Introduction
Head and neck cancer, which occurs in the
oropharynx, hypopharynx, larynx, or cervical esophagus, is often
diagnosed at an advanced stage. Additionally, this type of cancer
can lead to tumors which are either synchronous or metachronous.
Although total pharyngolaryngectomy with cervical esophagectomy
(TPLCE) is a highly invasive procedure, it is the standard surgical
and effective treatment for these types of cancer (1-5).
In this procedure, tracheal necrosis (TRN) is a common
post-operative complication. Previous studies have demonstrated
that occurs in 6-20% of patients who undergo TPLCE (6-8).
However, there are only a limited number of studies available on
techniques that may be used to prevent TRN following TPLCE
(6,7). Thus, the present study aimed to
identify a technique that may be used to prevent TRN following
TPLCE and describes eight surgical processes that may be used for
this purpose.
Patients and methods
Patient information
From January, 2010 to December, 2019, 48 patients
underwent TPLCE at Nara Medical University (Kashihara, Japan). A
retrospective analysis of the clinical records was conducted and
the incidence of TRN was calculated. Moreover, eight surgical
techniques that may be used to prevent TRN were examined. The
present retrospective study was approved by the Ethics Committee of
Nara Medical University Hospital. Informed consent was obtained
from all patients for the publication of the study and any
accompanying images.
The patient information and clinical characteristics
are presented in Table I. In total,
4 patients were female, and 44 were male. The mean age was 66 years
(range, 44-86 years). In addition, 4 patients had oropharyngeal
cancer, 34 patients had hypopharyngeal cancer, 5 patients had
laryngeal cancer, and 5 patients had cervical esophageal cancer.
The grading of the tumors in the present study as per the TNM
classification system for cancers is presented in Tables II and III. In all patients, the tissue type was
histopathologically confirmed as squamous cell carcinoma (9). The results of p16 immunohistochemical
analysis were negative in all patients with oropharyngeal
cancer.
 | Table IBackground information of the patients
in the present study. |
Table I
Background information of the patients
in the present study.
| Parameter | No. of patients
(n=48) |
|---|
| Sex | |
|
Male | 44 |
|
Female | 4 |
| Mean age (range),
years | 66 (44-86) |
| Site of tumor | |
|
Oropharynx | 4 |
|
Hypopharynx | 34 |
|
Larynx | 5 |
|
Cervical
esophagus | 5 |
| Treatment | |
|
Only
surgery | 14 |
|
Surgery with
POCRT | 14 |
|
or PORT | |
|
Salvage
surgery after | 13 |
|
CRT, RT or
surgery | |
|
NAC and
surgery | 2 |
|
NAC and
surgery | |
|
with POCRT
or PORT | 5 |
 | Table IITNM classification of patients with
oropharyngeal, hypopharyngeal and laryngeal cancer (n=43). |
Table II
TNM classification of patients with
oropharyngeal, hypopharyngeal and laryngeal cancer (n=43).
| | T stage | |
|---|
| T stage | N0 | N1 | N2b | N2c | N3b | Total no. of
patients |
|---|
| T2 | 6 (3a) | 1 | 2 (1a) | 2 (1a) | 0 | 11 |
| T3 | 3 (2a) | 1 (1a) | 5 | 2 | 1 | 12 |
| T4a | 4 (1a) | 2 | 2 | 9 (1a) | 2 | 19 |
| T4b | 1 (1a) | 0 | 0 | 0 | 0 | 1 |
| Total | 14 | 4 | 9 | 13 | 3 | 43 |
 | Table IIITNM classification of patients with
cervical esophageal cancer (n=5). |
Table III
TNM classification of patients with
cervical esophageal cancer (n=5).
| | N stage | |
|---|
| T stage | N0 | N1 | N2 | Total no. of
patients |
|---|
| T2 | 0 | 1 | 1 | 2 |
| T3 | 2 (2a) | 0 | 0 | 2 |
| T4 | 0 | 1 | 0 | 1 |
| Total | 2 | 2 | 1 | 5 |
A total of 13 patients underwent TPLCE as salvage
treatment for recurrent or residual cancer following
chemoradiotherapy (CRT) or radiotherapy (RT) alone or recurrent
post-surgery. In addition, 7 patients underwent TPLCE following
neoadjuvant chemotherapy. Docetaxel, cisplatin and 5-fluorouracil
were administered as neoadjuvant chemotherapy. Cisplatin and
5-fluorouracil, cisplatin alone, carboplatin alone, or cetuximab
alone were administered as CRT, and the irradiation dose ranged
from 60-70 Gy. In total, 19 patients received post-operative RT or
CRT due to the histopathological diagnosis, including extra-nodal
spread and multiple cervical lymph node metastases. TRN as the
necrosis of membranes or cartilage of more than one tracheal
ring.
Surgical treatment
TPLCE was performed by a head and neck surgeon. All
patients underwent reconstruction with a free jejunal transfer,
which was performed to compensate for the defect of the cervical
digestive tract and was harvested by an abdominal surgeon.
Microvascular anastomosis of a free jejunal transfer was performed
by a plastic surgeon. Finally, pharyngo-jejunal and
jejunal-esophageal anastomoses were performed manually by head and
neck surgeons. Although the extent of neck dissection was dependent
on the location and size of lymph node metastasis in each patient,
all patients underwent at least an ipsilateral neck lymph node
dissection and paratracheal node dissection. In this surgery, the
cutting lines were set at least 20 mm away from the margin of the
tumor to ensure negative surgical margin. Therefore, in all cases,
cervical esophagus was included in the resected tissue. In the
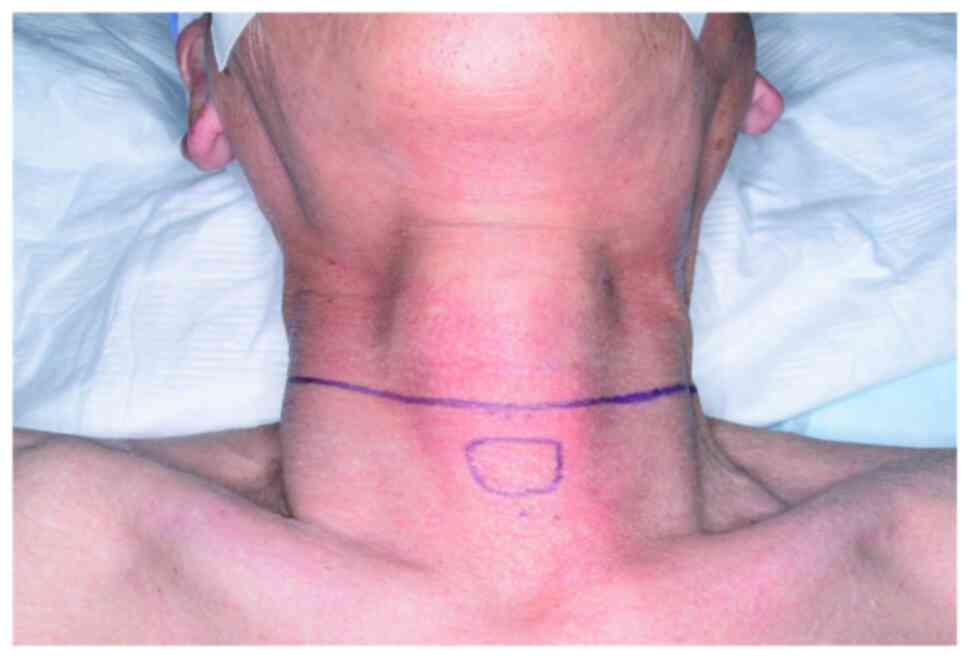
first process, a collar incision was applied to all patients who
underwent head and neck surgery as a cervical approach at Nara
Medical University (Fig. 1).
In tumor resections, care is taken so as not to peel
the esophageal membrane from the tracheal wall, as much as this is
possible, with the exception of cases in which there is tumor
invasion to the trachea in hypopharyngeal and laryngeal cancer and
in the case of esophageal cancer. At the same time, while peeling
this compartment, a scalpel was used instead of an electrocautery.
These methods comprised the second process.
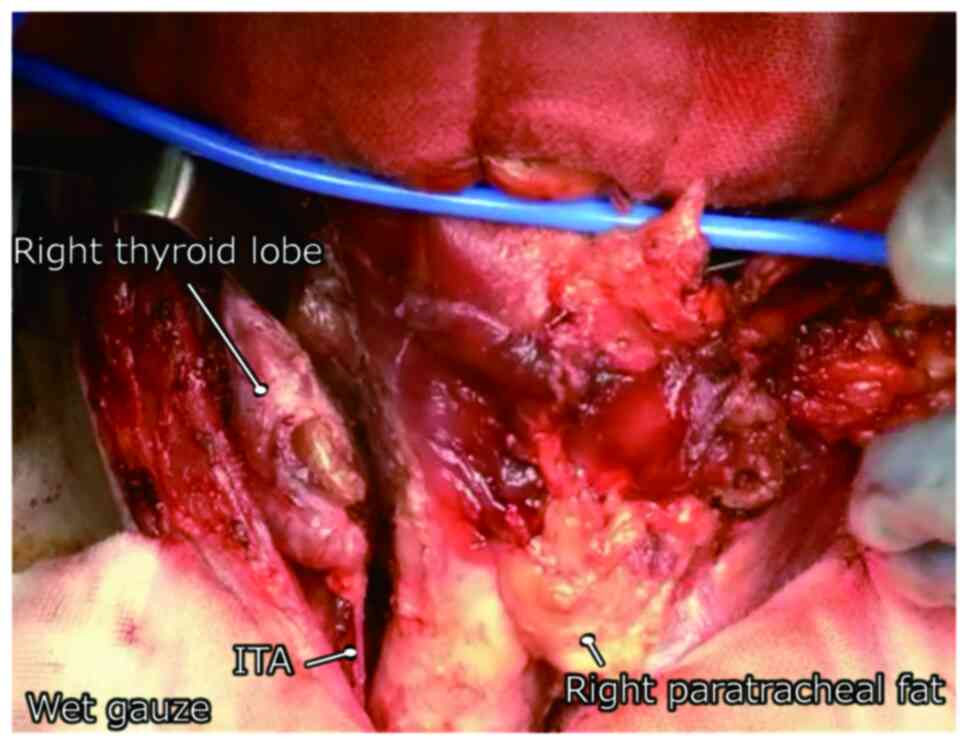
In the paratracheal operation, care was taken to
preserve the branches of the inferior thyroid artery (ITA) as a
third process (Fig. 2). When total
thyroidectomy or lobectomy is required in some cases, the ITA is
cut immediately in front of the thyroid gland. Hemostasis is
performed as little as possible, particularly on the surface of the
trachea, which indicates the fourth process. Immediately following
TPLCE, a small part of the tracheal edge was cut to examine the
blood supply to the trachea.
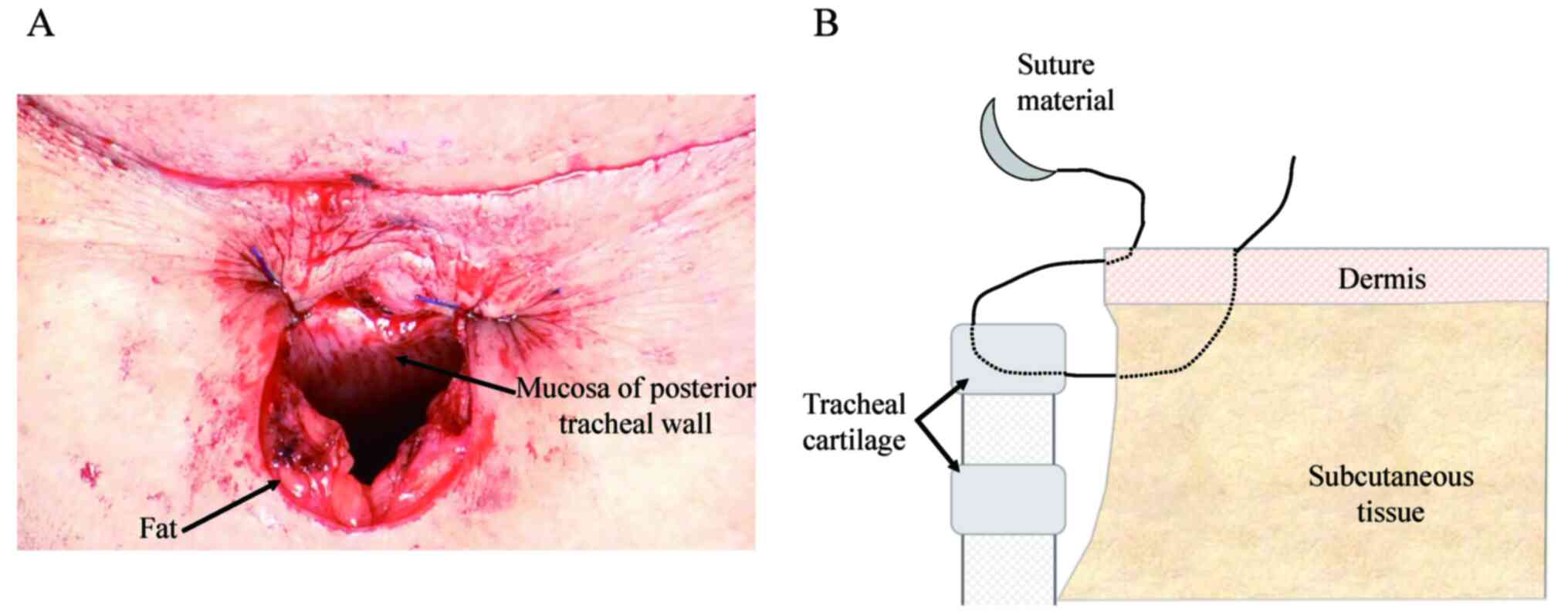
When forming the tracheal stoma, the subcutaneous
incision after denudation was designed, as shown in Fig. 3A during the fifth process. The
half-buried vertical mattress suture with non-absorbable thread was
applied to form the tracheal stoma, and the sutures were performed
at equal distances, which comprises the sixth process. First, the
half-buried vertical mattress suture starts from the epidermal side
to the tracheal side. The suture material crosses the wound and
tracheal cartilage, similar to a regular vertical mattress suture.
Second, the wound on the tracheal side did not cross when
returning. Finally, the subcutaneous edge on the epidermal side was
crossed, and a knot was made (Fig.
3B).
Surgical loupes magnification was used to view the
images more clearly and closely. In addition, the already operated
fields were covered with wet gauze to avoid drying. These are
routinely performed to preserve the small vessels and are defined
as the seventh and eighth processes.
Results
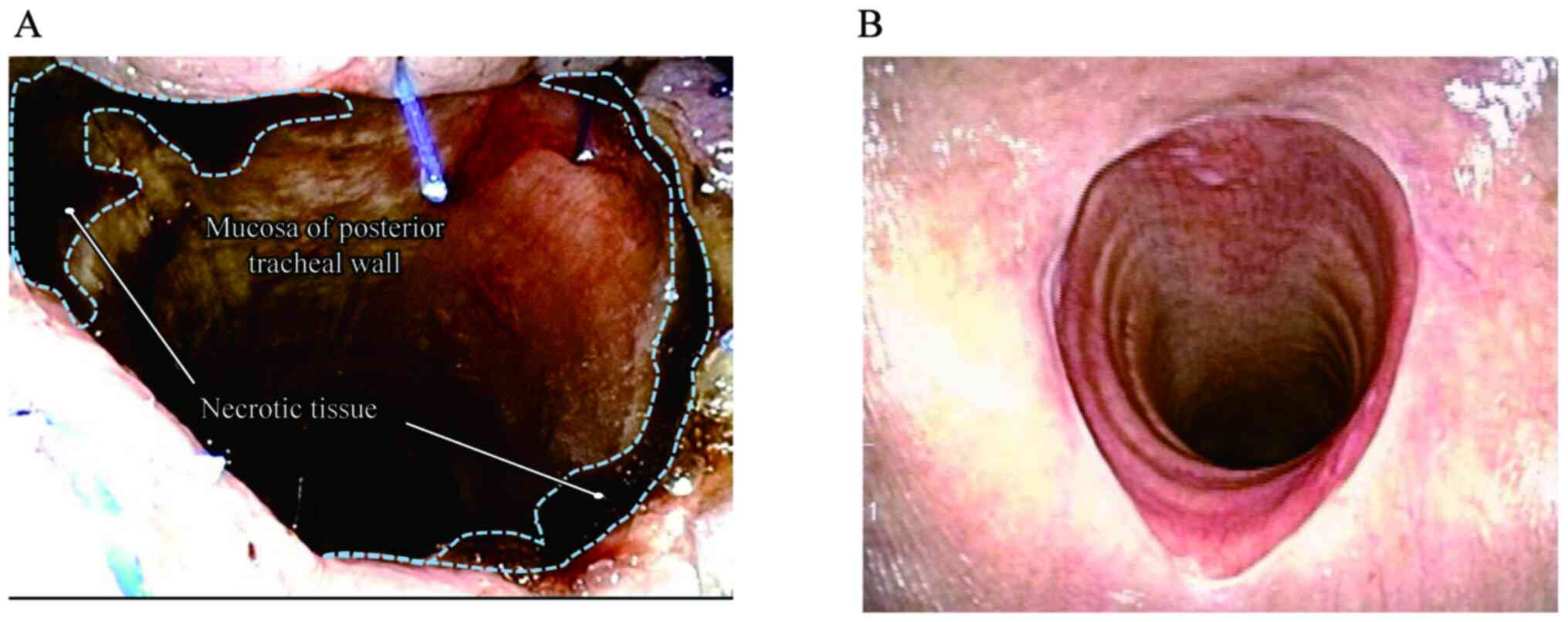
TRN developed in 3 patients (6%) within 1 week
following surgery. Additionally, all patients with TRN exhibited
necrosis within one tracheal ring (Fig.
4A). The clinical characteristics of the 3 patients with TRN
are presented in Table IV. Patient
1 underwent surgical debridement and tracheoplasty. As patient 2
experienced necrosis of the free jejunum simultaneously,
tracheoplasty and pharyngostomy were performed using a pectoral
major musculocutaneous flap. Patient 3 received only conservative
treatments, such as an ointment.
 | Table IVPatients with TRN following TPLCE. |
Table IV
Patients with TRN following TPLCE.
| Patient | Age, years | Sex | Comorbidity | Site | TNM | Preoperative
treatment | Neck dissection |
|---|
| 1 | 63 | Male | None | Ce | T2N2M0 | NAC | Bilateral neck and
bilateral paratracheal lymph node |
| 2 | 63 | Male | None | HP | T4aN2cM0 | None | Bilateral neck and
bilateral paratracheal lymph node |
| 3 | 69 | Male | DM, HT | HP | T3N3bM0 | None | Right lateral neck,
left lateral and posterior neck, and bilateral paratracheal lymph
node |
TRN developed in patients 1 and 2 before they
received post-operative CRT. TRN did not develop in any of the
other patients who received post-operative RT or CRT. Recurrence
around the tracheal stoma developed in only one out of the 48
patients (2%).
Consideration of the patients with
TRN
The reasons for the development of TRN in the 3
patients in the present study were as follows:
Patient 1 had a cervical esophageal carcinoma close
to the tracheal side (Fig. 5A). As
the tumor had to be resected up to the closest to the tracheal
wall, a number of ITA branches may have become damaged during this
procedure, which indicates that the second and third processes were
not fulfilled.
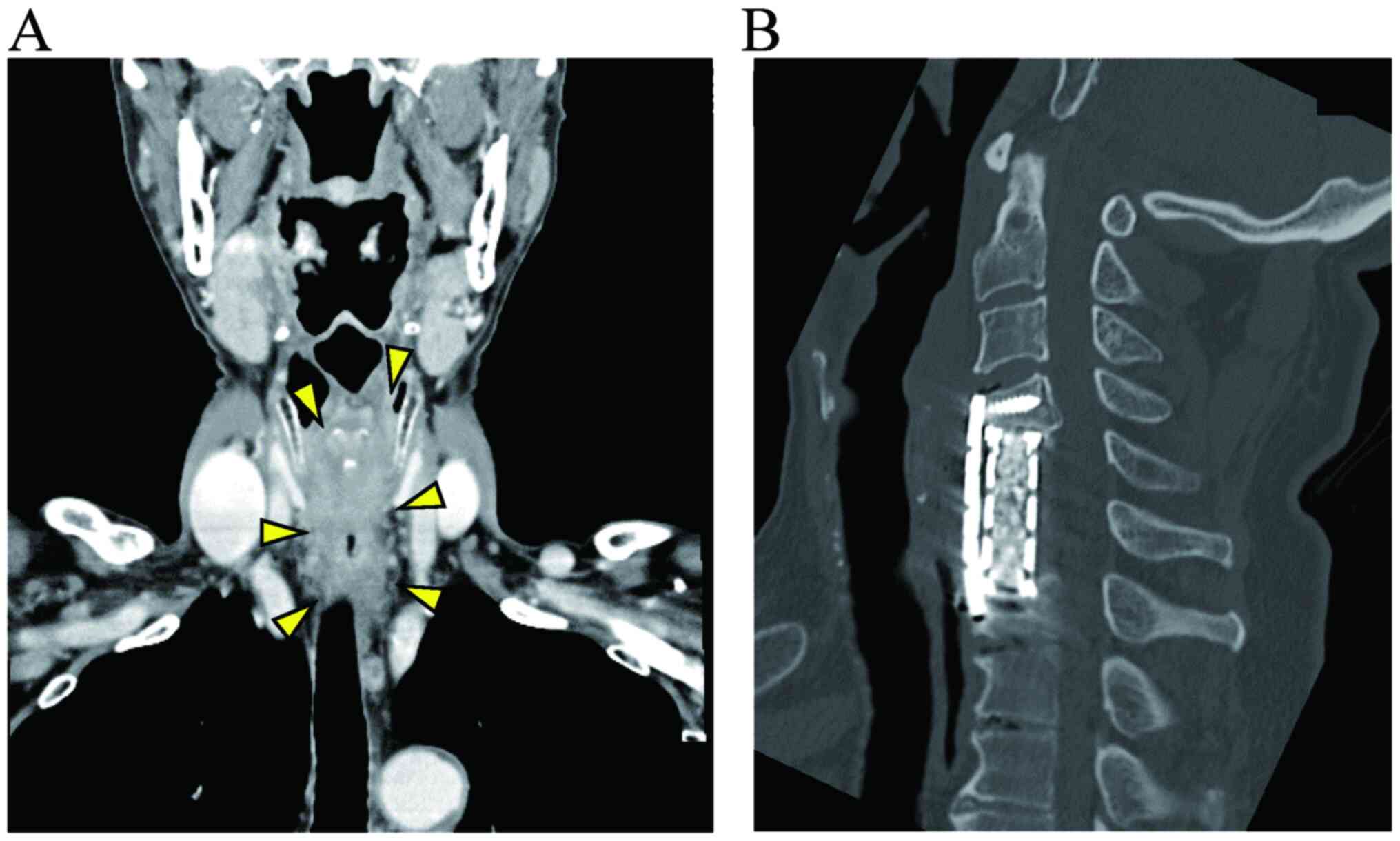
Patient 2 underwent anterior cervical discectomy and
fusion, and had a plate and screws (Fig.
5B). These materials were close to the tumor that they needed
to be removed at the same time. Therefore, the duration of the
surgery was lengthy, and the blood supply and tissue may have been
disrupted by dryness. Moreover, it was difficult to peel the
laryngopharynx and cervical esophagus from the surrounding tissue
due to the post-operative use of cicatrix due to anterior cervical
discectomy and fusion. In this procedure, several branches of the
ITA may have become damaged. A few days after the surgery, the free
jejunum was necrotized. Although this patient was salvaged by
tracheoplasty and pharyngostomy with a pectoral major
musculocutaneous flap, some processes could not be performed,
particularly the second and third, in the first surgery.
Patient 3 experienced TRN in only a small portion of
one tracheal ring. The preservation of the blood supply to the
trachea and the tissue around the tracheal stoma may be
insufficient, although care was taken with these eight processes.
Fortunately, the TRN improved only by application of an
ointment.
Discussion
TRN from an anatomical point of view. TRN is
one of the most commonly observed complications following TPLCE and
may lead to mortality. Nevertheless, there have been few reports
and detailed considerations from an anatomical point of view
(6,7). Moreover, a surgical strategy with which
to prevent TRN has not yet been established, at least to the best
of our knowledge.
The main blood supply to the trachea occurs via the
tracheoesophageal branches of the ITA and bronchial artery and the
innominate-subclavian system. Although there are some variations in
the branching pattern, the ITA is a particularly important conduit
for the cervical trachea. The branches of these arteries enter the
lateral walls of the trachea. They generally construct lateral
longitudinal anastomoses and run transversely around the tracheal
circumference to merge branches from the opposite side. The
membranous wall receives blood supply from the posterior branches
of the longitudinal anastomosis and branches of the esophageal
artery (10-13).
Eight processes for the prevention of TRN.
The preservation of the blood supply to the trachea is essential
for the prevention of TRN. The present study described eight
processes for the prevention of TRN.
In the first process, a collar incision helps to
preserve the supply of blood to the epithelium and maintain
postoperative neck flexibility (14). Adding a vertical incision, such as a
T-shaped incision, separates the epithelium into several segments,
cuts off more blood supply to the epithelium, and does not match
the neck striae.
The ITA mainly supplies blood to the cervical
trachea, and the preservation of the branches of this artery is
crucial (13). The second, third and
fourth processes focus on this procedure. Some branches of this
artery may be cut by peeling the esophagus from the trachea.
Additionally, a scalpel is recommended for peeling, as the heat of
the electrocautery may damage these branches. Researchers strive to
preserve the small vessels on the surface of the trachea, including
longitudinal anastomosis, by preventing unnecessary bleeding and
excessive devascularization as much as possible.
Some fats were not removed by setting the Y-shaped
subcutaneous incision in Fig. 3A to
form the tracheal stoma. These fats receive blood supply from the
epidermis, and tissues with blood supply can be applied to the
tracheal cartilage. Moreover, the dead space around the tracheal
cartilage can be decreased by these fats, which helps preserve
local complications such as infection.
The half-buried vertical mattress suture is often
used as a surgical technique and it sutures the two sides more
closely (15). The suture should be
performed at equal distances to ensure equal tension to the stoma.
Scar formation and granulation may be prevented by suturing both
sides closely (Fig. 4B).
In thyroid surgery, a medical binocular magnifying
glass reduces post-operative complications, such as
hypoparathyroidism and recurrent nerve paralysis, and is a safe and
effective technique (16-18).
Considering this evidence, medical binocular magnifying glass would
allow for a more detailed viewing, preventing unnecessary vascular
damage due to dissection and coagulation by surgical devices.
The tissue is sensitive to desiccation, which may
disrupt the blood supply. Dryness has already been shown to delay
wound healing (19,20). The dissected site is covered with wet
gauze to prevent tissue damage and preserve small vessels whenever
the site is not operated on. Intraoperatively, these gauzes were
kept moist by sprinkling water at appropriate time intervals.
Consideration for this study
In the present study, no patients experienced TRN
following RT or CRT, and TRN developed immediately after surgery.
It was thus considered that post-operative TRN mainly derived from
the surgical procedure and these eight processes were played an
important role in preserving the blood supply. These eight
processes can be applied by any surgeons, and there are few
recurrences around the tracheal stoma. In order to prevent TRN, the
preservation of the branches of the ITA is essential. Although, in
fact, there are some cases with unavoidable factors that may affect
the development of TRN, such as thyroidectomy and paratracheal node
dissection, the necessity of tracheal resection at a low level and
the difficulty in surgery due to pre-operative tracheostomy, care
is taken to preserve the blood supply to the trachea with the
current surgical technique. The current surgical technique is
effective at reducing the risk of developing TRN in cases with
these factors as well.
Due to the retrospective nature of the present
study, selection bias could not be avoided. Another limitation of
the study is the severity of the disease. In other hospitals,
surgeons may resect more aggressively owing to the advancement of
the disease.
In conclusion, to date, only a limited number of
studies have investigated TRN following TPLCE (6-8).
The present study described the incidence of TRN at Nara Medical
University and the surgical technique used. Knowledge regarding
detailed anatomical structures and intraoperative exertion will
lead to a decrease in the incidence of TRN. The authors hope that
the surgical processes described herein may help numerous patients.
Improved surgical techniques for the prevention of fatal
complications need to be further investigated.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
AT made substantial contributions to the conception
of the study and the acquisition of data, and drafted the
manuscript. HU, TM, IO, TKimura, HA, SA and TKitahara provided
cancer-related scientific inputs and collected clinical data. HU,
TM and TKitahara critically revised the manuscript. AT and TM
confirm the authenticity of all the raw data. All authors have
accepted responsibility for the entire content of this manuscript
and have approved the submission. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of Nara Medical University Hospital on April 28, 2021,
and the proposal number was 2977. All research subjects involved
provided consent for the reviewing of their clinical information
for the purposes of research.
Patient consent for publication
Patients have provided consent for the publication
of their personal data and related images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
McKee DM and Peters CR: Reconstruction of
the hypopharynx and cervical esophagus with microvascular jejunal
transplant. Clin Plast Surg. 5:305–312. 1978.PubMed/NCBI
|
|
2
|
Reece GP, Bengtson BP and Schusterman MA:
Reconstruction of the pharynx and cervical esophagus using free
jejunal transfer. Clin Plast Surg. 21:125–136. 1994.PubMed/NCBI
|
|
3
|
Ida S, Morita M, Hiyoshi Y, Ikeda K, Ando
K, Kimura Y, Saeki H, Oki E, Kusumoto T, Yoshida S, et al: Surgical
resection of hypopharynx and cervical esophageal cancer with a
history of esophagectomy for thoracic esophageal cancer. Ann Surg
Oncol. 21:1175–1181. 2014.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Schwartz LH, Ozsahin M, Zhang GN, Touboul
E, De Vataire F, Andolenko P, Lacau-Saint-Guily J, Laugier A and
Schlienger M: Synchronous and metachronous head and neck
carcinomas. Cancer. 74:1933–1938. 1994.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Erkal HS, Mendenhall WM, Amdur RJ,
Villaret DB and Stringer SP: Synchronous and metachronous squamous
cell carcinomas of the head and neck mucosal sites. J Clin Oncol.
19:1358–1362. 2001.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Fujiki M, Miyamoto S, Sakuraba M,
Nagamatsu S and Hayashi R: Risk factors for tracheal necrosis after
total pharyngolaryngectomy. Head Neck. 37:1207–1210.
2015.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Kamiyama R, Mitani H, Yonekawa H,
Fukushima H, Sasaki T, Shimbashi W, Seto A, Koizumi Y, Ebina A and
Kawabata K: A clinical study of pharyngolaryngectomy with total
esophagectomy: Postoperative complications, countermeasures, and
prognoses. Otolaryngol Head Neck Surg. 153:392–399. 2015.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Miyamoto S, Nakao J, Higashino T,
Yoshimoto S, Hayashi R and Sakuraba M: Clavien-Dindo classification
for grading complications after total pharyngolaryngectomy and free
jejunum transfer. PLoS One. 14(e0222570)2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Brierley JD, Gospodarowicz MK and
Wittekind C (eds): TNM Classification of Malignant Tumours, 8th
Edition. John Wiley & Sons, Inc., Hoboken NJ, 2017.
|
|
10
|
Grillo HC: Surgery of the trachea. Curr
Probl Surg. 3–59. 1970.PubMed/NCBI
|
|
11
|
Salassa JR, Pearson BW and Payne WS: Gross
and microscopical blood supply of the trachea. Ann Thorac Surg.
24:100–107. 1977.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Minnich DJ and Mathisen DJ: Anatomy of the
trachea, carina, and bronchi. Thorac Surg Clin. 17:571–585.
2007.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Miura T and Grillo HC: The contribution of
the inferior thyroid artery to the blood supply of the human
trachea. Surg Gynecol Obstet. 123:99–102. 1966.PubMed/NCBI
|
|
14
|
Grillo HC: Surgical approaches to the
trachea. Surg Gynecol Obstet. 129:347–352. 1969.PubMed/NCBI
|
|
15
|
Wu W, Chavez-Frazier A, Migden M and
Nguyen T: The buried half horizontal, half vertical mattress
suture: A novel technique for wound edges of unequal lengths.
Dermatol Surg. 42:1391–1393. 2016.PubMed/NCBI View Article : Google Scholar
|
|
16
|
D'Orazi V, Panunzi A, Di Lorenzo E and
Ortensi A, Cialini M, Anichini S and Ortensi A: Use of loupes
magnification and microsurgical technique in thyroid surgery: Ten
years experience in a single center. G Chir. 37:101–107.
2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Pata G, Casella C, Mittempergher F,
Cirillo L and Salerni B: Loupe magnification reduces postoperative
hypocalcemia after total thyroidectomy. Am Surg. 76:1345–1350.
2010.PubMed/NCBI
|
|
18
|
Testini M, Nacchiero M, Piccinni G,
Portincasa P, Di Venere B, Lissidini G and Bonomo GM: Total
thyroidectomy is improved by loupe magnification. Microsurgery.
24:39–42. 2004.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Ousey K, Cutting KF, Rogers AA and Rippon
MG: The importance of hydration in wound healing: reinvigorating
the clinical perspective. J Wound Care. 25:122. 24–30.
2016.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Lumbers M: Understanding and addressing
dryness during wound healing. Br J Community Nurs. 24 (Suppl
6):11–14. 2019.PubMed/NCBI View Article : Google Scholar
|