Introduction
Adrenal neuroblastoma (NB) is a tumor of the
autonomic nervous system originating from primordial neural crest
cells. The occurrence of NB is common in children but very rare in
adults, and the clinical manifestations are non-specific (1). NB is highly malignant, usually
characterized by invasive growth and propensity for organ
metastasis. Compared with pediatric patients, the prognosis of
adult patients with NB is poor (2). The most common primary site in adult
patients (aged 18-60 years) is the central nervous system (39%),
followed by the retroperitoneum (17%). The most common
manifestations of adrenal NB in adults are the presence of an
abdominal mass, abdominal pain, or other clinical manifestations
caused by tumor growth and metastasis, such as spinal cord
compression and hypertension (3).
Case report
In June 2016, a 40-year-old female patient was
admitted to the Affiliated Hospital of Guizhou Medical University
(Guiyang, China) with complaints of intermittent lower left back
pain and progressive pain in the lower right abdomen for >3
months. The patient had a history of nephrolithiasis for 10 years
and rheumatoid arthritis for 1 year, for which she received no
treatment. On admission, the patient had a height of 160 cm, a
weight of 70 kg and a blood pressure of 127/96 mmHg. No obvious
abnormalities were identified on physical examination. Urine
analysis showed hematuria. No abnormality was identified in the
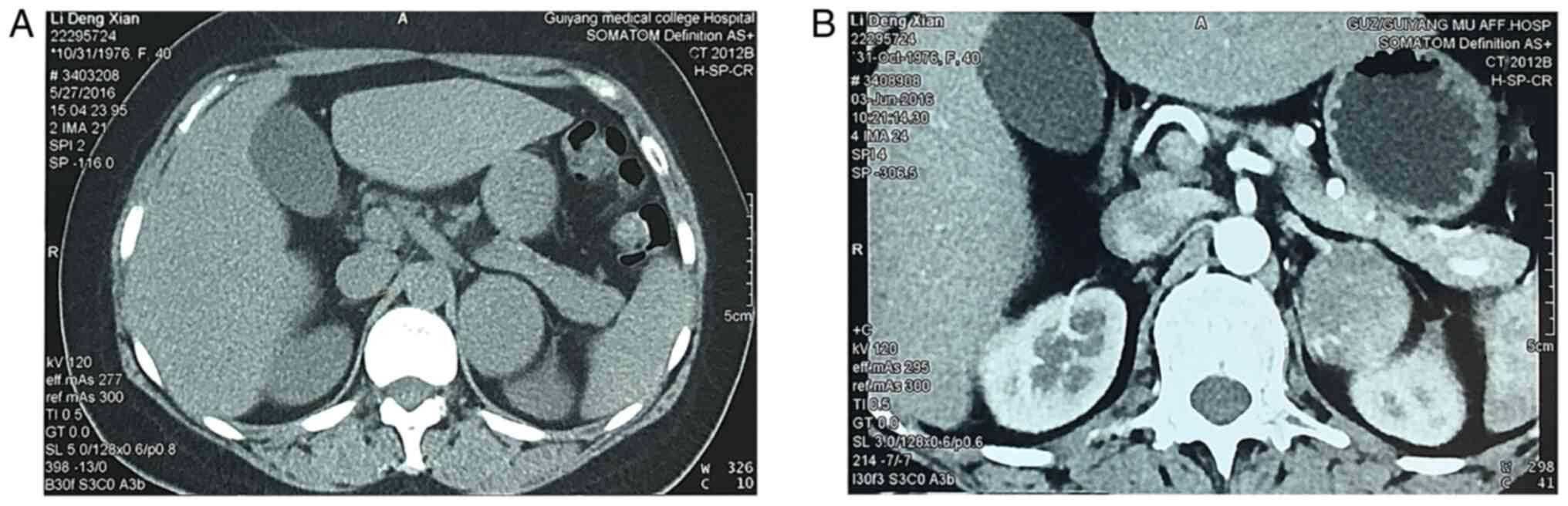
remaining laboratory tests. Computed tomography (CT) examination
(Fig. 1A and B) revealed the presence of a neoplastic
lesion in the left suprarenal gland, sized ~5.3x5.0x4.3 cm.
Following discussion with the patient and her family, laparoscopic
radical tumor resection was recommended. The surgery was
successful. Intraoperatively, the adrenal tumor was found to be
surrounded by an adipose tissue capsule and it was mobile. Finally,
the tumor was completely removed and sent to the Department of
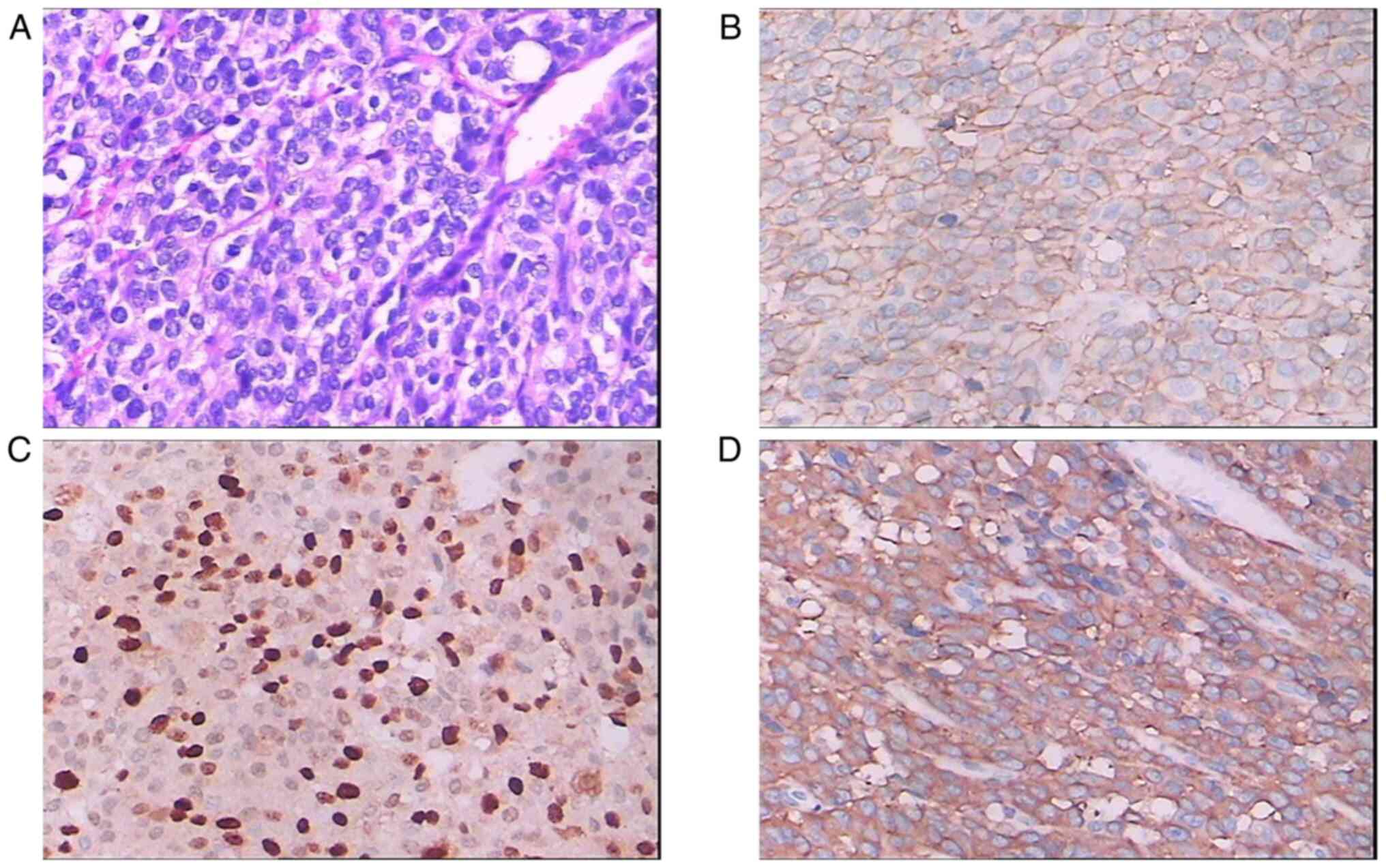
Pathology. The results of the pathological examination of the
surgical specimen (Fig. 2A-D)
included the following: H&E staining of the tumor revealed
round cells of different sizes, with little cytoplasm, deep
staining and diffuse nuclear distribution, as well as a small
number of lymphocytes in the fibrous stroma; in addition, the
cancer cells were arranged in nest-like solid sheets.
Immunohistochemical examination revealed that the tumor cells were
positive for synaptophysin, CD56, CD99 and chromogranin A,
partially positive for S-100 and Ki-67 (80%), and negative for
other markers, such as leukocyte common antigen, cytokeratin 5/6
and P63.
The final diagnosis was adrenal NB. Due to personal
and family-related issues, the patient did not undergo further
antitumor therapy, such as radiotherapy or chemotherapy. There were
no obvious abnormalities on imaging and laboratory examinations at
the 3-month postoperative follow-up, and no tumor recurrence was
observed on imaging examination at the 1-year postoperative
follow-up. However, a repeat CT at the 3-year postoperative
follow-up revealed pulmonary metastasis. The patient refused
chemotherapy and targeted therapy, and finally succumbed to the
disease within 1 month.
Discussion
Adrenal NB in adults is rare, and imaging plays an
important role in the diagnosis, staging, curative effect
evaluation and long-term follow-up of patients with NB (4). On CT examination, NB manifests as a
round cystic, solid, or irregular solid mass with uneven density,
necrotic areas and patchy calcification in the center, with
vascular entrapment and vasodilation in or around the tumor
(5). The typical manifestations of
NB on magnetic resonance imaging (MRI) examination include
calcification, necrosis, hemorrhage and cystic degeneration. In a
previous study, MRI revealed inhomogeneous signal intensity, low
signal intensity on T2-weighted imaging (T2WI) and high signal
intensity on T2WI (6).
Metaiodobenzylguanidine (MIBG) enters cells through the
norepinephrine transporter (7),
providing a sensitive and specific method of evaluating cartilage
and bone tumors. NBs produce catecholamine metabolites, which can
be used for the biological diagnosis of NB. The abnormal level of
catecholamines secreted by NB can be detected by examining the
levels of plasma epinephrine and norepinephrine (8); However, as this test lacks
specificity, it should be limited to cases with unclear symptoms
and should not be used for routine screening (9). The definitive diagnosis of NB
ultimately depends on histopathological and immunohistochemical
examination.
The International Neuroblastoma Risk Group (INRG)
staging system (10) has been
developed for statistical and clinical risk stratification of
different subgroups of patients with NB. The classification is
based on age at the time of diagnosis, INRG tumor stage,
histological classification, tumor differentiation, DNA ploidy,
MYCN oncogene locus and copy number status of chromosome 11q. In
the INRG staging system, the degree of local disease is determined
by the presence of image-defined risk factors (L1 and L2,
respectively), whereas Phase M is used for widely spread disease.
According to the 5-year event-free survival (EFS), Patients with
5-year EFS >85%, >75% to ≤85%, >50% to ≤75%, or <50%
were classified as very low, low, intermediate, or high risk,
respectively. The INRG classification system greatly promotes the
comparison of risk-based clinical trials conducted in different
parts of the world and the development of international
collaborative research (10).
There is currently no unified standard for the
treatment of adult NB. In the present case, laparoscopic resection
of the tumor was performed, but no adjuvant chemotherapy or
radiotherapy were administered postoperatively. Laparoscopic
surgery has the advantages of less trauma and quick recovery after
surgery, which is superior to traditional laparotomy (11). Owing to the rarity of adult NB,
there is a lack of chemotherapeutic drugs for standard treatment;
however, radiotherapy is recommended if the disease progresses
after surgery and chemotherapy. For high-risk patients, active
comprehensive treatment, including surgical resection, high-dose
chemotherapy combined with stem cell rescue, radiotherapy and
biological/immunotherapy can improve patient prognosis (12). In a Memorial-Sloan Kettering
retrospective study of 30 patients with advanced NB, >50% of the
patients were treated with high-dose induction chemotherapy after
surgery to achieve optimal results (13). Surgical resection is the main
treatment for low-risk patients. Alternative combination
chemotherapy includes cyclophosphamide, carboplatin, cisplatin,
etoposide, teniposide and doxorubicin (14). Compared with cisplatin alone, the
biological coupling of cobalt sulfur nanoparticles and cisplatin
led to a 57-78% reduction in NB cell proliferation (15). It has been demonstrated that the
anaplastic lymphoma kinase (ALK) gene is associated with NB
susceptibility, and that changes in MYCN gene status may also lead
to changes in ALK (16). ALK
mutations in patients with NB indicate a poor prognosis and are
accompanied by a corresponding invasive phenotype (16). Therefore, ALK is considered to be
an important oncogene in NB and a target for targeted therapy
(17). A retrospective study
demonstrated that the majority of adult NBs lacked MYCN
amplification (18).
The prognosis of NB originating from the adrenal
glands is poor, while that of NB originating from the thoracic
vertebrae is more favorable, with an overall survival rate 38%
higher compared with that of adrenal NB (19), which may be due to the lower risk
of metastatic spread, non-amplification of the MYCN oncogene and
overall favorable molecular biological characteristics. Metastasis
is the most important factor in determining the prognosis of
patients with NB. If recurrence or progression is suspected,
comprehensive evaluation should be made in combination with CT,
MRI, 123I-MIBG scintigraphy and positron emission
tomography-CT scans (20). The
prognosis of patients with NB aged >18 months with MYCN
amplification, 1p deletion and 17q increase is poor. Preventing and
reducing metastasis is the main clinical challenge in the treatment
of NB (21).
The results of Wevers et al (22) showed that the high-throughput plate
microfluidic model of the human blood-brain barrier may be used for
drug screening. Due to the expression of human transferrin receptor
on brain endothelial cells and the potential to support
receptor-mediated transcellular interaction, it is of particular
significance in drug targeted therapy. Identifying feasible
therapeutic targets is a major challenge in the treatment of adult
NB. Drug discovery is a complex and multidisciplinary process.
Efficient and high-throughput screening can be used to investigate
hundreds of thousands of compounds every day, which can greatly
reduce the cost and time of researchers (23). In recent years, some studies have
shown that the microfluidic brain microvascular chip device can
directionally control cell proliferation under conditions of
unidirectional flow. These cell systems exist in the vascular beds
of surrounding tissues, such as kidneys or lungs, and verify the
barrier function of our brain microvascular chips by measuring the
permeability of fluorescent dextran and human monoclonal antibodies
to further study the molecular transport mechanism of
fluorescence-labeled biological products, viruses or nanoparticles
across cells (24). At present,
organic compounds in the human brain can be used to simulate the
modeling, downstream analysis and application of various diseases.
Human brain organic compounds provide a platform for studying the
effects of substance or drug abuse on the central nervous system.
The brain organic compounds of patients can be implanted with high
throughput to test a large number of drugs and identify the most
beneficial drugs for patients, which provides a new idea for the
treatment of adrenal diseases, such as adrenal NB in adults
(25).
In conclusion, adrenal NB in adults is clinically
rare and highly malignant. Preoperative staging, surgical resection
and postoperative adjuvant therapy can help prolong patient
survival. When there is suspicion of adult NB, the feasibility of
surgical treatment should be comprehensively evaluated in
combination with imaging, laboratory and pathological examinations,
in order to avoid a missed diagnosis or misdiagnosis.
Acknowledgements
Not applicable.
Funding
The present study was supported by the National Natural Science
Foundation of China (grant no. 81660263) and Doctoral Fund of
Affiliated Hospital of Guiyang Medical College, (Guiyang, Guizhou,
China; grant no. C-2012-6).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
KT contributed to the concept and design of the
article; KT, SX, WZ and BC participated in the operation; SX wrote
the first draft of the article; KC and YM obtained the raw data of
outpatients, such as laboratory and imaging examinations,
preliminary examination of patients, and participated in the
diagnosis and treatment of patients. JZ and JH provided
postoperative pathological results, research direction and
concepts, and provided help for the diagnosis and treatment of
patients. PL and DL critically revised the manuscript as regards to
the content and design of the study. All the authors confirmed the
authenticity of the data.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of the Affiliated Hospital of Guizhou Medical University.
The patient provided written informed consent.
Patient consent for publication
The patient consented to the publication of the case
details and any associated images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Zhang H and Feng Z: Adrenal neuroblastoma
in an elderly adult: A case report and review of the literature. J
Med Case Rep. 13(284)2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Bosse KR and Maris JM: Advances in the
translational genomics of neuroblastoma: From improving risk
stratification and revealing novel biology to identifying
actionable genomic alterations. Cancer. 122:20–33. 2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Conter HJ, Gopalakrishnan V, Ravi V, Ater
JL, Patel S and Araujo DM: Adult versus pediatric neuroblastoma:
The M.D. Anderson cancer center experience. Sarcoma.
2014(375151)2014.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Bar-Sever Z, Biassoni L, Shulkin B, Kong
G, Hofman MS, Lopci E, Manea I, Koziorowski J, Castellani R,
Boubaker A, et al: Guidelines on nuclear medicine imaging in
neuroblastoma. Eur J Nucl Med Mol Imaging. 45:2009–2024.
2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Zhuang B, Lv DK, Gao SJ and Meng JJ:
Differential diagnosis of CT images in children with neuroblastomas
and ganglioneuroblastomas. Asian Pac J Cancer Prev. 15:10509–10512.
2014.PubMed/NCBI View Article : Google Scholar
|
|
6
|
D'Amuri FV, Maestroni U, Pagnini F, Russo
U, Melani E, Ziglioli F, Negrini G, Cella S, Cappabianca S,
Reginelli A, et al: Magnetic resonance imaging of adrenal gland:
State of the art. Gland Surg. 8 (Suppl 3):S223–S232.
2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Simon T: Neuroblastoma. Urologe. A
44:543–554, 555. 2005.PubMed/NCBI View Article : Google Scholar : (In German).
|
|
8
|
Candito M, Billaud E, Chauffert M,
Cottet-Emard JM, Desmoulin D, Garnier JP, Greffe J, Hirth C, Jacob
N, Millot F, et al: Biochemical diagnosis of pheochromocytoma and
neuroblastomas. Ann Biol Clin (Paris). 60:15–36. 2002.PubMed/NCBI(In French).
|
|
9
|
Leung FY and Griffiths J: Use of plasma
catecholamine values in diagnosing pheochromocytoma and
neuroblastoma. Can Med Assoc J. 111:1321–1322. 1974.PubMed/NCBI
|
|
10
|
Cohn SL, Pearson AD, London WB, Monclair
T, Ambros PF, Brodeur GM, Faldum A, Hero B, Iehara T, Machin D, et
al: The international neuroblastoma risk group (INRG)
classification system: An INRG task force report. J Clin Oncol.
27:289–297. 2009.PubMed/NCBI View Article : Google Scholar
|
|
11
|
International Pediatric Endosurgery Group.
IPEG guidelines for the surgical treatment of adrenal masses in
children. J Laparoendosc Adv Surg Tech A. 20:vii–ix.
2010.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Rogowitz E, Babiker HM, Kanaan M, Millius
RA, Ringenberg QS and Bishop M: Neuroblastoma of the elderly, an
oncologist's nightmare: Case presentation, literature review and
SEER database analysis. Exp Hematol Oncol. 3(20)2014.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Kushner BH, Kramer K, LaQuaglia MP, Modak
S and Cheung NK: Neuroblastoma in adolescents and adults: The
memorial sloan-kettering experience. Med Pediatr Oncol. 41:508–515.
2003.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Yalçin B, Kremer LC, Caron HN and van
Dalen EC: High-dose chemotherapy and autologous haematopoietic stem
cell rescue for children with high-risk neuroblastoma. Cochrane
Database Syst Rev: Oct 5, 2013 (Epub ahead of print). doi:
10.1002/14651858.CD006301.pub4.
|
|
15
|
Ertugrul MS, Nadaroglu H, Nalci OB,
Hacimuftuoglu A and Alayli A: Preparation of CoS
nanoparticles-cisplatin bio-conjugates and investigation of their
effects on SH-SY5Y neuroblastoma cell line. Cytotechnology.
72:885–896. 2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Janoueix-Lerosey I, Lequin D, Brugières L,
Ribeiro A, de Pontual L, Combaret V, Raynal V, Puisieux A,
Schleiermacher G, Pierron G, et al: Somatic and germline activating
mutations of the ALK kinase receptor in neuroblastoma. Nature.
455:967–970. 2008.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Holzhauser S, Lukoseviciute M,
Papachristofi C, Vasilopoulou C, Herold N, Wickström M, Kostopoulou
ON and Dalianis T: Effects of PI3K and FGFR inhibitors alone and in
combination, and with/without cytostatics in childhood
neuroblastoma cell lines. Int J Oncol. 58:211–225. 2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Podda MG, Luksch R, Polastri D, Gandola L,
Piva L, Collini P, Cefalo G, Terenziani M, Ferrari A, Casanova M,
et al: Neuroblastoma in patients over 12 years old: A 20-year
experience at the istituto nazionale tumori of milan. Tumori.
96:684–689. 2010.PubMed/NCBI
|
|
19
|
Salim A, Raitio A, Pizer B, Mullassery D
and Losty PD: Neuroblastoma: The association of anatomical tumour
site, molecular biology and patient outcomes. ANZ J Surg.
91:1000–1004. 2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Simon T, Hero B, Schulte JH, Deubzer H,
Hundsdoerfer P, von Schweinitz D, Fuchs J, Schmidt M, Prasad V,
Krug B, et al: 2017 GPOH Guidelines for diagnosis and treatment of
patients with neuroblastic tumors. Klin Padiatr. 229:147–167.
2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Bhoopathi P, Pradhan AK, Bacolod MD, Emdad
L, Sarkar D, Das SK and Fisher PB: Regulation of neuroblastoma
migration, invasion, and in vivo metastasis by genetic and
pharmacological manipulation of MDA-9/Syntenin. Oncogene.
38:6781–6793. 2019.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Wevers NR, Kasi DG, Gray T, Wilschut KJ,
Smith B, van Vught R, Shimizu F, Sano Y, Kanda T, Marsh G, et al: A
perfused human blood-brain barrier on-a-chip for high-throughput
assessment of barrier function and antibody transport. Fluids
Barriers CNS. 15(23)2018.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Aldewachi H, Al-Zidan RN, Conner MT and
Salman MM: High-Throughput screening platforms in the discovery of
novel drugs for neurodegenerative diseases. Bioengineering (Basel).
8(30)2021.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Salman MM, Marsh G, Kusters I, Delincé M,
Di Caprio G, Upadhyayula S, de Nola G, Hunt R, Ohashi KG, Gray T,
et al: Design and validation of a human brain endothelial
Microvessel-on-a-Chip open microfluidic model enabling advanced
optical imaging. Front Bioeng Biotechnol. 8(573775)2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Wang H: Modeling neurological diseases
with human brain organoids. Front Synaptic Neurosci.
10(15)2018.PubMed/NCBI View Article : Google Scholar
|