Introduction
More than half a million women are diagnosed with
cervical cancer (1). Introduction
of the Pap smear test has markedly decreased the mortality rate of
cervical cancer, but cervical cancer is the fourth most common
female malignancy worldwide and is still one of the leading causes
of death worldwide (1-5).
Incidence and mortality vary widely with geographic location, and
~90% of cervical cancers occur in low-income and middle-income
countries that lack organized screening and HPV vaccination
programs (1). To reduce cervical
cancer mortality, each management step - vaccination, screening,
colposcopy, and treatment - is essential (1,4,5). Among
these, colposcopy is frequently performed as a detailed examination
after an abnormal screening result (6,7).
Colposcopy is a visual examination, in which acetic acid is applied
to the cervix and then the cervix is visualized using magnification
through a colposcope. In Japan, colposcopy and consecutive biopsy
are performed for such patients as with abnormal cytology or normal
cytology and high-risk HPV infection.
Digital colposcopy built around a smartphone is
becoming common, and this has advantages for telemedicine and data
sharing by taking advantage of smartphone characteristics (8-12).
Also, digital colposcopy is considered to be promising in that it
can rapidly and relatively inexpensively screen the patients
(11). However, digital colposcopy
itself is not allowed in clinical practice in Japan. If digital
colposcopes can be shown to be comparable to traditional
colposcopes, then they can be useful to reduce the regional
disparity through telemedicine and data sharing mentioned above.
Also, efficient data collection may be contributed for development
of deep learning solutions (13).
For this reason, in this study we investigated the feasibility of
using a mobile digital colposcope that incorporates a smartphone,
in comparison with a traditional colposcope, in a population of
Japanese patients.
Materials and methods
Patient population
This study was approved by the Institutional Review
Board of Saitama Medical University International Medical Center
(approval no. 19-026, 12/Jun/2019; Hidaka, Japan). Patients who
underwent colposcopy at Saitama Medical University International
Medical Center between July 2019 and February 2020 were enrolled in
the study. The subjects were women aged 21-65 years old who were
referred for colposcopy following the standard of care. The
exclusion criteria were pregnancy, prior history of cervical
cancer, prior history of a cervical excisional procedure, and
hysterectomy. Written informed consent was obtained from all
subjects. A total of 40 patients (52 tests) were included in the
study. Some patients were tested two times through follow-up. The
clinical background of the patients is shown in Fig. 1. The median age was 46 (range,
27-65) years (Fig. 1A). Cytology
results are shown in Fig. 1B.
Colposcopy was performed at initial visit, just before conization
(preoperative examination), or if abnormal cytology was
detected.
Colposcopy
A standard colposcopy procedure was performed using
a conventional colposcope (Kolposkop 150 FC, Carl Zeiss), after
which an image of the cervix was captured using a mobile digital
colposcope that incorporated a smartphone (Eva Colpo, MobileODT)
(10-12).
All images were collected before biopsy. The Zeiss colposcope was
attached to a digital camera, but examiners mainly used the
binoculars for visualization. The images stored from the mobile
digital colposcope were evaluated after two weeks or more by the
examiner who had also performed the conventional examination. The
wait period of two weeks was used to ensure that the examiner would
no longer remember their initial clinical impression and allow a
fair comparison between the methods.
Evaluation
The diagnosis and site chosen for biopsy based on
conventional colposcopy were compared with those that would have
been determined using the digital images. Diagnoses were classified
as normal, cervical intraepithelial lesion (CIN) 1, CIN2, CIN3,
invasive cancer, adenocarcinoma in situ (AIS), and
unsatisfactory colposcopic findings (UCF). Diagnoses that matched
between conventional and digital colposcopy were defined as the
‘same’, and others were defined as ‘different’. Biopsy sites were
compared by dividing the cervix into twelve clockface regions. If
the actual (from conventional colposcopy) and assumed (from digital
colposcopy) biopsy sites matched, they were defined as the ‘same’;
if the sites differed by one clockface region, they were defined as
‘almost the same’; and all others were ‘different’. The
pathological findings were confirmed by biopsy or conization, and
the pathological diagnosis was confirmed by pathologists.
Statistical analysis
JMP 15 (SAS Institute, Inc.) was used for
statistical analysis. A paired t-test was used to compare the means
of matched rates between pathological diagnosis and colposcopy
diagnosis. The data are presented as the mean ± standard deviation.
P<0.05 was considered to indicate a statistically significant
difference.
Results
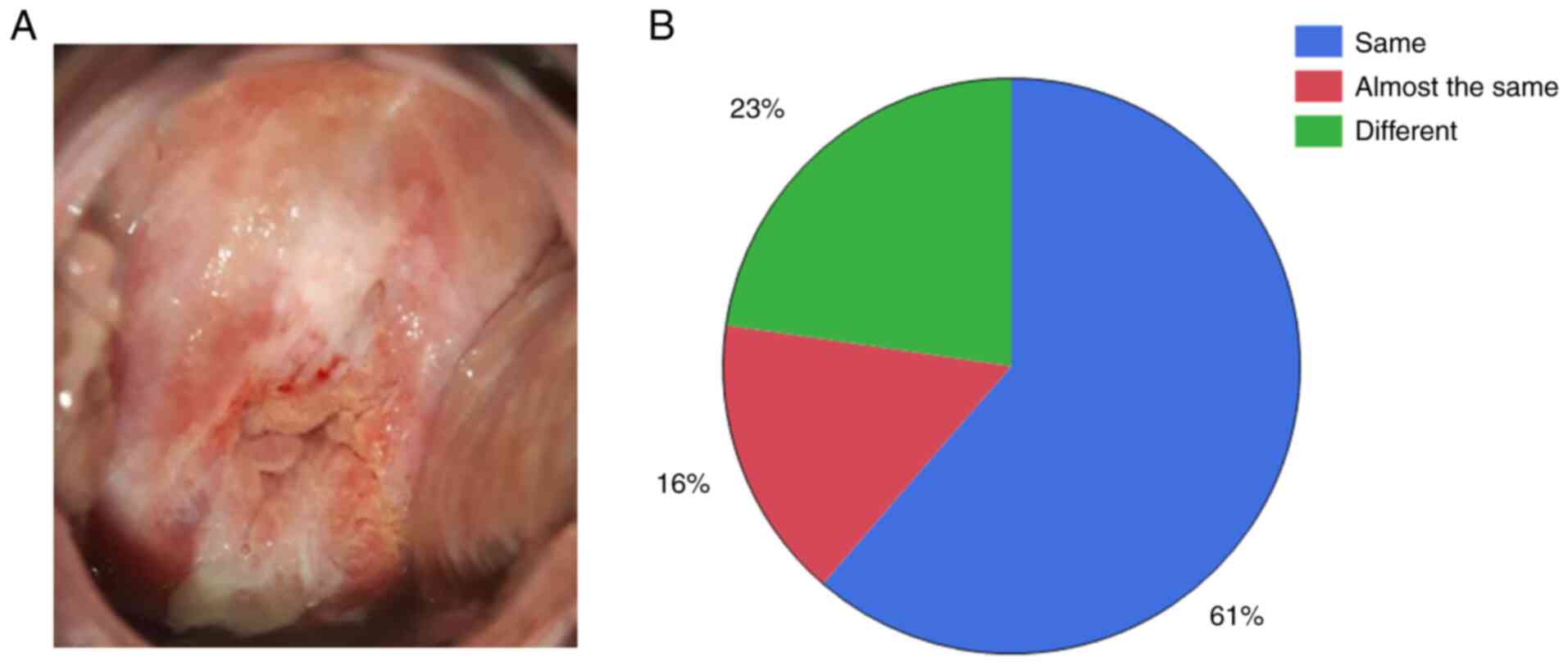
A representative image from digital colposcopy is
shown in Fig. 2A. The match rates
of the actual and assumed biopsy sites (Fig. 2B) were ‘same’ 61%, ‘almost the same’
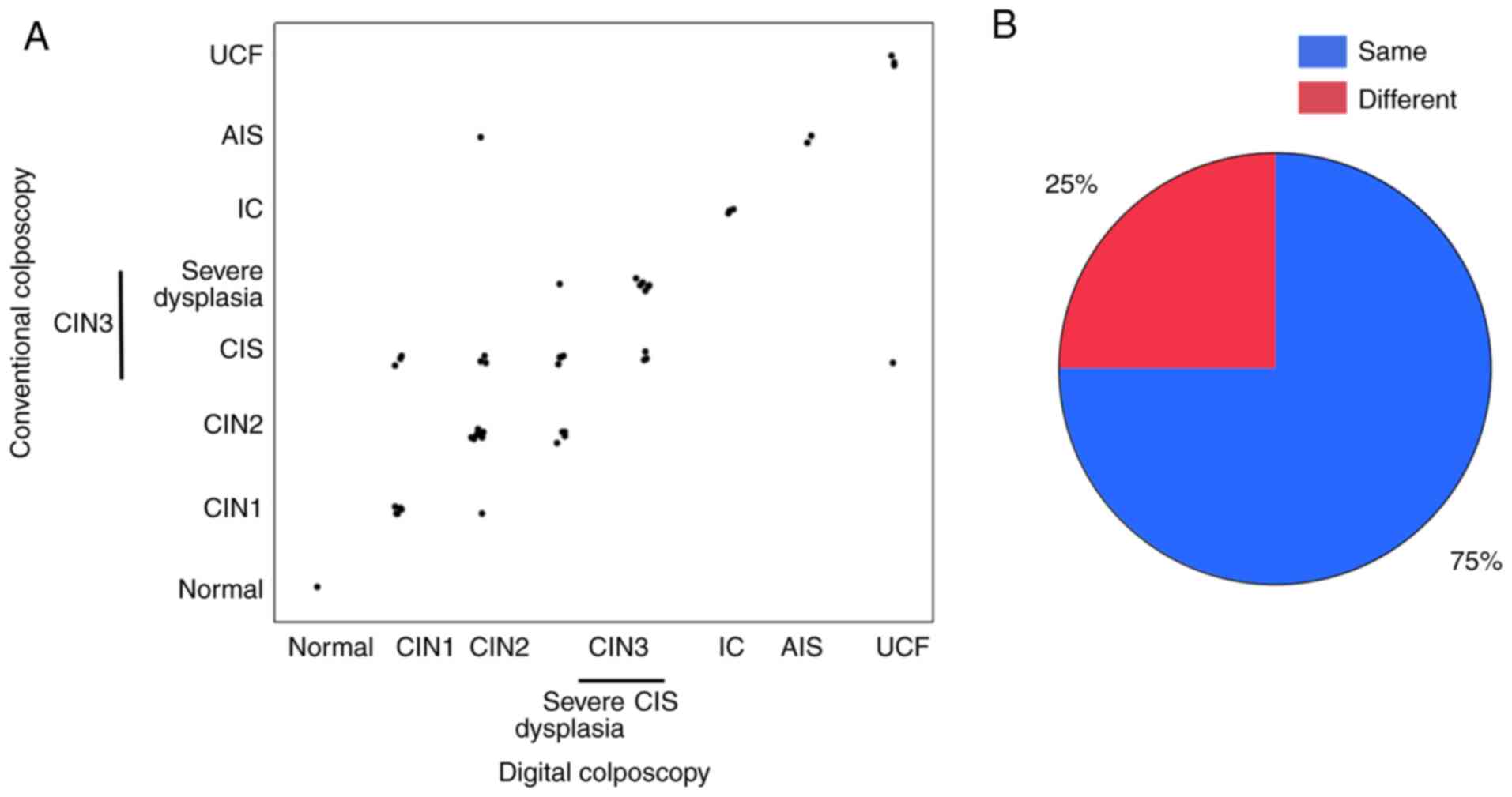
16%, and ‘different’ 23%. A comparison of diagnoses using
conventional and mobile digital colposcopy (Fig. 3A) gave match rates for diagnoses
(Fig. 3B) of ‘same’ 75% and
‘different’ 25%. Cases with diagnoses from visual examination that
were ‘different’ in Fig. 3A are
shown in Table I. Sample size was
too small to carry out any statistical analysis such as chi-square
test. It seemed that diagnoses of conventional colposcopy were more
matched to pathological diagnoses than those of digital colposcopy
in ‘different’ populations, however, overall matched rates between
pathological diagnosis and colposcopy diagnosis were 55.7±6.9%
(conventional colposcopy) and 46.1±6.9% (digital colposcopy). And
there were no significant differences (t-test, P=0.33).
 | Table ICases in which the results were
‘different’. |
Table I
Cases in which the results were
‘different’.
| Age, years | Gravida, n | Para, n | Pathological
diagnosis | Conventional
colposcopy | Digital
colposcopy |
|---|
| 30 | 0 | 0 | CIN1 | CIN1 | CIN2 |
| 51 | 2 | 2 | Adenocarcinoma | CIN2 | CIN3 |
| 47 | 2 | 2 | CIN3 | CIN2 | CIN3 |
| 48 | 4 | 2 | CIN3 | CIN2 | CIN3 |
| 45 | 4 | 3 | CIN2 | CIN2 | CIN3 |
| 47 | 1 | 1 | CIN3 | CIN3 | CIN2 |
| 37 | 0 | 0 | CIN3 | CIN3 | CIN2 |
| 50 | 0 | 0 | CIN2 | CIN3 | CIN1 |
| 50 | 0 | 0 | CIN2 | CIN3 | CIN2 |
| 47 | 1 | 1 | CIN3 | CIN3 | UCF |
| 47 | 1 | 1 | CIN3 | CIN3 | CIN1 |
| 27 | 1 | 1 | CIN3 | CIN3 | CIN1 |
| 46 | 2 | 2 | AIS | AIS | CIN2 |
Discussion
Digital colposcopy built around a smartphone is
becoming common, and this has advantages for telemedicine and data
sharing by taking advantage of smartphone characteristics (10-12).
However, digital colposcopy itself is not approved in Japan. In
this study, we investigated the feasibility of mobile digital
colposcopy using a smartphone for visualization, image capture, and
management in Japanese patients undergoing cervical screening. To
our knowledge, this is the first such study in a Japanese
population.
As shown in Figs. 2
and 3, the results from ≥75% of
cases were equivalent between mobile digital colposcopy and
conventional colposcopy. There is a study in Japan that reported
the possibility of using smartphones to perform colposcopy, and our
results are consistent with the report (14). The mobile digital colposcope used in
this study has been approved by the Food and Drug Administration
(FDA) and is in use in a number of Western countries (10-12).
These suggest that mobile digital colposcopy was not inferior to
conventional colposcopy even in Japanese population.
Our institution is a comprehensive cancer center,
which is why most of the patients required a treatment intervention
for HSIL or more (Fig. 1). As such,
there could be a selection bias in patient enrollment. In addition,
we seldom perform HPV testing because it does not always contribute
to the decision for the treatment.
Another limitation is that the study included only a
limited number of cases, and further validation at multiple centers
is required.
Cases in which the results were ‘different’ in
diagnosis were shown in Table I.
Pathological CIN3 should not be recognized as CIN2 by colposcopy,
because treatment may be delayed. As mentioned in the Results,
overall matched rates between pathological diagnosis and colposcopy
diagnosis were 55.7±6.9% (conventional colposcopy) and 46.1±6.9%
(digital colposcopy). And there were no significant differences
(t-test, P=0.33). These data suggested that digital colposcopy was
not inferior to conventional colposcopy as a screening examination.
Still, our primary focus was not to compare the pathological
diagnosis and the diagnosis from digital colposcopy, but rather to
compare the visual findings from conventional 3D colposcopy and
mobile digital colposcopy. The study protocol was that in the
examination using conventional colposcopy the clinician could
adjust their view of the cervix and could also observe the lesion
through the period, whereas only one image was captured by mobile
digital colposcopy. Capture of additional images may have resulted
in an even higher correlation rate.
Although the higher resolution of conventional
colposcopy was helpful in observing the lesion in detail, we
concluded that digital colposcopy was not inferior to conventional
colposcopy as a screening test, and that this method provides
sufficient details for judging the biopsy site or diagnosis using
acetic acid processing. We further speculate that digitally
captured images of the cervix can be used to train a machine
learning algorithm. Indeed, we previously reported the possibility
of deep learning application to colposcopy, using an image of only
150x150 pixels (13). This
resolution can easily be achieved by a mobile digital colposcope
incorporating a smartphone. Therefore, we hope this form of digital
colposcopy can be applied to clinical practice and data collection
in multiple centers.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
MS, DS, KF and KH designed the study. MS and DS
analyzed the patient data and were major contributors in writing
the manuscript. MS, DS, MH, SS and MM acquired the patient data.
AO, AY, AK and HY interpreted the data. MS, DS, KF and KH confirm
the authenticity of all the raw data. All authors read and approved
the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Institutional Review
Board of Saitama Medical University International Medical Center
(approval no. 19-026; 12/Jun/2019; Hidaka, Japan). Written informed
consent was obtained from all subjects.
Patient consent for publication
Written informed consent for publication from each
patient was obtained.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Cohen PA, Jhingran A, Oaknin A and Denny
L: Cervical cancer. Lancet. 393:169–182. 2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Cook DA, Smith LW, Law J, Mei W, van
Niekerk DJ, Ceballos K, Gondara L, Franco EL, Coldman AJ, Ogilvie
GS, et al: Aptima HPV Assay versus Hybrid Capture(®) 2
HPV test for primary cervical cancer screening in the HPV FOCAL
trial. J Clin Virol. 87:23–29. 2017.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Coste J, Cochand-Priollet B, de Cremoux P,
Le Galès C, Cartier I, Molinié V, Labbé S, Vacher-Lavenu MC and
Vielh P: French Society of Clinical Cytology Study Group. Cross
sectional study of conventional cervical smear, monolayer cytology,
and human papillomavirus DNA testing for cervical cancer screening.
BMJ. 326(733)2003.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Ginsburg O, Bray F, Coleman MP, Vanderpuye
V, Eniu A, Kotha SR, Sarker M, Huong TT, Allemani C, Dvaladze A, et
al: The global burden of women's cancers: A grand challenge in
global health. Lancet. 389:847–860. 2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Peirson L, Fitzpatrick-Lewis D, Ciliska D
and Warren R: Screening for cervical cancer: A systematic review
and meta-analysis. Syst Rev. 2(35)2013.PubMed/NCBI View Article : Google Scholar
|
|
6
|
García-Arteaga JD, Kybic J and Li W:
Automatic colposcopy video tissue classification using higher order
entropy-based image registration. Comput Biol Med. 41:960–970.
2011.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Khan MJ, Werner CL, Darragh TM, Guido RS,
Mathews C, Moscicki AB, Mitchell MM, Schiffman M, Wentzensen N,
Massad LS, et al: ASCCP Colposcopy Standards: Role of colposcopy,
benefits, potential harms, and terminology for colposcopic
practice. J Low Genit Tract Dis. 21:223–229. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
de Castro Hillmann E, Moreira Bacha O, Roy
M, Paris G, Berbiche D, Nizard V and Lopes Ramos JG: Cervical
digital photography: An alternative method to colposcopy. J Obstet
Gynaecol Can. 41:1099–1107. 2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Louwers JA, Kocken M, ter Harmsel WA and
Verheijen RH: Digital colposcopy: Ready for use? An overview of
literature. BJOG. 116:220–229. 2009.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Mink J and Peterson C: MobileODT: A case
study of a novel approach to an mHealth-based model of sustainable
impact. MHealth. 2(12)2016.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Thay S, Goldstein A, Goldstein LS, Govind
V, Lim K and Seang C: Prospective cohort study examining cervical
cancer screening methods in HIV-positive and HIV-negative Cambodian
Women: A comparison of human papilloma virus testing, visualization
with acetic acid and digital colposcopy. BMJ Open.
9(e026887)2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Xue Z, Novetsky AP, Einstein MH, Marcus
JZ, Befano B, Guo P, Demarco M, Wentzensen N, Long LR, Schiffman M
and Antani S: A demonstration of automated visual evaluation of
cervical images taken with a smartphone camera. Int J Cancer.
147:2416–2423. 2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Sato M, Horie K, Hara A, Miyamoto Y,
Kurihara K, Tomio K and Yokota H: Application of deep learning to
the classification of images from colposcopy. Oncol Lett.
15:3518–3523. 2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Tanaka Y, Ueda Y, Okazawa A, Kakuda M,
Matsuzaki S, Kobayashi E, Yoshino K and Kimura T: ‘Smartscopy’ as
an alternative device for cervical cancer screening: A pilot study.
BMJ Innov. 3:123–126. 2017.PubMed/NCBI View Article : Google Scholar
|