Introduction
Both general practitioners and specialized
palliative care teams tend to terminally ill cancer patients at
home. Predicting the degree of care a patient needs, and hence, the
suitable type or level of outpatient care required, is not trivial.
Erring on either side will result in withholding adequate care,
either by undertreating the index patient or by straining the
resources available to other patients. A number of scales and
scores in palliative care exists to estimate overall prognosis and
partly to identify areas of need (1). The difference between general and
specialized palliative care has often been defined by ‘complexity’,
which is in itself an ill-defined term, and most often translates
into the quantification of symptoms (2).
This analytic approach is largely driven by an
effort to fragmentize the need for palliative care into manageable
items, not least to justify costs. In its essence however,
palliative care is a holistic approach, qualified by the need to
keep in contact with the situation at large, whilst adequately
addressing present symptoms (3).
Hence, in this study, a tool to support decision-making in touch
with the patient's situation and the caregivers' intuition was
examined, attempting to establish criteria that are neither overly
detailed nor arbitrary.
In particular with regard to palliative care,
intuition appears to implicitly inform medical decisions more often
than generally presumed. This happens rather as an unacknowledged
subtext than a consciously employed and recorded method (4). Thus, to develop a scoring method, a
phenomenological grounded theory approach was employed (5), evaluating existing literature on
referral criteria and patient- or proxy-reported outcome measures
in palliative care (6-10).
The results showed that three core aspects directed the perception
of a terminally ill patient's multi-facetted situation.
In a first approach, these three items had been
termed ‘instability of the environment’, ‘weight of symptoms’ and
‘instability of the situation’. Upon validating this score, it
underwent further development using the grounded theory process.
The revised score then consisted of three dimensions termed
‘perception of strength’, ‘perception of support and stability’ and
‘medical prognosis’. This score placed a clearer distinction
between patient-reported and caregiver-observed criteria. In
addition, it was easier to apply in practice, as instead of being
deficiency-oriented, it was resource-oriented; that is, the higher
the value, the better off the patient.
As these terms, such as a coordinate system,
describe different dimensions, further consolidation into a single
figure would come at the price of losing information gained in the
process. Thus, it was decided to record the three dimensions
separately in addition to combining them into one score.
The primary aim of this exploratory,
non-interventional study was to assess whether this synthetic
approach to summarizing the information gathered by the initial
patient work-up in an ambulatory palliative care setting may
predict the level of care required.
The secondary aims were to assess whether such an
intuitive assessment and its documentation were feasible in daily
practice.
Patients and methods
Study design and ethics approval
In a monocentric study, 142 patients referred for
ambulatory palliative care were assessed in a mixed urban and rural
area in Germany over a 2-year period between October 2015 and
September 2017. Inclusion criteria were advanced and progredient
incurable disease with a short life expectancy of weeks to months
and complex symptoms. Exclusion criteria were incapability to give
informed consent or lack thereof, and incapability to participate
in a complete initial anamnestic and physical assessment. All
patients referred to ambulatory palliative care within the study
period were screened and finally included into the study. The
present study was approved by the Ethics Committee of the
Medizinische Hochschule Brandenburg Theodor Fontane and conducted
according to the Declaration of Helsinki as adopted by the World
Medical Organization in October 2013(11), and all patients provided written
informed consent to participate.
Patient characteristics
The distribution of the sexes of the total study
population was skewed towards males (n=83; 58% vs. n=59; 42%).
Excluding one pediatric patient from further evaluation, the median
age was 73 years (age range, 42-91 years), and 18% were living
alone. In the vast majority of patients, the life-limiting
diagnosis was malignant disease (90.1%). Amongst the 60 patients
evaluated using the final version of the scoring system, the
distribution of sexes was slightly more even with 33 male and 27
female patients (55 and 45%, respectively), the median age was 76
years (age range, 50-91 years), and 88.3% of the patients had a
malignant disease as the primary diagnosis; Table I shows the demographic
characteristics, Table II the
medical characteristics of the patients.
 | Table IDemographic patient
characteristics. |
Table I
Demographic patient
characteristics.
| Characteristic | Female | Male | Total |
|---|
| Sex, % | 41.5 | 58.5 | 100 |
| Age, years, mean | 73.5 | 71.7 | 72.4 |
| Age, years,
median | 72 | 75 | 73 |
| Age, 95 % confidence
interval | 53.1-93.9 | 50.3-91.6 | 51.7-92.5 |
 | Table IIMedical patient characteristics. |
Table II
Medical patient characteristics.
| Diagnostic
category | % | n |
|---|
| Total | 100 | 142 |
| Malignant | 90.1 | 128 |
| Hematologic | 9.2 | 13 |
| Solid, intermediate
stage | 17.6 | 25 |
| Solid, late
stage | 63.4 | 90 |
| Non-malignant | 6.3 | 9 |
| Unknown | 3.5 | 5 |
| Malignant
diagnoses | | |
| Leukemia | 2.1 | 3 |
| Lymphoma | 7 | 10 |
| Central nervous
system | 1.4 | 2 |
| Head and neck | 5.6 | 8 |
| Esophageal | 2.1 | 3 |
| Gastric | 4.2 | 6 |
| Intestinal | 1.4 | 2 |
| Colorectal | 7 | 10 |
| Liver | 7 | 10 |
| Pancreatic | 6.3 | 9 |
| Lung and pleura | 16.9 | 24 |
| Breast | 6.3 | 9 |
| Gynacological | 2.1 | 3 |
| Prostate | 5.6 | 8 |
| Urogenital | 7 | 10 |
| Melanoma, sarcoma or
neuroendocrine | 2.8 | 4 |
| Carcinoma of unknown
primary | 4.9 | 7 |
Study procedure
The assessments were performed by one of three
participating palliative care physicians, who contributed 67, 28,
and 5% of the assessments for this study. Patients' consent only
covered assessment by their assigned primary palliative care
physician. All participating physicians were board certified in
palliative medicine with >20 years professional experience each.
The initial outpatient palliative care visit routinely consisted of
recording a multi-dimensional patient history including medical,
family and psychosocial aspects, their current situation and
patients' perceptions and expectations, followed by a physical
examination and subsequent care-planning for the immediate future.
Upon completion of this visit, the physician rated and documented
the score parameters. After the end of ambulatory palliative care,
items describing each patient's pre-existing condition and the
palliative care effort delivered (documentation items) were
collected in a pseudonymized database.
Development and evaluation of the
score
A total of 82 patients were assessed with the first
scoring approach described in the introduction. Upon analyzing the
results, both as to practical applicability and prognostic value
for the required extent of palliative care, it was revisited, and
for the subsequent 60 patients, the score comprising the parameters
‘perception of strength’, ‘perception of support and stability’,
and ‘medical prognosis’ was used. Upon performing the initial
patient workup, the physician gave an estimate of these parameters
using a positive visual analog scale, where 10 was the best
possible or ‘healthy’ realization of each parameter and 0 was the
worst possible realization. The complete score for each patient was
calculated as the sum of the three constituent parameters, and thus
had a range of 0-30.
Both the complete score and its constituent
parameters were compared with two established scores, the Hospice
and Palliative care Evaluation (HOPE) (9) and the Karnofsky index (KI) (12), and with documentation items
indicating the actual care effort delivered to a patient. The
established scores were applied by the same physician at the same
time as the experimental score.
Statistical analysis
Statistical calculations were performed using SPSS
version 21.0 (TBM Corp). Numerically scaled values of the
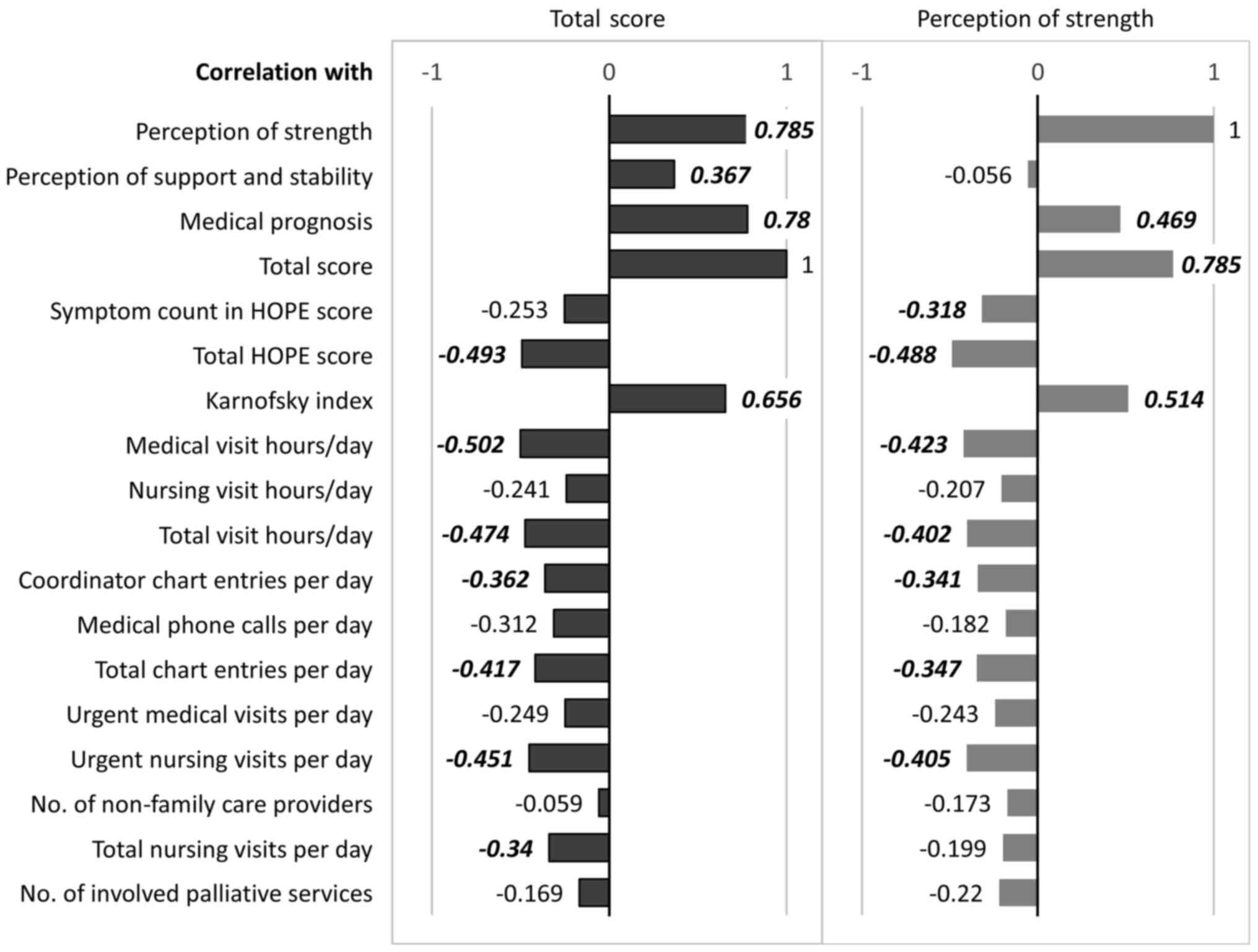
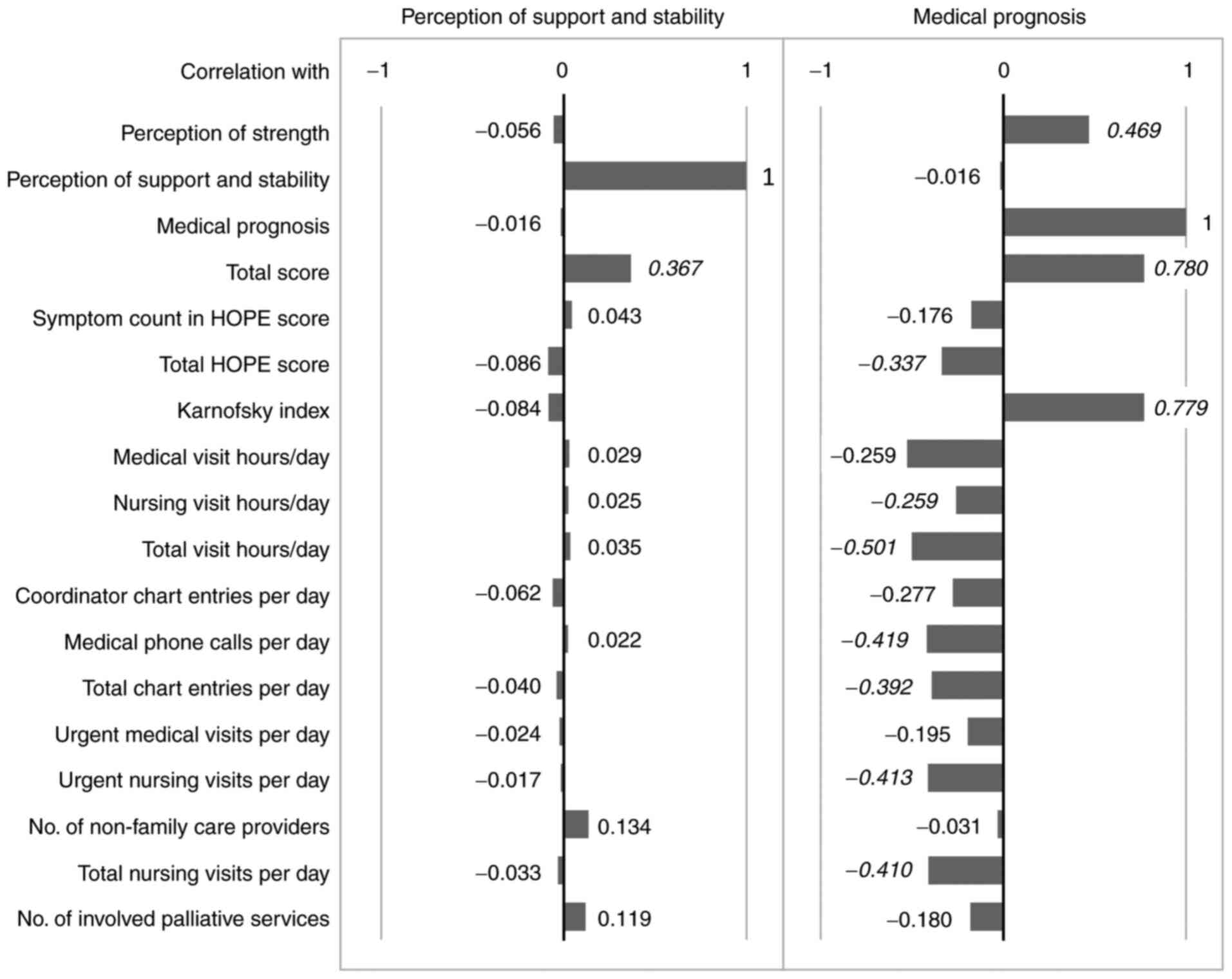
individual observation items as listed in Figs. 1 and 2 were compared to the total score value
using a Pearson's correlation analysis, followed by subsequent
multivariate regression analysis, where correlations >0.2 were
found to be significant. As all items were at least interval
scaled, this analysis was deemed appropriate to maintain a uniform
evaluation method. For the initial version of the score, a sample
size of n=83, and for the final version, a sample size of n=60 was
evaluated. For the sample size and distribution, the indicated
Pearson's r correlation coefficients were associated with the
following levels of significance according to the two-sided
Student's t-test: r>0.3, P<0.01; r>0.4, P<0.001;
r>0.5, P<0.0001. Correlation coefficients reaching a level of
significance of P<0.01 have been highlighted in bold italics in
the figures.
Results
Inter-rater variability
A direct comparison between raters on the same
patient was methodologically impossible. Comparing the two
physicians who together provided >90 percent of the assessments,
descriptive statistics revealed mean rating scores of 4.0/10 vs.
6.10/10 (perception of support and stability), 7.5/10 vs. 8.0/10
(perception of strength) and 7.95/10 vs. 7.5/10 (medical
condition), respectively. Due to the small number of interviews, a
meaningful comparison with the third participating physician was
not possible.
Primary score
To provide an impression of the actual score figures
with the initial scoring approach, the means (and confidence
intervals) were 19.67 (12.75-26.59) for the total and 5.13
(0.87-9.39) for ‘instability of the environment’, 7.28 (4.07-10.50)
for ‘weight of symptoms’ and 7.25 (4.12-10.39) for ‘instability of
the situation’. Here, the total score correlated well with all
three constituent parameters, but significant correlations were
found only of the total score, ‘weight of symptoms’ and
‘instability of the situation’ as score parameters, and the
documentation items ‘number of medical visits’, ‘number of urgent
medical visits’ and ‘number of medical phone calls’. None of these
reached a correlation coefficient of 0.3, which was considered the
significance threshold; thus, this score was not pursued any
further.-
Revised score
The means (and confidence intervals) of the revised
score were 16.1 (7.3-24.9) for the total score, 4.6 (0-9.5) for
‘perception of strength’, 6.8 (3.2-10.4) for ‘perception of support
and stability’ and 4.7 (0.1-9.3) for ‘medical prognosis’. From
sample size and distribution, the indicated Pearson's r correlation
coefficients were associated with the following significance
levels: r>0.3, P<0.01; r>0.4, P<0.001; and r>0.5,
P<0.0001. These results are summarized in Figs. 1 and 2, where statistically significant
correlations (P<0.01) have been highlighted.
With correlation coefficients of 0.66 and 0.49, the
scores of the present study correlated well with KI and HOPE
scores, respectively; the latter correlation being inverse as HOPE
increases with symptom load, whereas KI and the experimental score
increase with performance and resources. The constituent dimensions
‘perception of strength’ and ‘medical prognosis’ (correlation
coefficients 0.79 and 0.78, respectively) most strongly predicted
the total score (Figs. 1 and
2).
The actual care effort delivered to the patient did
not correlate with rural/urban residence, age, sex, number of
symptom-relieving drugs taken, assigned degree of nursing care,
tumor stage or number of residents in the household.
Looking at individual documentation items indicating
the palliative care efforts actually delivered, none correlated
with ‘perception of support and stability’ (Fig. 2). A subgroup defined by this
parameter in which the score was <5 however, showed consistently
high documentation item values for care effort, consistent with
high care requirements due to little existing support (data not
shown).
Both the total score and its constituent parameters
‘perception of strength’ and ‘medical prognosis’ correlated
inversely with the following documentation items for palliative
care effort: Time for medical visits, time for medical and nursing
visits, number of entries by coordinator and by palliative
physician, and number of urgent nursing visits. The number of
medical phone calls and the total number of nursing visits per day
correlated inversely with ‘medical prognosis’ and with the total
score.
Discussion
There are several different scoring systems
available for evaluating palliative care, starting with the KI and
ECOG scores developed for use in oncology. These are still being
amended to develop newer more accurate models (1,9,13).
However, the focus of these models is primarily on symptom severity
and overall prognosis, rather than estimation of resources needed
(1,6,14,15).
In 2016, an international group found six predominant themes, which
largely corresponded to the dimensions of the score developed in
the present study (10). Far from a
one-to-one translation, other groups also came across similar
dimensions to evaluate the need for palliative care. An
international consensus paper on referral criteria for outpatient
specialty palliative care by Hui et al (16) comprised 11 major and 36 minor
criteria. Thus, a demand for brief, patient-oriented assessment
tools has been recognized and is being addressed by newer scales,
such as the integrated palliative care outcome scale (IPOS)
(13,15).
In the present study, the practical reliability of
intuitive decisions regarding resource allocations in palliative
care, and whether this approach can be systematically incorporated
into structured decision-making was assessed. By applying a
phenomenological method to the experience of the examining
physician (4,5), it was assumed that intuition
facilitates perceptions that allow for a more focused comprehensive
picture, in that it does not seek separated parts, but incorporates
several meaningful entities which are difficult to measure. The
perceived entities arise and differ depending on the question
asked. Hence, the three dimensions of the score employed here feed
back on the reported perceptions of the rating physician and
focuses their attention towards them.
The score introduced here strongly correlated with
documentation items indicating palliative care effort, such as the
number of interactions of caregivers, the time required and the
number of emergency visits. In this, it may actually be suitable to
support decision-making about general or specialized palliative
care assignments. Yet the present study has clear limitations. The
numbers of patients as well as rating physicians were small, and it
was a single center study. If one were to ‘calibrate’ this score, a
larger population or a less diverse setting as to the patients'
environmental situation would be required. In addition, it would be
interesting to apply it in different countries and cultural
settings to see to what extent its questions and the perceptions
informing their answers are culturally defined or universal.
A very stimulating result in this context is the
lack of correlation between the initial ‘perception of support and
stability’ and the outcomes of interest. One explanation could be a
principal inaccuracy of assessment due to rapid changes in the
event of massive disturbances leading to hospital admissions or
relocation to the hospice. Therefore, this constituent parameter of
the score may be particularly prone to culturally defined
perceptions, and further phenomenological research should deal with
an intercultural and situational meaning of support. Another
explanation could be that this estimator serves as an internal
correction to the others. This is, in part, supported by the
observation that there may be a threshold effect where patients
with ‘less than sufficient’ perception of support and stability
require a greater degree of palliative care. To see this
statistically would again require larger numbers, but a closer
prospective look at this parameter in individual future patients
may help to resolve this question.
The good correlation of the scoring system developed
in the present study with that of the KI for general performance
poses the question whether both measure the same quality. The KI
basically pertains to general physical fitness, not to dimensions
of prognosis and self-perception of the patient. Still, these
qualities are associated with each other; improved physical
performance is likely associated with an improved perception of
strength and less subjective need of being cared for.
To test for this, the KI was statistically
incorporated into the scoring system, either as an additional or as
a substitute for the apparently weak predictor ‘perception of
support and stability’. In both cases, it performed worse in
predicting the actual care effort than the original score did (data
not shown), supporting a preliminary view that both do not measure
the same. Again, to confirm this statistically rather than
narratively will require larger datasets.
Beyond that however, the value of the present
approach by its intention should not be limited to an improved
prediction of care effort, but support a more comprehensive
attitude of interacting with the patient, their environment and a
patient-centered medical view, and to do so without being inferior
in prediction to existing scores.
The idea of this approach is to counter a tendency
towards ever more detailed itemizations and to direct time and
attention back to inter-personal patient attention and care. In
this, it is a radically pragmatic approach to utilize caregiver's
capabilities of intuitive assessment in an explicit and reflected
manner. It must be emphasized however, that this does not in any
way imply to save time by placing a precedence of ‘gut feeling’
over factual assessment. To the opposite, the score was gathered
only after a thorough initial patient workup.
Whilst this score may help to estimate the amount
and intensity of palliative care required, a question not addressed
here is its cutoff. Obviously, no precise threshold, but only scale
areas indicating ‘rather general palliative care’, ‘rather
specialized palliative care’ or ‘indeterminate’ may possibly be
established in the future.
In summary, the present study explored a 3D
phenomenological model and suggests, without yet defining a
practically applicable discriminator, that their combination
correlates with the required extent of care at least as well as
existing scores. It was also suggested that performing and
documenting this score is feasible in the actual everyday work of
ambulatory palliative care. To validate the system for prospective
application and decision-making; however, will require additional,
larger and multi-center studies.
Acknowledgements
Not applicable.
Funding
The study was in part funded by internal institutional funds
from the Brandenburg Medical School Theodor Fontane.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
DH, MR and PMD conceived the study, and analyzed and
interpreted the data. DH performed the background research. DH, DS
and FK collected the data. PMD wrote the manuscript. DH, MR and PMD
edited the manuscript. DH and PMD confirm the authenticity of all
the raw data. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of the Brandenburg Medical School Theodor Fontane
(approval no. E-01-20180716) and was performed in accordance with
the Declaration of Helsinki. Consent was obtained as described in
the Methods section. All patients provided written informed consent
to participate.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Bausewein C, Le Grice C, Simon S and
Higginson I: PRISMA. The use of two common palliative outcome
measures in clinical care and research: A systematic review of POS
and STAS. Palliat Med. 25:304–313. 2011.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Kamps H and Harms D: Komplexe
hausarztmedizin. Z Allg Med. 87(5)2011.
|
|
3
|
Julião M, Sobral MA, Calçada P, Antunes B,
Nunes B, Bragança A, Runa D, Faria de Sousa P, Chochinov HM and
Bruera E: ‘Truly holistic?’ Differences in documenting physical and
psychosocial needs and hope in Portuguese palliative patients.
Palliat Support Care. 19:69–74. 2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Todd PM and Gigerenzer G: Precis of Simple
heuristics that make us smart. Behav Brain Sci. 23:727–780.
2000.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Giorgi A: An affirmation of the
phenomenological psychological descriptive method: A response to
Rennie (2012). Psychol Methods. 19:542–551. 2014.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Glare P, Shariff I and Thaler HT: External
validation of the number of risk factors score in a palliative care
outpatient clinic at a comprehensive cancer center. J Palliat Med.
17:797–802. 2014.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Maltoni M, Scarpi E, Pittureri C, Martini
F, Montanari L, Amaducci E, Derni S, Fabbri L, Rosati M, Amadori D
and Nanni O: Prospective comparison of prognostic scores in
palliative care cancer populations. Oncologist. 17:446–454.
2012.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Shinall MC, Ely EW, Karlekar M, Robbins
SG, Chandrasekhar R and Martin SF: Psychometric properties of the
FACIT-Pal 14 administered in an outpatient palliative care clinic.
Am J Hosp Palliat Care. 35:1292–1294. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Stiel S, Pollok A, Elsner F, Lindena G,
Ostgathe C, Nauck F and Radbruch L: Validation of the symptom and
problem checklist of the german hospice and palliative care
evaluation (HOPE). J Pain Symptom Manage. 43:593–605.
2012.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Hui D, Meng YC, Bruera S, Geng Y, Hutchins
R, Mori M, Strasser F and Bruera E: Referral criteria for
outpatient palliative cancer care: A systematic review. Oncologist.
21:895–901. 2016.PubMed/NCBI View Article : Google Scholar
|
|
11
|
World Medical Association. World Medical
Association Declaration of Helsinki: Ethical principles for medical
research involving human subjects. JAMA. 310:2191–2194.
2013.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Crooks V, Waller S, Smith T and Hahn TJ:
The use of the karnofsky performance scale in determining outcomes
and risk in geriatric outpatients. J Gerontol. 46:M139–M144.
1991.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Roch C, Palzer J, Zetzl T, Stork S, Frantz
S and van Oorschot B: Utility of the integrated palliative care
outcome scale (IPOS): A cross-sectional study in hospitalised
patients with heart failure. Eur J Cardiovasc Nurs. 19:702–710.
2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Etkind SN, Lovell N, Bone AE, Guo P,
Nicholson C, Murtagh FEM and Higginson IJ: The stability of care
preferences following acute illness: A mixed methods prospective
cohort study of frail older people. BMC Geriatr.
20(370)2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Murtagh FE, Ramsenthaler C, Firth A,
Groeneveld EI, Lovell N, Simon ST, Denzel J, Guo P, Bernhardt F,
Schildmann E, et al: A brief, patient- and proxy-reported outcome
measure in advanced illness: Validity, reliability and
responsiveness of the Integrated Palliative care Outcome Scale
(IPOS). Palliat Med. 33:1045–1057. 2019.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Hui D, Mori M, Watanabe SM, Caraceni A,
Strasser F, Saarto T, Cherny N, Glare P, Kaasa S and Bruera E:
Referral criteria for outpatient specialty palliative cancer care:
An international consensus. Lancet Oncol. 17:e552–e559.
2016.PubMed/NCBI View Article : Google Scholar
|