Introduction
Cervical cancer is the second-most common malignant
tumor in females globally and one of the leading causes of
cancer-associated mortality (1).
In 2018, with an estimated 570,000 cases and 311,000 deaths,
cervical cancer ranked the fourth most frequently diagnosed cancer
and the fourth leading cause of cancer-associated death in females
worldwide (2). Radical
hysterectomy and lymphadenectomy are standard procedures in radical
surgery for cervical cancer. A lymphocele is a common complication
following radical hysterectomy and pelvic lymph node dissection.
The incidence ranges from 1-58%. A lymphocele is a cystic mass that
may occur in the retroperitoneum after pelvic lymphadenectomy.
Lymphoceles may be the cause of severe morbidity, or even mortality
in rare cases. In most patients affected, lymphoceles are
asymptomatic, while symptomatic lymphoceles manifest with pain due
to compression of adjacent structures, lymphoedema, deep vein
thrombosis or inflammation (3).
At our department, a patient who underwent pelvic
surgery presented with discomfort due to vaginal discharge. The
patient had a rare presentation of fistula formation between a
pelvic lymphocele and the vaginal stump. The present study reported
on the successful treatment of this patient and provided a review
of the pertinent literature. In the present article, the
feasibility and result of lymphatic embolization after radical
hysterectomy and sentinel pelvic lymph node biopsy were
demonstrated.
Case report
The patient was a 49-year-old female who presented
at the Center for Gynecologic Cancer, National Cancer Center Korea
(Goyang, Republic of Korea) with a profuse vaginal discharge of ~2
l/day at 5 months postoperatively (complication date, April 2021).
The vaginal discharge was a clear, yellow-colored fluid without any
admixture of blood. The patient had no symptoms other than vaginal
discharge. On physical examination, the vaginal mucosa appeared
normal.
The patient had undergone a robot-assisted radical
hysterectomy, bilateral adnexectomy and sentinel pelvic lymph node
biopsy for invasive squamous cell carcinoma of the cervix
(International Federation of Gynecology and Obstetrics stage IB1) 5
months previously. After cervical injection of indocyanine green,
sentinel lymph nodes (SLNs) were bilaterally identified among the
pelvic lymph nodes. No tumor was identified on the frozen sections
of the five left-sided pelvic lymph nodes and one right-sided
pelvic lymph node (Fig. 1). After
radical hysterectomy and sentinel pelvic lymph node biopsy,
retroperitonealization (closure of the peritoneum) was performed.
After hysterectomy, the vaginal stump was sutured and the
peritoneum on the bladder side (anterior side) and peritoneum on
the rectum (posterior side) were then sutured. Sutures were
performed on both sides in the direction of the incised round
ligament. The patient's postoperative course was uneventful and the
patient was discharged on postoperative day 2. Histopathological
examination revealed a 1.8-cm invasive squamous cell carcinoma.
There were no other risk factors, such as lymphovascular space
invasion, parametrial invasion, surgical margin or lymph node
complications.
As an initial investigation, the creatinine level of
the vaginal discharge was evaluated and was determined to be normal
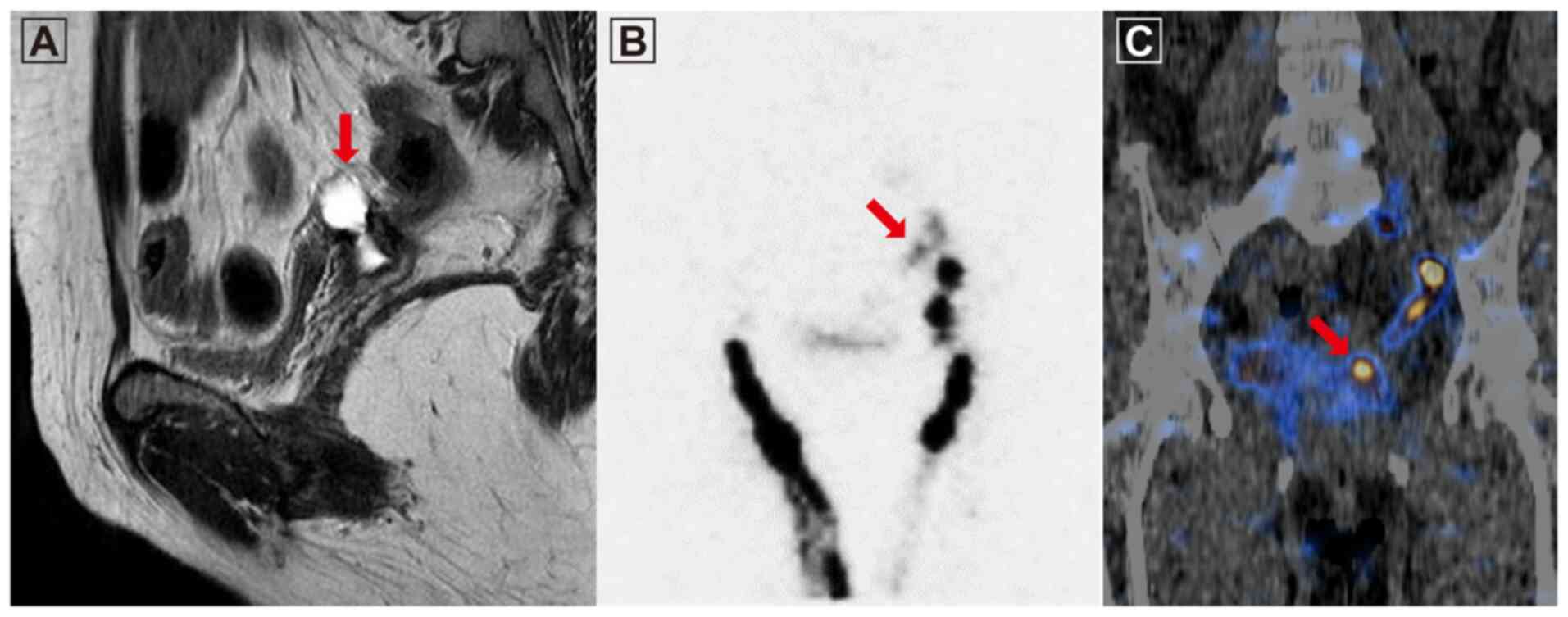
(0.51 mg/dl). Pelvic MRI revealed a 2.5x1.2 cm-sized cystic lesion
in the left superior region of the vaginal stump (Fig. 2A). Lymphoscintigraphy was performed
using technetium-99m-labeled phytate (4mCi) to determine whether a
fistulous connection between the pelvic lymphocele and the vaginal
stump was present. A radiopharmaceutical compound was injected into
the interphalangeal webs of both feet and the suspected route of
lymph flow to the vaginal lumen via the lymphocele was observed in
a planar image 10 min after the injection (Fig. 2B). Single photon emission CT/CT
identified radioactivity extending from the pelvic lymphocele to
the vaginal stump, followed by dynamic flow (Fig. 2C).
Lymphangiography was performed by accessing the
inguinal lymph nodes on both sides. Contrast enhancement of the
lymphatic ducts along the iliac chains on both sides occurred at a
slow rate. The contrast medium was observed to slowly leak from the
left iliac chain to the pelvic cavity after >1 h. The epithelial
layer was not intact according to the
lymphangiography/lymphoscintigraphy images (Video S1); therefore, it was not possible
to perform percutaneous catheter drainage (PCD) or sclerotherapy.
The leaking lymphatic vessels were embolized using coils and a
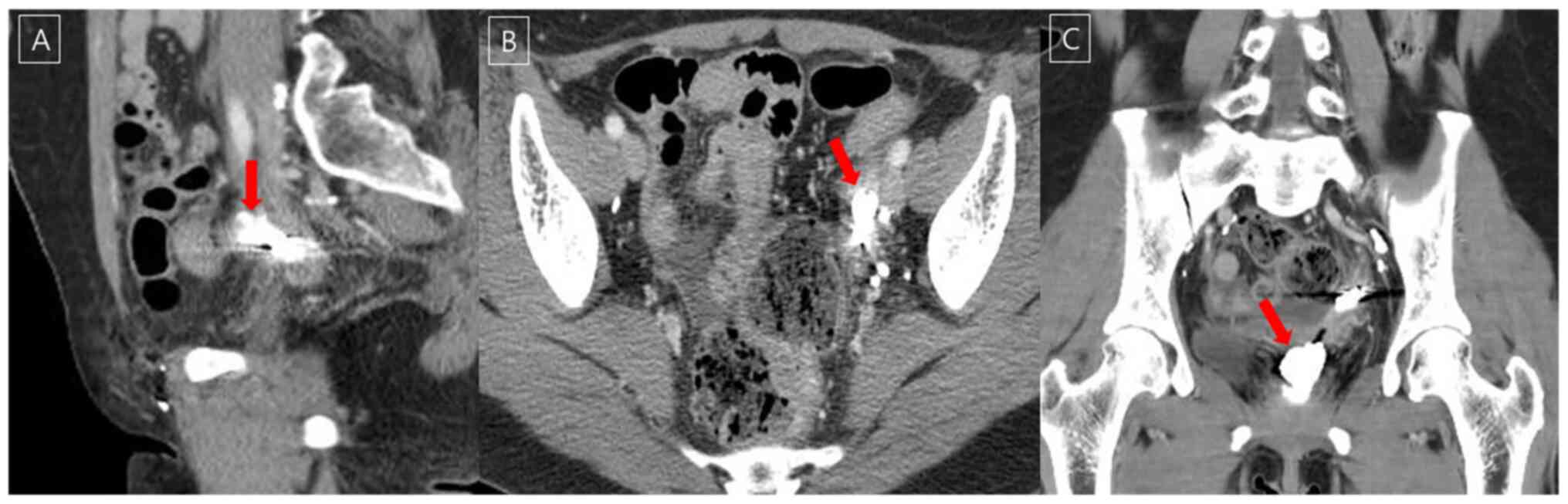
glue/lipiodol mix at a ratio of 1:2 (Fig. 3). After embolization, no further
discharge was observed from the vagina. The patient is currently
being followed up and is doing well without any notable side
effects. At three months after lymphatic embolization, a CT scan
revealed decreased fluid collection above the vaginal stump to the
left, communicating with the vagina (Fig. 4).
Discussion
A pelvic lymphocele is a collection of lymph with a
thick fibrotic wall but without any epithelial lining. Lymphoceles
are usually associated with extensive lymph node dissection
(4). However, the patient of the
present study developed a complicated pelvic lymphocele that
communicated with the vaginal stump following sentinel pelvic lymph
node biopsy. Even though the incidence of a lymphocele does not
increase depending on the mode of peritoneal closure, in the case
of the present study, retroperitonealization may have been an
additional risk factor for the development of a pelvic lymphocele
and a fistula to the vaginal stump due to the increased regional
pressure (5). Kadanali et
al (6) reported that an
unreconstructed peritoneum may reduce the incidence of adhesion.
Currently, it remains elusive whether retroperitonealization after
pelvic lymphadenectomy is beneficial (7).
Symptomatic lymphoceles typically occur due to
compression of the surrounding anatomic structures, resulting in
pelvic pain, leg edema, gastrointestinal obstruction, obstructive
uropathy and deep vein thrombosis. Furthermore, severe and
potentially life-threatening complications, including sepsis,
chylous ascites, lymphatic fistula formation and pulmonary
thromboembolism, may occur (8).
SLN biopsy was introduced in the field of gynecologic oncology to
minimize these complications. Currently, there are no pertinent
reports on complications after sentinel pelvic lymph node biopsy.
To the best of our knowledge, the present study was the first to
report complications following SLN biopsy. Several studies have
indicated that SLN mapping in early-stage cervical cancer patients
are feasible with excellent detection rates and sensitivity
(9,10). Although recent international
guidelines recommend performing SLN biopsy in addition to pelvic
lymph node dissection, SLN biopsy alone is not the gold standard
yet due to a lack of prospective evidence, particularly in terms of
long-term oncological safety. For the diagnosis of cervical cancer
stage I, a pelvic lymph node dissection other than SLN biopsy is
available. In the case of the present study, only SLN biopsy was
performed. There was no lesion suspicious of lymph node metastasis
in the preoperative MRI and there was no uptake on positron
emission tomography/CT. All SLN biopsy specimens, even those from
intraoperative frozen biopsy, were reported as negative. SLN was
performed according to the cervical cancer treatment guidelines
from the National Comprehensive Cancer Network (11). No other diagnostic method was
available.
The diagnosis of a lymphocele is based on imaging
findings. On MRI, lymphoceles appear as lobulated, hyperintense
structures on T2-weighted images with imperceptible walls and
negligible wall enhancement on postcontrast T1-weighted images.
There is no definitive consensus on the treatment of pelvic
lymphoceles. Conservative treatment is attempted first and
follow-up is performed using CT or ultrasonography to identify
lesion regression. Surgical marsupialization by open or
laparoscopic surgery or percutaneous catheter drainage are options
to manage pelvic lymphoceles (4).
In the last two decades, interventional radiology has become an
important strategy in the treatment of pelvic lymphoceles. PCD may
be combined with transcatheter ethanol sclerotherapy to augment the
therapeutic efficiency. PCD is an easy, safe and successful
treatment method in 80-90% of cases. However, it takes longer for
results to be achieved (10-20 days, as reported in the literature).
In addition, percutaneous techniques carry a risk for potential
infection (4,12-14).
Recently, lymphatic embolization using N-butyl cyanoacrylate glue
was performed to safely and effectively treat postoperative pelvic
lymphoceles, for which PCD is insufficient (15).
Among the aforementioned treatments, PCD and
sclerotherapy are relatively easy to perform. Lymphangiography is
able to determine how much radioactive material has been removed
from the injection site, how much has been absorbed into the
surrounding lymph nodes, whether there is a delay or blockage of
lymph drainage or whether dermal reflux occurs. Lymphangiography
and lymphatic embolization are invasive procedures including
incision or puncture and there are inherent risks such as
infection, pain and lipiodol extravasation during injection
(16). Even in the presence of
multiple leakage points, treatment is possible if the epithelial
layer of the cavity is adherent. However, patients with high-flow
leakages have a higher chance of recurrence, lowering the chance of
a cure as cavity adhesion slowly occurs. Since pedal
lymphoscintigraphy indicated that the epithelial layer was not
intact and that a lymphocele had not completely formed in the
present case, it would have been difficult to insert a percutaneous
catheter for drainage and/or attempt sclerotherapy. For successful
lymphatic embolization, leaking lymphatic vessels must be
obliterated. However, it was not possible to clearly localize the
point of leakage in the present case and a slow leak from the
external iliac chain was identified on lymphoscintigraphy and
lymphangiography. The larger lymph nodes around the leak may be
used for glue injection to achieve lymphatic obstruction. However,
no large lymph nodes were observed in the present case.
Alternatively, transvaginal lymphatic embolization was attempted
and performed successfully once.
In conclusion, transvaginal lymphatic embolization
is a rapid and reliable method that may be used to directly
visualize the tract (from the vaginal stump to the lesion in the
present case) prior to lymphatic blockage. The effect of treatment
may also be immediately confirmed.
Supplementary Material
Lymphangiography video images. The
video images indicated that contrast enhancement of the lymphatic
ducts along the iliac chains on both sides occurred at a slow rate.
The epithelial layer was not intact according to the
lymphangiography images.
Supplementary Data
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
requests.
Authors' contributions
YJL, IJL, SP, TSK and MCL were involved in the
conception and design of the current study. YJL wrote the
manuscript. IJL, SP, TSK and MCL supervised the study. YJL and MCL
confirm the authenticity of all the raw data. All authors have read
and approved the final version of the manuscript.
Ethics approval and consent to
participate
The Ethics Committee of National Cancer Center Korea
(Goyang, Korea) approved this case report. The patient provided
written informed consent.
Patient consent for publication
The patient provided informed consent for the
publication of her case including data and images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Mattiuzzi C and Lippi G: Cancer
statistics: A comparison between World health organization (WHO)
and global burden of disease (GBD). Eur J Public Health.
30:1026–1027. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Bray F, Ferlay J, Soerjomataram I, Siegel
RL, Torre LA and Jemal A: Global cancer statistics 2018: GLOBOCAN
estimates of incidence and mortality worldwide for 36 cancers in
185 countries. CA Cancer J Clin. 68:394–424. 2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Weinberger V, Cibula D and Zikan M:
Lymphocele: Prevalence and management in gynecological
malignancies. Expert Rev Anticancer Ther. 14:307–317.
2014.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Karcaaltincaba M and Akhan O: Radiologic
imaging and percutaneous treatment of pelvic lymphocele. Eur J
Radiol. 55:340–354. 2005.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Cheong YC, Bajekal N and Li TC: Peritoneal
closure-to close or not to close. Hum Reprod. 16:1548–1552.
2001.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Kadanali S, Erten O and Kucukozkan T:
Pelvic and periaortic pertioneal closure or non-closure at
lymphadenectomy in ovarian cancer: Effects on morbidity and
adhesion formation. Eur J Surg Oncol. 22:282–285. 1996.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ai W, Liang Z, Li F and Yu H: Internal
hernia beneath superior vesical artery after pelvic lymphadenectomy
for cervical cancer: A case report and literature review. BMC Surg.
20(312)2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Clarke-Pearson DL, Synan IS and Creasman
WT: Significant venous thromboembolism caused by pelvic
lymphocysts: Diagnosis and management. Gynecol Oncol. 13:136–143.
1982.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Cibula D and McCluggage WG: Sentinel lymph
node (SLN) concept in cervical cancer: Current limitations and
unanswered questions. Gynecol Oncol. 152:202–207. 2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Kim JH, Kim DY, Suh DS, Kim JH, Kim YM,
Kim YT and Nam JH: The efficacy of sentinel lymph node mapping with
indocyanine green in cervical cancer. World J Surg Oncol.
16(52)2018.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Abu-Rustum NR, Yashar CM, Bean S, Bradley
K, Campos SM, Chon HS, Chu C, Cohn D, Crispens MA, Damast S, et al:
NCCN guidelines insights: Cervical cancer, version 1.2020. J Natl
Compr Canc Netw. 18:660–666. 2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
vanSonnenberg E, Wittich GR, Casola G,
Wing VW, Halasz NA, Lee AS and Withers C: Lymphoceles: Imaging
characteristics and percutaneous management. Radiology.
161:593–596. 1986.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Aronowitz J and Kaplan AL: The management
of a pelvic lymphocele by the use of a percutaneous indwelling
catheter inserted with ultrasound guidance. Gynecol Oncol.
16:292–295. 1993.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Kim JK, Jeong YY, Kim YH, Kim YC, Kang HK
and Choi HS: Postoperative pelvic lymphocele: Treatment with simple
percutaneous catheter drainage. Radiology. 212:390–394.
1999.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Chu HH, Shin JH, Kim JW, Noh SY, Yang WJ
and Park S: Lymphangiography and lymphatic embolization for the
management of pelvic lymphocele after radical prostatectomy in
prostatic cancer. Cardiovasc Intervent Radiol. 42:873–879.
2019.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Lee EW, Shin JH, Ko HK, Park J, Kim SH and
Sung KB: Lymphangiography to treat postoperative lymphatic leakage:
A technical review. Korean J Radiol. 15:724–732. 2014.PubMed/NCBI View Article : Google Scholar
|