1. Introduction
The ‘7th Workshop on Paediatric Virology’ was held
virtually, due to the current coronavirus disease 2019 (COVID-19)
pandemic, on December 20, 2021. The workshop was organised by the
Institute of Paediatric Virology, which is located on the Island of
Euboea in Greece (1) (for further
information about the Institute of Paediatric Virology please visit
its official website at https://paediatricvirology.org). The workshop was
chaired by Dr Simon B. Drysdale, Consultant and Honorary Senior
Lecturer in Paediatric Infectious Diseases at St. George's
University Hospital NHS Trust and St. George's University of
London, UK (Chair of the ‘7th Workshop on Paediatric Virology’) and
Professor Anna Kramvis, Research Professor of Molecular Virology at
the University of the Witwatersrand in Johannesburg, South Africa
(Honorary Chair of the ‘7th Workshop on Paediatric Virology’). Dr
John Papadatos, former Clinical Director and Consultant Paediatric
Intensivist at the ‘Aglaia Kyriakou’ Children's Hospital in Athens,
Greece, was awarded with the ‘2021 George N. Papanicolaou
Humanitarian Award’ for his contribution in founding paediatric
intensive care in Greece (2). Mrs.
Vassiliki Rabaouni, High School Teacher of Hellenic Literature at
the ‘Zosimaia’ School of Ioannina, Greece and Coordinator during
the academic year 2020-2021 of the High School educational
programme entitled ‘From ‘nouson kakin’ of Homer to COVID-19’ (‘Από
την ‘νοῦσον κακήν’ του Ομήρου στον COVID-19’), was also awarded
with the ‘2021 Paediatric Virology Award’ for her contribution to
teaching high school students about severe acute respiratory
syndrome coronavirus 2 (SARS-CoV-2) infection (for further
information on ‘Zosimaia’ School of Ioannina please visit:
https://gym-zosim.ioa.sch.gr/).
The aim of the present review article is to provide
an overview of the key messages of the plenary lectures presented
at the ‘7th Workshop on Paediatric Virology’. The topics, which
were covered during the workshop, were the following: i) Viral
pandemics and epidemics in the ancient Mediterranean; ii) the
impact of obesity on the outcome of viral infections in children
and adolescents; and iii) COVID-19 and artificial intelligence
(Table I).
 | Table IThe top key messages of the ‘7th
Workshop on Paediatric Virology’ organised virtually by the
Institute of Paediatric Virology. |
Table I
The top key messages of the ‘7th
Workshop on Paediatric Virology’ organised virtually by the
Institute of Paediatric Virology.
| Viral epidemics in
the ancient Mediterranean | The most extensive
descriptions of infectious diseases in ancient Greece, including
viral epidemics, are derived from the ‘Hippocratic Corpus’ written
by Hippocrates, who reported the ‘cough of Perinthos’ epidemic in
the 5th century BC. |
| | Smallpox is a
strong candidate for the cause, or one of the causes, of the
well-known 5th century BC ‘Plague of Athens’ described by
Thucydides. |
| | Developments in the
recovery and identification of ancient pathogens' genomes are
expected to facilitate the identification of several viral
diseases. |
| Viral infections
and obesity | The world is
currently in the middle of two pandemics that have unfortunately
collided: Paediatric obesity has undergone an unprecedented
increase over the past decades with exponential rates during the
COVID-19 pandemic. |
| | The present review
of real-world data demonstrated that obese children and adolescents
have more severe outcomes in viral infections. |
| COVID-19 and
AI | AI technology
models can be of tremendous help during the ongoing COVID-19
pandemic. |
| | The use of AI can
easily track the spread of SARS-CoV-2, identify high-risk patients,
control the infection in real-time, predict mortality risk by
adequately analysing previous data of patients, fight against the
virus by population screening, medical help, notification and
suggestions about infection control, improve the planning,
treatment and reported outcomes of COVID-19 and reduce the workload
of healthcare workers. |
| | AI can be very
useful in drug delivery design and development, identifying useful
molecules at a much faster rate than usual and is also helpful for
clinical trials. |
| | However, such use
of information and big data raise ethical, legal and constitutional
issues that have to be carefully evaluated in order protect
humanity and human rights. |
2. Viral pandemics and epidemics in the
ancient Mediterranean: An overview
As the world begins to emerge from the devastation
of COVID-19, it is useful to remember that this is not the first
pandemic that human beings have survived. The ancient world
suffered through numerous pandemic and epidemic events, some of
which are lost to history. However, there is historical evidence of
several epidemics and pandemics, particularly in the ancient
Mediterranean. The evidence for these diseases comes from a number
of sources. First, of course, are the surviving ancient writings,
from physicians such as Hippocrates, Galen and Dioscourides
(3). The most extensive descriptions
of infectious diseases, including viral epidemics, are derived from
the ‘Hippocratic Corpus’ written by Hippocrates, who reported the
‘cough of Perinthos’ epidemic, an influenza-like outbreak in the
5th century B.C., and discussed in detail several cases
complicated with pneumonia or fatal outcome (4,5). Poets,
ancient historians, philosophers and general scientists, such as
Homer, Aristotle, Thucydides, Theophrastus, Lucretius and Pliny all
contributed to the current knowledge of the symptoms and social
impacts of epidemics; however, the identification of specific
diseases is impeded by their perspectives on the cause of diseases,
which frequently obscure the clear description of the symptoms
(6).
With a few historical exceptions, for the
identification of ancient epidemics, one must turn to the physical
remains of the victims. Mass burials or hastily constructed graves
provide information of catastrophic mortality events, and in the
absence of evidence for trauma, epidemics are usually suspected.
Moreover, unless the patient survives for several weeks, few
diseases leave evidence on bones, and the majority of these
diseases are bacterial, rather than viral. The mycobacterial
diseases, leprosy and tuberculosis, have a particular affinity for
bone in patients with chronic disease, and produce distinctive
changes to the skeleton; these are almost never diagnosed with a
degree of certainty, but rather represent the most probable cause
of the preserved lesions (7-9).
Bacteria are the source of the more well-known historical
epidemics, including the Plague, which first appeared in the reign
of the Roman emperor Justinian and was caused by Yersinia
pestis (10,11).
Viral epidemics are more elusive, as few viruses
directly affect bones in a manner that can lead to gross lesions
(8). When lesions are present, it is
difficult to identify the cause. Otitis and meningoencephalitis can
produce endocranial lytic lesions in the cranial vault and petrous
temporals; both diseases are described in the Hippocratic writings;
however, the specific infectious agent remains unknown (5). Lesions and bone formation on the
pleural surfaces of ribs are considered to be caused by infections,
usually bacterial or viral, although fungi, renal disease, cancer
and trauma may all be responsible, thus rendering the
identification of the causal agent more complex (12).
Developments in the recovery and identification of
ancient pathogen DNA have facilitated the identification of viral
diseases. Smallpox (Variola) periodically entered the
Mediterranean countries as early as the Bronze Age (13). The mummy of Pharaoh Ramses V (died in
1157 BC) exhibits the characteristic skin lesions of smallpox, and
variola virus DNA has been recovered from his remains (5). Smallpox is also one of the strong
candidates for the cause, or one of the causes, of the well-known
5th century BC ‘Plague of Athens’ described by
Thucydides (14). To date, only
typhoid fever has been identified in a small number of samples
obtained from a mass grave considered to be associated with the
event (15,16); but typhoid would have been endemic
and is unlikely to have caused the catastrophic infections in all
age groups described by Thucydides (14). Although smallpox reappeared over
millennia in the Eastern Mediterranean, populations were almost
certainly small enough that it would die out completely after a few
years. As a result, subsequent introductions of the disease would
find a population in which no one had any immunity, with
devastating effects each time (17).
Ancient writers describe the effects of other viral
diseases that can be tentatively identified as poliomyelitis,
chicken pox, shingles, hepatitis, mumps, herpes and others
(3,6). The majority of diseases have no
skeletal symptoms, although limb paralysis from poliomyelitis has
been tentatively identified through atrophied and shortened leg
bones, while histology and advanced imaging techniques have been
shown to aid in the diagnosis of less grossly obvious specimens
(18). However, as the recovery and
amplification techniques for viral DNA improve and the analyses
become both more affordable and common, it can be anticipated that
diseases that lack skeletal symptoms may finally be identified;
thus, more in-depth knowledge of the history of viral diseases in
the Mediterranean may be acquired.
3. The impact of obesity on the outcome of
viral infections in children and adolescents
The association between obesity and viral infections
has been studied for a number of years and in particular during the
2009 H1N1 influenza pandemic, when obese patients were considered
at an increased risk of influenza-related complications, a longer
intensive care unit (ICU) stay and a higher mortality (19,20).
Moreover, there is increasing evidence that the immune response of
obese patients is also impaired in other viral infections, such as
dengue and respiratory viruses, including the current SARS-CoV-2
pandemic strain. As data are limited and conflicting regarding the
paediatric population, the present study aimed to systematically
review the impact of obesity on the outcome of viral infections of
interest in order to provide insight into the prognosis and early
treatment of this subset of patients.
In the context of the ‘7th Workshop on Paediatric
Virology’, Dr Patra Koletsi and Dr Dimitra-Irinna Vitoratou
systematically reviewed published studies reporting on obesity or
body mass index (BMI) and their association with the outcome of
viral infections (21-40).
PubMed was searched for articles published up to August 30, 2021,
using the following terms: (obesity OR BMI OR metabolic syndrome)
AND (viral infection OR virus* OR influenza OR COVID-19 OR
SARS-CoV-2) AND (child OR adolescent). The PROSPERO registry was
searched for relevant review articles. The citations of selected
articles and relevant review articles were manually searched.
Subsequently, the two reviewers (PK and DIV) independently screened
the abstracts of the retrieved articles. From each article included
in the review, the following data were recorded: The study design,
study population number, age, country and month/year of enrolment.
In studies that included adult populations, the data referring to
children and adolescents were extracted. Conversely, studies
reporting on respiratory syncytial virus (RSV) including toddlers
and infants <2 years old were excluded, as obesity is not a
well-defined pathological condition in this subset of patients.
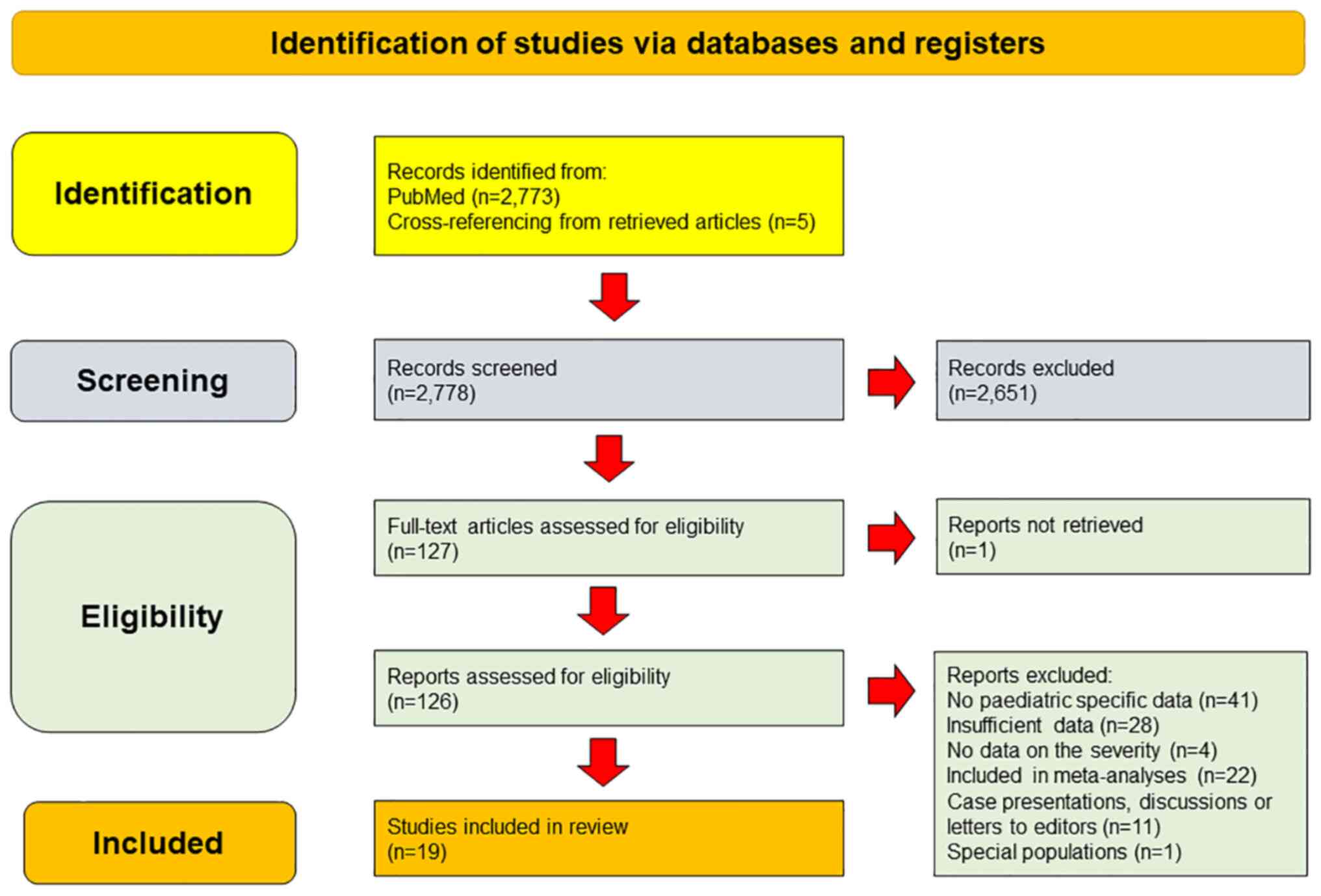
Among the 2,278 citations initially retrieved from
PubMed, 19 studies were identified as eligible for inclusion in the
review. The flow chart for the process of selection of included
studies in the review is illustrated in Fig. 1. The majority of studies used the
standard World Health Organization (WHO) or Centers for Disease
Control and Prevention (CDC) criteria to define obesity (see
https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
and https://www.cdc.gov/obesity/childhood/defining.html,
respectively). According to the WHO, for children <5 years of
age, obesity is considered when the weight-for-length/height score
is >3 standard deviations above the WHO Child Growth Standards
median (charts available at: https://cdn.who.int/media/docs/default-source/child-growth/child-growth-standards/indicators/weight-for-length-height/cht-wflh-boys-z-0-5.pdf?sfvrsn=6bcd4d28_11;
and https://cdn.who.int/media/docs/default-source/child-growth/child-growth-standards/indicators/weight-for-length-height/cht-wflh-girls-z-0-5.pdf?sfvrsn=7abd186d_9;
for boys and girls, respectively). For children aged between 5-19
years, obesity is considered when the z-score is >2 standard
deviations above the WHO Growth Reference median (charts available
at: https://cdn.who.int/media/docs/default-source/child-growth/growth-reference-5-19-years/bmi-for-age-(5-19-years)/bmifa-boys-z-5-19-labels.pdf?sfvrsn=5775aced_4;
and https://cdn.who.int/media/docs/default-source/child-growth/growth-reference-5-19-years/bmi-for-age-(5-19-years)/bmifa-girls-z-5-19-labels.pdf?sfvrsn=94b20617_4;
for boys and girls, respectively). According to the CDC, for a
child >2 years of age, obesity is defined as a BMI
≥95th percentile of the CDC sex-specific BMI-for-age
growth charts (charts available at: https://www.cdc.gov/growthcharts/data/set1clinical/cj41c023.pdf;
and https://www.cdc.gov/growthcharts/data/set1clinical/cj41c024.pdf;
for boys and girls, respectively). BMI is calculated by dividing
the weight of an individual in kg by the square of height in
meters.
The data extracted from each of the included studies
are presented in Table II. As
regards COVID-19, three out of four studies with a total population
aged <22 years of >44,000, identified obesity as a
significant risk factor for severe disease and subsequent
hospitalization (21-24).
That said, a surveillance study from Mexico (23) found a significant association with
progression to pneumonia only when combined with patients diagnosed
with type 2 diabetes. All three observational studies on
multisystem inflammatory syndrome in children (MIS-C) found a high
prevalence of obesity among paediatric patients of >25%.
However, the lack of cross-sectional design does not allow for firm
conclusions to be drawn. Likewise, among the eight influenza and
influenza-like illness (ILI) studies included in the review, four
studies (28,31,33,35)
revealed an unfavourable outcome for disease severity, the risk of
hospitalization and mortality, while the other four (29,30,32,34) did
not demonstrate a significant impact of obesity among children and
adolescents. Furthermore, obesity was associated with a greater
number of days of wheezing, fever and drip infusion in RSV
infection in toddlers and preschool children (36), and higher odds of developing severe
dengue infection (39). Finally, two
studies were identified referring to chronic hepatitis C, where
obesity was significantly associated with progression to liver
fibrosis and impaired sustained virologic response to treatment
(37,38).
 | Table IICharacteristics of studies included
in the narrative review on the impact of obesity on the outcome of
viral infections. |
Table II
Characteristics of studies included
in the narrative review on the impact of obesity on the outcome of
viral infections.
| Authors/(Refs.),
year | Study design | Setting: N; age
range; study population; country; month/year of enrolment | % Obesity in
studied populationsa | Outcome |
|---|
| COVID-19 | | | | |
| Kompaniyets
(21), 2021 |
Cross-sectional | 43,465 patients ≤18
years, USA (900 geographically dispersed USA hospitals;
03/2020-01/2021 | 2.5% | Strong risk factor
for hospitalization (aRR, 3.07; 95% CI, 2.66-3.54), but not for
severe COVID-19 infection |
| Tsankov et
al (22), 2021 | Meta-analysis and
systematic review (cross-sectional sub-analysis) | 6 of 42 studies
referring to 275,661 patients <21 years of age without and 9,353
children with comorbidities; international; 01/2020-10/2020 | NA | Obese children had
a higher relative RR for severe COVID-19 and associated mortality
compared to children without co-morbidities (RR, 2.87; 95% CI,
1.16-7.07; I2=36%) |
| Moreno-Noguez et al
(23), 2021 | Retrospective
surveillance study | 1,443 patients with
COVID-19 <19 years old; Mexico; 12/2019-03/2020 | 5.7% | Obesity not shown
to be a significant risk factor for COVID-19 pneumonia; however,
the combination of obesity/type-2 diabetes yielded an OR of 2.9
(OR, 2.9; 95% CI, 1.75-4.95) |
| Webb and Osburn
(24), 2021 | Retrospective case
series | 163 patients with
COVID-19 <22 years old; California; 05/2020-09/2020 | 27% | Significant
association for obesity: 19% of incidentally infected and 22% of
potentially symptomatic were obese vs. 60% of significantly
symptomatic patients (P=0.001) |
| MIS-C | | | | |
| Abrams et al
(25), 2021 | Retrospective
surveillance study (CDC MIS-C database) | 1,080 patients
<21 years old; USA; 03/2020-10/2020 | 26% | 29.2% of patients
admitted to the ICU were obese compared to 22% that were not
admitted; obesity was linked to decreased cardiac function (aOR,
1.4; 95% CI, 1.0-1.9) and further ICU admission |
| Bautista-Rodriguez
et al (26), 2021 | Retrospective
web-based data review of case series | 183 patients ≤18
years old; age range, 2.3-11.7 years; international;
03/2020-06/2020 | 26.2% (most common
co-morbidity) | There was no
difference in obesity rates between the groups that presented with
KD-like presentation, incomplete KD-like presentation or shock
presentation (P=0.57) |
| Hoste et al
(27), 2021 | Systematic
review | 953 patients with
MIS-C, age range, 0-21 years; 12/2019-08/2020 | 25.3% | 4/18 (22.2%) among
fatal cases were obese |
| Influenza/ILI | | | | |
| Moser et al
(28), 2019 | Observational
cohort | 1,530 patients
<19 years old with influenza or ILI; Mexico;
04/2010-03/2014 | 6.4% | Obese paediatric
participants were more likely to develop severe ILI compared to
their counterparts with a normal z-score (OR, 2.2; P=0.002); no
significant interactions between BMI and different pathogen groups
(influenza H1N1, H3N2 and B, coronavirus, metapneumovirus,
parainfluenza, and rhinovirus, RSV) |
| Neyer et al
(29), 2018 | Retrospective | 188 children with
severe influenza complications; USA; age range, 2-20 years;
08/2010-06/2013 | 8% | The association
between severe obesity and known high-risk condition (e.g., asthma,
pneumonia, diabetes) for influenza complications (hospitalization
or mortality) was not significant (P=0.61) |
| Bagdure et
al (30), 2010 | Retrospective | 80 of 301 children
< 18 years of age admitted to the ICU for severe 2009
H1N1influenza; USA; 05/2009-11/2009 | 19% | Obesity was not
associated with ICU admission (P=0.45) |
| Okubo et al
(31), 2018 | Retrospective | 27,781 children
<18 years of age hospitalized with bronchitis or pneumonia and
influenza,Japan; 07/2010-03/2015 | 9.9% | Obese patients were
younger (P<0.001), more likely to be male (P<0.001), more
likely to be hospitalized in winter, and more likely to be treated
with antivirals (P<0.001) than underweight, normal weight or
overweight children; no association was found between obesity and
the likelihood of ICU admission, mean total costs of
hospitalization or length of hospital stay |
| Morgan et al
(32), 2010 | Case-cohort | 11,660 patients
with 2009 H1N1 influenza vs. 71,228 controls; age range, 2-19
years; USA; 05/2009-07/2009 | 16.4% | No association was
found between being obese and hospitalization among those with or
without chronic medical conditions (OR, 2.2; 95% Cl, 0.4-13.4;
P=0.4); no association between BMI category and mortality (OR, 0.5;
95% Cl, <0.01-68; P=0.81) for children with or without chronic
medical conditions |
| Yu et al
(33), 2011 | Retrospective | 3,577 patients with
2009 H1N1 influenza; age range, 2-17 years; China;
09/2009-02/2010 | 12% | The proportion of
individuals with obesity was significantly higher among patients
with severe illness (patients admitted to the ICU) than among case
patients with non-severe illness (OR, 1.34; 95% Cl, 1.10-1.63;
P=0.004); the proportion of individuals with obesity was higher
among patients with non-severe illness than among the general
population (18% vs. 2%; OR, 10.45; 95% CI, 9.49-11.52) |
| Gill et al
(34), 2015 | Review and
meta-analysis | 5 of 27 studies
including 1,782 children with influenza or ILI; age range, 0-19
years; 1980-2010 | 19% | Obesity was not a
risk factor for hospital admission (OR, 0.99; 95% Cl,
0.61-1.62) |
| Garcia et al
(35), 2015 | Retrospective | 696 children with
2009 H1N1 influenza; age range, 0-18 years; Texas, USA;
04/2009-06/2010 | 1.9% (probably
under-reported) | Obesity was
associated with greater disease severity (aOR, 3.28; 95% Cl,
1.05-10.21; P=0.04) |
| RSV infection | | | | |
| Akiyama et
al (36), 2011 | Retrospective | 243 patients with
RSV bronchiolitis or pneumonia, age range, 1-6 years; Japan;
01/2000-12/2008 | NA | When the obesity
ratiob was ≤6, the days
of wheezing exhibited a significant negative association with
obesity ratios (OR, 0.13; 95% Cl, -0.21-0.05; P=0.001); when the
obesity ratio was >6, the days of wheezing (OR, 0.19; 95% Cl,
0.06-0.31; P=0.004), days of fever after admission (OR, 0.07; 95%
Cl, 0.01-0.14; P=0.021) and days of drip infusion (OR, 0.15; 95%
Cl, 0.07-0.24; P=0.001) exhibited a significant positive
association with obesity ratios |
| HCV Infection | | | | |
| Pokorska-Śpiewak
et al (37), 2015 | Retrospective | 42 children with
chronic hepatitis C infection; age range, 7-14.4 years; Poland;
2002-2013 | 17% | BMI z-score was
independent positive predictor of progression to liver fibrosis
(P=0.03); BMI was not associated with the presence of lymphoid
aggregates or steatosis |
| Delgado-Borrego
et al (38), 2010 | Retrospective | 123; age range,
4.6-19.8 years; Boston, MA, USA; 06/1993-06/2007 | Overweight and
obese (29.3%) | The presence of
steatosis was significantly associated with higher mean (±SE) BMI
percentiles [72nd (±5.8) vs. 58th (±3.5) percentile, P=0.04];
non-responders to treatment had a higher mean (±SE) BMI percentile
(70th ± 7.4) when compared to responders (50th ± 6.5) in univariate
and multivariate analyses (P=0.04 and P=0.02, respectively); one
standard deviation increase in baseline BMI z-score is associated
with a 12% decrease in the probability of a sustained virological
response |
| Dengue virus | | | | |
| Zulkipli et
al (39), 2018 | Review and
meta-analysis | 15 studies, 7,133
patients; age range, 0-18 years with dengue fever; international;
2000-2016 | NAc | 38% higher odds of
developing severe dengue infection among obesec children compared
to non-obese children (OR, 1.38; 95% CI, 1.10-1.73; P=0.01;
I2=36.7%) |
The literature review demonstrated the unfavourable
implication of obesity on the outcome of respiratory, as well as
vector-and blood-borne infectious diseases in children and
adolescents. Translational studies have indicated that obesity is
characterized by chronic low-grade inflammation with a disrupted
balance between pro- (e.g., IL-6, TNF-α, IL-1β and leptin) and
anti-inflammatory (e.g., IL-10 and adiponectin) cytokines, leaning
towards an overall pro-inflammatory state (40-42).
Cardiovascular changes in obesity, such as left heart hypertrophy
and high blood pressure, that lead to endothelial injury, have been
recognized even in very young children. Specifically, for COVID-19,
human post-mortem studies have demonstrated the inclusion of
coronavirus particles in endothelial cells, possibly via the
angiotensin-converting enzyme 2 receptors, as well as the
accumulation of inflammatory cells, pulmonary venous congestion and
intestinal endothelial inflammation (42,43).
Leptin, the levels of which are usually elevated in obese patients,
damages the endothelium, leading to less nitric oxide production
and modulates the innate and adaptive immune response leading to
inflammation aggravation. Furthermore, obese children and
adolescents appear to have higher influenza viral loads in exhaled
droplets compared with their leaner counterparts and shed the virus
for longer periods of time (42).
Similarly, adiponectin, the levels of which are
reduced in obese patients, has been demonstrated to exert a
protective effect against Fas-mediated hepatocyte death (37,38).
This subsequently affects regulatory processes, which are critical
in inflammatory and immune responses that drive the outcome in
hepatis C virus infection (38).
Finally, in obese patients with dengue infection, the increased
production of IL-6, IL-8 and TNF-α by adipose tissue increases
capillary permeability, which further contributes to the process of
severe plasma leakage (39). Given
the substantial increase in obesity rates in children during the
current pandemic induced by the prolonged quarantine durations and
the reduced physical activity, public health policies need to be
urgently redirected to the prevention of excess weight gain in
children. Improving the metabolic health and immunity of children
may be an effective preventive measure for counteracting the
consequences of viral infectious diseases.
4. COVID-19 and artificial intelligence
SARS-CoV-2 has caused an unprecedented pandemic
viral threat globally, which is still in progress (44-47).
To date, it has affected human life in several aspects, not only
through the loss of millions of individuals worldwide, but also
through the implementation of unprecedented and particularly strict
measures that modern societies could never have conceived. For the
first time, in a time of peace, the Olympic Games were postponed.
However, such decisions have a marked impact on economic,
educational, psycho-emotional and social levels, causing an
additional worldwide crisis, the results of which may have not yet
been fully observed.
The early identification of infected individuals,
whether they are in the pre-symptomatic, asymptomatic or
symptomatic stage, their isolation by monitoring their health and
the simultaneous search and isolation of their close contacts has
proven to be the cornerstone of dealing with the pandemic, as there
are only a limited number of effective treatments available thus
far (48-52).
In addition, due to shortages in medical and nursing staff and
infrastructure, it is absolutely necessary to select the most
suitable patients who require clinical and/or laboratory
examination, hospitalization or admission to the ICU. In this area,
the contribution of technology through the use of artificial
intelligence (AI) models, may be of great assistance (48,51,53). In
addition, the use of technology has played a crucial role in the
search for appropriate therapeutic substances, as well as in the
development of vaccines, at a rate at which has not been previously
observed (54,55).
At the beginning of the SARS-CoV-2 pandemic in
China, AI programs were used to identify and track infected
individuals or those with a travel history to a high-risk area (via
face recognition with thermal cameras), robots were tasked to
transport food and medicine to enclosed areas, while drones were
used to patrol persons under quarantine, transmit messages that
urged individuals to stay home and also disinfect certain public
areas (56). In addition, cell phone
data, debit and credit card transactions (tracking down infected
individuals or quarantine cases), popular internet searches and
social media posts can all provide information on the epidemiology
of numerous communicable diseases. Korea successfully dealt with
the transmission of the virus without the imposition of bans by
using such data (50). Another good
example is BlueDot software (Canadian surveillance platform
https://bluedot.global/healthcare/) that uses an AI
algorithm with data from the issuance of airline tickets worldwide,
which issued a warning for the onset of COVID-19 on December 31,
2019, the same time as the clinical detection of the first cases
(57). On the other hand, specific
attention should be paid to the processing of the information
‘storm’ that can be collected, in order to avoid any adverse
results, such as misinformation or propaganda or issues with
privacy (53).
AI technology includes machine learning (ML) and
deep learning (DL). Through smart devices, it imitates human
intelligence and the processing of the human spirit, based on
algorithms (51). ML, a subtype of
AI, applies mathematical models (statistics) to examples and data
and recognizes patterns in the information gathered in order to
draw future conclusions, without prior knowledge or specific
planning, while DL is the most tangible manifestation of ML, which
exploits artificial neural networks and functions, similar to a
model of human cognitive function (51,52).
AI-based technologies, using patients' personal health data, create
cognitive datasets that help clinicians in decision-making and in
the planning of personalized care for patients (54). They can aid in the early
identification of diseases and epidemics, and predict the mode of
transmission and probable outbreaks in different geographical
areas. They have been used in the past for the diagnosis of
tuberculosis, using the artificial immune recognition system
(ARIS), as well as in the diagnosis of malaria, and of the Ebola
and Zika viruses; however, they have also contributed to the
treatment of previous epidemics of other coronaviruses, such as the
one causing SARS in 2003 and the Middle East respiratory syndrome
in 2012, using the autoregressive integrated moving average (ARIMA)
system. The collaboration of King's College London (London, UK)
with Massachusetts General Hospital (Boston, MA, USA) created an AI
tool for COVID-19 symptom tracker on smartphones that among others,
recognized the onset of anosmia as an early sign of
COVID-19(58). At the onset of the
pandemic on January 22, 2020, Johns Hopkins University (Baltimore,
MA, USA), and in particular the Centre for Science and Engineering,
published a toolbar (https://www.arcgis.com/apps/dashboards/bda7594740fd40299423467b48e9ecf6)
that located, with accuracy, reported cases of COVID-19 in
real-time, contributing to the timely identification of new cases,
proposing remedial measures (e.g., quarantine) and informing
travellers in these areas (59).
Such use of information though, raises ethical,
legal and constitutional issues. Currently, it is crucial that
researchers, law professionals and technocrats work together to
create a secure framework for processing the sensitive personal
data of each citizen, so that the progress of technology is not
hindered and individual freedom is guaranteed.
5. Conclusions and future perspectives
The ‘7th Workshop on Paediatric Virology’ not only
brought together researchers and clinical scientists from Greece,
Canada, South Africa and the UK, but also addressed crucial and
relevant issues in the rapidly increasing educational field of
paediatric virology. Epidemics and pandemics are not new to
humankind, having been documented in ancient cultures, including
the ancient Mediterranean era. New technologies, such as
next-generation sequencing on DNA extracted from fossils, may
provide tools for the retrospective identification of the role of
viruses in ancient pandemics. Paediatric obesity, which has been
aggravated by the COVID-19 pandemic, poses a critical risk factor,
impacting on the development, progression and severity of viral
infections. Therefore, weight management in children may prove to
be an important preventive measure against viral infections in
formulating public health policies and decision-making strategies.
During the current COVID-19 pandemic, AI has been used to
facilitate the identification, monitoring and prevention of
SARS-CoV-2. In the future, it will play a fundamental role in
surveillance of epidemic-prone infectious diseases, repurposing of
older therapies and computer-aided design of new therapeutic agents
against viral infections. The current COVID-19 pandemic has
highlighted the need for collaboration between different medical
specialties as well as between diverse scientific fields, including
archaeology, history, epidemiology, nutritional technologies,
mathematics, computer technology, engineering, medical law and
ethics. This need should definitely be encouraged in modern medical
education.
Acknowledgements
The present review article was published in the
context of the ‘7th Workshop on Paediatric Virology’, which was
organised virtually by the Institute of Paediatric Virology (IPV;
https://paediatricvirology.org),
which is located on the island of Euboea in Greece, on December 20,
2021. In the context of the same workshop two more articles on the
foundation of paediatric intensive care in Greece written by
Papatheodoropoulou et al (2)
and the potential involvement of viruses in the pathogenesis of
neuroblastoma in childhood written by Rovigatti et al
(60) were published at the World
Academy of Sciences Journal. The authors would like to thank
Professor Anne Greenough, Professor of Neonatology and Clinical
Respiratory Physiology at the King's College London (London, UK)
and President of the Academic Board of the Institute of Paediatric
Virology for her support and valuable comments.
Funding
Funding: No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
All authors (INM, ML, PK, DIV, CK, AP, HK, MT, AK,
SBD and DAS) contributed equally to the conception and design of
the study, wrote the original draft, edited and critically revised
the manuscript. All authors have read and approved the final
manuscript. Data authentication is not applicable.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
INM, MT and DAS are co-founders of the Institute of
Paediatric Virology. ML, PK, DIV, CK, AP, HK, AK and SBD declare
that they have no competing interests.
References
|
1
|
Mammas IN, Greenough A, Theodoridou M and
Spandidos DA: The foundation of the Institute of Paediatric
Virology on the Island of Euboea, Greece (Review). Exp Ther Med.
20(302)2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Papatheodoropoulou A, Mammas IN and
Spandidos DA: Founding paediatric intensive care in Greece: An
interview with Dr John Papadatos, the first paediatric intensivist
in Greece at the ‘P. & A. Kyriakou’ Children's Hospital. World
Acad Sci J. 4(11)2022.
|
|
3
|
Mammas IN and Spandidos DA: Paediatric
virology in the hippocratic corpus. Exp Ther Med. 12:541–549.
2016.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Vallance JT: Hippocrates. In: The Oxford
Classical Dictionary, revised 3rd edition. Hornblower S and
Spawforth A (eds). Oxford University Press, Oxford, pp710-711,
2003.
|
|
5
|
Grmek MD: Diseases in the Ancient Greek
World, M. Muellner and L. Muellner, translators. The Johns Hopkins
University Press, Baltimore, MD, 1989.
|
|
6
|
Buikstra JE: A brief history and
21st century challenges. In: Ortner's Identification of
Pathological Conditions in Human Skeletal Remains. 3rd edition.
Buikstra JE (ed). Academic Press, London, pp11-20, 2019.
|
|
7
|
Roberts CA and Buikstra JE: Bacterial
infections. In: Ortner's Identification of Pathological Conditions
in Human Skeletal Remains. 3rd edition. Buikstra JE (ed). Academic
Press, London, pp321-439, 2019.
|
|
8
|
Drago L, Romanò CL, Morelli I and
Benzakour T: Viral bone infection: A neglected disease?
Microorganisms. 8(797)2020.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Mays S: How should we diagnose disease in
paleopathology? Some epistemological considerations. Int J
Paleopathol. 20:12–19. 2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Wagner DM, Klunk J, Harbeck M, Devault A,
Waglechner N, Sahl JW, Enk J, Birdsell DN, Kuch M, Lumibao C, et
al: Yersinia pestis and the plague of Justinian 541-543 AD:
A genomic analysis. Lancet Infect Dis. 14:319–326. 2014.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Stathakopoulos D: Crime and punishment:
The plague in the Byzantine empire, 541-749. In: Plague and the End
of Antiquity: The Pandemic of 541-750. Little LK (ed). Cambridge
University Press, Cambridge, pp99-118, 2007.
|
|
12
|
Nicklisch N, Maixner F, Ganslmeier R,
Friederich S, Dresely V, Meller H, Zink A and Alt KW: Rib lesions
in skeletons from early neolithic sites in central Germany: On the
trail of tuberculosis at the onset of agriculture. Am J Phys Anth.
149:391–404. 2012.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Crosby AW: Smallpox. In: The Cambridge
World History of Human Disease. Kiple KF (ed). Cambridge University
Press, Cambridge, pp1008-1013, 1993.
|
|
14
|
Littman RJ: The plague of athens:
Epidemiology and paleopathology. Mt Sinai J Med. 76:456–467.
2009.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Papagrigorakis MJ, Yapijakis C, Synodinos
PN and Baziotopoulou-Valavani E: DNA Examination of ancient dental
pulp incriminates typhoid fever as a probable cause of the Plague
of Athens. Int J Infectious Diseases. 10:206–214. 2006.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Papagrigorakis MJ, Yapijakis C and
Synodinos PN: Typhoid fever epidemic in Ancient Athens. In:
Paleomicrobiology: Past Human Infections. Raoult D and Drancourt M
(eds). Springer-Verlag, Berlin, pp161-173, 2008.
|
|
17
|
Salares R: The Ecology of the Ancient
Greek World. Duckworth, London, 1991.
|
|
18
|
Berner M, Pany-Kucera D, Doneus N, Sladek
V, Gamble M and Eggers S: Challenging definitions and diagnostic
approaches for ancient rare diseases: The case of poliomyelitis.
Int J Paleopathol. 33:113–127. 2021.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Díaz E, Rodríguez A, Martin-Loeches I,
Lorente L, Del Mar Martín M, Pozo JC, Montejo JC, Estella A,
Arenzana Á and Rello J: H1N1 SEMICYUC Working Group. Impact of
obesity in patients infected with 2009 influenza A(H1N1). Chest.
139:382–386. 2011.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Green WD and Beck MA: Obesity impairs the
adaptive immune response to influenza virus. Ann Am Thorac Soc. 14
(Suppl. 5):S406–S409. 2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Kompaniyets L, Goodman AB, Belay B,
Freedman DS, Sucosky MS, Lange SJ, Gundlapalli AV, Boehmer TK and
Blanck HM: Body mass index and risk for COVID-19-Related
hospitalization, intensive care unit admission, invasive mechanical
ventilation, and death - United States, March-December 2020. MMWR
Morb Mortal Wkly Rep. 70:355–361. 2021.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Tsankov BK, Allaire JM, Irvine MA, Lopez
AA, Sauvé LJ, Vallance BA and Jacobson K: Severe COVID-19 infection
and pediatric comorbidities: A systematic review and meta-analysis.
Int J Infect Dis. 103:246–256. 2021.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Moreno-Noguez M, Rivas-Ruiz R, Roy-García
IA, Pacheco-Rosas DO, Moreno-Espinosa S and Flores-Pulido AA: Risk
factors associated with SARS-CoV-2 pneumonia in the pediatric
population. Bol Méd Hosp Infant Méx. 78:251–258. 2021.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Webb NE and Osburn TS: Characteristics of
hospitalized children positive for SARS-CoV-2: Experience of a
large center. Hosp Pediatr. 11:e133–e141. 2021.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Abrams JY, Oster ME, Godfred-Cato SE,
Bryant B, Datta SD, Campbell AP, Leung JW, Tsang CA, Pierce TJ,
Kennedy JL, et al: Factors linked to severe outcomes in multisystem
inflammatory syndrome in children (MIS-C) in the USA: A
retrospective surveillance study. Lancet Child Adolesc Health.
5:323–331. 2021.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Bautista-Rodriguez C, Sanchez-de-Toledo J,
Clark BC, Herberg J, Bajolle F, Randanne PC, Salas-Mera D, Foldvari
S, Chowdhury D, Munoz R, et al: Multisystem inflammatory syndrome
in children: An international survey. Pediatrics.
147(e2020024554)2021.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Hoste L, Van Paemel R and Haerynck F:
Multisystem inflammatory syndrome in children related to COVID-19:
A systematic review. Eur J Pediatr. 180:2019–2034. 2021.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Moser JS, Galindo-Fraga A, Ortiz-Hernández
AA, Gu W, Hunsberger S, Galán-Herrera JF, Guerrero ML,
Ruiz-Palacios GM and Beigel JH: La Red ILI 002 Study Group.
Underweight, overweight, and obesity as independent risk factors
for hospitalization in adults and children from influenza and other
respiratory viruses. Influenza Other Respir Viruses. 13:3–9.
2019.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Neyer VL, Woo JG and Siegel RM: Severe
obesity in children may not pose independent risk for influenza
complications. J Pediatr Nurs. 42:21–24. 2018.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Bagdure D, Curtis DJ, Dobyns E, Glodé MP
and Dominguez SR: Hospitalized children with 2009 pandemic
influenza A (H1N1): Comparison to seasonal influenza and risk
factors for admission to the ICU. PloS One.
5(e15173)2010.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Okubo Y, Michihata N, Uda K, Morisaki N,
Miyairi I, Matsui H, Fushimi K and Yasunaga H: Dose-response
relationship between weight status and clinical outcomes in
pediatric influenza-related respiratory infections. Pediatr
Pulmonol. 53:218–223. 2018.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Morgan OW, Bramley A, Fowlkes A, Freedman
DS, Taylor TH, Gargiullo P, Belay B, Jain S, Cox C, Kamimoto L, et
al: Morbid obesity as a risk factor for hospitalization and death
due to 2009 pandemic influenza A(H1N1) disease. PLoS One.
5(e9694)2010.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Yu H, Feng Z, Uyeki TM, Liao Q, Zhou L,
Feng L, Ye M, Xiang N, Huai Y, Yuan Y, et al: Risk factors for
severe illness with 2009 pandemic influenza A (H1N1) virus
infection in China. Clin Infect Dis. 52:457–465. 2011.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Gill PJ, Ashdown HF, Wang K, Heneghan C,
Roberts NW, Harnden A and Mallett S: Identification of children at
risk of influenza-related complications in primary and ambulatory
care: A systematic review and meta-analysis. Lancet Respir Med.
3:139–149. 2015.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Garcia MN, Philpott DC, Murray KO,
Ontiveros A, Revell PA, Chandramohan L and Munoz FM: Clinical
predictors of disease severity during the 2009-2010 A(HIN1)
influenza virus pandemic in a paediatric population. Epidemiol
Infect. 143:2939–2949. 2015.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Akiyama N, Segawa T, Ida H, Mezawa H, Noya
M, Tamez S and Urashima M: Bimodal effects of obesity ratio on
disease duration of respiratory syncytial virus infection in
children. Allergol Int. 60:305–308. 2011.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Pokorska-Śpiewak M, Kowalik-Mikołajewska
B, Aniszewska M, Pluta M, Walewska-Zielecka B and Marczyńska M:
Determinants of liver disease progression in children with chronic
hepatitis C virus infection. Pol J Pathol. 66:368–375.
2015.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Delgado-Borrego A, Healey D, Negre B,
Christofi M, Sabharwal S, Ludwig DA, Chung RT and Jonas MM:
Influence of body mass index on outcome of pediatric chronic
hepatitis C virus infection. J Pediatr Gastroenterol Nutr.
51:191–197. 2010.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Zulkipli MS, Dahlui M, Jamil N, Peramalah
D, Wai HVC, Bulgiba A and Rampal S: The association between obesity
and dengue severity among pediatric patients: A systematic review
and meta-analysis. PLoS Negl Trop Dis. 12(e0006263)2018.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Fang X, Henao-Mejia J and Henrickson SE:
Obesity and immune status in children. Curr Opin Pediatr.
32:805–815. 2020.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Tagliabue C, Principi N, Giavoli C and
Esposito S: Obesity: Impact of infections and response to vaccines.
Eur J Clin Microbiol Infect Dis. 35:325–331. 2016.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Smith M, Honce R and Schultz-Cherry S:
Metabolic syndrome and viral pathogenesis: Lessons from influenza
and coronaviruses. J Virol. 94:e00665–20. 2020.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Sanchis-Gomar F, Lavie CJ, Mehra MR, Henry
BM and Lippi G: Obesity and outcomes in COVID-19: When an epidemic
and pandemic collide. Mayo Clin Proc. 95:1445–1453. 2020.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Mammas IN, Kramvis A, Papaevangelou V,
Doukas SG, Naya SD, Doukas PG, Melikoki V, Bouros D, Thiagarajan P,
Chrousos GP, et al: SARS-CoV-2 infection and children: Insights
from the 6th Workshop on Paediatric Virology (Review). World Acad
Sci J. 4(15)2022.
|
|
45
|
Mammas IN, Theodoridou M and Spandidos DA:
COVID-19 and paediatric challenges: An interview with professor of
paediatrics Vana Papaevangelou (University of Athens School of
Medicine). Exp Ther Med. 20(296)2020.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Koutsaftiki C, Papatheodoropoulou A,
Papaioannou G, Korovessi P, Mammas IN, Theodoridou M and Spandidos
DA: COVID-19 threat and frontline paediatric care professionals.
Exp Ther Med. 20(291)2020.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Mammas IN, Theodoridou M and Spandidos DA:
COVID-19 threat and the 1918 Spanish flu outbreak: The following
day. Exp Ther Med. 20(292)2020.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Bansal A, Padappayil RP, Garg C, Singal A,
Gupta M and Klein A: Utility of artificial intelligence amidst the
COVID-19 pandemic: A review. J Med Syst. 44(156)2020.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Yadav AK, Verma D, Kumar A, Kumar P and
Solanki PR: The perspectives of biomarker-based electrochemical
immunosensors, artificial intelligence and the Internat of medical
things toward COVID-19 diagnosis and management. Mater Today Chem.
20(100443)2021.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Lin L and Hou Z: Combat COVID-19 with
artificial intelligence and big data. J Travel Med.
27(taaa080)2020.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Rasheed J, Jamil A, Hameed AA, Al-Turjman
F and Rasheed A: COVID-19 in the age of artificial intelligence: A
comprehensive review. Interdiscip Sci. 13:153–175. 2021.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Vaid S, Kalantar R and Bhandari M: Deep
Learning COVID-19 detection bias: Accuracy through artificial
intelligence. Int Orthop. 44:1539–1542. 2020.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Kumar A, Gupta PK and Srivastava A: A
review of modern technologies for trackling COVID-19 pandemic.
Diabetes Metab Syndr. 14:569–573. 2020.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Malik YS, Sircar S, Bhat S, Ansari MI,
Pande T, Kumar P, Mathapati B, Balasubramanian G, Kaushik R,
Natesan S, et al: How artificial intelligence may help the COVID-19
pandemic: Pitfalls and lessons for the future. Rev Med Virol.
31:1–11. 2021.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Schultz MB, Vera D and Sinclair DA: Can
artificial intelligence identify effective COVID-19 therapies? EMBO
Mol Med. 12(e12817)2020.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Ruiz Estrada MA: The uses of drones in
case of massive epidemics contagious diseases relief humanitarian
aid: Wuhan-COVID-19 crisis. SSRN Electron J: Feb 29, 2020 (Epub
ahead of print). doi: http://dx.doi.org/10.2139/ssrn.3546547.
|
|
57
|
Niiler E: An AI Epidemiologist Sent the
First Warnings of the Coronavirus|WIRED [Internet]. https://www.wired.com/story/ai-epidemiologist-wuhan-public-health-warnings/.
Accessed November 1, 2021.
|
|
58
|
Menni C, Valdes AM, Freidin MB, Sudre CH,
Nguyen LH, Drew DA, Ganesh S, Varsavsky T, Cardoso MJ, El-Sayed
Moustafa JS, et al: Real-time tracking of self-reported symptoms to
predict potential COVID-19. Nat Med. 26:1037–1040. 2020.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Dong E, Du H and Gardner L: An interactive
web-based dashboard to track COVID-19 in real time. Lancet Infect
Dis. 20:533–534. 2020.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Rovigatti U, Papaioannou G, Mammas IN,
Koutsaftiki C, Papatheodoropoulou A, Theodoridou M and Spandidos
DA: Neuroblastoma in childhood and its potential viral involvement:
A webinar by the Paediatric Virology Study Group. World Acad Sci J.
4(16)2022.
|