Introduction
Differentiated thyroid cancer (DTC) represents the
vast majority (90%) of all thyroid cancers, and it includes
papillary and follicular neoplasms (1). According to epidemiologic estimations
there were 63.000 new cases of DTC in the United States in 2014
compared to 37.200 in 2009(1). This
trend has been attributed almost entirely to the increase of the
incidence of the papillary thyroid carcinoma (PTC) which is the
most common form of DTC (1). In
particular, the increasing use of neck ultrasonography resulted in
a considerable rise of the new cases of PTC ≤1 cm which is
distinguished as the papillary thyroid microcarcinoma (PTMC)
(1,2). Additionally, there has been a doubling
of the clinically-occult thyroid cancers which are detected
incidentally during the pathologic exam after thyroidectomy for
benign indication (2).
PTC involves cervical lymph node metastases in
20-50% of the patients, and the frequency of lymph node
micrometastases (<2 mm) may approach 90% in some series
(1). In addition, there have been
interesting reports of rare cases of incidental detection of PTMC
in cervical lymph nodes without identifiable tumour within the
thyroid gland (3). These
extra-thyroid PTMC foci have been stipulated as metastases from an
unknown primary deriving from the thyroid parenchyma despite
thorough pathologic examination of the specimen (3). Due to their rare occurrence, their
clinical potential is not discussed in the American Thyroid
Association (ATA) guidelines (1).
With this communication we aim to provide an expert
opinion concerning the clinical importance of PTC microscopic foci
in cervical lymph nodes with no identifiable tumour within the
thyroid, despite meticulous pathologic examination of the gland.
For this objective, a clinical case is briefly described and it is
discussed in view of the revised recommendation of the available
ATA guidelines (1) regarding a
present primary PTMC with lymph node micrometastases.
Case report
A 43-year old white male patient was referred to the
Department of Endocrine Surgery, Euroclinic Hospital, Athens,
Greece due to thyroid multinodular goiter in September 2017. He had
a feeling of mild pressure in the neck in the past few months,
which was exhibited particularly during swallowing. The largest
nodule was 29 mm and displayed TI-RADS 2 characteristics in
imaging. According to his anamnesis the nodule had grown in
dimension. Thyroglobulin, calcitonin and CEA levels were normal and
the patient was euthyroid. Further observation or surgical options
were discussed with the patient and a total en-block thyroidectomy
was performed in consideration of his preferences.
The surgical specimen of total thyroidectomy was
inserted in buffered formalin (1:10) and the entire gland underwent
thorough macroscopic and histopathologic examination by two
experienced endocrine pathologists. The thyroid gland weighted 22
g. The dimensions of the right lobe were 4.5x3x1.7 cm, and the
dimensions of the left lobe were 5x2.5x2.2 cm with the inclusion of
the isthmus and the pyramidal lobe. The specimen capsule was
intact. The thyroid gland was seriously sectioned and sampled into
its entirety with a total of 26 parafine blocks and a mean width of
2.1 mm for each slice. Hematoxylin and eosin staining were employed
for morphologic assessment. Commercially available immune
antibodies were used to detect thyroglobulin receptors (Τhermo,
1:600, Ab-6 coctail). Pre-digestion was performed for 3 min with
0.05% protease VIII in a 0.1 Μ phosphate buffer with ph=7.8 at
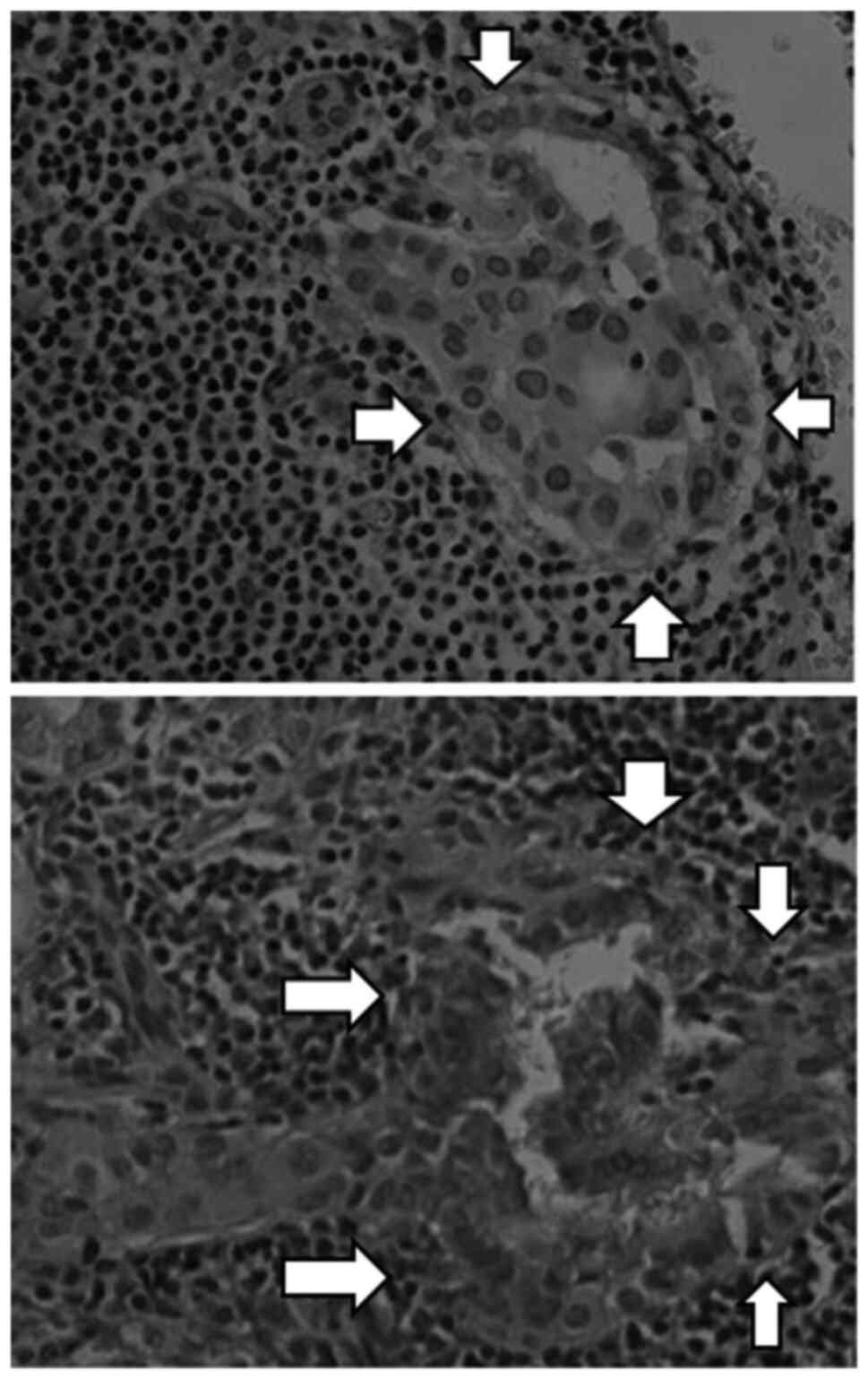
37˚C. The findings were consistent with thyroid multinodular
hyperplasia and there was no detectable tumor in the thyroid. Two
of the excised lymph nodes from the central neck compartment
displayed multiple confluent papillary micro-formations (0.3-1 mm
of diameter) with clear irregular nuclei and papillary thyroid
cancer phenotype. In immunohistochemistry the carcinoma cells were
positive for thyroglobulin receptors. The microformations are shown
in Fig. 1 with positive
thyroglobulin immunostaining.
The existing guidelines did not consider at all PTMC
cases with an absent primary. The decision of the
multi-disciplinary neck-endocrine oncological meeting classified
the patient in the group of intermediate risk for recurrence or
metastasis. The patient underwent post-operative radioactive iodine
(RAI) therapy and a standard treatment-policy was employed in the
course of this study. At three years and three months of follow-up
the is no sign of recurrence and the serum thyroglobulin level
remains low (<0.3 ng/ml).
The patient consented in written for the publication
of his case in the form of a case report. Approval from the ethical
committee is not required in our hospital for case report
publications.
Discussion
The presence of PTC tissue in cervical lymph nodes
without identification of any cancer in the thyroid itself is a
very uncommon event with unknown etiology. So far, it has been
considered to represent lymph node metastatic disease from an
occult primary thyroid microcarcinoma (3). A recent review of the literature by Xu
et al has reported that there have been only 9
well-documented cases of metastatic thyroid carcinoma in cervical
lymph nodes with no detectable primary, despite a thorough
histopathologic examination of the thyroid (3).
The meticulous pathologic examination that was
performed in the case that we describe herein failed to show any
original cancer in the thyroid parenchyma. The mechanism of this
rare phenomenon remains unknown (3)
as the attainment of direct proof is more than challenging.
Therefore, possible suggestions concerning its etiology are rather
theoretic. It has been proposed that even exhaustive
histopathologic examination may miss a microcarcinoma <3 mm in
size, which is a lesion that may have the potential to develop
metastases (3,4). In our case, the histologic sections
had a mean thickness of 2.1 mm which provided a good possibility
for the detection of even smaller lesions (less than 1-2 mm). The
second theory suggests the probability that the primary tumor
regresses to fibrotic tissue within the thyroid parenchyma
(3). Bearing in mind the
comprehensive pathologic examination in our case-which included an
extended re-evaluation of the specimen -, the undersigned authors
consider and propose an additional alternative etiologic
possibility without rejecting the existing ones. A PTMC focus in
the thyroid parenchyma may be indeed absent in some of the cases.
The explanation could be hidden in the uncommon but well-documented
(5) presence of inclusions of
benign thyroid tissue in cervical lymph nodes. Consequently, the
possibility that such benign deposits evolved to intra-lymph node
PTC micro-deposits due to the action of unknown biochemical or
molecular stimuli can not be dismissed.
Concerning the clinical aspect of our case, it
should be highlighted that the current guidelines do not deal at
all with the rare entity of PTC micro-foci in the cervical lymph
nodes with no detectable thyroid primary (1). Proper disease risk-stratification
should be the main objective also in cases of PTC micro-inclusions
in cervical lymph nodes with an occult or questionable primary
tumor in order to guide therapy and follow-up. As the ATA
guidelines consider only the eventuality of a known primary PTC
with or without nodal metastases (1), we believe that the closest
extrapolation that can be dragged for our case is to assume the
same lymph node invasion pattern in a patient with a detected PTMC.
The previous version (2009) of the ATA guidelines advocated that
patients with a primary PTMC and any cervical lymph node metastasis
belong to the intermediate-risk group for recurrence or metastasis
(6). However, the subsequent
version of these guidelines which was published in 2015 considered
that the clinical implication of regional lymph node
micrometastases may be less significant than previously thought
(1). The new ATA proposal was
therefore modified accordingly and downgraded the patients with a
known primary PTMC and ≤5 of regional lymph node micrometastases in
the low-risk group (1).
The herein case with two local micro-foci of PTC in
regional lymph nodes and absent or occult intra-thyroid cancer
(despite thorough pathologic examination) would correspond rather
to the intermediate-risk group of the 2009 ATA risk stratification
(6). However, by extrapolating the
information provided in the latest ATA guidelines (1) for patients with a known primary PTMC
and ≤5 regional node micrometastases, our case displays a pattern
with better association to a weak malignant potential and therefore
it should be included in the low-risk group. This change in the
stratification of the risk of the same patient between the current
and the previous version of the ATA recommendations is clinically
important as both versions advocate that RAI adjuvant therapy
should be administered in the intermediate-risk patients, but not
for those with low-risk. Low-risk patients that have undergone
total thyroidectomy should have routine post-operative measurements
of serum thyroglobulin with the consideration of ultrasound and/or
RAI scanning for diagnostic purposes (1). In turn, a different case with multiple
(>5) PTC micro-inclusions in lymph nodes and without an
identifiable primary after total thyroidectomy would better pertain
to the intermediate-risk and therefore adjuvant RAI should be
considered.
It should be noted that our specimen was not tested
for a BRAFV600E mutation, however in our opinion this poses only a
marginal limitation to this study. The current ATA recommendations
are not routinely recommending BRAF mutational evaluation for
initial postoperative risk stratification in DTC (1). In particular, PTMC harboring BRAFV600E
mutations with no other worrisome features are considered as
low-risk lesions (1). It could be
possible that a BRAFV600E mutation is followed by increased risk of
recurrence or mortality in larger DTCs, however there is not enough
evidence yet that this factor could be used in isolation for the
risk-stratification (1). Moreover,
the follow-up of our case reached 3,25 years. A concern could be
raised if this patient would continue to remain disease-free or
not, as the possibility for a recurrence is not well documented in
literature for a PTMC after the course of 5 years (1,7).
However, it is known that the initial risk estimates are modified
during time for DTC and they improve if there is no evidence of
disease during follow-up (1,7). It
should be noted that the risk of recurrence in patients initially
classified as at intermediate risk drops from 35 to 1-2% if they
display excellent response at 18 months of follow-up (1,7).
Bearing in mind this example and the excellent course of our
(low-risk) patient during follow-up it could be inferred that the
probability of a recurrence could be even less than 1%. A very
interesting review by Xu et al identified five
well-documented cases of metastatic PTMC without evidence of any
thyroid primary (3). Half of these
patients were positive for BRAFV600E, two patients received
postoperative radioiodine therapy (with 2 and 5 positive lymph
nodes, respectively), and all five were alive and without evidence
of recurrence at a median follow-up of 2.2 years (3). This additional evidence concurs that
PTMC foci in lymph nodes with absent primary is rather a low-risk
entity. In conclusion, patients with a few (≤5) PTC microscopic
(<2 mm) deposits in cervical lymph nodes with an occult (or
questionable) primary tumor appear to bear a low potential for
recurrence or metastasis after total thyroidectomy. Extrapolating
from the latest ATA guidelines concerning the same lymph
node-involvement pattern but a detected primary PTMC in the
pathologic examination, adjuvant RAI therapy should be regarded
rather as an overtreatment and should be avoided.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
Data sharing is not applicable to this article, as
no datasets were generated or analyzed during the current
study.
Authors' contributions
EK and AK conceived the current study. EK, AK, IK,
CI and TF designed the current study. EK, AK, IK, CI and TF
acquired the data. EK, AK, IK, CI and TF drafted the manuscript.
EK, AK and CI revised the manuscript. EK and AK provided final
approval for the manuscript. All authors read and approved the
final manuscript. EK and AK confirm the authenticity of all the raw
data.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
The patient provided written informed consent for
the publication of his data.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Haugen BR, Alexander EK, Bible KC, Doherty
GM, Mandel SJ, Nikiforov YE, Pacini F, Randolph GW, Sawka AM,
Schlumberger M, et al: 2015 American thyroid association management
guidelines for adult patients with thyroid nodules and
differentiated thyroid cancer: The American thyroid association
guidelines task force on thyroid nodules and differentiated thyroid
Cancer. Thyroid. 26:1–133. 2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Siegel R, Ma J, Zou Z and Jemal A: Cancer
statistics 2014. CA Cancer J Clin. 64:9–29. 2014.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Xu B, Scognamiglio T, Cohen PR, Prasad ML,
Hasanovic A, Tuttle RM, Katabi N and Ghossein RA: Metastatic
thyroid carcinoma without identifiable primary tumor within the
thyroid gland: A retrospective study of a rare phenomenon. Hum
Pathol. 65:133–139. 2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Ghossein R, Ganly I, Biagini A, Robenshtok
E, Rivera M and Tuttle RM: Prognostic factors in papillary
microcarcinoma with emphasis on histologic subtyping: A
clinicopathologic study of 148 cases. Thyroid. 24:245–253.
2014.PubMed/NCBI View Article : Google Scholar
|
|
5
|
León X, Sancho FJ, García J, Sañudo JR,
Orús C and Quer M: Incidence and significance of clinically
unsuspected thyroid tissue in lymph nodes found during neck
dissection in head and neck carcinoma patients. Laryngoscope.
115:470–474. 2005.PubMed/NCBI View Article : Google Scholar
|
|
6
|
American Thyroid Association (ATA)
Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid
Cancer. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel
SJ, Mazzaferri EL, McIver B, Pacini F, et al: Revised American
thyroid association management guidelines for patients with thyroid
nodules and differentiated thyroid cancer. Thyroid. 19:1167–1214.
2009.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Lamartina L and Handkiewicz-Junak D:
Follow-up of low risk thyroid cancer patients: Can we stop
follow-up after 5 years of complete remission? Eur J Endocrinol.
182:D1–D16. 2020.PubMed/NCBI View Article : Google Scholar
|