Introduction
Various neoplastic and non-neoplastic conditions can
involve the mediastinal lymph nodes; hence, correct
histopathological diagnosis is very important for appropriate
treatment of patients with mediastinal lymphadenopathy.
Endobronchial ultrasound-guided transbronchial needle aspiration
(EBUS-TBNA) is a technique in which the needle is advanced through
the channel of the bronchoscope with real-time visualisation of the
target lesion by ultrasound and obtaining a sample by fine-needle
aspiration from the target lesion (1). EBUS-TBNA has been recognised as a
useful and minimally invasive technique for sampling mediastinal
lymph nodes (1,2). The high sensitivity and specificity of
EBUS-TBNA in staging for non-small cell lung carcinoma
(irrespective of the presence of metastasis in the mediastinal
lymph nodes) has been well recognised (1). Therefore, the current guidelines
recommend EBUS-TBNA as the first-line approach for lymphadenopathy
of the mediastinal lymph nodes in patients with lung cancer
(3).
It is also very important to determine the cause of
lymphadenopathy of the mediastinal lymph nodes in patients without
lung cancer, i.e., reactive/inflammatory change (including
sarcoidosis) or neoplastic change (such as malignant lymphoma). The
usefulness of EBUS-TBNA in the diagnosis of lymphadenopathy in
patients without lung cancer has also been reported (4). However, few studies have evaluated the
diagnostic results of mediastinal lymphadenopathy using EBUS-TBNA
in consecutive patients with or without lung cancer (4,5). The
aim of the present study was to analyse the results of the
cytological examination using EBUS-TBNA in the diagnosis of
mediastinal lymphadenopathy in a single centre, and also discuss
the usefulness and diagnostic problems in cytological examination
using EBUS-TBNA in patients with mediastinal lymphadenopathy.
Patients and methods
Patient selection
We enrolled 41 consecutive patients who underwent
EBUS-TBNA for the cytological and histopathological diagnosis of
mediastinal lymphadenopathy from January 2008 to December 2019 at
the Kansai Medical University Hospital.
This study was conducted in accordance with the
Declaration of Helsinki, and the study protocol was approved by the
institutional review board of the Kansai Medical University
Hospital (protocol no. 160954).
Cytological analyses
The cytological specimens obtained by EBUS-TBNA were
fixed in alcohol and subsequently routinely stained with
Papanicolaou stain; air-dried cytological specimens were also
stained with Giemsa stain according to routine hospital procedures.
No liquid-based cytology was performed in the present study.
Furthermore, rapid on-site evaluation (ROSE) of the cytological
specimens was not performed.
The cytological characteristics were independently
evaluated by one diagnostic pathologist and two cytopathologists.
Disagreements were resolved by reassessment using a multi-headed
microscope.
Histological analyses
Two diagnostic pathologists independently evaluated
the histopathological features of the biopsy specimens obtained by
EBUS-TBNA.
Results
Clinical features
This cohort included 41 patients (29 males and 12
females), who were aged 22-83 years. The reasons for performing the
EBUS-TBNA were as follows: Mediastinal lymphadenopathy of unknown
cause (16 patients), suspicion of sarcoidosis (15 patients), lung
cancer (9 patients), and lymphadenopathy due to metastatic tumour
(1 patient). There were no severe complications associated with the
EBUS-TBNA procedure in the present cohort. The information about
node stations sampled was not available for this cohort.
Cytological features
Table I summarises
the results of the cytological examinations of the samples obtained
by EBUS-TBNA in this cohort. Malignancy was seen in 16 patients
(39.0%), 1 patient (2.4%) had suspected malignancy, 22 patients
(53.6%) had no malignancy, and the sample was inadequate for
diagnosis in 2 patients (4.9%). Patients with malignancy included
small cell carcinoma (4 patients), adenocarcinoma (3 patients),
squamous cell carcinoma (2 patients), and non-small cell carcinoma
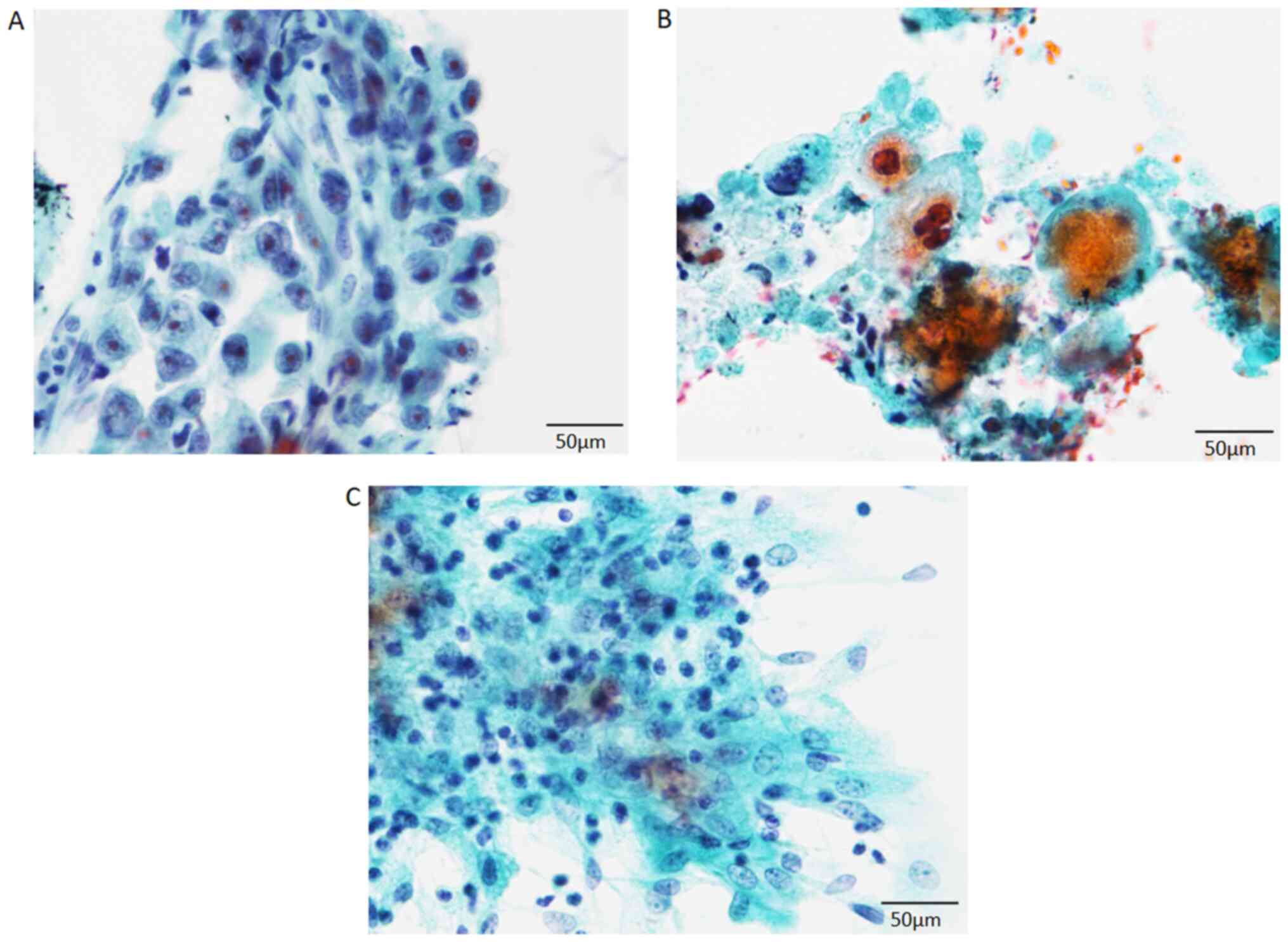
(7 patients) (Fig. 1). In 3
patients who had no malignancy, only a few epithelioid granulomas
were observed; thus, sarcoidosis was suspected.
 | Table ISummary of the results of the
cytological examination of the mediastinal lymph nodes in 41
patients. |
Table I
Summary of the results of the
cytological examination of the mediastinal lymph nodes in 41
patients.
| Results | Patients, n (%) |
|---|
|
Positive/malignancy | 16 (39.0) |
|
Small cell
carcinoma | 4 (9.8) |
|
Adenocarcinoma | 3 (7.3) |
|
Squamous
cell carcinoma | 2 (4.9) |
|
Non-small
cell carcinoma | 7 (17.1) |
| Suspicious of
malignancy | 1 (2.4) |
| Negative | 22 (53.6) |
| Insufficient | 2 (4.9) |
Histological features and correlation
with cytological diagnosis
Table II summarises
the results of the histological examination. Carcinoma was
diagnosed in 17 patients (adenocarcinoma in 6 patients, small cell
carcinoma in 4 patients, squamous cell carcinoma in 3 patients, and
non-small cell carcinoma in 4 patients). One patient who had
adenocarcinoma was considered cytologically negative because the
carcinoma was not visible in the cytological specimens. Thus, 16 of
17 (94.1%) patients with carcinoma were diagnosed as having
carcinoma (positive/malignancy) by cytological examination.
Moreover, one patient with suspected malignancy on cytological
examination did not have carcinoma on histological examination. The
sensitivity, specificity, and positive predictive value of the
cytological examination of carcinoma (malignancy) were 94, 100 and
100%, respectively.
 | Table IISummary of the results of the
histological examination of the mediastinal lymph nodes in 41
patients. |
Table II
Summary of the results of the
histological examination of the mediastinal lymph nodes in 41
patients.
| Results | Patients (%) |
|---|
| Carcinomas | 17 (41.5) |
|
Small cell
carcinoma | 4 (9.8) |
|
Adenocarcinoma | 6 (14.6) |
|
Squamous
cell carcinoma | 3 (7.3) |
|
Non-small
cell carcinoma | 4 (9.8) |
| Benign
conditions | 24 (58.5) |
|
Sarcoidosis | 11 (26.8) |
|
Cystic
lesion | 2 (4.9) |
|
Inflammatory
conditions | 1 (2.4) |
|
Schwannoma | 1 (2.4) |
|
Not
specified | 9 (22.0) |
The histological diagnosis of the remaining 24
patients revealed benign conditions, which included sarcoidosis (11
patients), benign cystic lesion (2 patients), non-specific
inflammatory condition (1 patient), schwannoma (1 patient), and
unspecified condition (9 patients). Only 3 of 11 patients with
sarcoidosis were diagnosed by cytological examination (27.3%).
Discussion
The present study analysed the usefulness and
problems associated with EBUS-TBNA-based cytological examination of
the mediastinal lymph nodes in our institute. In this cohort, the
sensitivity, specificity, and positive predictive value of the
cytological examination for carcinoma (malignancy) were 94.1, 100
and 100%, respectively. However, the diagnostic accuracy for
sarcoidosis was low; only 3 of 11 (27.3%) patients with sarcoidosis
were cytologically diagnosed as sarcoidosis.
The usefulness of EBUS-TBNA is well known,
particularly its high sensitivity and specificity in detecting
metastasis in the mediastinal lymph nodes in patients with lung
cancer (1). Most of the previously
published studies demonstrated that the sensitivity was more than
80% and the specificity was almost 100% (1). Therefore, EBUS-TBNA has been
considered as a superior performance tool compared to other staging
modalities, such as computed tomography (1). In one series, the sensitivity of
diagnosis of mediastinal lymph node metastases from lung cancer was
~70%, and the positive predictive value was ~95%. Moreover, the
superiority of liquid-based cytology compared to that of
conventional cytological examination has been reported (4). In the present study, sensitivity,
specificity, and positive predictive value were ~100%. Thus,
EBUS-TBNA is an accurate and useful method for detecting metastatic
carcinoma in the mediastinal lymph node in patients with lung
cancer.
However, the cytological diagnosis of the
mediastinal lymph nodes using EBUS-TBNA might be challenging
because the mediastinal lymph nodes can have diverse non-neoplastic
conditions, including sarcoidosis. Sarcoidosis is a systemic
autoimmune disease characterised by the presence of granulomatous
inflammation, which mainly affects the lungs, lymph nodes, eyes,
and skin; hilar and mediastinal lymph nodes are also frequently
involved (6). The utility of
EBUS-TBNA in the diagnosis of sarcoidosis (detection of granulomas)
has also been reported (7,8). According to a study of cytological
specimens using EBUS-TBNA, well-formed non-necrotising granulomas
were noted in 90% of the patients with sarcoidosis (38/42
patients), and the remaining 4 patients had poorly formed
granulomas. The extent of granulomas was as follows: Rare,
occasional, and numerous in 26, 36 and 38% of the patients,
respectively (9). High sensitivity
(>85%) of EBUS-TBNA in patients with a high clinical suspicion
of sarcoidosis has also been reported (10). However, the rate of detection of
sarcoidosis (epithelioid granulomas) was low (27.3%) in the present
cohort. This might be due to the amount of the sample because the
retrospective analysis of the cytological specimens failed to
detect epithelioid granulomas in these cases with epithelioid
granulomas. Improvement in the sampling technique and/or method
might be required for these patients. The presence of the
cytologist at the time of obtaining the cytological specimens and
performance of ROSE improved the detection of the targeted lesions
in various organs, according to previous studies (11,12).
It has been reported that yields of the conventional TBNA with ROSE
and EBUS-TBNA with or without ROSE were higher than those of the
conventional TBNA without ROSE, although the rates of granuloma
detection were not significantly different (7). Moreover, the utility of granuloma
detection using ROSE was also reported (9). Therefore, ROSE might improve the
detection rate of granulomas in EBUS-TBNA.
In conclusion, the present study analysed the
usefulness and problems associated with EBUS-TBNA in the
cytological examination of the mediastinal lymph nodes in our
institute. The sensitivity, specificity, and positive predictive
value of the cytological examination for carcinoma (malignancy)
were high. Thus, EBUS-TBNA is a useful method for detecting
mediastinal lymph node metastasis in patients with lung cancer.
However, the diagnostic accuracy of sarcoidosis was low; therefore,
an improvement in the sampling technique might be required.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
MI contributed to conception and design of the
study. KS, MI, KO and HI contributed to the analyses of the
cytological specimens. MI and KT contributed to the analyses of the
histological specimens. KS and MI confirm the authenticity of all
the raw data, and contributed to drafting of the manuscript, tables
and figures. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The study was conducted in accordance with the
Declaration of Helsinki, and the study protocol was approved by the
institutional review board of the Kansai Medical University
Hospital (Hirakata, Japan; protocol no. 160954). Opt-out consent
was obtained from participants of this study due to the
retrospective design of the study and no risk to the
participants.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
VanderLaan PA, Wang HH, Majid A and Folch
E: Endobronchial ultrasound-guided transbronchial needle aspiration
(EBUS-TBNA): An overview and update for the cytopathologist. Cancer
Cytopathol. 122:561–576. 2014.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Michael CW, Faquin W, Jing X, Kaszuba F,
Kazakov J, Moon E, Toloza E, Wu RI and Moreira AL: Committee II:
Guidelines for cytologic sampling techniques of lung and
mediastinal lymph nodes. Diagn Cytopathol. 46:815–825.
2018.PubMed/NCBI View
Article : Google Scholar
|
|
3
|
Vilmann P, Clementsen PF, Colella S,
Siemsen M, De Leyn P, Dumonceau JM, Herth FJ, Larghi A,
Vazquez-Sequeiros E, Hassan C, et al: Combined endobronchial and
esophageal endosonography for the diagnosis and staging of lung
cancer: European society of gastrointestinal endoscopy (ESGE)
guideline, in cooperation with the European respiratory society
(ERS) and the European society of thoracic surgeons (ESTS).
Endoscopy. 47:545–559. 2015.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Xu C, Qin L, Lei W, Jiang J, Ni C and
Huang J: The role of endobronchial ultrasound-guided transbronchial
needle aspiration liquid-based cytology in the diagnosis of
mediastinal lymphadenopathy. Diagn Cytopathol. 48:316–321.
2020.PubMed/NCBI View
Article : Google Scholar
|
|
5
|
Gupta N, Klein M, Chau K, Vadalia B,
Khutti S, Gimenez C and Das K: Adequate at rapid on-site evaluation
(ROSE), but inadequate on final cytologic diagnosis: Analysis of
606 cases of endobronchial ultrasound-guided trans bronchial needle
aspirations (EBUS-TBNA). Diagn Cytopathol. 47:367–373.
2019.PubMed/NCBI View
Article : Google Scholar
|
|
6
|
James WE, Koutroumpakis E, Saha B, Nathani
A, Saavedra L, Yucel RM and Judson MA: Clinical features of
extrapulmonary sarcoidosis without lung involvement. Chest.
154:349–356. 2018.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Madan K, Dhungana A, Mohan A, Hadda V,
Jain D, Arava S, Pandey RM, Khilnani GC and Guleria R: Conventional
transbronchial needle aspiration versus endobronchial
ultrasound-guided transbronchial needle aspiration, with or without
rapid on-site evaluation, for the diagnosis of sarcoidosis: A
randomized controlled trial. J Bronchology Interv Pulmonol.
24:48–58. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Smojver-Jezek S, Peros-Golubicić T,
Tekavec-Trkanjec J, Mazuranić I and Alilović M: Transbronchial fine
needle aspiration cytology in the diagnosis of mediastinal/hilar
sarcoidosis. Cytopathology. 18:3–7. 2007.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Odronic SI, Maskovyak AE, Springer BS,
Dyhdalo KS, Abdul-Karim FW and Booth CN: Utility and morphologic
features of granulomas on rapid on-site evaluation of endobronchial
ultrasonography-guided fine-needle aspiration. J Am Soc Cytopathol.
3:79–85. 2014.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Gupta D, Dadhwal DS, Agarwal R, Gupta N,
Bal A and Aggarwal AN: Endobronchial ultrasound-guided
transbronchial needle aspiration vs. conventional transbronchial
needle aspiration in the diagnosis of sarcoidosis. Chest.
146:547–556. 2014.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Sandoh K, Ishida M, Okano K, Miyasaka C,
Mori S, Tokuhara M, Suzuki R, Okazaki T, Nakamura N and Tsuta K:
Utility of endoscopic ultrasound-guided fine-needle aspiration
cytology in rapid on-site evaluation for the diagnosis of gastric
submucosal tumors: Retrospective analysis of a single-center
experience. Diagn Cytopathol. 47:869–875. 2019.PubMed/NCBI View
Article : Google Scholar
|
|
12
|
Shield PW, Cosier J, Ellerby G, Gartrell M
and Papadimos D: Rapid on-site evaluation of fine needle aspiration
specimens by cytology scientists: A review of 3032 specimens.
Cytopathology. 25:322–329. 2014.PubMed/NCBI View Article : Google Scholar
|