Introduction
Recently developed immune checkpoint-blockade
therapies have been demonstrated to have remarkable benefits for
the treatment of patients with recurrent/metastatic head and neck
squamous cell carcinoma (R/M HNSCC) (1,2). Many
studies have focused on achieving a deeper understanding of the
interaction between tumor cells and associated immune cells within
the tumor microenvironment, to not only predict but also improve
immunotherapeutic responsiveness (3,4).
Similarly, in the bloodstream complex interactions between tumor
cells and immune cells play an important role in the formation of
distant metastases and in clinical outcomes (5-7).
Most tumor cells that enter the bloodstream through
intravasation from primary sites die by anoikis induced by
detachment from the extracellular matrix, the shearing force of
blood pressure, or immune surveillance. However, some are able to
survive in the bloodstream through phenotypic and functional
alterations that confer resistance to environmental stress and are
called circulating tumor cells (CTCs). Among the three forms of
cell death mentioned, immune surveillance is the most complex and
fluctuates depending on the patient's disease progression,
nutritional status, and treatment pressure. In contrast, protumoral
skewing of the immune system supports evasion of immune
surveillance and promotes tumor cell dissemination. To date, the
role of systemic immunity in cancer patients has been exclusively
investigated and reported with regard to its clinical significance
(8,9); however, the relationship between
systemic immunity and CTCs remains unclear. Interestingly, in
patients with breast cancer, the presence of CTCs has been
correlated with a reduction in CD3+, CD4+,
and CD8+ T cells (10).
Another study in lung-cancer patients showed that numbers of CTCs
were negatively correlated with those of CD3+,
CD4+, and CD4+/CD8+ T cells
(11). However, further studies are
needed to more precisely evaluate the impact of systemic immunity
on CTCs in the bloodstream.
To address this issue, we first investigated whether
the proportions of circulating immune cells were correlated with
clinical features. We then analyzed the potential correlations with
the molecular characteristics of CTCs.
Materials and methods
Patients
This study enrolled 44 patients with untreated HNSCC
from a previous study (12). Their
median age was 66 years (range: 47-86). The tumor origins included
the oral cavity (n=4), nasopharynx (n=2), oropharynx (n=17),
hypopharynx (n=14), larynx (n=4), and nasal cavity (n=3). We
evaluated several clinical variables, including age, T factor, N
factor, stage, locoregional recurrence, distant metastasis, initial
treatment response, and presence of CTCs. This study was approved
by the Ethical Committee of Gunma University Hospital (no. 12-12),
and written informed consent was obtained from each patient.
Data acquisition and systemic
immune-related markers
Laboratory data, including neutrophil, lymphocyte,
monocyte, and platelet counts, as well as serum C-reactive protein
(CRP) and albumin levels, were collected from patients' clinical
records within 2 weeks of blood collection for CTC isolation. The
neutrophil-lymphocyte ratio (NLR), platelet-lymphocyte ratio (PLR),
and lymphocyte-monocyte ratio (LMR) were calculated by dividing the
absolute values of the corresponding hematological parameters. The
systemic immune-inflammation index (SII), prognostic nutrition
index (PNI), and CRP/albumin ratio (CAR) were calculated as: SII =
(platelet count x neutrophil count)/lymphocyte count (13), PNI = (10 x serum albumin) + (0.005 x
lymphocyte count) (14), and CAR =
CRP/albumin (15).
CTC detection and gene expression
CTC detection and molecular data from a previous
study were used (12). Blood
samples were collected from 44 patients with untreated HNSCC; CTCs
were isolated using a CellSieve™ microfilter (Creatv
MicroTech, Inc.). In brief, peripheral blood samples (7.5 ml) were
passed through a CellSieve™ microfilter. The filter was
then washed with phosphate-buffered saline three times and
transferred into a new tube, labeled as CTCs. The first filtrate
was passed through a second filter to capture control leukocytes.
The second filter was washed, transferred into another tube, and
used as a control.
Total RNA from the CTCs was extracted using an
RNeasy Micro Kit (Qiagen, Inc.) according to the manufacturer's
instructions. Complementary DNA synthesis was performed using the
QuantiTect Reverse Transcription kit (Qiagen, Inc.) with 14 cycles
of preamplification using the TaqMan™ PreAmp Master Mix Kit
(Applied Biosystems). The products were analyzed using the
real-time quantitative polymerase chain reaction (Applied
Biosystems). Primers for the 14 target genes epithelial cell
adhesion molecule [EPCAM: Hs00158980_m1], MET:
Hs01565576_m1, keratin 19 [KRT19: Hs00761767_s1], epidermal
growth factor receptor [EGFR: Hs01076090_m1],
phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit
alpha [PIK3CA: Hs00907957_m1], cyclin D1 [CCND1:
Hs00765553_m1], snail family transcriptional repressor 1
[SNAI1: Hs00195591_m1], vimentin [VIM:
Hs00958111_m1], CD44: Hs01075861_m1, nanog homeobox
[NANOG: Hs04399610_g1], aldehyde dehydrogenase 1 family
member A1 [ALDH1A1: Hs00946916_m1], CD47:
Hs00179953_m1, CD274: Hs01125301_m1, and programmed cell
death 1 ligand 2 [PDCD1LG2: Hs01057777_m1] and ACTB
(Hs01060665_g1, normalization control) were purchased from Applied
Biosystems (TaqMan™ Gene Expression Assays). CTC gene expression
levels were determined using a relative quantification method.
Detection of at least one of the four epithelial-related genes
(EPCAM, MET, KRT19, and EGFR) was defined as CTC
positivity. The cycle threshold (Ct) values of the target genes
were normalized to those of the reference gene ACTB.
Expression levels were estimated as fold changes and compared to
those in the control leukocyte group using the 2-∆∆Ct
relative quantification method (16). When the 2-∆∆Ct value was
>1, the sample was assessed as positive for the expression of
the gene.
Statistical analysis
GraphPad Prism version 8.0 for Windows (GraphPad
Software, Inc.) was used for all analyses. Mann-Whitney U tests
were used to assess differences in continuous variables.
Kaplan-Meier curves were plotted and compared using log-rank tests
to compare survival curves between subgroups. The optimal cutoff
values of circulating immune cells as well as their related markers
for progression-free survival (PFS) and overall survival (OS) were
determined based on receiver operating characteristic curve
analysis. Two-sided P-values <0.05 were considered to be
statistically significant.
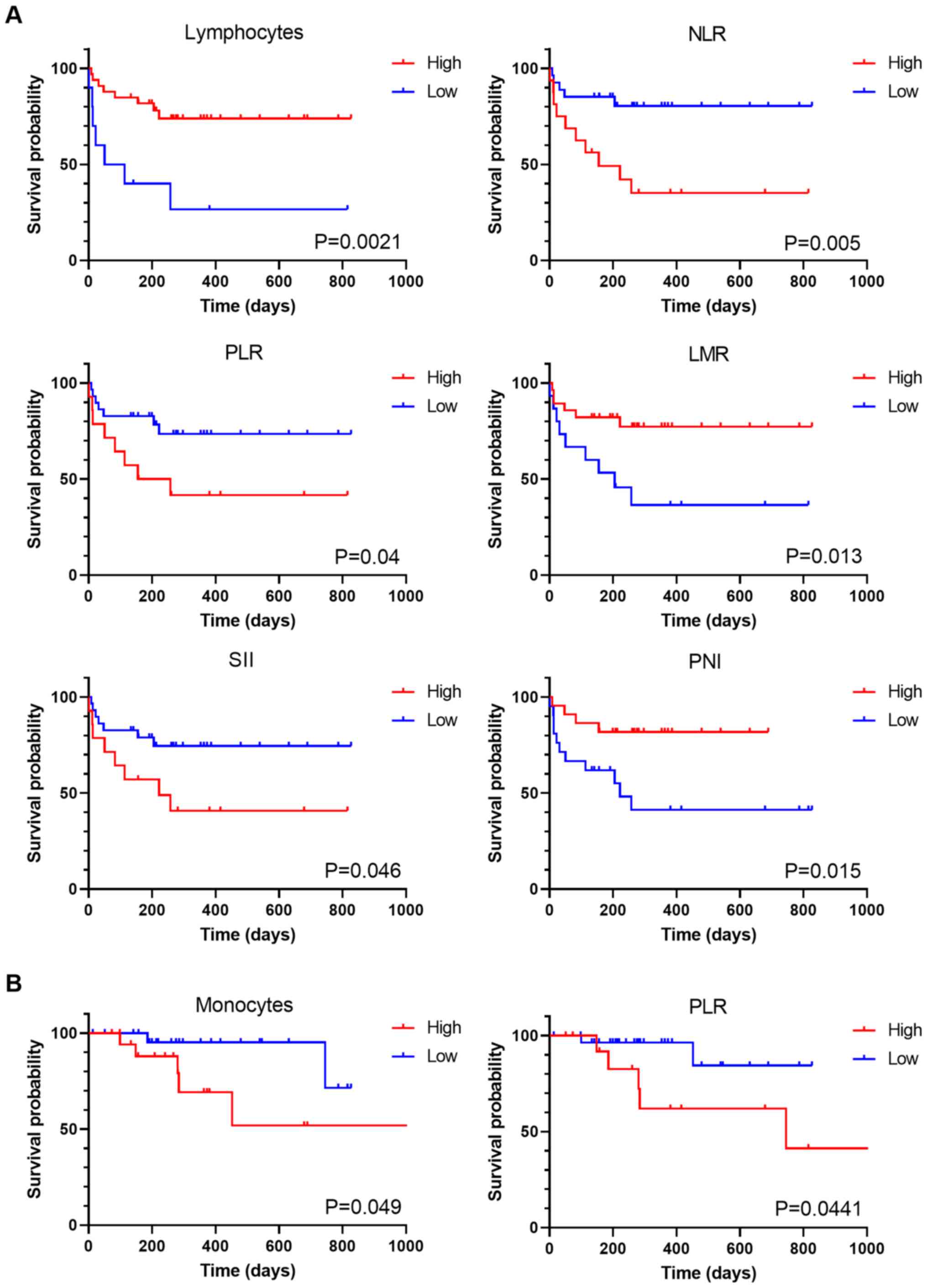
Results
Clinical significance of systemic
immune-related markers
A total of 44 treatment-naïve patients with HNSCC
were enrolled in this study. Their characteristics are listed in
Table I. Twenty-eight (63.6%) of
the 44 were positive for CTCs as described previously (12). First, we determined whether systemic
immune-related markers were associated with clinical factors and
the presence of CTCs. Monocyte counts in elderly patients were
significantly higher than those in younger patients (P=0.0339).
Patients with advanced-stage disease exhibited significantly higher
monocyte counts and LMR values than those with early-stage disease.
Interestingly, patients with distant metastases during the
follow-up period had significantly lower lymphocyte counts, NLR,
and LMR. Meanwhile, there was no significant correlation between
the presence of CTCs and any systemic immune-related markers. Next,
we analyzed the prognostic significance of systemic immune-related
markers in these 44 patients (Table
II). As expected, various systemic immune-related markers,
including lymphocyte counts, NLR, PLR, LMR, SII, and PNI, were
associated with PFS (lymphocyte counts, P=0.0021; NLR, P=0.005;
PLR, P=0.04; LMR, P=0.013; SII, P=0.046; and PNI, P=0.015).
Monocyte counts and PLR were significantly associated with OS
(monocyte counts, P=0.049; PLR, P=0.0441). The corresponding
Kaplan-Meier survival curves are shown in Fig. 1.
 | Table IClinicopathological characteristics
of patients with head and neck squamous cell carcinoma (n=44). |
Table I
Clinicopathological characteristics
of patients with head and neck squamous cell carcinoma (n=44).
| Clinical
variable | N (%) | Neutrophils,
x109/l | P-value | Lymphocytes,
x109/l | P-value | Monocytes,
x109/l | P-value | CRP, mg/dl | P-value | NLR | P-value | PLR | P-value | LMR | P-value | SII | P-value | PNI | P-value | CAR | P-value |
|---|
| Age, years | | | | | | | | | | | | | | | | | | | | | |
|
<66 | 21 (47.7) | 4.190
(3.760-5.685) | 0.2855 | 1.700
(1.355-2.030) | 0.7054 | 0.320
(0.250-0.390) | 0.0339a | 0.18
(0.065-0.730) | 0.4878 | 2.661
(1.888-3.947) | 0.4419 | 138.8
(103.5-173.2) | 0.9629 | 5.813
(3.710-6.842) | 0.0605 | 586.1
(453.5-1090.0) | 0.6086 | 52.20
(48.93-55.43) | 0.0639 | 0.0311
(0.0143-0.1156) | 0.2736 |
|
≥66 | 23 (52.3) | 4.910
(4.220-7.090) | | 1.610
(0.940-2.330) | | 0.410
(0.290-0.560) | | 0.23
(0.080-0.480) | | 3.273
(1.923-5.517) | | 143.5
(102.8-166.7) | | 3.927
(2.789-5.935) | | 736.5
(443.6-1090.0) | | 48.65
(45.80-51.50) | | 0.0548
(0.0205-0.1346) | |
| T status | | | | | | | | | | | | | | | | | | | | | |
|
T1-2 | 13 (29.5) | 4.150
(3.570-5.645) | 0.1317 | 1.670
(0.980-2.390) | 0.7460 | 0.280
(0.230-0.520) | 0.1421 | 0.08
(0.040-0.580) | 0.1039 | 2.742
(1.764-4.625) | 0.7032 | 122.2
(99.6-213.3) | 0.8589 | 5.015
(2.947-6.921) | 0.6633 | 523.1
(465.6-1168.0) | 0.6474 | 53.15
(43.40-55.43) | 0.4484 | 0.0205
(0.0091-0.1784) | 0.1860 |
|
T3-4 | 31 (70.5) | 5.370
(3.960-7.090) | | 1.700
(1.430-2.300) | | 0.370
(0.300-0.500) | | 0.23
(0.100-0.560) | | 2.974
(1.947-5.517) | | 143.5
(103.2-160.9) | | 5.152
(3.115-6.122) | | 745.6
(442.4-1165.0) | | 49.35
(46.65-52.20) | | 0.0536
(0.0214-0.1204) | |
| N status | | | | | | | | | | | | | | | | | | | | | |
|
N0 | 10 (22.7) | 4.655
(4.053-7.963) | 0.8402 | 1.740
(1.308-2.255) | 0.9503 | 0.405
(0.338-0.568) | 0.0335a | 0.12
(0.068-0.705) | 0.4937 | 2.473
(1.686-5.020) | 0.7097 | 142.8
(111.3-170.6) | 0.8148 | 4.354
(1.948-5.457) | 0.2061 | 527.5
(436.9-1358.0) | 0.8571 | 48.93
(46.46-52.29) | 0.6062 | 0.0262
(0.0165-0.1923) | 0.6164 |
|
N1-3 | 34 (77.3) | 4.850
(3.815-6.540) | | 1.645
(1.105-2.308) | | 0.315
(0.260-0.448) | | 0.25
(0.080-0.500) | | 2.972
(1.941-5.193) | | 139.5
(101.7-171.8) | | 5.227
(3.255-6.496) | | 711.9
(443.3-1173.0) | | 50.25
(46.18-55.31) | | 0.0548
(0.0187-0.1209) | |
| Stage | | | | | | | | | | | | | | | | | | | | | |
|
I-II | 10 (22.7) | 4.345
(3.428-5.440) | 0.1135 | 1.750
(1.435-2.158) | 0.6537 | 0.275
(0.220-0.345) | 0.0202a | 0.23
(0.063-0.870) | 0.9945 | 2.551
(1.675-3.357) | 0.1682 | 128.3
(99.0-183.3) | 0.8148 | 6.435
(4.615-8.466) | 0.0389a | 505.7
(466.2-804.7) | 0.3538 | 52.80
(49.91-55.39) | 0.1226 | 0.0494
(0.0144-0.2158) | >0.9999 |
|
III-IV | 34 (77.3) | 5.140
(3.940-7.230) | | 1.615
(1.043-2.340) | | 0.375
(0.298-0.528) | | 0.22
(0.078-0.500) | | 3.124
(2.047-5.563) | | 145.2
(102.0-167.6) | | 4.467
(2.933-6.032) | | 757.8
(421.7-1205.0) | | 49.28
(45.56-52.29) | | 0.050
(0.0184-0.1209) | |
| Locoregional
recurrence | | | | | | | | | | | | | | | | | | | | | |
|
(+) | 13 (29.5) | 4.300
(3.850-6.515) | 0.8149 | 1.560
(0.950-2.205) | 0.3900 | 0.390
(0.275-0.510) | 0.6889 | 0.22
(0.070-0.565) | 0.8838 | 3.729
(1.818-5.758) | 0.5760 | 111.7
(88.3-187.1) | 0.4300 | 3.600
(2.828-6.181) | 0.3300 | 470.6
(322.7-1238.0) | 0.5417 | 47.75
(44.95-52.38) | 0.1816 | 0.050
(0.0184-0.1359) | 0.9434 |
|
(-) | 31 (70.5) | 4.910
(3.840-7.090) | | 1.700
(1.270-2.300) | | 0.330
(0.270-0.470) | | 0.22
(0.080-0.480) | | 2.724
(1.947-3.969) | | 146.9
(115.6-170.4) | | 5.152
(3.560-6.684) | | 687.4
(473.8-1141.0) | | 51.20
(47.50-53.35) | | 0.0495
(0.0178-0.1241) | |
| Distant
metastasis | | | | | | | | | | | | | | | | | | | | | |
|
(+) | 13 (29.5) | 5.370
(4.000-7.040) | 0.5213 | 1.060
(0.865-1.850) | 0.0289a | 0.380
(0.295-0.510) | 0.7847 | 0.23
(0.100-0.475) | 0.7076 | 4.349
(3.087-6.035) | 0.0239a | 160.9
(111.2-237.9) | 0.1921 | 3.115
(2.325-5.874) | 0.0491a | 1141.0
(443.0-1252.0) | 0.2104 | 48.65
(43.70-51.70) | 0.1162 | 0.0548
(0.0222-0.1291) | 0.5085 |
|
(-) | 31 (70.5) | 4.780
(3.660-6.390) | | 1.780
(1.490-2.330) | | 0.330
(0.270-0.470) | | 0.20
(0.070-0.650) | | 2.494
(1.829-3.608) | | 135.6
(98.5-151.3) | | 5.227
(3.808-6.684) | | 531.2
(464.5-982.0) | | 51.40
(47.50-53.35) | | 0.0433
(0.0175-0.1328) | |
| Initial
treatment | | | | | | | | | | | | | | | | | | | | | |
|
CR | 33 (75.0) | 4.910
(3.860-7.115) | 0.4343 | 1.780
(1.350-2.235) | 0.2083 | 0.330
(0.275-0.510) | 0.9202 | 0.27
(0.080-0.755) | 0.2852 | 2.724
(2.014-4.527) | 0.7284 | 143.5
(106.8-165.6) | 0.8100 | 5.152
(3.521-6.435) | 0.3593 | 687.4
(472.2-1153.0) | 0.4535 | 51.00
(47.63-53.25) | 0.2569 | 0.0555
(0.0182-0.1624) | 0.3983 |
|
PR/SD/PD | 11 (25.0) | 4.190
(3.740-6.040) | | 1.440
(0.930-2.460) | | 0.390
(0.250-0.500) | | 0.13
(0.070-0.350) | | 3.729
(1.713-5.698) | | 118.6
(78.1-207.5) | | 3.600
(2.789-6.240) | | 443.6
(309.6-1279.0) | | 47.00
(44.10-52.55) | | 0.0302
(0.0184-0.0972) | |
| CTC | | | | | | | | | | | | | | | | | | | | | |
|
Positive | 28 (63.6) | 5.390
(3.715-7.128) | 0.6949 | 1.740
(1.198-2.493) | 0.6508 | 0.330
(0.288-0.550) | 0.5661 | 0.28
(0.080-0.890) | 0.2177 | 2.579
(1.761-5.237) | 0.7084 | 147.5
(99.3-222.8) | 0.5065 | 5.129
(3.435-5.984) | 0.7673 | 636.8
(478.3-1448.0) | 0.6037 | 51.30
(45.40-55.14) | 0.5997 | 0.0587
(0.0180-0.2205) | 0.4231 |
|
Negative | 16 (36.4) | 4.655
(3.870-6.168) | | 1.645
(1.055-2.268) | | 0.365
(0.253-0.463) | | 0.16
(0.070-0.365) | | 3.108
(1.962-4.900) | | 128.9
(105.1-164.6) | | 4.885
(3.029-6.590) | | 634.7
(442.7-1165.0) | | 49.33
(46.39-52.53) | | 0.0394
(0.0184-0.1164) | |
 | Table IIPrognostic value of systemic
immune-related markers in patients with head and neck squamous cell
carcinoma (n=44). |
Table II
Prognostic value of systemic
immune-related markers in patients with head and neck squamous cell
carcinoma (n=44).
| A, Progression-free
survival |
|---|
| Variables | N | P-value | HR | 95% CI |
|---|
| Neutrophils,
x109/l | | | | |
|
<3.670 | 8 | 0.1919 | 3.5330 | 1.0010-12.4800 |
|
≥3.670 | 36 | | | |
| Lymphocytes,
x109/l | | | | |
|
<1.090 | 10 | 0.0021a | 0.2339 | 0.0608-0.9001 |
|
≥1.090 | 34 | | | |
| Monocytes,
x109/l | | | | |
|
<0.375 | 25 | 0.2740 | 1.7460 | 0.6204-4.9160 |
|
≥0.375 | 19 | | | |
| CRP, mg/dl | | | | |
|
<0.065 | 36 | 0.1440 | 0.2489 | 0.0738-0.8397 |
|
≥0.065 | 8 | | | |
| NLR | | | | |
|
<3.710 | 28 | 0.0050a | 4.1040 | 1.3960-12.0600 |
|
≥3.710 | 16 | | | |
| PLR | | | | |
|
<157.1 | 30 | 0.0400a | 2.7610 | 0.9080-8.3980 |
|
≥157.1 | 14 | | | |
| LMR | | | | |
|
<3.704 | 15 | 0.0130a | 0.2951 | 0.0985-0.8842 |
|
≥3.704 | 29 | | | |
| SII | | | | |
|
<1,027 | 30 | 0.0460a | 2.6870 | 0.8890-8.1210 |
|
≥1,027 | 14 | | | |
| PNI | | | | |
|
<49.43 | 21 | 0.0150a | 0.2697 | 0.0969-0.7504 |
|
≥49.43 | 23 | | | |
| CAR | | | | |
|
<0.01745 | 9 | 0.1010 | 4.6300 | 1.4350-14.9300 |
|
≥0.01745 | 35 | | | |
| B, Overall
survival |
| Variables | N | P-value | HR | 95% CI |
| Neutrophils,
x109/l | | | | |
|
<4.000 | 13 | 0.1053 | Undefined | Undefined |
|
≥4.000 | 31 | | | |
| Lymphocytes,
x109/l | | | | |
|
<1.465 | 15 | 0.2465 | 0.4250 | 0.0910-1.9860 |
|
≥1.465 | 29 | | | |
| Monocytes,
x109/l | | | | |
|
<0.375 | 25 | 0.0490a | 4.4270 | 0.9467-20.7000 |
|
≥0.375 | 19 | | | |
| CRP, mg/dl | | | | |
|
<0.065 | 36 | 0.1320 | Undefined | Undefined |
|
≥0.065 | 8 | | | |
| NLR | | | | |
|
<3.710 | 28 | 0.1090 | 3.4560 | 0.7702-15.5000 |
|
≥3.710 | 16 | | | |
| PLR | | | | |
|
<157.1 | 30 | 0.0441a | 4.4910 | 0.9573-21.0700 |
|
≥157.1 | 14 | | | |
| LMR | | | | |
|
<6.496 | 35 | 0.2147 | Undefined | Undefined |
|
≥6.496 | 9 | | | |
| SII | | | | |
|
<836 | 27 | 0.0975 | 3.5890 | 0.7962-16.1800 |
|
≥836 | 17 | | | |
| PNI | | | | |
|
<43.63 | 5 | 0.6657 | 0.7170 | 0.1209-4.2520 |
|
≥43.63 | 39 | | | |
| CAR | | | | |
|
<0.01745 | 9 | 0.1060 | Undefined | Undefined |
|
≥0.01745 | 35 | | | |
Association between systemic
immune-related markers and the molecular characteristics of
CTCs
Finally, we analyzed whether systemic immune-related
markers were associated with specific molecular characteristics of
CTCs. Gene expression tests revealed that the expression levels of
five genes, PIK3CA, CD44, NANOG, CD47,
and PDCD1LG2, were significantly correlated with systemic
immune-related markers (Table
III). In particular, PIK3CA expression in CTCs was
significantly correlated with higher lymphocyte counts (P=0.035)
and PNI (P=0.0157). Patients with CTCs expressing CD47
showed significantly higher neutrophil (P=0.0031) and monocyte
counts (P=0.0016). Furthermore, those with CTCs expressing
PDCD1LG2 showed significantly lower CRP (P=0.0271) and CAR
(P=0.0207) levels.
 | Table IIIAssociation between systemic
immune-related markers and molecular characteristics of CTCs in
patients (n=28). |
Table III
Association between systemic
immune-related markers and molecular characteristics of CTCs in
patients (n=28).
| Gene symbol | N (%) | Neutrophils,
x109/l | P-value | Lymphocytes,
x109/l | P-value | Monocytes,
x109/l | P-value | CRP, mg/dl | P-value | NLR | P-value | PLR | P-value | LMR | P-value | SII | P-value | PNI | P-value | CAR | P-value |
|---|
| PIK3CA | | | | | | | | | | | | | | | | | | | | | |
|
Positive | 14 (50.0) | 4.415
(3.800-5.723) | 0.8036 | 1.900
(1.478-2.535) | 0.0350a | 0.380
(0.258-0.410) | 0.8299 | 0.100
(0.070-0.320) | 0.1270 | 2.261
(1.711-3.789) | 0.0556 | 121.6
(96.9-152.5) | 0.2273 | 5.675
(3.817-7.343) | 0.0690 | 506.0
(329.2-886.7) | 0.1936 | 51.85
(49.20-55.35) | 0.0157a | 0.0222
(0.0172-0.0717) | 0.0869 |
|
Negative | 14 (50.0) | 4.785
(3.905-7.200) | | 1.445
(0.868-1.883) | | 0.310
(0.243-0.563) | | 0.265
(0.093-0.705) | | 3.887
(2.609-5.926) | | 150.0
(107.7-211.9) | | 3.299
(1.986-6.310) | | 1020.0
(463.9-1205.0) | | 47.38
(44.66-49.76) | | 0.0760
(0.0213-0.1819) | |
| CCND1 | | | | | | | | | | | | | | | | | | | | | |
|
Positive | 14 (50.0) | 4.655
(4.133-5.433) | 0.9820 | 1.875
(1.328-2.535) | 0.1139 | 0.395
(0.283-0.460) | 0.3228 | 0.310
(0.095-0.500) | 0.2306 | 2.556
(1.711-4.248) | 0.2273 | 132.9
(93.4-170.0) | 0.8743 | 4.577
(3.390-7.343) | 0.6027 | 672.7
(353.4-1012.0) | 0.4824 | 50.55
(46.84-53.24) | 0.5189 | 0.0738
(0.0218-0.1254) | 0.2405 |
|
Negative | 14 (50.0) | 4.785
(3.670-7.963) | | 1.525
(0.960-1.920) | | 0.310
(0.243-0.478) | | 0.115
(0.063-0.265) | | 3.650
(2.312-6.035) | | 128.3
(108.9-167.6) | | 4.885
(2.502-6.351) | | 634.4
(459.2-1218.0) | | 48.95
(46.18-52.68) | | 0.0262
(0.0145-0.0675) | |
| SNAI1 | | | | | | | | | | | | | | | | | | | | | |
|
Positive | 10 (35.7) | 5.400
(3.890-7.948) | 0.4081 | 1.740
(1.328-2.535) | 0.3318 | 0.395
(0.305-0.455) | 0.4567 | 0.200
(0.078-0.383) | 0.8226 | 3.330
(1.989-5.592) | 0.9063 | 128.9
(102.6-153.1) | 0.4642 | 4.524
(3.479-6.404) | 0.9812 | 783.7
(353.4-1173.0) | 0.7595 | 51.85
(47.51-53.24) | 0.3375 | 0.0450
(0.0198-0.1029) | 0.9720 |
|
Negative | 18 (64.3) | 4.375
(3.815-5.678) | | 1.640
(0.945-2.118) | | 0.315
(0.243-0.493) | | 0.135
(0.070-0.418) | | 2.985
(1.899-4.533) | | 134.9
(102.0-205.6) | | 4.885
(2.815-6.919) | | 523.4
(459.2-1181.0) | | 49.15
(46.18-51.96) | | 0.0346
(0.0179-0.1254) | |
| VIM | | | | | | | | | | | | | | | | | | | | | |
|
Positive | 12 (42.9) | 4.415
(3.643-7.868) | 0.9818 | 1.585
(1.255-2.428) | 0.9454 | 0.395
(0.268-0.455) | 0.4850 | 0.135
(0.070-0.358) | 0.8100 | 3.227
(1.706-5.634) | 0.8731 | 133.4
(84.4-167.4) | 0.8017 | 5.967
(2.895-6.590) | 0.8372 | 687.0
(316.2-1163.0) | >0.9999 | 49.28
(46.74-52.46) | 0.9725 | 0.0346
(0.0177-0.1177) | 0.9549 |
|
Negative | 16 (57.1) | 4.785
(3.870-5.485) | | 1.685
(0.975-2.153) | | 0.315
(0.245-0.485) | | 0.200
(0.073-0.448) | | 3.108
(2.442-4.303) | | 128.9
(113.2-162.8) | | 4.220
(3.029-6.984) | | 616.9
(448.8-1165.0) | | 50.18
(45.21-53.13) | | 0.0450
(0.0189-0.1143) | |
| CD44 | | | | | | | | | | | | | | | | | | | | | |
|
Positive | 15 (53.6) | 5.440
(4.190-8.360) | 0.0520 | 1.620
(0.990-2.460) | 0.7168 | 0.410
(0.320-0.500) | 0.0314a | 0.180
(0.080-0.480) | 0.6088 | 3.691
(1.713-6.253) | 0.3627 | 122.2
(98.5-166.7) | 0.4672 | 3.821
(3.000-6.122) | 0.2737 | 745.6
(359.3-1226.0) | 0.6177 | 49.30
(47.75-52.45) | 0.9372 | 0.0400
(0.0205-0.1200) | 0.7077 |
|
Negative | 13 (46.4) | 4.150
(3.600-5.395) | | 1.670
(1.120-2.135) | | 0.270
(0.220-0.380) | | 0.100
(0.070-0.345) | | 2.724
(2.002-3.947) | | 148.8
(110.4-181.7) | | 6.185
(3.233-7.716) | | 523.1
(454.0-1020.0) | | 51.00
(45.33-54.35) | | 0.0222
(0.0174-0.1210) | |
| NANOG | | | | | | | | | | | | | | | | | | | | | |
|
Positive | 10 (35.7) | 4.205
(3.800-4.783) | 0.1749 | 1.905
(1.463-2.473) | 0.1749 | 0.355
(0.235-0.530) | 0.9343 | 0.325
(0.078-0.713) | 0.2293 | 2.448
(1.711-3.498) | 0.0987 | 111.2
(75.6-142.9) | 0.0800 | 5.967
(3.390-8.523) | 0.3318 | 453.5
(323.4-1001.0) | 0.0400a | 50.15
(44.06-55.35) | 0.8973 | 0.1095
(0.0198-0.1819) | 0.1868 |
|
Negative | 18 (64.3) | 5.425
(3.965-7.200) | | 1.525
(0.960-2.203) | | 0.365
(0.265-0.448) | | 0.135
(0.070-0.322) | | 3.710
(2.351-5.701) | | 150.0
(117.1-167.6) | | 4.273
(2.815-6.351) | | 836.0
(484.6-1239.0) | | 49.30
(46.56-52.26) | | 0.0346
(0.0179-0.0717) | |
| ALDH1A1 | | | | | | | | | | | | | | | | | | | | | |
|
Positive | 14 (50.0) | 4.835
(3.345-8.603) | 0.8388 | 1.525
(1.185-2.308) | 0.5714 | 0.360
(0.258-0.418) | 0.8123 | 0.100
(0.070-0.398) | 0.3331 | 3.330
(1.871-5.926) | 0.6347 | 128.9
(96.9-161.3) | 0.6673 | 5.189
(3.450-6.257) | 0.9459 | 634.4
(329.2-1275.0) | 0.9459 | 50.43
(46.91-52.48) | 0.4473 | 0.0222
(0.0172-0.1093) | 0.2502 |
|
Negative | 14 (50.0) | 4.655
(3.930-5.670) | | 1.735
(0.960-2.280) | | 0.365
(0.235-0.530) | | 0.265
(0.093-0.425) | | 2.953
(2.017-4.211) | | 134.9
(108.4-176.3) | | 4.273
(2.657-7.762) | | 672.7
(459.2-1084.0) | | 48.85
(44.66-53.84) | | 0.0622
(0.0213-0.1450) | |
| CD47 | | | | | | | | | | | | | | | | | | | | | |
|
Positive | 16 (57.1) | 5.435
(4.240-8.018) | 0.0031a | 1.615
(1.010-2.250) | 0.6642 | 0.410
(0.368-0.515) | 0.0016a | 0.260
(0.100-0.448) | 0.1350 | 3.849
(2.171-6.144) | 0.0593 | 147.4
(111.0-169.5) | 0.2803 | 3.710
(2.745-6.045) | 0.0661 | 923.2
(466.0-1219.0) | 0.0816 | 49.33
(47.98-52.53) | 0.3776 | 0.0598
(0.0222-0.1213) | 0.1182 |
|
Negative | 12 (42.9) | 3.890
(3.115-4.725) | | 1.685
(1.060-2.290) | | 0.255
(0.225-0.323) | | 0.075
(0.048-0.335) | | 2.693
(1.686-3.518) | | 118.1
(91.4-150.6) | | 6.213
(4.011-8.042) | | 481.0
(322.0-867.4) | | 48.38
(45.09-52.89) | | 0.0195
(0.0107-0.0930) | |
| CD274 | | | | | | | | | | | | | | | | | | | | | |
|
Positive | 11 (39.3) | 4.790
(3.840-8.360) | 0.5784 | 1.490
(0.860-2.100) | 0.2255 | 0.360
(0.260-0.470) | 0.7902 | 0.180
(0.080-0.320) | 0.9170 | 3.691
(2.441-5.517) | 0.2255 | 143.5
(121.0-205.0) | 0.0659 | 3.821
(2.660-7.250) | 0.4581 | 821.8
(464.5-1425.0) | 0.2441 | 51.00
(46.30-52.45) | 0.9172 | 0.0400
(0.0205-0.1200) | 0.8440 |
|
Negative | 17 (60.7) | 4.530
(3.820-5.915) | | 1.670
(1.355-2.395) | | 0.370
(0.250-0.455) | | 0.140
(0.070-0.465) | | 2.724
(1.708-4.067) | | 111.7
(82.8-157.1) | | 5.813
(3.299-6.496) | | 523.1
(322.7-1165.0) | | 49.30
(46.23-52.95) | | 0.0389
(0.0180-0.1137) | |
|
PDCD1-LG2 | | | | | | | | | | | | | | | | | | | | | |
|
Positive | 8 (28.6) | 4.870
(3.798-9.088) | 0.5327 | 1.475
(0.900-2.458) | 0.8227 | 0.370
(0.268-0.463) | 0.6445 | 0.075
(0.048-0.123) | 0.0271a | 4.244
(1.895-6.579) | 0.4385 | 132.9
(88.0-198.2) | 0.8617 | 4.480
(2.745-5.898) | 0.4688 | 856.9
(341.7-1722.0) | 0.5327 | 50.43
(47.56-52.29) | 0.7379 | 0.0190
(0.0111-0.0282) | 0.0207a |
|
Negative | 20 (71.4) | 4.655
(3.870-5.483) | | 1.645
(1.313-2.153) | | 0.365
(0.250-0.478) | | 0.265
(0.100-0.513) | | 2.985
(1.962-4.116) | | 128.3
(105.1-157.7) | | 5.216
(3.207-7.109) | | 634.7
(448.8-1042.0) | | 49.18
(45.93-53.13) | | 0.0622
(0.0222-0.1327) | |
Discussion
Circulating immune-related cells extravasate,
migrate toward the tumor site, and perform multiple important
functions in the immune response against tumor cells. It is well
known that the interaction between immune cells and tumor cells in
the tumor microenvironment is associated with prognosis and
treatment efficacy (3,4). Systemic immunity in cancer patients
also plays a crucial role in processes ranging from tumor
initiation to metastatic progression. To date, several systemic
immune-related markers, including NLR, PLR, and SII, have been
reported to reflect disease progression and therapeutic response as
well as predict prognosis in patients with HNSCC (17-19).
In the present study, despite its small sample size, several
immune-related markers were clearly correlated with clinical
features and prognosis. Patients with advanced disease exhibited
significantly higher monocyte counts and lower LMR than those with
early-stage disease. Our previous study on peripheral monocytes in
patients with oropharyngeal squamous cell carcinoma (OPSCC)
indicated that elevated monocyte counts and lower LMR were
independent prognostic factors for PFS and OS, respectively
(20). In line with our previous
study, in cases of HNSCC including OPSCC, similar findings were
observed, suggesting that circulating monocytes in patients with
HNSCC are closely related to disease status. Although the reason
for this association is not yet fully understood, a high monocyte
count generally reflects chronic inflammatory conditions, which can
promote angiogenesis, induce cell proliferation, increase reactive
oxygen species production, and suppress antitumor immunity
(21,22). In our previous study, the presence
of CTCs was associated with treatment response, locoregional
recurrence, and PFS (12); however,
there was no significant correlation between the presence of CTCs
and systemic immune-related markers. Therefore, systemic
immune-related markers may be insufficient to assess antitumor
immunity against CTCs. Notably, lymphocyte-related markers,
lymphocyte counts, NLR, and LMR were significantly associated with
distant metastasis. These findings imply that lymphocyte-mediated
systemic immune responses may contribute to the prevention of
distant metastasis. So far, several studies have investigated the
relationship between systemic immune-related markers and primary
tumor characteristics using immunohistochemistry or molecular
analysis; however, it seems that no meaningful correlations have
yet been observed (23-25).
In the dynamic multistep process of colonization of distant organs,
CTCs that disseminate in the bloodstream and seed new tumors at
distant organ sites might have acquired a status of dormancy in the
peripheral bloodstream. Therefore, we investigated the relationship
between the molecular characteristics of CTCs and systemic
immune-related markers.
Among the 10 genes tested, PIK3CA,
CD47, and PDCD1LG2 expression levels in CTCs were
significantly correlated with two systemic immune-related markers.
PIK3CA is an oncogene that is known to play a role in
regulating cell proliferation, invasion, and metabolism (26,27).
Chen et al demonstrated that PIK3CA overexpression
promotes the epithelial-mesenchymal transition and enriches cancer
stem cells in both murine and human HNSCC cell lines (28). Moreover, PIK3CA
overexpression was reported to be associated with poor outcomes
(29). Patients with
PIK3CA-positive CTCs showed higher lymphocyte counts and
higher PNI, suggesting that CTCs could acquire immune resistance
through PIK3CA expression. Indeed, in mouse experiments
using pancreatic cancer cell lines, PIK3CA-AKT signaling in tumors
was found to reduce the cell-surface expression levels of major
histocompatibility complex I molecules and CD80, which promote
immune evasion (30). Additionally,
a tendency toward significance between the other two
lymphocyte-related markers (NLR and LMR) and PIK3CA
expression in CTCs suggests immune evasion by PIK3CA
expression in CTCs.
CD47-positive CTCs were found in patients
with higher neutrophil and monocyte counts. In addition, high NLR,
low LMR, and high SII showed a tendency toward CD47
expression in CTCs. CD47 has been shown to be highly expressed in
multiple cancer types, including HNSCC (31-34).
We previously reported that CD47 is expressed in approximately half
(56.8%) of oral SCC tissues and that CD47 expression correlates
with poor OS (34). Most
importantly, CD47 acts as a signal to inhibit phagocytic activity
by binding to signal regulatory protein α (SIRPα) present on
phagocytes (35); thus, it has been
suggested that tumor cells evade the host's immune surveillance by
expressing CD47 on their surface. As SIRPα is known to be expressed
on monocytes, macrophages, neutrophils, and dendritic cells
(36,37), in cases of higher circulating
monocyte and/or neutrophil counts, CTCs may be more likely to be
phagocytosed and killed by these cells. Some CTCs may upregulate
CD47 expression to evade the innate immune response mediated by
neutrophils and monocytes.
Finally, PDCD1LG2 expression in CTCs was
observed in patients with lower CRP values and lower CARs. Similar
to programmed cell death 1 ligand 1 (PD-L1), PD-L2 encoded by the
PDCD1IG2 gene binds to PD-1 on T cells and inhibits T-cell
proliferation and effector functions (38). Moreover, the expression of PD-L2 is
regulated by interferon receptor signaling pathways, particularly
the interferon-γ (IFN-γ) pathway (39). CRP is an acute inflammatory protein
that increases in response to infection and inflammation. Recently,
Yoshida et al demonstrated that CRP inhibits proliferation,
activation-associated phenotypes, and the effector function of
activated T cells in patients with melanoma (40). Thus, high CRP levels may impair
adaptive immunity and consequently affect PD-L2 expression on CTCs
via reduced IFN-γ production.
Although the relatively small sample size partially
limits the strength of these findings, our results indicate that
circulating immune cells and their related markers are correlated
with disease progression and clinical outcomes in patients with
HNSCC. Moreover, the interaction between CTCs and circulating
immune cells appears to provide survival advantages via molecular
alterations to CTCs. Further elucidation of the survival mechanisms
of CTCs in the blood microenvironment may provide new insights into
novel therapeutic strategies targeting CTCs.
Acknowledgements
Not applicable.
Funding
The present study was supported in part by a Grant-in-Aid for
Scientific Research (grant nos. 20K18243, 20K09747, 19K18794,
19K18758 and 20H03834) from the Japan Ministry of Education,
Culture, Sports, Science and Technology.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
HTad and KC conceived and designed the study. HTak,
YN, TM, SI and IM acquired the data. HTad and HTak analyzed and
interpreted the data. HTad, HTak and KC confirm the authenticity of
the raw data. HTad and KC wrote the manuscript. All authors have
read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethical
Committee of Gunma University Hospital (Maebashi, Japan; approval
no. 12-12), and written informed consent was obtained from each
patient.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ferris RL, Blumenschein G Jr, Fayette J,
Guigay J, Colevas AD, Licitra L, Harrington K, Kasper S, Vokes EE,
Even C, et al: Nivolumab for recurrent squamous-cell carcinoma of
the head and neck. N Engl J Med. 375:1856–1867. 2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Burtness B, Harrington KJ, Greil R,
Soulières D, Tahara M, de Castro G Jr, Psyrri A, Basté N, Neupane
P, Bratland Å, et al: Pembrolizumab alone or with chemotherapy
versus cetuximab with chemotherapy for recurrent or metastatic
squamous cell carcinoma of the head and neck (KEYNOTE-048): A
randomised, open-label, phase 3 study. Lancet. 394:1915–1928.
2019.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Pitt JM, Marabelle A, Eggermont A, Soria
JC, Kroemer G and Zitvogel L: Targeting the tumor microenvironment:
Removing obstruction to anticancer immune responses and
immunotherapy. Ann Oncol. 27:1482–1492. 2016.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Murciano-Goroff YR, Warner AB and Wolchok
JD: The future of cancer immunotherapy: Microenvironment-targeting
combinations. Cell Res. 30:507–519. 2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Alečković M, McAllister SS and Polyak K:
Metastasis as a systemic disease: Molecular insights and clinical
implications. Biochim Biophys Acta Rev Cancer. 1872:89–102.
2019.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Diakos CI, Charles KA, McMillan DC and
Clarke SJ: Cancer-related inflammation and treatment effectiveness.
Lancet Oncol. 15:e493–e503. 2014.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Janssen LME, Ramsay EE, Logsdon CD and
Overwijk WW: The immune system in cancer metastasis: Friend or foe?
J Immunother Cancer. 5(79)2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Dolan RD, Laird BJA, Horgan PG and
McMillan DC: The prognostic value of the systemic inflammatory
response in randomised clinical trials in cancer: A systematic
review. Crit Rev Oncol Hematol. 132:130–137. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Gutkin DW and Shurin MR: Clinical
evaluation of systemic and local immune responses in cancer: Time
for integration. Cancer Immunol Immunother. 63:45–57.
2014.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Mego M, Gao H, Cohen EN, Anfossi S,
Giordano A, Sanda T, Fouad TM, De Giorgi U, Giuliano M, Woodward
WA, et al: Circulating tumor cells (CTC) are associated with
defects in adaptive immunity in patients with inflammatory breast
cancer. J Cancer. 7:1095–1104. 2016.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Ye L, Zhang F, Li H, Yang L, Lv T, Gu W
and Song Y: Circulating tumor cells were associated with the number
of T lymphocyte subsets and NK cells in peripheral blood in
advanced non-small-cell lung cancer. Dis Markers.
2017(5727815)2017.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Tada H, Takahashi H, Kuwabara-Yokobori Y,
Shino M and Chikamatsu K: Molecular profiling of circulating tumor
cells predicts clinical outcome in head and neck squamous cell
carcinoma. Oral Oncol. 102(104558)2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Hu B, Yang XR, Xu Y, Sun YF, Sun C, Guo W,
Zhang X, Wang WM, Qiu SJ, Zhou J and Fan J: Systemic
immune-inflammation index predicts prognosis of patients after
curative resection for hepatocellular carcinoma. Clin Cancer Res.
20:6212–6222. 2014.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Onodera T, Goseki N and Kosaki G:
Prognostic nutritional index in gastrointestinal surgery of
malnourished cancer patients. Nihon Geka Gakkai Zasshi.
85:1001–1005. 1984.PubMed/NCBI(In Japanese).
|
|
15
|
Ranzani OT, Zampieri FG, Forte DN, Azevedo
LC and Park M: C-reactive protein/albumin ratio predicts 90-day
mortality of septic patients. PLoS One. 8(e59321)2013.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408.
2001.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Jiang W, Chen Y, Huang J, Xi D, Chen J,
Shao Y, Xu G, Ying W, Wei J, Chen J, et al: Systemic
immune-inflammation index predicts the clinical outcome in patients
with nasopharyngeal carcinoma: A propensity score-matched analysis.
Oncotarget. 8:66075–66086. 2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Diao P, Wu Y, Li J, Zhang W, Huang R, Zhou
C, Wang Y and Cheng J: Preoperative systemic immune-inflammation
index predicts prognosis of patients with oral squamous cell
carcinoma after curative resection. J Transl Med.
16(365)2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Szilasi Z, Jósa V, Zrubka Z, Mezei T, Vass
T, Merkel K, Helfferich F and Baranyai Z: Neutrophil-to-lymphocyte
and platelet-to-lymphocyte ratios as prognostic markers of survival
in patients with head and neck tumours-results of a retrospective
multicentric study. Int J Environ Res Public Health.
17(1742)2020.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Takahashi H, Sakakura K, Tada H, Kaira K,
Oyama T and Chikamatsu K: Prognostic significance and population
dynamics of peripheral monocytes in patients with oropharyngeal
squamous cell carcinoma. Head Neck. 41:1880–1888. 2019.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Grivennikov SI, Greten FR and Karin M:
Immunity, inflammation, and cancer. Cell. 140:883–899.
2010.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Greten FR and Grivennikov SI: Inflammation
and cancer: Triggers, mechanisms, and consequences. Immunity.
51:27–41. 2019.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Chen ZY, Raghav K, Lieu CH, Jiang ZQ, Eng
C, Vauthey JN, Chang GJ, Qiao W, Morris J, Hong D, et al: Cytokine
profile and prognostic significance of high neutrophil-lymphocyte
ratio in colorectal cancer. Br J Cancer. 112:1088–1097.
2015.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Yersal Ö, Çetinkünar S, Aktimur R, Aziret
M, Özdaş S, Erdem H and Yildirim K: Neutrophil/lymphocyte and
platelet/lymphocyte ratios are not different among breast cancer
subtypes. Asian Pac J Cancer Prev. 18:2227–2231. 2017.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Cao Z, Ji J, Zhang C, Wang F, Xu H, Yu Y
and Sun Y: The preoperative neutrophil-to-lymphocyte ratio is not a
marker of prostate cancer characteristics but is an independent
predictor of biochemical recurrence in patients receiving radical
prostatectomy. Cancer Med. 8:1004–1012. 2019.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Samuels Y and Ericson K: Oncogenic PI3K
and its role in cancer. Curr Opin Oncol. 18:77–82. 2006.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Rogers SJ, Box C, Harrington KJ, Nutting
C, Rhys-Evans P and Eccles SA: The phosphoinositide 3-kinase
signalling pathway as a therapeutic target in squamous cell
carcinoma of the head and neck. Expert Opin Ther Targets.
9:769–790. 2005.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Chen X, Cao Y, Sedhom W, Lu L, Liu Y, Wang
H, Oka M, Bornstein S, Said S, Song J and Lu SL: Distinct roles of
PIK3CA in the enrichment and maintenance of cancer stem cells in
head and neck squamous cell carcinoma. Mol Oncol. 14:139–158.
2020.PubMed/NCBI View Article : Google Scholar
|
|
29
|
García-Escudero R, Segrelles C, Dueñas M,
Pombo M, Ballestín C, Alonso-Riaño M, Nenclares P,
Álvarez-Rodríguez R, Sánchez-Aniceto G, Ruíz-Alonso A, et al:
Overexpression of PIK3CA in head and neck squamous cell carcinoma
is associated with poor outcome and activation of the YAP pathway.
Oral Oncol. 79:55–63. 2018.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Sivaram N, McLaughlin PA, Han HV, Petrenko
O, Jiang YP, Ballou LM, Pham K, Liu C, van der Velden AW and Lin
RZ: Tumor-intrinsic PIK3CA represses tumor immunogenecity in a
model of pancreatic cancer. J Clin Invest. 129:3264–3276.
2019.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Willingham SB, Volkmer JP, Gentles AJ,
Sahoo D, Dalerba P, Mitra SS, Wang J, Contreras-Trujillo H, Martin
R, Cohen JD, et al: The CD47-signal regulatory protein alpha
(SIRPa) interaction is a therapeutic target for human solid tumors.
Proc Natl Acad Sci USA. 109:6662–6667. 2012.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Baccelli I, Stenzinger A, Vogel V,
Pfitzner BM, Klein C, Wallwiener M, Scharpff M, Saini M,
Holland-Letz T, Sinn HP, et al: Co-expression of MET and CD47 is a
novel prognosticator for survival of luminal breast cancer
patients. Oncotarget. 5:8147–8160. 2014.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Wang H, Tan M, Zhang S, Li X, Gao J, Zhang
D, Hao Y, Gao S, Liu J and Lin B: Expression and significance of
CD44, CD47 and c-met in ovarian clear cell carcinoma. Int J Mol
Sci. 16:3391–3404. 2015.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Sakakura K, Takahashi H, Kaira K, Toyoda
M, Murata T, Ohnishi H, Oyama T and Chikamatsu K: Relationship
between tumor-associated macrophage subsets and CD47 expression in
squamous cell carcinoma of the head and neck in the tumor
microenvironment. Lab Invest. 96:994–1003. 2016.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Matozaki T, Murata Y, Okazawa H and
Ohnishi H: Functions and molecular mechanisms of the CD47-SIRPalpha
signalling pathway. Trends Cell Biol. 19:72–80. 2009.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Adams S, van der Laan LJ, Vernon-Wilson E,
Renardel de Lavalette C, Döpp EA, Dijkstra CD, Simmons DL and van
den Berg TK: Signal-regulatory protein is selectively expressed by
myeloid and neuronal cells. J Immunol. 161:1853–1859.
1998.PubMed/NCBI
|
|
37
|
Kharitonenkov A, Chen Z, Sures I, Wang H,
Schilling J and Ullrich A: A family of proteins that inhibit
signalling through tyrosine kinase receptors. Nature. 386:181–186.
1997.PubMed/NCBI View
Article : Google Scholar
|
|
38
|
Rozali EN, Hato SV, Robinson BW, Lake RA
and Lesterhuis WJ: Programmed death ligand 2 in cancer-induced
immune suppression. Clin Dev Immunol. 2012(656340)2012.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Garcia-Diaz A, Shin DS, Moreno BH, Saco J,
Escuin-Ordinas H, Rodriguez GA, Zaretsky JM, Sun L, Hugo W, Wang X,
et al: Interferon receptor signaling pathways regulating PD-L1 and
PD-L2 expression. Cell Rep. 19:1189–1201. 2017.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Yoshida T, Ichikawa J, Giuroiu I, Laino
AS, Hao Y, Krogsgaard M, Vassallo M, Woods DM, Stephen Hodi F and
Weber J: C reactive protein impairs adaptive immunity in immune
cells of patients with melanoma. J Immunother Cancer.
8(e000234)2020.PubMed/NCBI View Article : Google Scholar
|