Introduction
Gray zone lymphoma (GZL) is a rare type of B-cell
lymphoma, with features intermediate between diffuse large B-cell
lymphoma (DLBCL) and classical Hodgkin lymphoma (cHL) (1). Despite advancements in
immunophenotyping and molecular diagnostics in addition to the
conventional morphologic approach, the diagnosis of GZL remains
complex and challenging (2).
Although GZL is commonly observed in young adults, the survival of
patients with GZL is worse than that of patients with DLBCL or cHL.
That is, one-third of patients present with primary refractory
disease, and the 2-year progression-free survival (PFS) rate is
~40% (3,4). Although its outcomes are inferior, an
optimal treatment strategy for relapsed/refractory (R/R) GZL has
not yet been identified. Allogenic stem cell transplantation (SCT)
for R/R GZL may be a treatment option. However, the incidence of
transplant-related mortality (TRM) or graft-versus-host disease is
still a major problem. Therefore, more effective and less toxic
therapy should be developed for patients with R/R GZL.
Brentuximab vedotin (BV), an anti-CD30 antibody drug
conjugate, is highly effective for different types of lymphomas,
including CD30-positive non-Hodgkin lymphoma and cHL (5-7).
Recently, in the AETHERA trial, BV maintenance after autologous SCT
(ASCT) had a statistically significant prognostic impact in
patients with R/R cHL (8). However,
only few studies showed that BV + conventional chemotherapy is
effective for treatment-naïve GZL or BV maintenance therapy for R/R
GZL (5,9,10).
Herein, we report a patient with R/R GZL that is highly resistant
to conventional chemotherapy and radiation therapy (RT). The
patient achieved long-term remission after receiving BV maintenance
treatment after ASCT.
Case report
A 19-year-old male patient was referred to our
institution for further examination of left neck and right axillary
lymphadenopathy and anterior mediastinal mass without B symptoms.
The patient's lactate dehydrogenase and soluble interleukin-2
receptor levels were high at 317 U/l (normal upper limit: 245 U/l)
and 2,040 U/ml, respectively. With consideration of malignant
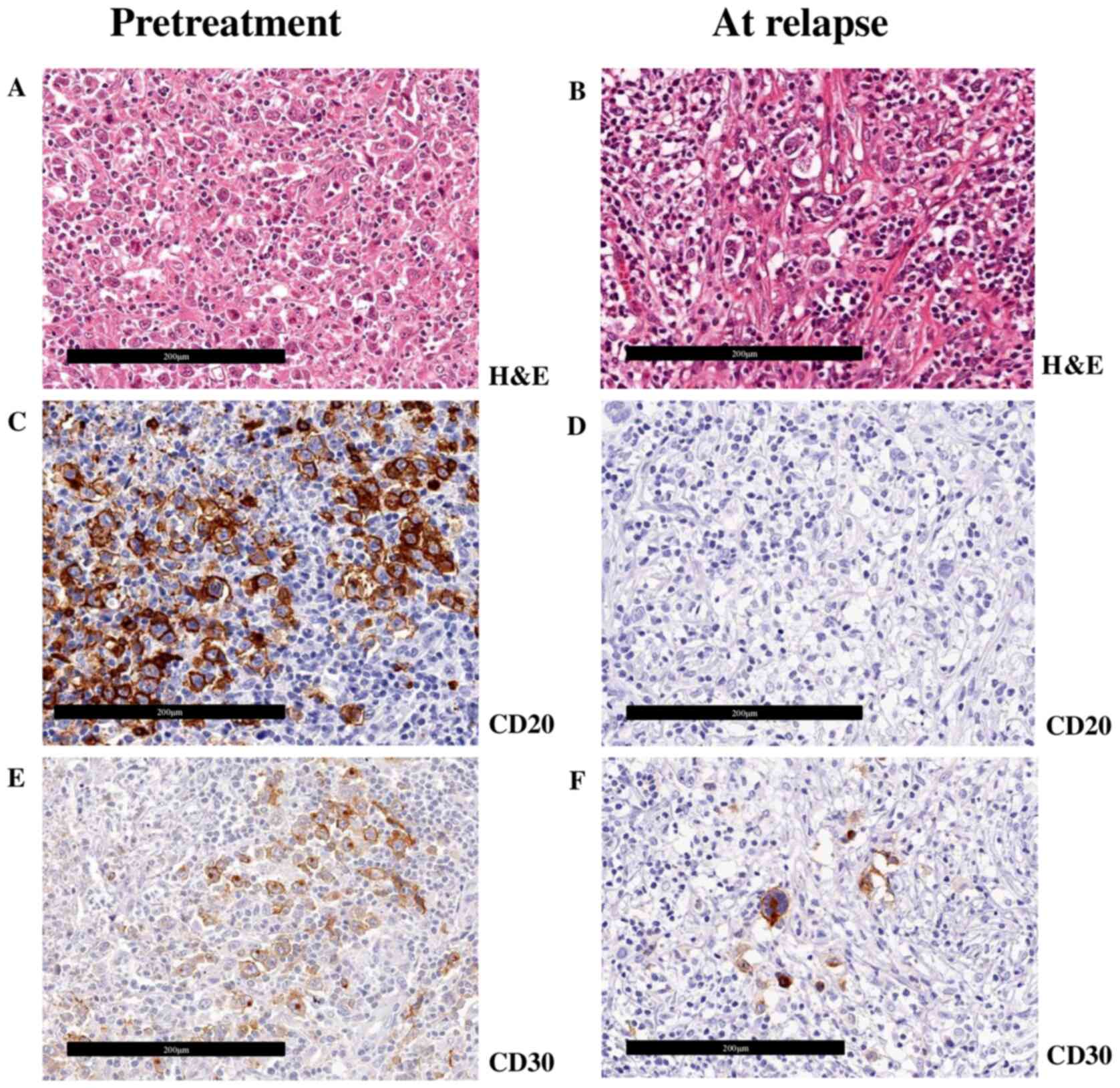
lymphoma, the patient underwent left neck lymph node biopsy. The
pathological finding showed morphologic proliferation of atypical
large lymphoma cells and the presence of few polynuclear
Reed-Sternberg (RS)-like cells surrounded by infiltrating
inflammatory cells (Fig. 1A). On
immunohistochemical studies, the large lymphoma cells were positive
for CD15, CD20 (Fig. 1C), CD30
(Fig. 1E), CD79a, PAX-5, and PD-L1
and were negative for CD5 and EBER. The Ki-67 index was 80%.
Collectively, after a cautious review, the patient was diagnosed
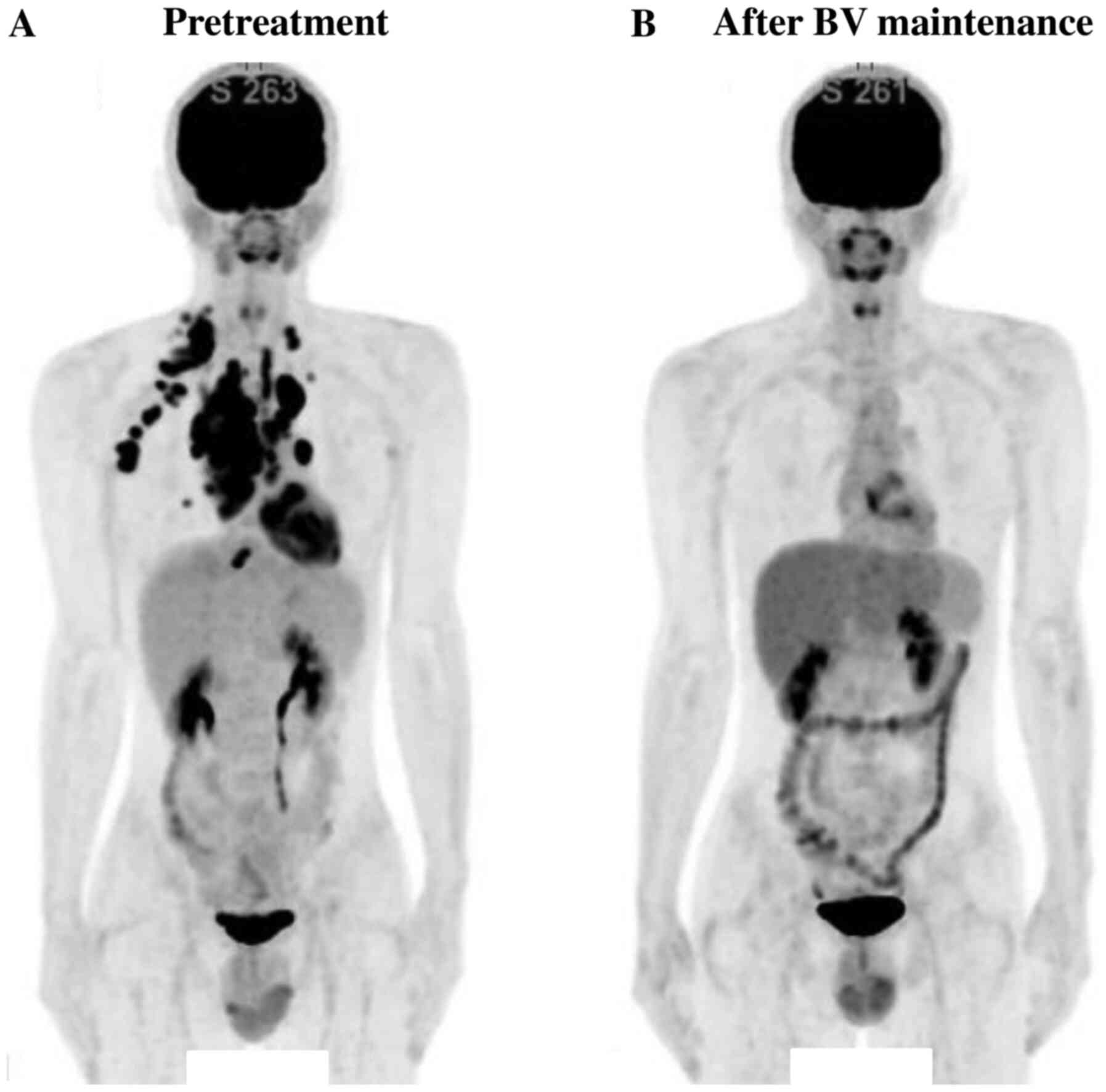
with GZL. Positron emission tomography (PET)/computed tomography
(CT) scan was performed prior to treatment. Results revealed that
the maximum standardized uptake value (SUVmax) was 11.4 (Fig. 2A). After completing eight cycles of
dose-adjusted etoposide, prednisone, vincristine, cyclophosphamide,
doxorubicin, and rituximab (DA-EPOCH-R), PET/CT scan revealed a
residual fluorodeoxyglucose (FDG)-uptake lesion, with an SUVmax of
6.8, in the mediastinum. Lymph node biopsy was performed with a
mediastinoscope to identify the pathological characteristics of the
residual mediastinal lesion. It showed the presence of CD15 and
CD30-positive RS-like cells (Fig.
1B and F) surrounded by various
inflammatory cells, but not CD20 and CD79a-positive atypical large
lymphoma cells (Fig. 1D). This
result indicated a phenotypic change from GZL to cHL. Consolidative
involved-field RT to the mediastinal lesion at a dose of 41.4 Gy
was performed. However, after 2 months, PET/CT revealed a new
FDG-uptake lesion in the lymph node in front of the liver. Then,
CT-guided lymph node biopsy was performed, and this new lesion was
found to have pathological features similar to those of CD15 and
CD30-positive cHL, but not DLBCL. The patient underwent additional
three cycles of ifosfamide, cisplatin, and etoposide (ICE) and
sequentially received high-dose chemotherapy with ranimustine,
etoposide, cytarabine, and melphalan, followed by ASCT. PET/CT scan
prior ASCT revealed the residual lymph node in the mediastinum with
FDG uptake (SUVmax=3.53, partial metabolic response), scored as 4
by Deauville 5-point scales (5-PS). However, the patient eventually
achieved complete metabolic remission (CMR) with 5-PS score of 3 on
PET/CT scan on day 90 after ASCT. Based on the clinical course
showing treatment resistance, this patient was at extremely high
risk of GZL recurrence. To decrease such a risk, the patient was
treated with BV maintenance targeting CD30 expression in lymphoma
cells. BV monotherapy maintenance (1.8 mg/kg every 3 weeks) was
initiated 3 months after ASCT. After 16 cycles of BV maintenance
therapy, the patient was still on CMR and reached 5-PS of 1 on
PET/CT scan on day 410 after BV initiation (Fig. 2B). Any adverse effects (AEs), such
as peripheral neuropathy and neutropenia, were not observed during
BV maintenance treatment.
Discussion
This report showed that BV maintenance after ASCT
might be effective in a patient with R/R GZL. GZL is pathologically
composed of cHL and primary mediastinal B-cell lymphoma (PMBL), and
its component may change between cHL and PMBL during the clinical
course (4). Our case showed the
phenotypic change from GZL to cHL after DA-EPOCH-R and RT with
sustaining CD30-positivity of lymphoma cells, therefore, BV
targeting CD30 was considered to be a promising therapeutic agent
in our case. However, GZL showed negative for CD30 in some cases
(2,4). Thus, re-biopsy of lymphoma lesion
should be performed to confirm CD30 expression in lymphoma
cells.
Previous reports showed that BV had a better
prognostic impact on both R/R cHL and CD30-positive DLBCL. That is,
the overall response rate (ORR) of R/R cHL and CD30-positive DLBCL
were 75 and 44%, respectively (6,7). In
the AETHERA trial, the PFS and 5-year PFS of patients who received
treatment with BV maintenance after ASCT for R/R cHL were 42.9
months and 59%, respectively (8,11). On
the other hand, although a small number of cases, two patients with
treatment-naïve CD30-positive GZL have been shown to benefit from
combination of BV and chemotherapy (5). In other previous reports, BV was
administered to 4 patients with R/R GZL, resulting in achieving
complete remission in 2 patients and presenting resistant for BV in
another 2 patients (9,10). Although these results showed the
efficacy of BV for R/R GZL, this has been still unknown due to the
rarity of this disease. Allogenic SCT is another salvage option for
potentially achieving cure, however, it is concerned about
transplant-related mortality and long-term toxicity. Our patient
was at high risk of recurrence due to resistance to various
chemotherapy (DA-EPOCH-R and ICE) and radiation, and the
pathological diagnosis of residual disease prior ASCT showed a
phenotypic change from GZL to cHL. Moreover, the prognosis of GZL
is reported to be poorer than that of cHL or DLBCL (3). Considering of these points, our
patient had received BV maintenance therapy after ASCT to lower the
risk of recurrence based on the AETHERA study (11), and achieved long-term remission.
To date, our patient has maintained long-term
remission after BV maintenance therapy. However, due to the history
of resistance for treatment, he is still at risk of recurrence. At
the time of recurrence after BV maintenance, the chemotherapy
sensitivity of GZL is extremely low. Therefore, checkpoint
inhibitors (CPIs) could be another therapeutic option. In patients
with R/R cHL who received nivolumab, the ORR and 6-months PFS were
66.3 and 76.9%, respectively (12).
In patients with R/R PMBL who received pembrolizumab, the ORR and
1-year PFS were 46% and ~40%, respectively (13). These data showed that CPIs might be
an alternative therapeutic option for R/R GZL and could be a
potential therapeutic option for our patient in future
recurrence.
In summary, despite achieving CMR after ASCT, BV
maintenance after ASCT was considered effective in a patient with
GZL refractory to chemotherapy and RT, and severe AEs were not
observed. Although a fraction of patients with R/R GZL is often
difficult to treat, the change in morphology and immunophenotype,
including CD30 expression, at the time of recurrence should be
confirmed. Hence, BV maintenance after ASCT could be an extremely
effective therapeutic modality for transplant-eligible patients
with CD30-positive GZL.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
TT and JY wrote and edited the manuscript, provided
patient care and reviewed the literature. NY, YMG and YM provided
patient care and acquired the clinical data. KS analyzed and
evaluated PET-CT images. MS and GI conducted pathological reviews.
All authors read and approved the final manuscript. TT and JY
confirm the authenticity of all the raw data.
Ethics approval and consent to
participate
The present case study was approved by the Ethics
Committee of the National Cancer Center Hospital East (approval no.
2018-416). The patient provided consent for inclusion in this
study.
Patient consent for publication
The patient in this case provided consent to have
this case published with removal of all identifying information to
remain anonymous and retain privacy.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Traverse-Glehen A, Pittaluga S, Gaulard P,
Sorbara L, Alonso MA, Raffeld M and Jaffe ES: Mediastinal gray zone
lymphoma: The missing link between classic Hodgkin's lymphoma and
mediastinal large B-cell lymphoma. Am J Surg Pathol. 29:1411–1421.
2005.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Pilichowska M, Pittaluga S, Ferry JA,
Hemminger J, Chang H, Kanakry JA, Sehn LH, Feldman T, Abramson JS,
Kritharis A, et al: Clinicopathologic consensus study of gray zone
lymphoma with features intermediate between DLBCL and classical HL.
Blood Adv. 1:2600–2609. 2017.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Evens AM, Kanakry JA, Sehn LH, Kritharis
A, Feldman T, Kroll A, Gascoyne RD, Abramson JS, Petrich AM, Herna
dez-Ilizaliturri FJ, et al: Gray zone lymphoma with features
intermediate between classical Hodgkin lymphoma and diffuse large
B-cell lymphoma: Characteristics, outcomes, and prognostication
among a large multicenter cohort. Am J Hematol. 90:778–783.
2015.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Kritharis A, Pilichowska M and Evens AM:
How I manage patients with grey zone lymphoma. Br J Haematol.
174:345–350. 2016.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Svoboda J, Bair SM, Landsburg DJ, Nasta
SD, Nagle SJ, Barta SK, Khan N, Filicko-O'Hara J, Gaballa S,
Strelec L, et al: Brentuximab vedotin in combination with
rituximab, cyclophosphamide, doxorubicin, and prednisone as
frontline treatment for patients with CD30-positive B-cell
lymphomas. Haematologica: May 15, 2020 (Epub ahead of print).
|
|
6
|
Younes A, Gopal AK, Smith SE, Ansell SM,
Rosenblatt JD, Savage KJ, Ramchandren R, Bartlett NL, Cheson BD, de
Vos S, et al: Results of a pivotal phase II study of brentuximab
vedotin for patients with relapsed or refractory Hodgkin's
lymphoma. J Clin Oncol. 30:2183–2189. 2012.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Jacobsen ED, Sharman JP, Oki Y, Advani RH,
Winter JN, Bello CM, Spitzer G, Palanca-Wessels MC, Kennedy DA,
Levine P, et al: Brentuximab vedotin demonstrates objective
responses in a phase 2 study of relapsed/refractory DLBCL with
variable CD30 expression. Blood. 125:1394–1402. 2015.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Moskowitz CH, Nademanee A, Masszi T, Agura
E, Holowiecki J, Abidi MH, Chen AI, Stiff P, Gianni AM, Carella A,
et al: Brentuximab vedotin as consolidation therapy after
autologous stem-cell transplantation in patients with Hodgkin's
lymphoma at risk of relapse or progression (AETHERA): A randomised,
double-blind, placebo-controlled, phase 3 trial. Lancet.
385:1853–1862. 2015.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Li J, Sim J, Leung AYH and Kwong YL:
Favorable response of relapsed/refractory gray-zone lymphoma to
brentuximab vedotin. Ann Hematol. 97:551–554. 2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Ebisawa K, Masamoto Y, Koya J, Shimura A,
Shinozaki-Ushiku A, Toyama K, Nakazaki K and Kurokawa M: Long-term
remission by brentuximab vedotin for non-mediastinal gray zone
lymphoma refractory to autologous stem cell transplantation. Clin
Lymphoma Myeloma Leuk. 19:e602–e604. 2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Moskowitz CH, Walewski J, Nademanee A,
Masszi T, Agura E, Holowiecki J, Abidi MH, Chen AI, Stiff P,
Viviani S, et al: Five-year PFS from the AETHERA trial of
brentuximab vedotin for Hodgkin lymphoma at high risk of
progression or relapse. Blood. 132:2639–2642. 2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Younes A, Santoro A, Shipp M, Zinzani PL,
Timmerman JM, Ansell S, Armand P, Fanale M, Ratanatharathorn V,
Kuruvilla J, et al: Nivolumab for classical Hodgkin's lymphoma
after failure of both autologous stem-cell transplantation and
brentuximab vedotin: A multicentre, multicohort, single-arm phase 2
trial. Lancet Oncol. 17:1283–1294. 2016.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Armand P, Rodig S, Melnichenko V,
Thieblemont C, Bouabdallah K, Tumyan G, Özcan M, Portino S,
Fogliatto L, Caballero MD, et al: Pembrolizumab in relapsed or
refractory primary mediastinal large B-cell lymphoma. J Clin Oncol.
37:3291–3299. 2019.PubMed/NCBI View Article : Google Scholar
|