Introduction
Cervical intraepithelial neoplasia (CIN) is a
premalignant lesion that can be divided into three stages (1,2 and
3). In particular, CIN2 and 3, also known as a high-grade squamous
intraepithelial lesion (HSIL), are high-risk stages of cervical
cancer (1). It is estimated that,
in 70% of affected women, CIN 2 and 3 can persist or progress to
cervical cancer after 10-20 years (2). For this reason, early diagnosis and
management of the premalignant lesions is important to reduce the
natural progression of these lesions to cervical uterine
cancer.
Cervical conization is the gold standard for the
treatment of precancerous diseases of the uterine cervix, and
various conization methods have been described in previous
literature (2-4).
Depending on which surgical method is used, the incidence rates of
perioperative and postoperative complications differ (2,3). In
Japan, 11.6% of patients who underwent therapeutic conization were
treated with using the Shimodaira-Taniguchi (S-T) conization method
(4). The S-T conization method is
associated with decreased thermal damage, improved margin
interpretability, and an increased likelihood of excision of a
single, non-traumatized specimen that can be easily evaluated to
determine the histologic type, grade, glandular involvement, and
margin status using high-frequency current with a triangular probe
and rigid linear electrode (5).
However, English-language articles on S-T conization are limited
(3,5-7),
and the surgical, oncological and obstetric outcomes of S-T
conization have not yet been fully described. The aim of the
present study was to investigate the surgical, oncological, and
obstetric outcomes of the S-T conization method. The present study
also reviewed the previous literature regarding the S-T conization
method.
Materials and methods
Data source
The Institutional Review Board (IRB) of Osaka Rosai
Hospital approved the present study (IRB approval number: 2021-62,
date of approval: September 30, 2021). The medical records of
patients managed at the Osaka Rosai Hospital between January 2010
and December 2018 were retrospectively reviewed. A total of 858
cases in which the therapeutic S-T conization method was used for
HSIL were identified. Patients with diagnostic S-T conization were
excluded from the study. The resected specimens were evaluated by
pathologists according to the WHO Classification of Tumors of
Female Reproductive Organs.
Surgical procedures and postoperative
follow-up
All the included women provided their written
informed consent for the therapeutic procedures. For the present
study, the Institutional Review Board granted an opt-out
recruitment approach and waived the requirement for written
informed consent for participation from each patient. We routinely
performed cervical conization using the S-T method with an Honest
Medical High Frequency Surgical Unit (MGI-202; Honest Medical,
Tokyo, Japan) under intravenous or spinal anesthesia. The probes
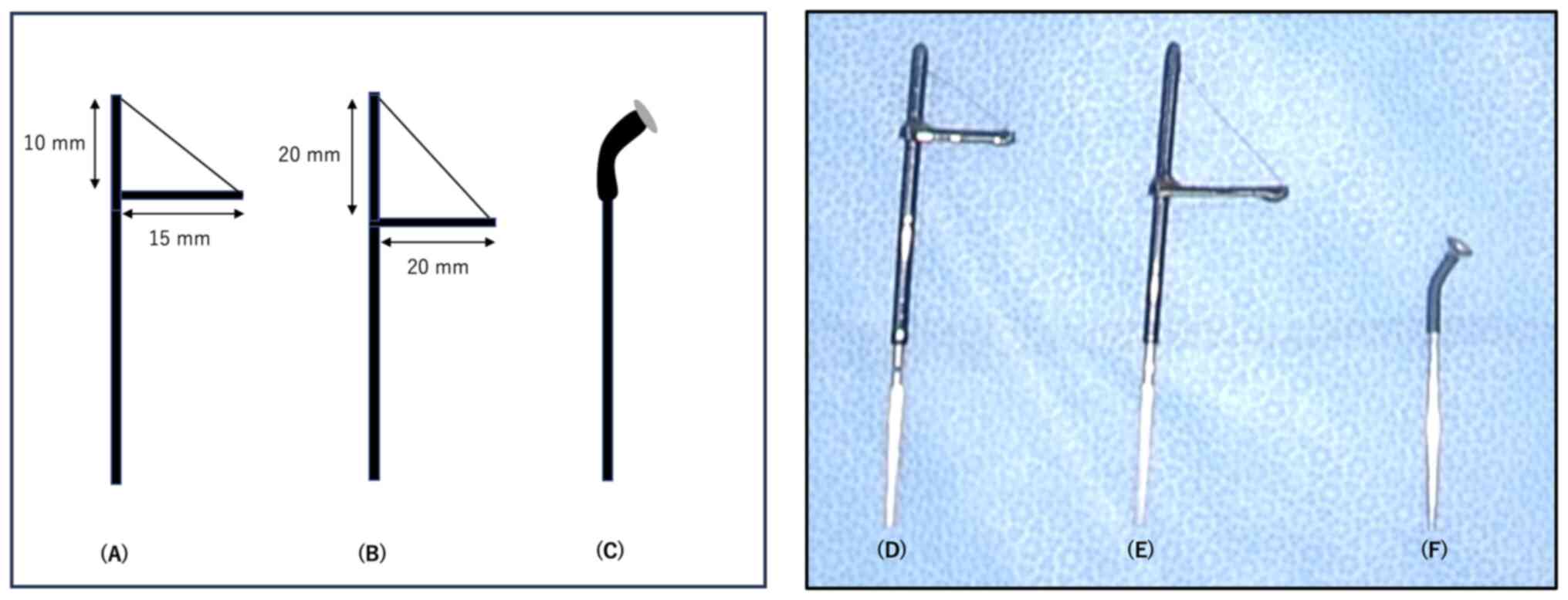
used for the S-T conization method are illustrated in Fig. 1. The cutting probe was inserted
into the cervical canal and rotated to extract a cone of tissue as
a single informative specimen (Video
S1), which can be easily performed regardless of the skill of
the surgeon. The cervical tissue resected by conization was
carefully divided into 12 specimens, and a pathological diagnosis
was made by a pathologist. Within 3-4 months after conization,
cervical cytology was conducted in 813 of the 858 cases. The
cervical cytology results were reported according to the Bethesda
System 2001.
Outcome measurements
The surgical outcomes, including operative time,
number of resected specimens, and complication rates, were
evaluated. The patient characteristics were compared between
patients with and without cervical stenosis, a surgical
complication. Cervical stenosis was defined as cervical narrowing
that limited or prevented the insertion of collection devices for
obtaining cervical cytology samples or uterine sounds, closure
requiring surgical intervention, or any other cases where a
clinician recorded the presence of stenosis in the medical records.
Although decrease in menstrual blood flow may be complication, we
did not have the data regarding the menstrual blood flow before and
after conization. Therefore, we did not define decrease in
menstrual blood flow as a complication. We also analyzed the
factors potentially associated with recurrent/persistent disease
after conization. Recurrent/persistent disease after conization was
defined as the occurrence of HSIL, diagnosed by histopathological
evaluation of a biopsy specimen or subsequent surgical specimen, at
any time after the initial conization procedure. Obstetric outcomes
after conization were also reviewed and potential factors were
compared between the patients with term and preterm delivery in
subsequent pregnancies.
Statistical analysis
The proportions of categorical variables were
analyzed for statistical significance using the χ2 test
(8). The probability of
recurrence-free status was analyzed using the Kaplan-Meier method
and was evaluated for statistical significance using the log-rank
test. Univariate and multivariate analyses were performed to
identify the factors that could potentially affect the risk of
recurrent/persistent disease after conization. We used multivariate
regression analysis to control selection bias. Nominal variables
were dichotomized arbitrarily (presence vs. absence). Variables of
interest were entered into a regression model using the Cox
proportional hazards model. P<0.05. All statistical analyses
were performed using EZR (Saitama Medical Center, Jichi Medical
University, Saitama, Japan) (9), a
graphical user interface for R (The R Foundation for Statistical
Computing, Vienna, Austria). More precisely, it is a modified
version of the R commander designed to add statistical functions
frequently used in biostatistics.
Results
Patients' characteristics
The characteristics of the 858 patients included in
this study are shown in Table I.
The median age was 38 years (Interquartile range (IQR): 33-45); and
BMI was 20.7 (IQR: 19.2-22.6). Of the 858 patients, 297 (34.6%)
were nulliparous, 220 (25.6%) were smokers, and 831 (96.9%) had
CIN3. Sixty-one (7.1%) women underwent conization within 12 months
of childbirth.
 | Table IPatient characteristics (n=858). |
Table I
Patient characteristics (n=858).
| Characteristics | Value |
|---|
| Median age, years
(IQR) | 38 (33-45) |
| Median BMI,
kg/m2 (IQR) | 20.7 (19.2-22.6) |
| Parity, n | |
|
Yes | 561 |
|
No | 297 |
| Smoking status,
n | |
|
Yes | 220 |
|
No | 638 |
| Histology, n | |
|
CIN2 | 27 |
|
CIN3 | 831 |
| Conization within 1
year after delivery, n | |
|
Yes | 61 |
|
No | 797 |
Surgical outcomes
The surgical outcomes are shown in Table II. The median operative time was
5.0 min (IQR: 3-8). Among the 858 patients, 834 (97.2%) had
intraoperative blood loss of ≤50 ml. The number of specimens
obtained by the S-T method was also evaluated; in most cases
(81.3%), a single adequate specimen was extracted. Postoperative
complications that occurred in the patients were as follows:
postoperative bleeding, n=71 (8.3%); cervical stenosis, n=19
(2.2%); postoperative fever, n=1 (0.1%); and abdominal pain, n=2
(0.2%).
 | Table IISurgical outcomes. |
Table II
Surgical outcomes.
| Variables | Value |
|---|
| Median operative
time, min (IQR) | 5.0 (3.0-8.0) |
| Blood loss, n
(%) | |
|
≤50 ml | 834 (97.2) |
|
≥51 ml | 24 (2.8) |
| Median weight of
resected specimen, g (IQR) | 3.0 (2.0-3.8) |
| Number of resected
specimens, n (%) | |
|
1 | 698 (81.3) |
|
≥2 | 160 (18.7) |
| Complication, n
(%) | |
|
Postoperative
bleeding | 71 (8.3) |
|
Cervical
stenosis | 19 (2.2) |
|
Fever | 1 (0.1) |
|
Abdominal
pain | 2 (0.2) |
| Surgical margin
status, n (%) | |
|
Negative | 699 (81.5) |
|
Positive | 159 (18.5) |
| Endocervical margin
involvement, n (%) | |
|
Yes | 86 (10.0) |
|
No | 73 (8.5) |
| Median follow-up
duration, months (IQR) | 28.0 (14-49) |
| Cervical cytology
within 3-4 months after conization, n (%) | |
|
Negative for
intraepithelial lesion and malignancy | 701 (81.7) |
|
Other | 112 (13.1) |
|
N/A | 45 (5.2) |
| Recurrence, n
(%) | |
|
Yes | 42 (4.9) |
|
No | 816 (95.1) |
As shown in Table
III, 6 of the 631 (0.95%) younger patients (<45 years of
age) experienced cervical stenosis. In contrast, 13 of 227 (5.7%)
older patients (≥45 years) experienced cervical stenosis. The
proportion of older patients with cervical stenosis was
significantly higher (P<0.001). Factors such as the number of
resected specimens, conization within one year after delivery,
intraoperative blood loss (≥51 ml), and suturing for hemostasis did
not have any statistically significant impact on the occurrence of
cervical stenosis.
 | Table IIIFactors potentially associated with
cervical stenosis after conization. |
Table III
Factors potentially associated with
cervical stenosis after conization.
| | Stenosis | |
|---|
| Factors | Yes | No | P-value |
|---|
| Age, years | | | <0.001 |
|
<45 | 6 | 625 | |
|
≥45 | 13 | 214 | |
| Number of resected
specimens | | | 0.358 |
|
1 | 17 | 681 | |
|
≥2 | 2 | 158 | |
| Conization within 1
year after delivery | | | 0.558 |
|
No | 17 | 780 | |
|
Yes | 2 | 59 | |
| Intraoperative
blood loss, ml | | | 0.455 |
|
≤50 | 19 | 815 | |
|
≥51 | 0 | 24 | |
| Suturing for
hemostasis | | | |
|
No | 16 | 761 | 0.338 |
|
Yes | 3 | 78 | |
Factors associated with
recurrent/persistent disease after conization
As shown in Table
II, the median follow-up period was 28 months (IQR: 14-49).
Among the 858 patients, 42 (4.9%) developed disease recurrence
during the observation period. A positive surgical margin was
observed in 159 (18.5%) of the 858 patients. Of the 159 patients
with a positive surgical margin, 86 (10.0%) had a positive
endocervical margin and 73 (8.5%) had no endocervical involvement.
As shown in Table IV, the
following baseline factors showed a significant association with a
higher recurrence rate in univariate analysis: age ≥45 years
(P<0.001) and positive surgical margin status (P<0.001). The
number of resected specimens and the smoking status were not
statistically significant. In multivariate analysis, age ≥45 years
(hazard ratio (HR) 3.22, 95% confidence interval (CI) 1.73-6.02,
P<0.001) and positive surgical margin status (HR 6.39, 95% CI
3.44-11.8, P<0.001) also showed an independent association with
recurrent disease.
 | Table IVUnivariate and multivariate Cox
regression analyses for recurrent/persistent disease after
conization. |
Table IV
Univariate and multivariate Cox
regression analyses for recurrent/persistent disease after
conization.
| | Univariate
analysisa | Multivariate
analysisa |
|---|
| Variables | HR | 95% CI | P-value | HR | 95% CI | P-value |
|---|
| Age, years | | | | | | |
|
<45 | 1 | | | 1 | | |
|
≥45 | 3.170 | 1.724-5.828 | <0.001 | 3.220 | 1.730-6.020 | <0.001 |
| Number of resected
specimens | | | | | | |
|
1 | 1 | | | | | |
|
≥2 | 0.755 | 0.318-1.793 | 0.524 | 0.665 | 0.273-1.560 | 0.342 |
| Surgical margin
status | | | | | | |
|
Negative | 1 | | | | | |
|
Positive | 6.098 | 3.313-11.20 | <0.001 | 6.390 | 3.440-11.800 | <0.001 |
| Smoking | | | | | | |
|
No | 1 | | | | | |
|
Yes | 1.129 | 0.567-2.249 | 0.730 | 1.210 | 0.607-2.431 | 0.581 |
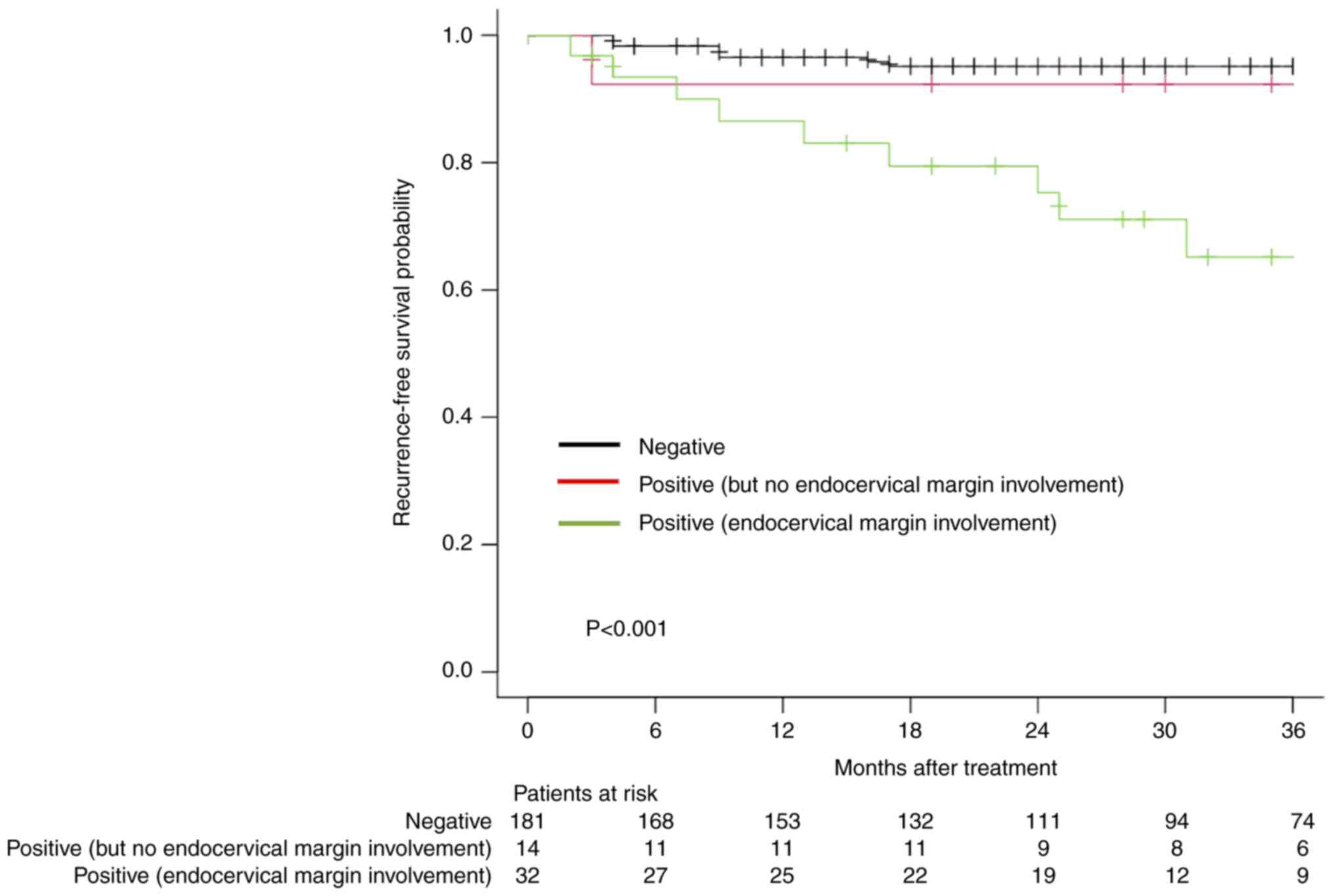
The recurrence-free survival rates in older patients
according to surgical margin status are shown in Fig. 2. Older patients with endocervical
margin involvement had a higher recurrence rate (3-year recurrence
rate, 28.1%).
Obstetric outcomes after
conization
The obstetric outcomes are shown in Table V. The study included 62 pregnant
women and 66 live births. Among the 66 deliveries, there were 62
term deliveries (93.9%) and 4 were preterm deliveries (6.1%). The
proportion of patients with maternal comorbidities and smoking
status did not differ significantly between the patients with term
and preterm pregnancies. Two of the 10 patients (20%) who had a
short interval from conization to conception (≤3 months)
experienced preterm delivery. In contrast, 2 of the 56 patients
(3.6%) with a >3 months interval from conization to conception
experienced term pregnancy. The proportion of patients who
experienced preterm delivery after conization was significantly
higher in those with a short interval from conization to conception
(P=0.045).
 | Table VObstetrical outcomes after
Shimodaira-Taniguchi conization. |
Table V
Obstetrical outcomes after
Shimodaira-Taniguchi conization.
| Variables | Term pregnancy,
n | Preterm pregnancy,
n | P-value |
|---|
| Number of live
births | 62 | 4 | |
| Comorbidity | | | 0.918 |
|
No | 55 | 4 | |
|
Myoma | 2 | 0 | |
|
Obesity | 3 | 0 | |
|
Asthma | 2 | 0 | |
| Smoking | | | 0.763 |
|
No | 42 | 3 | |
|
Yes | 20 | 1 | |
| Interval from
conization to conception | | | 0.045 |
|
≤3
months | 8 | 2 | |
|
>3
months | 54 | 2 | |
| Gestational
age | | | |
|
≤27 weeks 6
days | 0 | 1 | |
|
28 weeks 0
days to 31 weeks 6 days | 0 | 1 | |
|
32 weeks 0
days to 33weeks 6 days | 0 | 0 | |
|
34 weeks 0
days to 36 weeks 6 days | 0 | 2 | |
|
≥37 weeks 0
days | 62 | 0 | |
| Mode of
delivery | | | 0.783 |
|
Vaginal
delivery | 50 | 3 | |
|
Cesarean
section | 12 | 1 | |
Discussion
We searched the PubMed database for all
English-language articles related to S-T conization published by
July 10, 2022, using the following key words and combinations of
key words: ‘Shimodaira-Taniguchi’ and ‘conization.’ Only five
articles regarding S-T conization for HSIL have been previously
reported (3-7)
(Table VI). The overall
recurrence rate was reported to be 1.3-5.8% and a positive surgical
margin was observed in 13.4-39.1% of the patients, which was
consistent with the present study. However, postoperative
complications and obstetric outcomes after S-T conization have not
been fully described in the previous literature. The strengths of
the current study were to evaluate not only the oncological
outcomes, but also the surgical and obstetric outcomes of S-T
conization and to review the previous literature regarding S-T
conization.
 | Table VISummary of previous studies regarding
Shimodaira-Taniguchi conization for high-grade squamous
intraepithelial lesions. |
Table VI
Summary of previous studies regarding
Shimodaira-Taniguchi conization for high-grade squamous
intraepithelial lesions.
| First author/s,
year | Number of
patients | Median or mean
postoperative follow-up duration, months (range) | Recurrent and
residual disease, n (%) | Margin positive, n
(%) | Cervical stenosis,
n (%) | Total number of
deliveries after conization | Preterm delivery, n
(%) | (Refs.) |
|---|
| Tanaka et
al, 2017 | 522 | 19
(20-83)a | 25 (4.8) | 87 (16.7) | 28 (5.2) | N/A | N/A | (3) |
| Ikeda et al,
2021 | 1,024 | N/A | N/A | 184 (18.0) | N/A | N/A | N/A | (4) |
| Matsumura et
al, 2010 | 455 | (13-60) | 6 (1.3) | 178 (39.1) | 15 (3.3) | N/A | N/A | (5) |
| Miyoshi et
al, 2012 | 243 | 18.8
(1-100)a | 14 (5.8) | 45(19) | N/A | N/A | N/A | (6) |
| Kigure et
al, 2018 | 689 | 36.8
(0-107)b | 22 (3.2) | 62 (13.4) | 21 (3.0) | 107 | 15 (14.0) | (7) |
| Present study | 858 | 28
(14-49)a | 42 (4.9) | 159 (18.5) | 19 (2.2) | 66 | 4 (6.1) | - |
The incidence of cervical stenosis after conization
in previous studies varies up to 29% (10), depending on the definition
employed. Various factors, including age, deep incision, and time
within one year of delivery, are associated with cervical stenosis
(3,11). In the current study, cervical
stenosis was more likely to occur in individuals older than 45
years. These findings might be due to the migration of the
transformation zone to the cervical canal with increasing age and
after menopause (12). In contrast
to younger patients, the squamocolumnar junction (SCJ) in older
patients is usually located in the endocervix. Therefore, deep
conization is required to excise precancerous lesions in these
patients, which may lead to cervical stenosis. Furthermore,
cervical stenosis after conization in elderly patients may be
associated with amenorrhea or a decreased frequency of
menstruation. The lack of natural dilatation of the cervical canal
by menstrual blood may be the main reason for this complication
(3). Cervical stenosis can make it
difficult to check for the deeper side of the cervical canal.
Cervical stenosis can lead to an unsatisfactory follow-up after
conization with a risk of unseen relapse. Therefore, a careful
follow-up of older patients is required.
Surgical margin status is a well-known prognostic
factor for persistent or recurrent disease. There is no consensus
on the safety margin when performing conization for HSIL. In the
present study, the rate of positive surgical margins was 18.5%. In
comparison to the loop electrosurgical excision procedure (LEEP)
(11.2%) or cold knife conization (CKC) (8.1%), it seems higher
(13-15).
However, the overall recurrence rate after the S-T method was
approximately 5%, which was comparable to that after LEEP (8.1%)
and CKC (2.1%) (13-15).
Although a precise explanation for the low recurrence rate with the
S-T method is unclear, it may be associated with the use of a
coagulation probe. A small flat probe, as shown in Fig. 1, was applied to the entire cervical
stump to coagulate the remaining part of the lesion. This step may
help prevent recurrence in patients with positive surgical
margins.
We found that older age (≥45 years) was not only an
independent prognostic factor for recurrence after conization, but
also an independent prognostic factor for cervical stenosis, which
may lead to unsatisfactory follow-up. In particular, focusing on
surgical margin status, older patients with endocervical margin
involvement showed a higher rate of recurrence (3-year recurrence
rate: 28.1%) (Fig. 1). When
residual disease is present in the endocervix, postsurgical
stenosis can prevent adequate follow-up. Therefore, when
endocervical margin involvement is confirmed in older patients with
no visible SCJ, it is beneficial to recommend the performance of a
subsequent hysterectomy.
Few studies have investigated obstetric outcomes
after S-T conization. In the current study, the rate of preterm
delivery was 6.1%, which was consistent with the rate of preterm
delivery in the general Japanese population (5.6%) (16). We found that a short interval
between conization and pregnancy (≤3 months) was associated with
preterm delivery (Table V). Some
authors have suggested that a 3- to 4-month interval from
conization to pregnancy increases the risk of preterm delivery
(17,18), while others have suggested that the
time interval from conization is not associated with preterm
delivery (19,20). Various other factors are
potentially associated with preterm birth after conization,
including cone depth (21), size
of the resected specimen (22) and
pre- and post-treatment cervical length (23). Therefore, whether the interval from
conization to conception is associated with preterm birth remains
controversial. The cervical length was reported to heal to nearly
the same length as the pretreatment level at 6 months of
posttreatment follow-up in patients who delivered at term in a
subsequent pregnancy (23).
Although it is difficult to determine the optimal interval from
conization to pregnancy, an interval of at least 6 months would be
reasonable, considering the risk of preterm birth and the time
required for regeneration of cervical length.
The present study is associated with some
limitations. First, the data used in this study were retrospective,
and the sample size was relatively small. A larger sample size is
needed to support our results. Second, confounding factors for
recurrent disease, such as preoperative and postoperative HPV
infection status, were not analyzed. This type of information
strengthened the results of our study. Third, a comparison with a
different surgical method, such as CKC or LEEP, would be helpful
for demonstrating the validity of the S-T conization method.
In conclusion, the Shimodaira-Taniguchi conization
method was found to be effective regarding the surgical,
oncological, and obstetric outcomes. We found that older patients
with endocervical margin involvement had a higher incidence of
recurrence and postoperative cervical stenosis after therapeutic
conization than younger patients. A careful follow-up is required,
and a secondary hysterectomy should be considered in older patients
with endocervical margin involvement. Furthermore, to increase the
likelihood of term pregnancy after conization, a short interval of
≤3 months between conization and conception should be avoided.
Supplementary Material
Shimodaira-Taniguchi conization
method.
Supplementary Video
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
SH, YT, TD and YS conceptualized the study. SH, YT,
MS and YS contributed to the methodology. SH and YT handled the
software used. TD and MS validated the data. SH and YT confirm the
authenticity of all the raw data. SH and YT analyzed the data. SH,
YT, TD, MS and YS curated the data, wrote the original draft, and
reviewed and edited the manuscript. All authors read and approved
the final manuscript.
Ethics approval and consent to
participate
Ethical approval for the present study was obtained
from the Ethics Committee of Osaka Rosai Hospital (approval no.
2021-62; date of approval, September 30, 2021; Sakai, Japan), and
it was conducted in line with the guidelines of The Declaration of
Helsinki. The Institutional Review Board granted an opt-out
recruitment approach and waived the requirement for written
informed consent from each patient. The document of ethical
approval for the present study is available on the website of Osaka
Rosai Hospital.
Patient consent for publication
Patient consent for Video S1 was obtained.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ostör AG: Natural history of cervical
intraepithelial neoplasia: A critical review. Int J Gynecol Pathol.
12:186–192. 1993.PubMed/NCBI
|
|
2
|
Santesso N, Mustafa RA, Wiercioch W, Kehar
R, Gandhi S, Chen Y, Cheung A, Hopkins J, Khatib R, Ma B, et al:
Systematic reviews and meta-analyses of benefits and harms of
cryotherapy, LEEP, and cold knife conization to treat cervical
intraepithelial neoplasia. Int J Gynaecol Obstet. 132:266–271.
2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Tanaka Y, Ueda Y, Kakuda M, Kubota S,
Matsuzaki S, Iwamiya T, Okazawa A, Matsuzaki S, Hashimoto K,
Kobayashi E, et al: Predictors for recurrent/persistent high-grade
intraepithelial lesions and cervical stenosis after therapeutic
conization: A retrospective analysis of 522 cases. Int J Clin
Oncol. 22:921–926. 2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Ikeda M, Mikami M, Yasaka M, Enomoto T,
Kobayashi Y, Nagase S, Yokoyama M and Katabuchi H: Association of
menopause, aging and treatment procedures with positive margins
after therapeutic cervical conization for CIN 3: A retrospective
study of 8,856 patients by the Japan Society of Obstetrics and
Gynecology. J Gynecol Oncol. 32(e68)2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Matsumura M, Ota T, Takeshima N and
Takizawa K: Shimodaira-Taniguchi conization method: Its utility and
reliability. Int J Gynecol Cancer. 20:1025–1030. 2010.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Miyoshi Y, Miyatake T, Ueda Y, Morimoto A,
Yokoyama T, Matsuzaki S, Kimura T, Yoshino K, Fujita M, Ohashi H,
et al: Prediction, based on resection margins, of long-term outcome
of cervical intraepithelial neoplasia 3 treated by
Shimodaira-Taniguchi conization. Arch Gynecol Obstet.
285:1427–1432. 2012.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Kigure K, Nakamura K, Kitahara Y, Nakao K,
Hirakawa T, Rokukawa S, Ito M, Nishimura T, Ito I, Kagami I and
Itoga S: An electrical scalpel conization versus
Shimodaira-Taniguchi conization procedure for cervical
intraepithelial neoplasia. Medicine (Baltimore).
97(e12640)2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Kirkwood BR and Sterne JAC: Essential
medical statistics. 2nd edition. Blackwell, Oxford, pp168-169,
2003.
|
|
9
|
Kanda Y: Investigation of the freely
available easy-to-use software ‘EZR’ for medical statistics. Bone
Marrow Transplant. 48:452–458. 2013.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Kobayashi Y: Conization. Comprehensive
Gynecology and Obstetrics. In: Surgery for Gynecologic Cancer.
Mikami M (ed). Springer, pp43-54, 2019.
|
|
11
|
Hasegawa K, Torii Y, Kato R, Udagawa Y and
Fukasawa I: The problems of cervical conization for postmenopausal
patients. Eur J Gynaecol Oncol. 37:327–331. 2016.PubMed/NCBI
|
|
12
|
Bae HS, Chung YW, Kim T, Lee KW and Song
JY: The appropriate cone depth to avoid endocervical margin
involvement is dependent on age and disease severity. Acta Obstet
Gynecol Scand. 92:185–192. 2013.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Bogani G, DI Donato V, Sopracordevole F,
Ciavattini A, Ghelardi A, Lopez S, Simoncini T, Plotti F, Casarin
J, Serati M, et al: Recurrence rate after loop electrosurgical
excision procedure (LEEP) and laser Conization: A 5-year follow-up
study. Gynecol Oncol. 159:636–641. 2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Reich O, Pickel H, Lahousen M, Tamussino K
and Winter R: Cervical intraepithelial neoplasia III: Long-term
outcome after cold-knife conization with clear margins. Obstet
Gynecol. 97:428–430. 2001.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Reich O, Lahousen M, Pickel H, Tamussino K
and Winter R: Cervical intraepithelial neoplasia III: Long-term
follow-up after cold-knife conization with involved margins. Obstet
Gynecol. 99:193–196. 2002.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Ministry of Health, Labor and Welfare of
Japan: Vital Statistics of Japan, 2019. https://www.mhlw.go.jp/english/database/db-hw/dl/81-1a2en.pdf.
Accessed January 22, 2023.
|
|
17
|
Sasieni P, Castanon A, Landy R, Kyrgiou M,
Kitchener H, Quigley M, Poon L, Shennan A, Hollingworth A, Soutter
WP, et al: Risk of preterm birth following surgical treatment for
cervical disease: Executive summary of a recent symposium. BJOG.
123:1426–1429. 2016.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Himes KP and Simhan HN: Time from cervical
conization to pregnancy and preterm birth. Obstet Gynecol. 109 (2
Pt 1):314–319. 2007.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Heinonen A, Gissler M, Riska A, Paavonen
J, Tapper AM and Jakobsson M: Loop electrosurgical excision
procedure and the risk for preterm delivery. Obstet Gynecol.
121:1063–1068. 2013.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Conner SN, Cahill AG, Tuuli MG, Stamilio
DM, Odibo AO, Roehl KA and Macones GA: Interval from loop
electrosurgical excision procedure to pregnancy and pregnancy
outcomes. Obstet Gynecol. 122:1154–1159. 2013.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Noehr B, Jensen A, Frederiksen K, Tabor A
and Kjaer SK: Depth of cervical cone removed by loop
electrosurgical excision procedure and subsequent risk of
spontaneous preterm delivery. Obstet Gynecol. 114:1232–1238.
2009.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Bevis KS and Biggio JR: Cervical
conization and the risk of preterm delivery. Am J Obstet Gynecol.
205:19–27. 2011.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Kyrgiou M, Valasoulis G, Stasinou SM,
Founta C, Athanasiou A, Bennett P and Paraskevadis E: Proportion of
cervical excision for cervical intraepithelial neoplasia as a
predictor of pregnancy outcomes. Int J Gynaecol Obstet.
128:141–147. 2015.PubMed/NCBI View Article : Google Scholar
|