Introduction
Malignant pleural mesothelioma (MPM) is often
associated with asbestos exposure and carries an extremely poor
prognosis (1). The mean latency of
MPM following asbestos exposure is 40 years (1). Although several non-surgical
treatments for MPM are available, the role of surgery is still
important (1). Extra-pleural
pneumonectomy (EPP) has long been considered a radical approach;
however, the Mesothelioma and Radical Surgery (MARS) study reported
that EPP has a 14.4-month median survival and might harm patients
(2). Thereafter extended pleural
decortication (PD) was recommended over EPP due to fewer
complications (1).
PD entails removal of the parietal and visceral
pleura with sparing of the pulmonary parenchyma in an effort to
excise all macroscopic tumors (3).
Patients with PD have lower complication and mortality rates than
patients with EPP; however, complete resection (R0) is extremely
difficult with little improvement in prognosis (3). As additional intraoperative treatment,
photodynamic therapy (PDT) can improve the prognosis of patients
with MPM (4); however, PDT is
currently not authorized for use in patients with MPM in Japan.
Argon plasma coagulation (APC) is effective for
tumor resection or hemostasis with minimal complications and is
commonly used for treatment of endobronchial tumors (5-7);
however, there are no reports involving the use of APC in the
treatment of MPM. We have mainly used APC for hemostasis during PD
since 2015, and we recently noticed an anti-tumor effect for
patients with MPM. The aim of this study was to determine the
effectiveness of APC in the treatment of patients with MPM who
undergo a radical PD.
Materials and methods
Ethics approval
This study was approved by the Ethics Committee of
Toho University Omori Medical Center (M20085).
Study population
APC was performed for hemostasis after decortication
on all patients who underwent a radical PD from July 2015 to March
2020. We retrospectively analyzed clinical data from all 11
patients who had undergone a radical PD with APC treatment at Toho
University Hospital from July 2015 to March 2020. The clinical
features, local recurrence, and prognoses were further
evaluated.
The following parameters were retrieved from the
medical records: Gender, age, pathologic diagnoses, pathologic TNM
staging, adjuvant therapy, local recurrences, and outcomes.
Surgical methods
We performed a radical PD through the 5 and 9th
intercostal spaces. Of note, the 9th intercostal space was used for
resection of pleura at the costodiaphragmatic recess of the pleural
cavity. All visceral and parietal pleura, including the interlobar
spaces, were resected with caution to avoid the pericardium and
peritoneum, thus minimizing the risk of tumor dissemination to the
pericardial or abdominal cavities. After pleural resection, we
performed APC to the chest wall while avoiding the nerves, vessels,
and pericardium.
APC
The patients received standard rather than novel or
experimental clinical treatment. All patients were treated with an
ERBE Argon Plasma Coagulator VIO300D/APC2 (Elektromedizin GmbH).
The argon gas flow rate was 2 l/min with a maximum electrical power
setting of 80 W. The APC applicator was 110 mm in length and 2.3 mm
in diameter.
Statistical analysis
We evaluated the prognosis and survival time, based
on Kaplan-Meier analysis, from the date of surgery until the time
of recurrence or death or last follow-up evaluation, and univariate
comparison was performed using the log-rank test. All statistical
analyses were performed using JMP software, version 14.0 (SAS
Institute Inc.).
Results
Characteristics of the study
population
The patient characteristics are shown in Table I. Of the 11 patients, the oldest
patient was 79 years of age. No complications were associated with
APC. One patient had a sarcomatoid mesothelioma. One inpatient died
due to a cardiac arrhythmia (Table
II).
 | Table IClinical characteristics of patients
with malignant pleural mesothelioma. |
Table I
Clinical characteristics of patients
with malignant pleural mesothelioma.
| Clinical factor | Number of
patients |
|---|
| Patient number | 11 |
| Age, mean
(range) | 65.8 (48-79) |
| Sex | |
|
Male | 7 |
|
Female | 4 |
| Location | |
|
Right
side | 7 |
|
Left
side | 4 |
| Pathological TNM
stage | |
|
IA(T1N0M0) | 7 |
|
IB(T2N0M0) | 3 |
|
IIIA(T3N1M0) | 1 |
| Pathological
diagnosis | |
|
Epithelioid | 5 |
|
Biphasic | 5 |
|
Sarcomatoid | 1 |
 | Table IIFrequency of each complication-related
factor. |
Table II
Frequency of each complication-related
factor.
| Clinical factor | Total |
|---|
| Adjuvant therapy | |
|
Chemotherapy | 9 |
|
No
chemotherapy | 2 |
| Adjuvant
chemotherapy | |
|
CDDP+PEM | 4 |
|
CBDCA+PEM | 5 |
| Recurrence | |
|
Positive | 7 |
|
Negative | 3 |
|
Inpatient
death | 1 |
| Recurrence in
CDDP+PEM | |
|
Positive | 2 |
|
Negative | 2 |
| Recurrence in
CBDCA+PEM | |
|
Positive | 4 |
|
Negative | 1 |
Prognoses
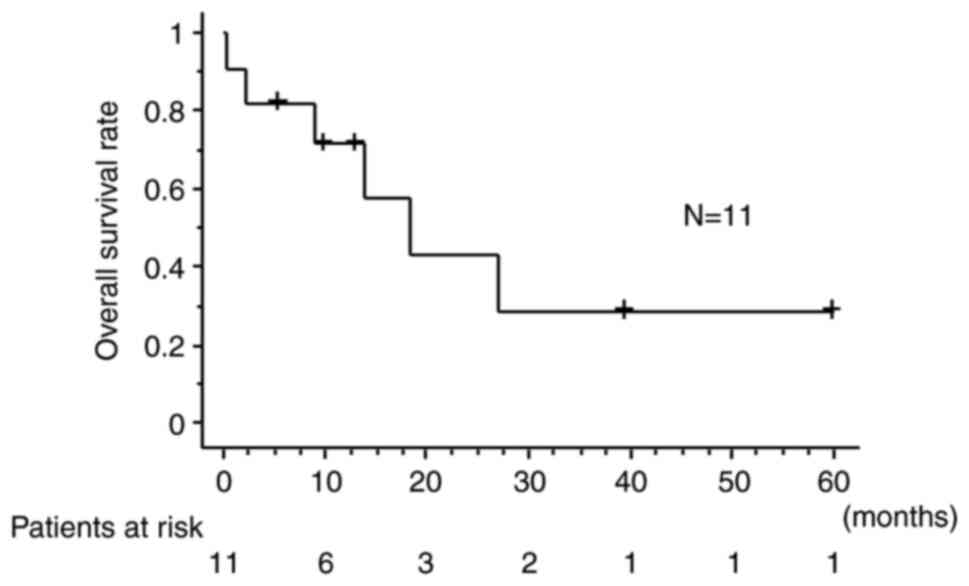
The median overall survival was 18.5 months. The 1-
and 2-year overall survival rates were 71.6 and 43.0%, respectively
(Fig. 1). One patient survived 5
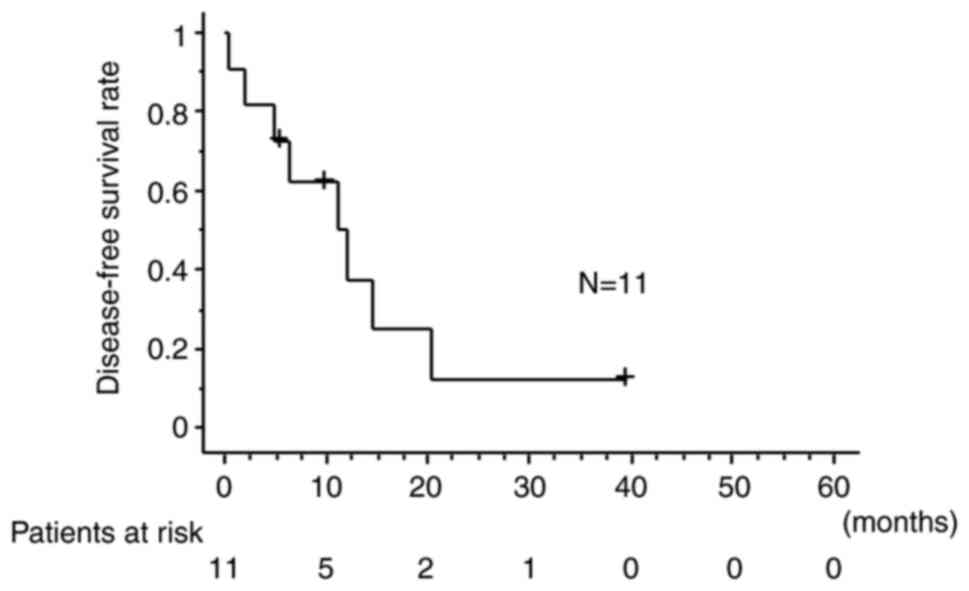
years, but had recurrent tumors. The median disease-free survival
was 11.1 months. The 1- and 2-year disease-free survival rates were
49.9 and 12.5%, respectively (Fig.
2). Three patients had no recurrences, two of whom had been
followed continuously (39.6 and 10.2 months). On overall survival
and disease-free survival, there was no significant difference
between patients with epithelioid type and with non-epithelioid
(overall survival, P=0.8558, disease-free survival, P=0.2559).
Discussion
PD for patients with MPM is considered less invasive
compared to EPP, and PD is recommended for some patients over EPP
(1); however, PD alone is not
sufficient to cure MPM because the goal of surgery in patients with
MPM is to achieve macroscopic complete resection, while multimodal
treatments, including additional intraoperative treatments for
local control, have been attempted (1,4).
Friedberg et al (4)
performed PDT therapy after radical pleurectomy with good outcomes
and concluded that PDT might have a role in extending survival via
direct cell death, breakdown of tumor neovasculature, and/or the
immune response, although PDT does not appear to have a positive
impact on local control (4).
Unfortunately, PDT cannot be used for patients with MPM in Japan
due to a lack of social insurance system coverage.
APC is considered a minimally invasive procedure
with fewer complications compared to the Nd-YAG laser. APC is
commonly used for treatment of endobronchial tumors given the
benefits of minimal smoke and good visual control (7). APC is useful for intraoperative
hemostasis without severe complications, and APC results for tumors
may be equal to the reported laser results (7).
We have mainly used APC for hemostasis during PD
since 2015 and we recently noticed an anti-tumor effect among
patients with MPM. Although APC is useful for intraoperative
hemostasis in patients with MPM, our study showed that APC may have
an anti-tumor effect secondary to coagulation. In the present study
1 patient survived 5 years and 3 patients had disease-free survival
with the median overall survival of 18.5 months and the median
disease-free survival of 11.1 months. A prior phase I trial of
intraoperative hyperthermic treatments using cisplatin and
gemcitabine for MPM revealed that the median overall and
recurrence-free survival times were 20.3 and 10.7 months,
respectively, the results of which were similar to our results
(8), although chemotherapy of
pemetrexed plus cisplatin for MPM revealed the median overall
survival of 16.1 months (9). Our
study revealed longer median survival compared to group with
chemotherapy alone. Considering the rationale underlying PD is to
achieve macroscopic complete resection without microscopic complete
resection, this is the first report demonstrating the usefulness of
APC for patients with MPM. Indeed, there are few reports involving
experimental or feasibility studies combined with hyperthermic
intrathoracic chemoperfusion therapy on cold plasma coagulation
(10,11). Hoffman et al (11) reported the feasibility of cold
plasma coagulation using helium gas and several adverse events were
reported; however, there was no reference to the prognostic impact
of cold plasma coagulation. In contrast, no complications were
associated with APC. Although Hoffman et al (11) combined cold plasma coagulation with
hyperthermic intrathoracic chemoperfusion therapy, we did not and
only performed APC intraoperatively. Although APC differs from cold
plasma coagulation, the adverse events reported in the Hoffman
et al study (11) might be
related to a combination of hyperthermic intrathoracic
chemoperfusion therapy.
The reason why our results revealed no complications
related to APC might be because we exercised caution in protecting
nerves, vessels, and the pericardium from the APC during radical
PD. Indeed, normal organs must be protected from collateral injury
during APC.
We acknowledge the limitations of this study. Our
study had a retrospective single arm and consisted of a small
cohort, which limited the generalizability of our results. Because
this study was retrospective, we could not get patients' consents.
The potential participants were given the opportunity to decline to
be further enrolled in the study (opt-out). However, despite these
limitations, we did not report any adverse events associated with
APC and the outcomes were favorable.
We believe that APC may be able to be selected as a
potential intraoperative adjuvant treatment for MPM due to the
potential anti-tumor effects. We look forward to evaluating our
findings in a larger and multi-center study involving APC in
patients with MPM.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Author's contributions
YA, TS, SK, HO, NT, KI, AS and AI were involved in
the conception and design of the study. AI wrote the manuscript.
YA, TS, SK, HO and AS collected data. NT and KI supervised the
study. AI and AS confirm the authenticity of all the raw data. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Toho
University Omori Medical Center Ethics Committee (approval no.
M20085). Due to the retrospective nature of the present study,
informed consent was not required from patients according to the
Ethical Guidelines for Medical and Health Research involving Human
Subjects of the Ministry of Health, Labour and Welfare in Japan
(https://www.mhlw.go.jp/file/06-Seisakujouhou-10600000-Daijinkanboukouseikagakuka/0000080278.pdf).
The present study design was accepted by the Ethics Committee on
the condition that a document declaring an opt-out policy by which
any possible patient and/or relatives could decline to be included
in this study was uploaded on the web page of the Toho University
Omori Medical Center (https://www.omori.med.toho-u.ac.jp/byoin/ethical_committee/pdf/rinri_M20085.pdf).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Opitz I, Scherpereel A, Berghmans T,
Psallidas I, Glatzer M, Rigau D, Astoul P, Bölükbas S, Boyd J,
Coolen J, et al: ERS/ESTS/EACTS/ESTRO guidelines for the management
of malignant pleural mesothelioma. Eur J Cardiothorac Surg.
58:1–24. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Treasure T, Lang-Lazdunski L, Waller D,
Bliss JM, Tan C, Entwisle J, Snee M, O'Brien M, Thomas G, Senan S,
et al: Extra-pleural pneumonectomy versus no extra-pleural
pneumonectomy for patients with malignant pleural mesothelioma:
Clinical outcomes of the Mesothelioma and Radical Surgery (MARS)
randomised feasibility study. Lancet Oncol. 12:763–772.
2011.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Bovolato P, Casadio C, Billè A, Ardissone
F, Santambrogio L, Ratto GB, Garofalo G, Bedini AV, Garassino M,
Porcu L, et al: Does surgery improve survival of patients with
malignant pleural mesothelioma?: A multicenter retrospective
analysis of 1365 consecutive patients. J Thorac Oncol. 9:390–396.
2014.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Friedberg JS, Culligan MJ, Mick R,
Stevenson J, Hahn SM, Sterman D, Punekar S, Glatstein E and Cengel
K: Radical pleurectomy and intraoperative photodynamic therapy for
malignant pleural mesothelioma. Ann Thorac Surg. 93:1658–1665;
discussion 1665-1667. 2012.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Bolliger CT, Sutedja TG, Strausz J and
Freitag L: Therapeutic bronchoscopy with immediate effect: Laser,
electrocautery, argon plasma coagulation and stents. Eur Respir J.
27:1258–1271. 2006.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Kesrouani A, Dabar G, Rahal S and Ghorra
C: Treatment of tracheal mucoepidermoid carcinoma by argon plasma
coagulation during pregnancy. Int Surg. 100:927–929.
2015.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Okada S, Yamauchi H, Ishimori S, Satoh S,
Sugawara H and Tanaba Y: Endoscopic surgery with a flexible
bronchoscope and argon plasma coagulation for tracheobronchial
tumors. J Thorac Cardiovasc Surg. 121:180–182. 2001.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Burt BM, Richards WG, Lee HS, Bartel S,
Dasilva MC, Gill RR, Jaklitsch MT, Johnson BE, Swanson SJ, Bueno R
and Sugarbaker DJ: A Phase I Trial of surgical resection and
intraoperative hyperthermic cisplatin and gemcitabine for pleural
mesothelioma. J Thorac Oncol. 13:1400–1409. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Zalcman G, Mazieres J, Margery J,
Greillier L, Audigier-Valette C, Moro-Sibilot D, Molinier O, Corre
R, Monnet I, Gounant V, et al: Bevacizumab for newly diagnosed
pleural mesothelioma in the mesothelioma avastin cisplatin
pemetrexed study (MAPS): A randomised, controlled, open-label,
phase 3 trial. Lancet. 387:1405–1414. 2016.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Hoffmann M, Ulrich A, Schloericke E,
Limmer S, Habermann JK, Wolken H, Bruch HP and Kujath P: The
application of cold-plasma coagulation on the visceral pleura
results in a predictable depth of necrosis without fistula
generation. Interact Cardiovasc Thorac Surg. 14:239–243.
2012.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Hoffmann M, Bruch HP, Kujath P and Limmer
S: Cold-plasma coagulation in the treatment of malignant pleural
mesothelioma: Results of a combined approach. Interact Cardiovasc
Thorac Surg. 10:502–505. 2010.PubMed/NCBI View Article : Google Scholar
|