Introduction
Hip rotationplasty was first reported by Winkelmann
in 1986 as a hip reconstruction method for proximal femoral
malignant tumors (1). It is a
surgical method in which the remaining distal femur is rotated 180˚
after resection of the tumor and fixed to the outside of the
pelvis. The knee joint functions as the hip joint and the ankle
joint functions as the knee joint. A few reports of reconstructed
bone fractures after rotationplasty following excision of femoral
malignant tumors have been reported (2,3);
however, to the best of the authors' knowledge there are no
previous reports on detailed surgical interventions in patients
with a reconstructed bone fracture status after hip
rotationplasty.
The present study presents a case of fracture of the
reconstructed bone status after hip rotationoplasty 28 years after
surgery treated by open reduction and internal fixation (ORIF) and
external fixation.
Case report
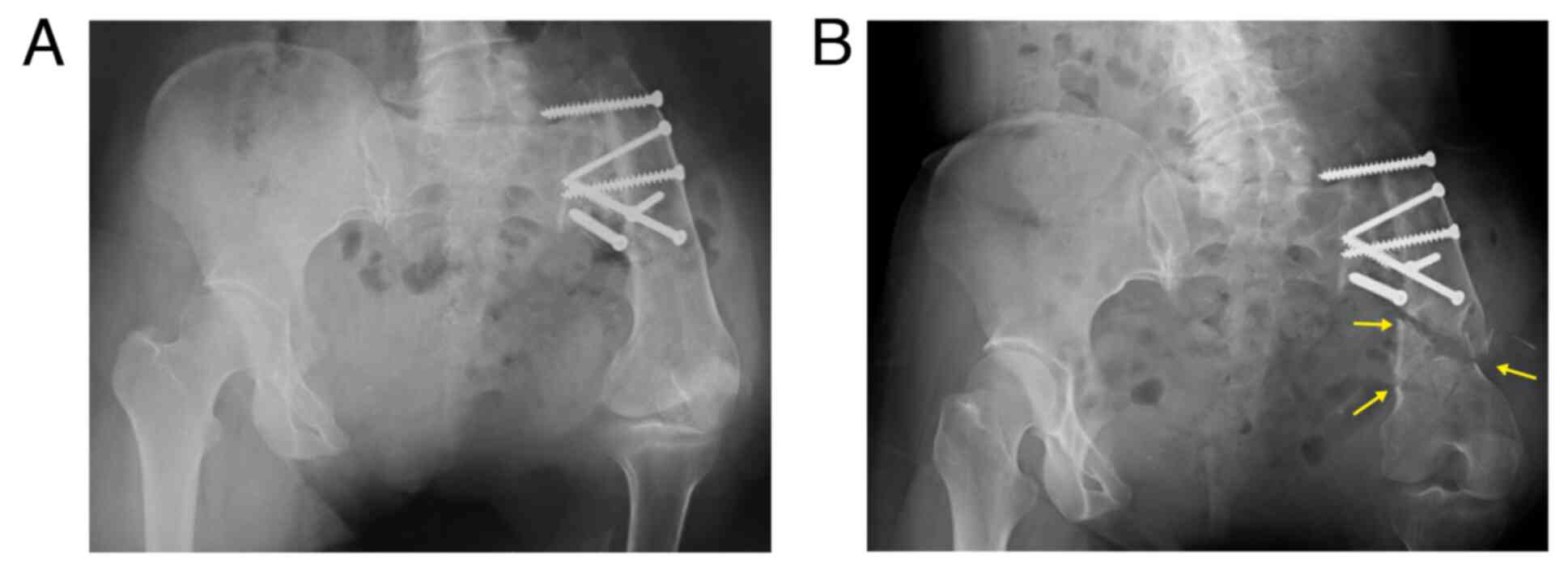
A 52-year-old woman underwent hip rotationplasty for
Ewing sarcoma of the proximal left femur at the age of 24 years and
was followed up annually at the Department of Orthopedic Surgery,
Graduate School of Medicine, University of the Ryukyus (Fig. 1A). Her crutches were caught in the
step while climbing stairs at home, making her fall and hit her
left buttock. The patient was transported to the hospital by
ambulance because of severe pain and difficulty with mobility.
Physical observations at the time of ambulance transport were as
follows: A subcutaneous hematoma was found around the left buttock,
no open wound was observed, the patient had pain in the left
buttock when the patient moved and had difficulty walking even with
a prosthetic leg. Radiography revealed a distal comminuted fracture
of the reconstructed bone (Fig.
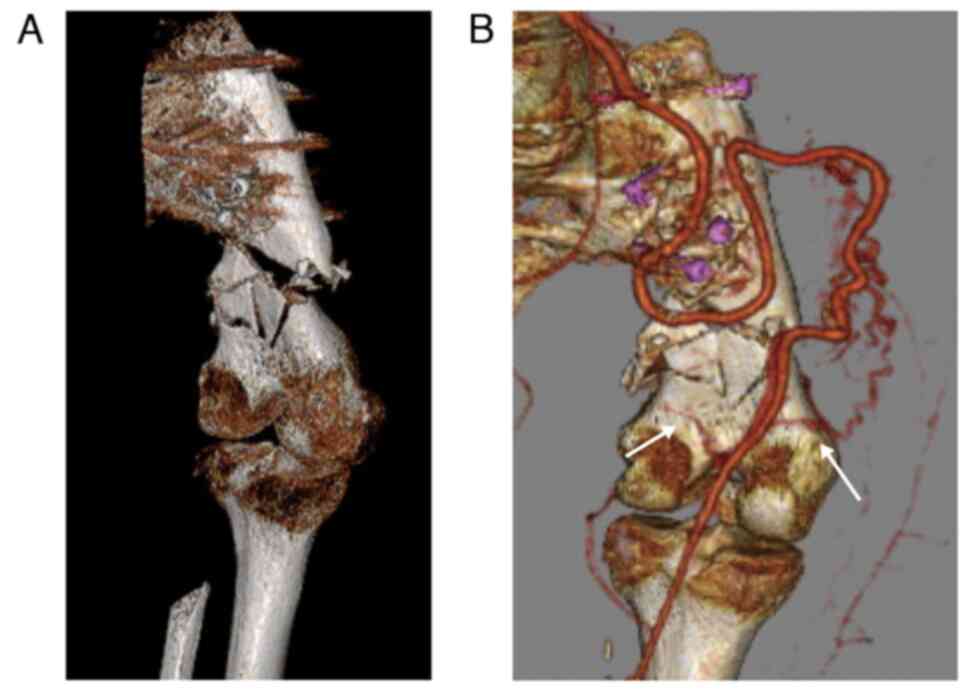
1B). Computed tomography (CT) revealed a comminuted fracture of
the reconstructed bone, similar to the radiograph, and blood
vessels flowed into the distal bone fragment (Fig. 2A and B).
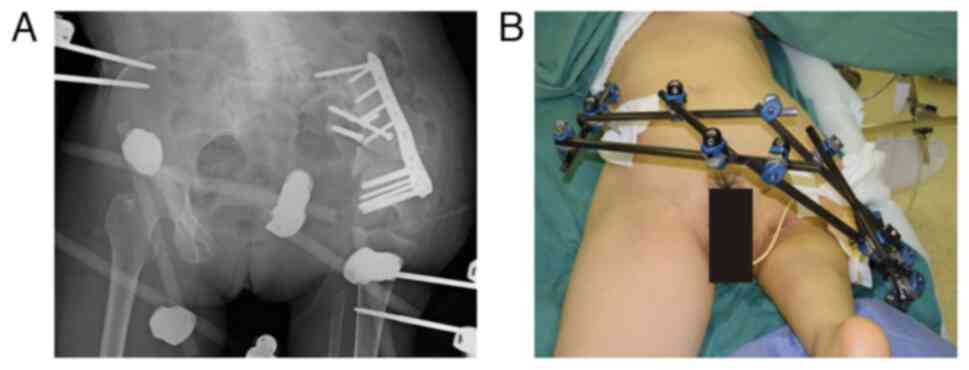
The patient underwent ORIF and external fixator.
Under general anesthesia, a pillow was placed under the left
buttock, and the patient was placed in the right half-side-lying
position. An approximately 20 cm longitudinal skin incision was
made on the lateral side of the left buttock. The proximal and
distal parts of the reconstructed bone were exposed without
dissection of the fractured part to preserve the blood flow to the
fracture site. Conformability of the distal femoral Locking
Compression Plate® (DePuy Synthes) was confirmed using a
fluoroscope. The interfering screws were removed. Four locking
screws for the Locking Compression Plate® were inserted
into the proximal bone fragment, and six locking screws into the
distal bone fragment for the Locking Compression Plate®,
respectively (Fig. 3A). Then, two
half-pins for the external fixator were inserted into the proximal
tibia and two half pins were inserted into the contralateral iliac
crest (Fig. 3B). At two days
following surgery, 10 sessions of hyperbaric oxygen therapy and
low-intensity pulsed ultrasound therapy were started to control
excess soft tissue damage and reduce fracture healing time for six
months (4). Denosumab (60 mg per
six months) was administered for osteoporosis treatment after
surgery. External fixation was removed 1 month after the surgery.
Partial weight bearing with prosthetics was allowed 8 weeks after
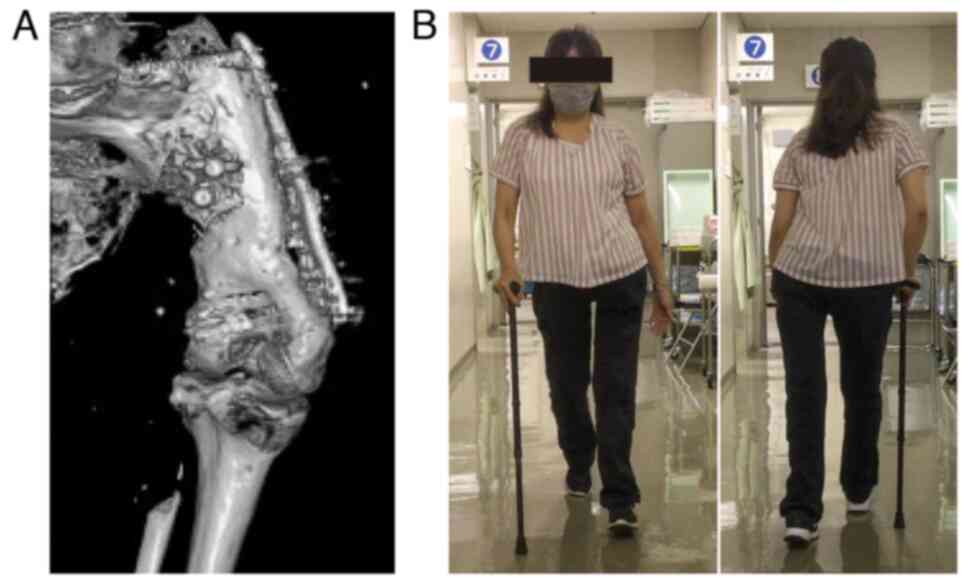
surgery and full weight bearing 15 weeks after surgery. After 24
months after the surgery at the latest follow-up, bone union was
confirmed using 3-dimensional CT (Fig.
4A). The patient could walk with prosthetics and a T-cane and
return to work as an architect (Fig.
4B).
Discussion
Surgical methods for malignant tumors of the
proximal femur include hip disarticulation (5,6),
endoprosthetic arthroplasty (7,8), and
hip rotationplasty (1-3).
Hip rotationplasty was first reported by Winkelmann in 1986 in
patients with malignant tumors of the proximal femur (1). Hip rotationplasty has several
advantages and is an alternative to amputation or extendable
endoprosthesis, resulting in good function. Therefore, it has been
suitable for children with malignant bone tumor in lower limbs
(2,9). This procedure has been performed as
re-operation even after complications such as deep infection
(10). Reports of complications of
hip rotationplasty include loosening of osteosynthesis, venous
thrombosis, arterial thrombosis, delayed wound healing, bone
fractures, and compartment syndrome (2,3,11).
Postoperative complication rates of bone fractures
after rotationplasty were 4-11% in previous reports, which occurred
from 11 months to 12 years following surgery (2,3).
Bone fractures occur in the proximal tibia, distal tibia, or tibial
shaft. In previous reports, surgical intervention or conservative
therapy has been performed for bone fractures after rotationplasty
(2,3). ORIF or shortening osteotomy is
performed for bone fractures after rotationoplasty (2,3).
However, there are no detailed reports on reconstruction. In the
present case, the patient underwent a combination of ORIF and
temporal external fixation for comminuted reconstructed bone
fractures. At the last follow-up, bone union was achieved, and the
patient recovered ambulatory ability.
In the present study, temporal external fixation was
performed to achieve strong fixation for bone fracture after hip
rotationplasty. Temporal external fixation was performed after hip
transposition arthroplasty to stabilized bone and soft tissue,
which was removed 6 weeks after first surgery (12-14).
Hip transposition arthroplasty, also known as resection
arthroplasty, is a procedure that resects malignant bone tumor of
the pelvis or acetabulum and transfers the femoral head to the
lateral surface of the resected sacrum or ilium (12-14).
In a previous study, patients who underwent hip transposition
arthroplasty with temporary external fixation were able to move the
day after surgery, stand with partial weight-bearing seven days
after surgery, and transfer to a wheelchair eight days after
surgery (13). Additional temporal
external fixation might enable early rehabilitation after surgery
to achieve solid immobilization. In this study, ORIF and an
external fixator were used to obtain strong fixation and perform
early rehabilitation.
In conclusion, the present study described the case
of comminuted reconstructed bone fracture 28 years after hip
rotationplasty; the combination of ORIF and temporal external
fixation effectively led to bone union and regain of ambulatory
ability.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated and analyzed during this study
are included in this published article.
Authors' contributions
YuT, HO, KM, YaT, and KN contributed to conception
of this study. YuT, HO, and KM contributed to acquisition of data.
YuT, HO, KM, YaT, and KN wrote and edited the manuscript. HO and
YaT performed surgery and postoperative management, respectively.
YaT and KN conducted revision of the manuscript for important
intellectual content. YuT and YaT confirm the authenticity of all
the raw data. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent for the publication and use
of images was obtained from the patient.
Competing interests
YaT is on the editorial board for Cancer
Diagnosis and Prognosis. KN is on the editorial board of the
Journal of Orthopaedic Research and is a board member of the
International Society for the Study of Lumbar Spine. The authors
declare that they have no competing interests.
References
|
1
|
Winkelmann WW: Hip rotationplasty for
malignant tumors of the proximal part of the femur. J Bone Joint
Surg Am. 68:362–369. 1986.PubMed/NCBI
|
|
2
|
Hardes J, Gosheger G, Vachtsevanos L,
Hoffmann C, Ahrens H and Winkelmann W: Rotationplasty type BI
versus type BIIIa in children under the age of ten years. Should
the knee be preserved? J Bone Joint Surg Br. 87:395–400.
2005.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Sawamura C, Hornicek FJ and Gebhardt MC:
Complications and risk factors for failure of rotationplasty:
Review of 25 patients. Clin Orthop Relat Res. 466:1302–1308.
2008.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Rutten S, van den Bekerom MPJ, Sierevelt
IN and Nolte PA: Enhancement of bone-healing by low-intensity
pulsed ultrasound: A systematic review. JBJS Rev.
4(e6)2016.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Hagi T, Nakamura T, Nagano A, Koike H,
Yamada K, Aiba H, Fujihara N, Wasa J, Asanuma K, Kozawa E, et al:
Clinical outcome in patients who underwent amputation due to
extremity soft tissue sarcoma: Tokai musculoskeletal oncology
consortium study. Jpn J Clin Oncol. 52:157–162. 2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Miwa S, Kamei M, Yoshida S, Yamada S, Aiba
H, Tsuchiya H and Otsuka T: Local dissemination of osteosarcoma
observed after massage therapy: A case report. BMC Cancer.
19(993)2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Chandrasekar CR, Grimer RJ, Carter SR,
Tillman RM, Abudu A and Buckley L: Modular endoprosthetic
replacement for tumours of the proximal femur. J Bone Joint Surg
Br. 91:108–112. 2009.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Kabukcuoglu Y, Grimer RJ, Tillman RM and
Carter SR: Endoprosthetic replacement for primary malignant tumors
of the proximal femur. Clin Orthop Relat Res. 358:8–14.
1999.PubMed/NCBI
|
|
9
|
Winkelmann WW: Type-B-IIIa hip
rotationplasty: An alternative operation for the treatment of
malignant tumors of the femur in early childhood. J Bone Joint Surg
Am. 82:814–828. 2000.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Okazaki N, Kumagai K, Egashira M, Osaki M,
Murata M, Tomita M and Shindo H: Hip rotationplasty with
antibiotic-loaded bone cement spacer for severe infection following
limb-sparing surgery. Orthopedics. 31(713)2008.PubMed/NCBI
|
|
11
|
Gupta SK, Alassaf N, Harrop AR and Kiefer
GN: Principles of rotationplasty. J Am Acad Orthop Surg.
20:657–667. 2012.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Hillmann A, Hoffmann C, Gosheger G, Rödl
R, Winkelmann W and Ozaki T: Tumors of the pelvis: Complications
after reconstruction. Arch Orthop Trauma Surg. 123:340–344.
2003.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Kunisada T, Fujiwara T, Hasei J, Nakata E,
Senda M and Ozaki T: Temporary external fixation can stabilize hip
transposition arthroplasty after resection of malignant
periacetabular bone tumors. Clin Orthop Relat Res. 477:1892–1901.
2019.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Ozaki T, Hillmann A and Winkelmann W:
Treatment outcome of pelvic sarcomas in young children: Orthopaedic
and oncologic analysis. J Pediatr Orthop. 18:350–355.
1998.PubMed/NCBI
|