 µg/ml: NR 0-0.8 µg/ml).
We speculated that our patient had enhanced-fibrinolytic-type DIC.
For this type of DIC, combination therapy with heparin and
tranexamic acid has been reported to be very effective (9). In our case, addition of tranexamic
acid was not considered because there was no bleeding symptom, and
her DIC was in a stable condition at the time of UFH start. The
mean survival time in metastatic disease was 6.4 months (range:
1-11 months) in 7 cases of angiosarcoma with DIC reported by Farid
et al (4). Therefore, we
speculate that the use of UFH helped prolong our patient's life.
Mono-chemotherapy with PTX after first-line anticoagulant therapy
with recombinant thrombomodulin-α could not stabilize DIC, but
combination therapy of PTX and UFT after chemoradiotherapy could.
So, we considered that UFH, rather than PTX, contributed to the
stabilization of her DIC.
Self-subcutaneous injection of heparin is effective
for chronic DIC associated with aortic aneurysm and vascular
malformations, and is sometimes indicated for these patients
(10,11). However, there have been few case
reports where it was used to treat DIC with malignancy. Some
studies on cancers other than angiosarcoma reported results similar
to ours. Makari et al (12)
reported a case of gastric cancer with Trousseau's syndrome and
pulmonary embolism treated with S-1 while receiving subcutaneous
injections of heparin. Odani et al (13) reported a case of Trousseau's
syndrome caused by clear cell adenocarcinoma of the ovary, wherein
the patient received four courses of PTX and carboplatin
chemotherapy while receiving subcutaneous injections of
unfractionated heparin.
In Japan, many oncologists tend to try first-line
chemotherapy with anticoagulant therapy for solid tumors with DIC.
However, once the patient's DIC relapses, if there is no
second-line chemotherapy with a high response rate, they often
decide that the tumors, as well as DIC, are beyond control and
hence give up on aggressive treatments. Our case suggests that if
self-subcutaneous injections of UFH are used, some patients with
PASB complicated by DIC can continue to receive chemotherapies or
chemoradiotherapies in the outpatient setting without impairing
quality of life. Nevertheless, we would like to acknowledge a
limitation in this case report. Including our case, there have been
few case reports on DIC associated with malignancies treated by
self-subcutaneous injection of UFH. DIC associated with more
aggressive PASB may not be controllable by self-subcutaneous
injections of UFH. This study is based on only one case report;
therefore, further prospective investigations are needed to
elucidate the clinical efficacy of self-subcutaneous injections of
UFH for the treatment of PASB with DIC.
In summary, we reported the case of a woman with
PASB complicated by DIC. The DIC relapsed after the first line
anticoagulant therapy of thrombomodulin-α, but the second line
danaparoid sodium followed by self-subcutaneous injection of UFH
resulted in long-term stabilization of the DIC. Our case suggests
that if self-subcutaneous injections of UFH are used, some patients
diagnosed with PASB with DIC can continue to receive chemotherapies
or chemoradiotherapies in the outpatient setting without having
their quality of life impaired. Nevertheless, further prospective
clinical trials are needed to verify the efficacy of
self-subcutaneous injection of UFH in similar settings.
Acknowledgements
The authors would like to thank Mr. Kikuichi
Nakagawa for his technical assistance.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
TY conceived the present study. HN pathologically
diagnosed the patient and revised the manuscript. TW, YI, HT, HS,
KY, MW and ST collected clinical data. All authors read and
approved the final manuscript prior to submission. TY and ST
confirm the authenticity of all the raw data.
Ethics approval and consent to
participate
The soft tissue mass of the patients was collected
after written informed consent was obtained from the patient
according to the protocol approved by the Osaka International
Cancer Institute (Osaka, Japan).
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of patient data and associated
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Antonescu CR, Hunt KK, Rowe JJ and Thway
K: Primary angiosarcoma of the breast. In: Breast Tumours. 5th
edition. WHO Classification of Tumours Editorial Board (ed.)
International Agency for Research on Cancer, Lyon, pp200-201,
2019.
|
|
2
|
Adem C, Reynolds C, Ingle JN and
Nascimento AG: Primary breast sarcoma: Clinicopathologic series
from the Mayo clinic and review of the literature. Br J Cancer.
91:237–241. 2004.PubMed/NCBI View Article : Google Scholar
|
|
3
|
D'Angelo SP, Munhoz RR, Kuk D, Landa J,
Hartley E, Bonafede M, Dickson MA, Gounder M, Keohan ML, Crago AM,
et al: Outcomes of systemic therapy for patients with metastatic
angiosarcoma. Oncology. 89:205–214. 2015.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Farid M, Ahn L, Brohl A, Cioffi A and Maki
RG: Consumptive coagulopathy in angiosarcoma: A recurrent
phenomenon? Sarcoma. 2014(617102)2014.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Asakura H, Takahashi H, Uchiyama T, Eguchi
Y, Okamoto K, Kawasugi K, Kobayashi T, Taki M, Tujinaka T, et al:
Diagnostic criteria for DIC from the Japanese Society on Thrombosis
and Hemostasis-2017 edition. Jpn J Thromb Hemost. 28:369–391.
2017.(In Japanese).
|
|
6
|
Fujisawa Y, Yoshino K, Kadono T, Miyagawa
T, Nakamura Y and Fujimoto M: Chemoradiotherapy with taxane is
superior to conventional surgery and radiotherapy in the management
of cutaneous angiosarcoma: A multicentre, retrospective study. Br J
Dermatol. 171:1493–1500. 2014.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Honda K, Ando M, Sugiyama K, Mitani S,
Masuishi T, Narita Y, Taniguchi H, Kadowaki S, Ura T and Muro K:
Successful treatment of cardiac angiosarcoma associated with
disseminated intravascular coagulation with nab-paclitaxel: A case
report and review of the literature. Case Rep Oncol. 10:863–870.
2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Rosen EA, Vallurupalli M, Choy E, Lennerz
JK and Kuter DJ: Management of disseminated intravascular
coagulation in a patient with hepatic angiosarcoma: A case report.
Medicine (Baltimore). 97(e13321)2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Asakura H: Classifying types of
disseminated intravascular coagulation: Clinical and animal models.
J Intensive Care. 2(20)2014.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Miyahara S, Yasu T, Yamada Y, Kobayashi N,
Saito M and Momomura S: Subcutaneous injection of heparin calcium
controls chronic disseminated intravascular coagulation associated
with inoperable dissecting aortic aneurysm in an outpatient clinic.
Intern Med. 46:727–732. 2007.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Yamada S and Asakura H: Management of
disseminated intravascular coagulation associated with aortic
aneurysm and vascular malformations. Int J Hematol. 113:15–23.
2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Makari Y, Nagase H, Iijima S, Miyo M,
Sakamoto T, Doi T, Hoshi M, Miyake Y, Oshima S, Ikeda K, et al: A
case of advanced gastric cancer with Trousseau syndrome and
pulmonary embolism. Gan To Kagaku Ryoho. 39:2363–2365.
2012.PubMed/NCBI(In Japanese).
|
|
13
|
Odani N, Ono T, Kusumoto A, Sanada Y, Oda
H, Tanabe R, Nishimura M, Takikawa K, Matsumoto K, et al: A case of
Trousseau's syndrome: Multiple cerebral infarction caused by clear
cell adenocarcinoma of the ovary. Tokyo Sanka Fujinka Gakkai
Zasshi. 64:509–514. 2015.(In Japanese).
|