Introduction
Mixed tumour of the skin also known as chondroid
syringoma (CS) is a rare, mostly benign tumour categorized under
cutaneous adnexal neoplasms. These neoplasms exhibit morphologic
differentiation towards the primary adnexal structures found in
normal skin, including hair follicles, sebaceous glands and
apocrine and eccrine (sweat) glands (1). CS was first described by Billroth in
1859 as a tumor on the salivary glands, a few years later, Virchow
regarded the tumour as being identical to mesenchymal neoplasm and
called it ‘mixed tumor’. However, the first case of mixed tumor of
the skin was reported by Nasse in 1892 (2,3).
Several decades later in 1961, upon a review of 188 cases of mixed
tumour of the skin, the name ‘Chondroid syringoma’ was coined
(4). Although contested, the
Hirsch and Helwig (4) chondroid
terminology resulted from observation that the biggest number of
mostly scalp lesion cases had cartilaginous properties in the tumor
stroma (4,5). Other tumour locations, reportedly
demonstrate a myxoid stroma (5).
Moreover, several mixed tumour studies by Headington (6) and Hassab-el-Naby et al
(7) have demonstrated 2
morphologically distinct types of mixed tumours referred to as
apocrine-type cutaneous mixed tumor (AMT) and eccrine-type
cutaneous mixed tumor (EMT).
The incidence of CS is reportedly <0.36% of all
primary skin tumours (2). The
tumour affects mostly middle-aged men, and commonly found in
various sites of the head and neck region including the scalp,
nose, cheek and lips (2-4).
However, from professional literature more cases in the upper lips
have been described compared to the lower lips (5-26).
The clinical diagnosis of CS is mainly based on
pathology that demonstrates the epithelial and mesenchymal
components of CS. Histology shows the tubular and glandular
structures with one or two layers of epithelial cells-inner and
outer cells, in a fibrous or chondroid stroma (matrix). However,
the presence of minor salivary glands in the lower lip poses a
challenging CS diagnostic problem. Cutaneous adnexal tumours, such
as pleomorphic adenoma (PA) of the salivary gland exhibit similar
clinical and histopathological features and may localise in the
lower lip as well (27-29).
Further, there is a strong possibility of a close molecular level
relationship between CS and PA tumor types (30). The genetic or protein expression
profile of the 2 tumour types is not yet completely deciphered.
However, recent work has demonstrated that both tumours possess
similar chromosomal rearrangements involving genes such as the
fusion genes encoding pleomorphic adenoma gene 1 (PLAG1) zinc
finger protein and the high-mobility group AT-hook 2 (HMGA2)
protein (30,31). Notwithstanding, Russell-Goldman
et al (31) have recently
demonstrated that the mechanisms of expression of these genes could
be different for the AMT and EMT tumour types and suggested the
molecular relationship between CS and PA maybe limited to AMT
tumour type. Additionally, the immunohistochemistry (IHC) of CS
reveals a different protein marker expression profile for each of
the three cellular components-inner, outer and matrix. The inner
component expression profile includes inter alia
cytokeratins (CK), carcinoembryonic antigen (CEA) and epithelial
membrane antigen (EMA). However, the outer and matrix expression
profile includes vimentin, S100 protein, neuron-specific enolase,
glial fibrillary acidic protein or different types of actin, such
as the smooth muscle actin protein (SMA) (27,32).
The objective of this report is to document this
rare benign skin lesion of the lower lip in a 58-year-old man, and
promote clinical awareness, recapitulate the diagnostic challenges
and emphasise the importance of appropriate treatment and
prognostic evaluation.
Case report
Patient description
A 58-year-old Japanese man was referred to the
Department of Oral and Maxillofacial Surgery at the University of
the Ryukyus Hospital by a private practitioner in October 2019. The
patient complained of a slow-progressing, painless swelling in the
lower lip, which followed an accidental biting of the inside of the
lip in 2010. In addition, the patient had fears of anecdote
postoperative functional and aesthetic effects of surgery.
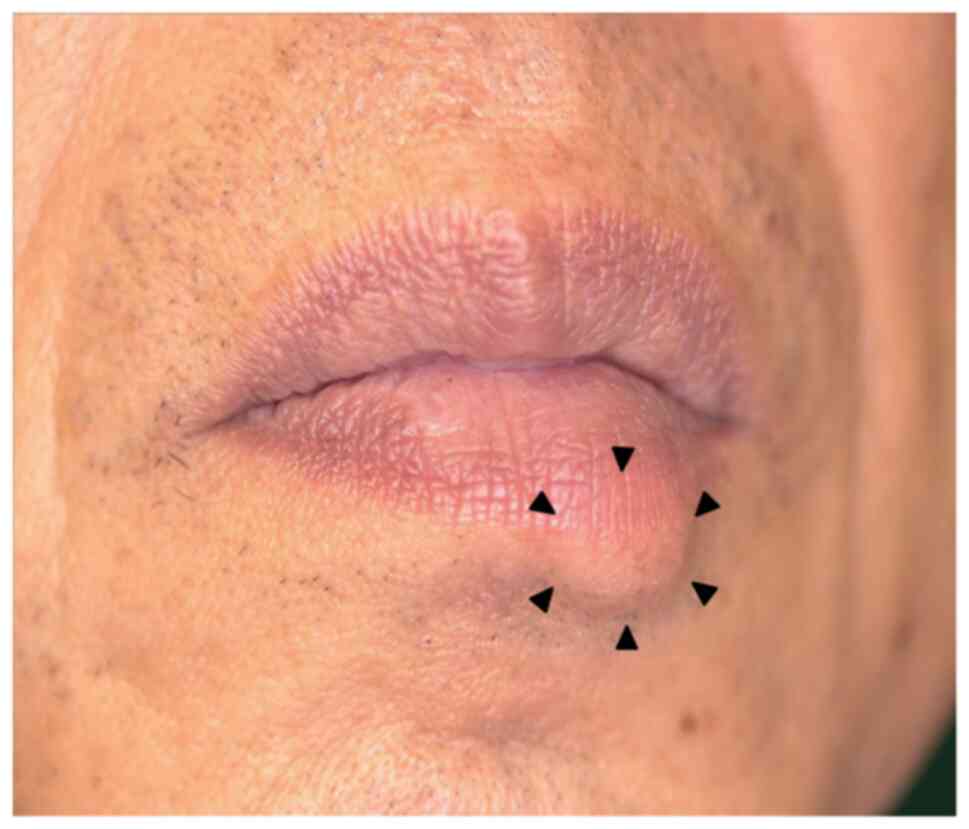
Physical examination revealed the patient was in
good general condition, with no pallor, oedema, jaundice or
cervical or generalised lymphadenopathy; and systemic examinations
were within normal limits. Intraoral examination was unremarkable;
however, a non-tender, slightly hard and mobile mass measuring
~11x11x7 mm3 in size was felt on palpating the left
lateral side of the lower lip (Fig.
1). The overlying mucocutaneous surface appeared normal and
smooth without evidence of ulceration.
Investigations
With differential diagnoses of epidermal or dermoid
cyst, neurofibroma and dermatofibroma, the patient underwent
radiological, routine haematological and pathological
investigations. Radiology involved ultrasonography (US) and
magnetic resonance imaging (MRI) of the lip and oral cavity
respectively. US was performed with an 18-MHz scanner and a L64
linear transducer or probe (Hitachi Aloka Medical, Ltd.). The probe
was fitted with a rubber sheath and filled with degassed water to
minimize acoustic artifacts and ensure acoustic coupling. It was
used without the water-soluble gel. The examination was performed
with the patient opening the mouth, and gently extending the lower
lip with gauze. Light pressure was applied to the surface of the
lesion to prevent shape distortion. MRI was performed using a 3.0-T
Ingenia Elition X Philips system (Philips Healthcare) scanner.
Briefly, the patient underwent 3-dimensional (3D) spoiled-gradient
multiple echo modified Dixon (mDIXON) sequence on the scanner using
the following acquisition parameters: 2 echoes (n x1.94 ms echo
time (TE) with n=3.3), 15˚ flip angle, 6.0 msec repetition time
(TR), 200x200x150 mm3 field of view (FOV), 224x224x150
matrix size, 3 min 9 sec scan time. The acquisition was in single
breath-hold with patient in supine position. For signal reception,
a 20 channel body-array coil was used. The acquisition was
performed on the Head and Neck region.
Histopathological evaluations utilised fresh
surgical excision biopsy obtained by extracapsular dissection (ECD)
of the lower lip lesion. Briefly, after finding the haematology
results within normal ranges, the excisional biopsy was performed
over the intraoral side of the lower lip mucocutaneous junction,
through a 15 mm vertical incision in the lateral third of the lip.
The tumor was well circumscribed with no adhesions and was easily
bluntly dissected and removed in its entirety including a free
margin of about 3 mm. The incision was closed with a 6.0
polypropylene suture and the entire specimen was submitted to the
university hospital pathology department for histologic
examination. In the department, standard diagnostic laboratory
histopathological staining protocols and interpretation of obtained
images were observed. Hematoxylin and eosin (H&E) staining was
done on 96% ethanol fixed frozen biopsy material cut into 4 µm
thick sections. The fixed sliced sections-slides, were incubated in
a 10% formalin solution for 24 h. Thereafter, slides were rinsed
with sterile water before staining with hematoxylin for 30 sec.
After hematoxylin staining, the slides were rinsed under running
water for 5 min, before counterstaining with eosin Y for 15 sec.
Finally, the slides were dehydrated in ethanol (96 and 99.8%),
fixed with xylene, and coverslipped with a mounting medium. All the
diagnostic images were taken under a Nikon Eclipse CI microscope
and captured with a Nikon DS-Fi3 camera. (Nikon Eclipse Ci).
Differential staining of acid mucopolysaccharides by AIcian blue
was achieved by staining the fixed slides with 1% (w/v) Alcian Blue
8 GX (Sigma) in 3% (v/v) acetic acid (pH 2.5). Then microwaved for
5 min at 80 W, followed by an additional 10-min incubation in the
warm Alcian blue solution, and then washed three times in distilled
water, dehydrated and mounted with dibutyl phathalate xylene (DPX)
Mountant (Sigma-Aldrich; cat. no. 44581) before the microscopy
examination (Nikon Eclipse Ci).
IHC utilised the streptavidin-peroxidase technique
on biopsy sections of 4-µm thickness. Briefly, the 4-µm sections
were rinsed with phosphate-buffered saline (PBS) and pepsase
activity of 10 min was used for antigen retrieval. After washing in
PBS, the sections were incubated in methanol with addition of 3%
hydrogen peroxide to deactivate the endogenous peroxidases and
blocked with PBS 0.5% Tween-20 (PBS-T; Sigma), containing 3% bovine
serum albumin (BSA) (Sigma) for 1 h at room temperature. The slides
were incubated at 4˚C overnight with primary antibodies of
epithelial markers including CK7, CK15, EMA, and CEA and
mesenchymal and myoepithelial markers including SMA, S-100, and
tumor protein 63 aka transformation-related protein 63 (p63). For
instance, for the basal epithelial differentiation marker CK15, the
primary antibody, rabbit anti CK15 (1:200; ab52816; Abcam) was
used. After three washes with PBS, a secondary antibody, goat
anti-rabbit IgG H&L (HRP) (1:1,000; ab205718; Abcam) was added
with fresh Diaminobenzidine as the substrate. Negative controls
utilized PBS as a replacement for the primary antibody. All images
were acquired using Philips IntelliSite Pathology Solution
(Philips), and analysed by at least 2 pathologists.
Results
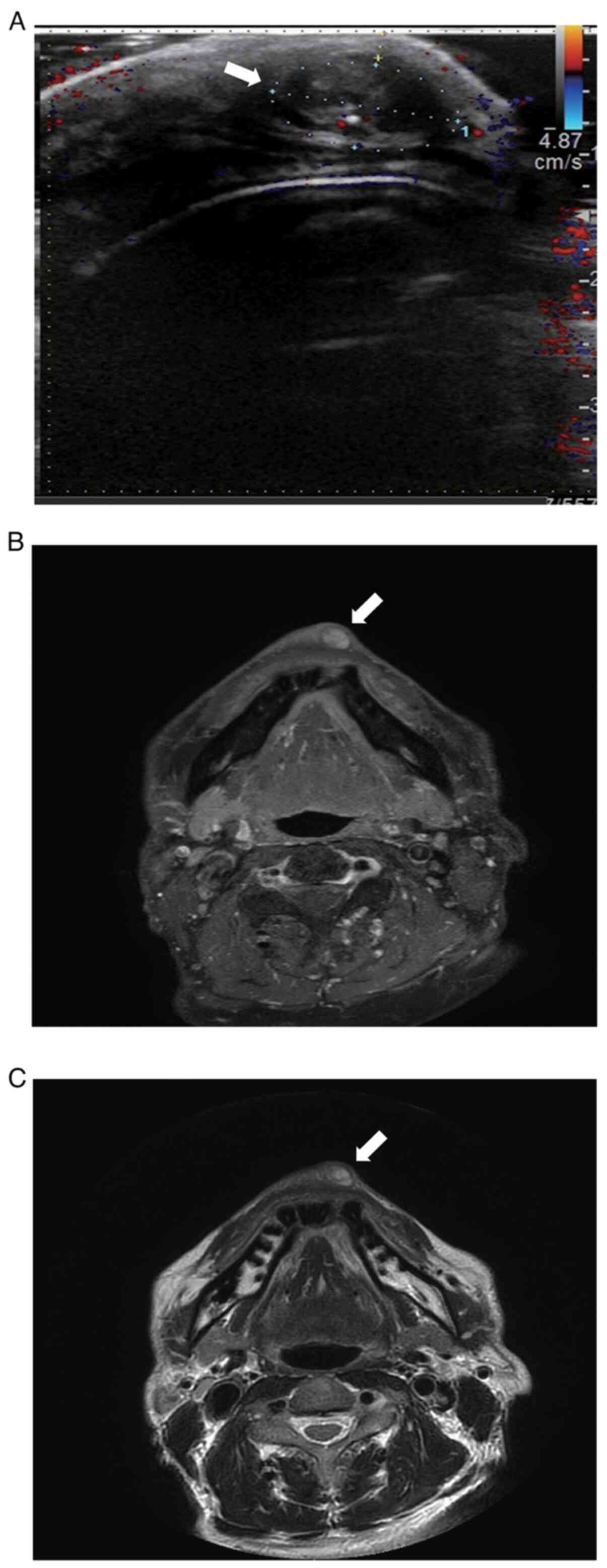
US revealed a well-defined, heterogenous, hypoechoic
lesion measuring 11x11x7 mm3 in size at a depth of ~2 mm
in subcutaneous plane of the lower lip with increased internal
vascularity, but no lymph node swelling or other tumourous lesions
were identified (Fig. 2A). MRI
demonstrated low signal intensity on T1 weighted images and
intermediate to high signal intensity on T2 weighted images in the
left lateral third of the lower lip (Fig. 2B and C). ECD revealed a tumour covered with a
capsula fibrosa located between the orbicularis oris muscle and the
skin (Fig. 3). On gross
examination, the excision biopsy was round, yellowish-white tumour
covered by a thin fibrous capsule (Fig. 4).
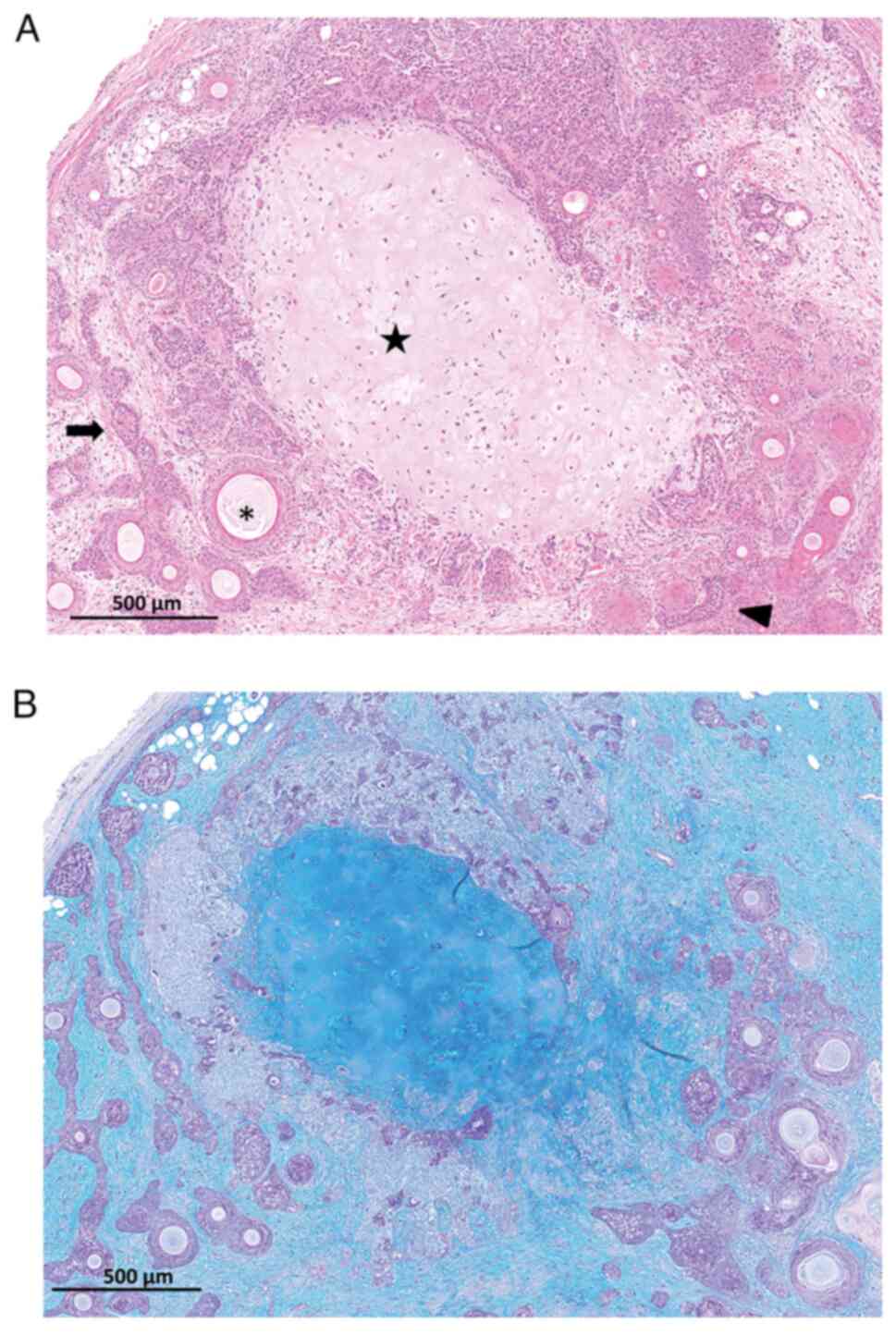
Histologically, a relatively well-defined nodular
lesion was observed (Fig. 5A) with
features ranging from mucinous interstitium, proliferation and
migration of short-spindle stellate cells that comprised epithelial
nests and many cysts mimicking fused and scattered epithelial and
hair follicle infundibula and partially differentiated bone,
cartilage and adipose tissue structures. In addition, IHC showed
inner epithelial cell expression of CK15, CK7, EMA, and CEA and
outer epithelial cells expression of mesenchymal and myoepithelial
markers, S-100, SMA and p63. However, the expression of CK15
(Fig. 5B) and p63 were stronger
(higher) compared to the other markers (data not shown). A
diagnosis of CS was retrospectively made.
Treatment and follow-up
The ECD surgery performed to obtain a complete free
margin excision biopsy also served as the definitive treatment for
the benign CS. Moreover, the patient was offered preoperative
counselling to reduce anxiety and enhance postoperative
satisfaction through interprofessional collaboration practice with
the plastic surgery team. The patient had an uneventful healing
(Fig. S1) and the MRI after a
follow-up of nearly 2 years did not indicate evidence of recurrence
(Fig. S2).
Literature review Literature search
strategy
The literature search for review, summarized in a
schema (Fig. S3), mainly focused
on original articles about patients with cutaneous mixed tumours of
the head and neck region that were written in English. Non-English
articles were evaluated for pertinence and content of new
information. Databases including inter alia Medline, Embase
and Web of Science were searched using various combinations of the
following search terms: Head and Neck region, cutaneous adnexal
tumours, mixed tumour of the skin, chondroid syringoma, upper lip,
and lower lip. There was no restriction on date of publication and
the earliest article used was published in 1859. However, the
review excluded articles of other mixed tumours, malignant tumours,
salivary gland tumours, pleomorphic adenoma, or the benign
cutaneous mixed tumours located on other parts of the body
including trunk and extremities.
Articles were screened manually and selected
according to the inclusion and exclusion criteria in a two-step
process by two authors (SG and EHN). Selected articles were
reviewed based on the title and abstract before screening the full
texts.
Findings
The literature search resulted in the identification
of a total of 394 related records (Fig. S3). Of these, 336 entries for other
tumours, such as PA and malignant tumours were excluded. Based on
the title and abstract review, 38 records of CS localized in other
parts of the body were dropped, leaving 20 articles eligible for
full-text review. The full-text review is summarized in Table I where 17/20 (85%) articles
reported 38 cases of CS of the upper lip and only 3/20 (15%)
articles reported 4 cases of CS of the lower lip (Table I).
 | Table IPublished cases of chondroid syringoma
in the lip. |
Table I
Published cases of chondroid syringoma
in the lip.
| Authors, year | Lip location | Number of
patients | Sex | Age, years | (Refs.) |
|---|
| Stout and Gorman,
1959 | Upper lip (n=38) | 16 | - | - | (10) |
| Triantafyllou and
Rapidis, 1986 | | 1 | Male | 38 | (12) |
| Adlam and Wood,
1986 | | 1 | - | - | (14) |
| Zumdick et
al, 1995 | | 1 | Male | 85 | (24) |
| Shimizu et
al, 1996 | | 1 | Female | 68 | (25) |
| Bekerecioglu et
al, 2002 | | 3 | Male | 27 | (9) |
| | | | Females | 24,28 | |
| Satter and Graham,
2003 | | 1 | Male | 25 | (26) |
| Shimizu et
al, 2003 | | 1 | Male | 68 | (16) |
| Arikan et
al, 2004 | | 1 | Male | 73 | (15) |
| Dubb and Michelow,
2010 | | 1 | Female | 58 | (17) |
| Girgis et
al, 2015 | | 1 | Male | 23 | (18) |
| Shilpa et
al, 2016 | | 1 | Male | 48 | (11) |
| Kundu et al,
2016 | | 1 | Male | 46 | (19) |
| Min et al,
2016 | | 5 | Males | 39,44,47,64 | (20) |
| | | | Female | 65 | |
| Reddy et al,
2018 | | 1 | Male | 35 | (13) |
| Syed et al,
2019 | | 1 | Male | 44 | (22) |
| Vázquez Hernández
et al, 2021 | | 1 | Male | 65 | (21) |
| Stout and Gorman,
1959 | Lower lip | 2 | - | - | (10) |
| Rodrigues et
al, 2021 | (n=4 in
searched | 1 | Male | 43 | (8) |
| Palit et al,
2021 | articles) | 1 | Male | 42 | (23) |
| Present study | | 1 | Male | 58 | - |
Discussion
Mixed tumour of the skin, arguably referred to as
CS, is a rare and mostly benign skin lesion, comprising both
epithelial and mesenchymal stromal derived elements (4,5). CS
can originate either from apocrine or eccrine sweat glands
(6,7) or result from idiopathic proliferation
of abnormally located embryonic tissue (33). As observed in our patient medical
history, it is also suggested that trauma could be a predisposing
factor to the development of CS (8,33).
The most common CS site location in the head and
neck region is the face, especially on the nose and its
surroundings (4). Hirsch and
Helwig (4) reported a 79.8%
occurrence of CS in the head or maxillofacial region and
highlighted the lower lip site as extremely rare, with only 2 out
of 150 cases (1.3%). Similarly, Stout and Gorman (10) reported only 2 out of 134 cases
(1.5%) of CS in the head and neck region occurred on the lower lip.
Consistent with previous reports (4,10),
our professional literature search indicated that CS of the lower
lip remains rare with only 4 out of 42 cases (9.5%) reported in the
identified articles on CS of the lips (8-26).
CS mostly manifests clinically as a painless,
isolated, solid, elastic and hard mass, with a relatively slow
increase in size and an average diameter of ~1 cm (12,34,35).
CS has no specific clinically observable characteristics (36). Hence, histopathological
examinations are indispensable in distinguishing CS from other
mixed tumours of skin, such as the PA. Histologically, the tumour
with ducts surrounded by a bilayer of epithelium and forms a
dilated lumen or cystic cavity is the AMT type, whereas the one
that forms a small lumen surrounded by a single layer of epithelium
is the EMT type (37). The sweat
glands found on facial skin are heterogeneous, and comprise both
eccrine and apocrine glands. The eccrine glands are distributed all
over the facial skin except the lips, whereas the apocrine glands
are mainly distributed on the alae nasi, nasal vestibule and ear
canal. Notably, although the beard area of the face contains
apocrine glands (38), they are
comparatively less distributed in the lower lip. This might justify
the reported low incidence of CS in this site. In our case,
morphological differentiation toward the hair follicles was
illustrated. Further, although IHC markers are of limited value to
differentiate AMT from EMT types of CS, the findings of especially
the strong expression of CK15 and p63 together with EMA and CEA
suggested the tumour to be of AMT type. CEA is positive on the
secretory lumen of secretory cells and the luminal surface of the
duct in eccrine sweat glands, while on the apocrine secretory
cells, it may also label the luminal membranes (34). The stromal component in CS may be
myxoid, chondroid, adipocytic or fibrous. In our case, the stromal
cells showed myoepithelial differentiation as suggested by the
positive expression of S100 protein. However, most important
diagnostic findings were the illustration of histomorphology of CS
including the differentiation toward bone, chondroid and adipose
tissue in this case. Histology did not show features suspicious of
malignancy such as cytological atypia, increased mitotic figures,
infiltrative margins, satellite tumor nodules or tumor necrosis. In
addition, there was no evidence of recurrence or metastases after a
follow-up period of nearly 2 years. Hence, a diagnosis of atypical
or malignant CS was excluded.
In principle, the treatment of CS is complete
surgical excision (5). Inadequate
surgical excision of CS reportedly causes recurrence (39) and malignant transformation
(40,41). Therefore, a careful determination
of the extent of resection should always be done; and ensure a
regular postoperative examination and long-term follow-up of
patients (40,41). In this case, because the patient
had aesthetic concerns, we opted for the less invasive and safer
ECD surgical approach commonly subjected to surgery of the parotid
gland. Additionally, we approached the excision of the tumour from
the intraoral side to limit exposure of the surgical scar.
Interprofessional collaborative practice of managing the tumour
with the plastic surgery team allayed the patient's anxieties and
positively influenced postoperative satisfaction.
In conclusion, although CS of the lower lip is a
rare tumor, it should be considered in the differential diagnosis
of lip masses. Interprofessional collaborative management of the
patients is encouraged where necessary and should include complete
excision of the lesion and long-term follow-up since malignant
forms of CS have been reported.
Supplementary Material
Postoperative follow-up image. The
patient appeared to have healed uneventfully (white
arrowheads).
MRI image (nearly 2 years
postoperative) showing no evidence of recurrence (white arrow).
MRI, magnetic resonance imaging.
Schema for the inclusion and exclusion
criteria of articles for the literature review. CS, chondroid
syringoma; PA, pleomorphic adenoma.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analysed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
SG, EHN, YS and HN were involved in the conception
and design of the report. SG, EHN, TN, AM and SM analysed and
interpreted the patient data. SG, EHN and AM drafted and critically
revised the manuscript for important intellectual content. YS and
HN confirmed the authenticity of all the raw data and provided
final approval of the completed article. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for both the surgical treatment and publication of any
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Sulochana S, Manoharan M and Anith :
Chondroid syringoma-an unusual presentation. J Clin Diagn Res.
8:FD13–FD14. 2014.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Billroth T: Observations on the tumors of
salivary glands. Archiv Pathol Anat Physiol Clin Med. 17:357–375.
1859.
|
|
3
|
Gianotti R, Coggi A and Alessi E:
Cutaneous apocrine mixed tumor: Derived from the apocrine duct of
the folliculo-sebaceous-apocrine unit? Am J Dermatopathol.
20:53–55. 1998.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Hirsch P and Helwig EB: Chondroid
syringoma. Mixed tumor of skin, salivary gland type. Arch Dermatol.
84:835–847. 1961.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Bergeron S, Ito H, Arthurs B and Burnier
MN Jr: Pleomorphic adenoma of the eyelid skin: A series of three
atypical cases. Human pathology: Case Reports. 20(200384)2020.
|
|
6
|
Headington JT: Mixed tumors of skin:
Eccrine and apocrine types. Arch Dermatol. 84:989–996.
1961.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Hassab-el-Naby HM, Tam S, White WL and
Ackerman AB: Mixed tumors of the skin. A histological and
immunohistochemical study. Am J Dermatopathol. 11:413–428.
1989.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Rodrigues BTG, Romañach MJ, de Andrade
BAB, de Almeida Freire N and Israel MS: Chondroid syringoma of the
lower lip: Case report. J Oral Maxillofac Surg Med Pathol.
33:486–488. 2021.
|
|
9
|
Bekerecioglu M, Tercan M, Karakok M and
Atik B: Benign chondroid syringoma: a confusing clinical diagnosis.
Eur J Plast Surg. 25:316–318. 2002.
|
|
10
|
Stout AP and Gorman JG: Mixed tumors of
the skin of the salivary gland type. Cancer. 12:537–543.
1959.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Shilpa K, Leelavathy B, Divya G and
Lakshmi D: Chondroid syringoma: Histopathology a cornerstone tool
in diagnosis. Indian J Dermatopathol Diagn Dermatol. 3(20)2016.
|
|
12
|
Triantafyllou AG and Rapidis AD: Chondroid
syringoma of the upper lip: Report of a case. J Oral Maxillofac
Surg. 44:744–748. 1986.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Reddy PB, Nandini DB, Sreedevi R and
Deepak BS: Benign chondroid syringoma affecting the upper lip:
Report of a rare case and review of literature. J Oral Maxillofac
Pathol. 22:401–405. 2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Adlam DM and Wood GA: The chondroid
syringoma (mixed tumor of skin). Report of a case in the upper lip.
Oral Surg Oral Med Oral Pathol. 61:69–72. 1986.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Arikan OK, Erdoğan S, Muluk NB and Koç C:
Chondroid syringoma of the upper lip: A case report. Kulak Burun
Bogaz Ihtis Derg. 13:25–27. 2004.PubMed/NCBI
|
|
16
|
Shimizu M, Kawano K, Fujiwara S, Noguchi T
and Goto Y: Mixed tumor of the skin (chondroid syringoma) occurring
in the upper lip: Report of a case. J Jpn Soc Oral Oncol. 15:37–41.
2003.(In Japanese).
|
|
17
|
Dubb M and Michelow P: Cytologic features
of chondroid syringoma in fine needle aspiration biopsies: A report
of 3 cases. Acta Cytol. 54:183–186. 2010.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Girgis S, Gillan G and Piper K: Rare
benign mixed tumour of the upper lip: A case report. Ann Med Surg
(Lond). 4:380–383. 2015.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Kundu R, Punia RS, Handa U and Dalal U:
Chondroid syringoma: Cytomorphology of four cases and review of
literature. Arch Cytol Histopathol Res. 1:63–67. 2016.
|
|
20
|
Min KH, Byun JH, Lim JS, Lee HK, Lee WM
and Joo JE: Chondroid syringoma on face. Arch Craniofac Surg.
17:173–175. 2016.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Vázquez Hernández A, Pérez Campos AE,
Gamboa Jiménez TI and Fenton Navarro BF: Giant chondroid syringoma
on the upper lip: A case report. Dermatol Online J: May 15, 2021
(Epub ahead of print). doi: 10.5070/D327553622, 2021.
|
|
22
|
Syed MA, Paudel U, Rajbhandari A, Pokhrel
DB, Adhikari RC and Parajuli S: Fine needle aspiration cytology as
a preliminary diagnostic tool in chondroid syringoma: A case report
and review. Clin Cosmet Invest Dermatol. 12:209–218.
2019.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Palit A, Sethy M, Nayak AK, Ayyanar P and
Behera B: Dermoscopic features in a case of chondroid syringoma.
Indian J Dermatol Venereol Leprol. 87:89–92. 2021.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Zumdick M, Milde P, Ruzicka T and Hölzle
E: Apokriner kutaner Mischtumor mit follikulärer Differenzierung.
Der Hautarzt. 46:481–484. 1995.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Shimizu S, Han-Yaku H, Fukushima S and
Shimizu H: Immunohistochemical study of mixed tumor of the skin
with marked ossification. Dermatology. 193:255–257. 1996.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Satter EK and Graham BS: Chondroid
syringoma. Cutis. 71:49–55. 2003.PubMed/NCBI
|
|
27
|
Wan H, Xu M and Xia T: Clinical and
pathological study on mixed tumors of the skin. Medicine
(Baltimore). 97(e12216)2018.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Greeley PW, Gleason MC and Curtin JW:
Mixed cell tumors of the skin. Plast Reconstr Surg (1946).
18:427–435. 1956.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Chęciński M, Sikora M, Sielski M and
Chlubek D: Pleomorphic adenoma of the lip-a case report. Pomeranian
J Life Sci. 67:27–32. 2021.
|
|
30
|
Matsuyama A, Hisaoka M and Hashimoto H:
PLAG1 expression in cutaneous mixed tumors: An immunohistochemical
and molecular genetic study. Virchows Arch. 459:539–545.
2011.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Russell-Goldman E, Dubuc A and Hanna J:
Differential expression of PLAG1 in apocrine and eccrine cutaneous
mixed tumors: Evidence for distinct molecular pathogenesis. Am J
Dermatopathol. 42:251–257. 2020.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Nakayama H, Miyazaki E, Hiroi M, Kiyoku H,
Naruse K and Enzan H: So‐called neoplastic myoepithelial cells in
chondroid syringomas/mixed tumors of the skin: Their subtypes and
immunohistochemical analysis. Pathol Int. 48:245–253.
1998.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Paik YS and Liess BD: Chondroid syringoma
of the scalp: Case report and discussion of clinical features,
histopathology, and treatment. Ear Nose Throat J. 90:190–191.
2011.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Saga K: Histochemical and
immunohistochemical markers for human eccrine and apocrine sweat
glands: An aid for histopathologic differentiation of sweat gland
tumors. J Investig Dermatol Symp Proc. 6:49–53. 2001.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Kakuta M, Tsuboi R, Yamazaki M, Sakuma M,
Yoshikata R and Ogawa H: Giant mixed tumor of the face. J Dermatol.
23:369–371. 1996.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Kerimoglu U, Aydingoz U, Ozkaya O, Aksu AE
and Ergen FB: MRI of a benign chondroid syringoma. Br J Radiol.
79:e59–e61. 2006.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Kunikane H, Ishikura H, Yamaguchi J,
Yoshiki T, Itoh T and Aizawa M: Chondroid syringoma (mixed tumor of
the skin). A clinicopathological study of 13 cases. Acta Pathol
Jpn. 37:615–625. 1987.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Ishimura E, Iwamoto H, Kobashi Y, Yamabe H
and Ichijima K: Malignant chondroid syringoma. Report of a case
with widespread metastasis and review of pertinent literature.
Cancer. 52:1966–1973. 1983.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Sharvill DE: Mixed salivary-type tumour of
the skin with malignant recurrence. Br J Dermatol. 74:103–104.
1962.PubMed/NCBI
|
|
40
|
Redono C, Rocamora A, Villoria F and
Garcia M: Malignant mixed tumor of the skin: Malignant chondroid
syringoma. Cancer. 49:1690–1696. 1982.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Gardner JM and Smoller BR: Malignant mixed
tumor of skin. In: Rare Malignant Skin Tumors. Springer, New York,
NY, pp77-80, 2015.
|