Introduction
On March 11, 2020, coronavirus disease 2019
(COVID-19) was recognized as a pandemic by the World Health
Organization (WHO) (1). It has thus
far affected >600 million individuals worldwide, with a total of
6.47 million related deaths (https://www.worldometers.info/coronavirus/). It has
been highlighted that 75% of patients hospitalized for COVID-19
have at least one COVID-19-associated comorbidity. It has been
reported that those with underlying chronic diseases are more prone
to infection and to becoming seriously ill (2,3).
Patients with COVID-19 who have a history of cardiovascular
disease, malignancy, obesity, chronic respiratory disease, diabetes
mellitus, or neurological disorders have the worst outcomes and are
more susceptible to developing pneumonia or acute respiratory
distress syndrome (2,3).
COVID-19 can affect the respiratory tract via a
number of mechanisms and at varying degrees of severity, depending
on the individual's immune system, age and comorbidities. Symptoms
can vary from minor to severe, including cough, dyspnea and fever,
as well as respiratory failure, shock and multi-organ system
failure. As a result, prior respiratory disorders, such as
interstitial lung disease, asthma and chronic obstructive pulmonary
disease (COPD) may be exacerbated by COVID-19(4).
Swyer-James-MacLeod syndrome is an uncommon clinical
entity associated with post-infectious infantile bronchiolitis
obliterans. It is characterized by pulmonary arterial hypoplasia
and/or agenesis, resulting in the hypoperfusion of the lung
parenchyma. Traditionally, the diagnosis is confirmed in infancy
following an inquiry for recurring respiratory infections; however,
in certain cases, patients with minimal or no bronchiectasis have
few or no symptoms, and the syndrome may thus remain undetected
until adulthood (5). Other symptoms
include wheezing, breathlessness on exertion, decreased exercise
tolerance and cough, which may be accompanied by hemoptysis and
chest pain (6).
The most common finding associated with this
condition on pulmonary function tests is airflow obstruction
(7), while the presence of pulmonary
hyperlucency on chest imaging is a hallmark of the syndrome
(8). Swyer-James-MacLeod syndrome
complications include recurrent infections, particularly in
patients with bronchiectasis, lung abscess and pneumothorax
(9,10). The cornerstone of treatment is
conservative management. Surgery is only used in certain
situations, such as when a patient has recurrent lung infections,
does not respond to treatment, or has symptoms that are
insufficiently handled by the most appropriate medical care.
Pneumonectomy and lung volume reduction procedures, such as
lobectomy and segmentectomy are surgical treatment options
(6).
The present study describes the case of a
45-year-old patient with Swyer-James-MacLeod syndrome hospitalized
due to COVID-19, which is the first one to be reported to date, at
least to the best of our knowledge.
Case report
A 45-year-old male patient (non-smoker) presented to
the department of Infectious Diseases-COVID-19 unit of Laiko
General Hospital with complaints of fever, post-nasal drip, dry
cough and dyspnea at rest over the past 12 days. He had a medical
history of Swyer-James-MacLeod syndrome and gastroesophageal
reflux. His medications included omeprazole and a combination of
inhaled indacaterol/glycopyrronium bromide.
A clinical examination of this respiratory system
revealed crackles on auscultation in all lung fields of the right
lung and diminished lung sounds in all lung fields of the left
lung. The evaluation of the other bodily systems did not reveal any
abnormalities. His blood pressure was 135/80 mmHg, his heart rate
was 120 beats per minute, his oxygen saturation in room air was
89%, and his body temperature was 38.5˚C. An electrocardiography
revealed sinus tachycardia.
Arterial blood gas analysis revealed a partial
pressure of oxygen (pO2) of 56 mmHg, a partial pressure
of carbon dioxide (pCO2) of 28 mmHg, pH 7.51 and
bicarbonate (HCO3-) levels of 22.3 mmol/l in room air. A
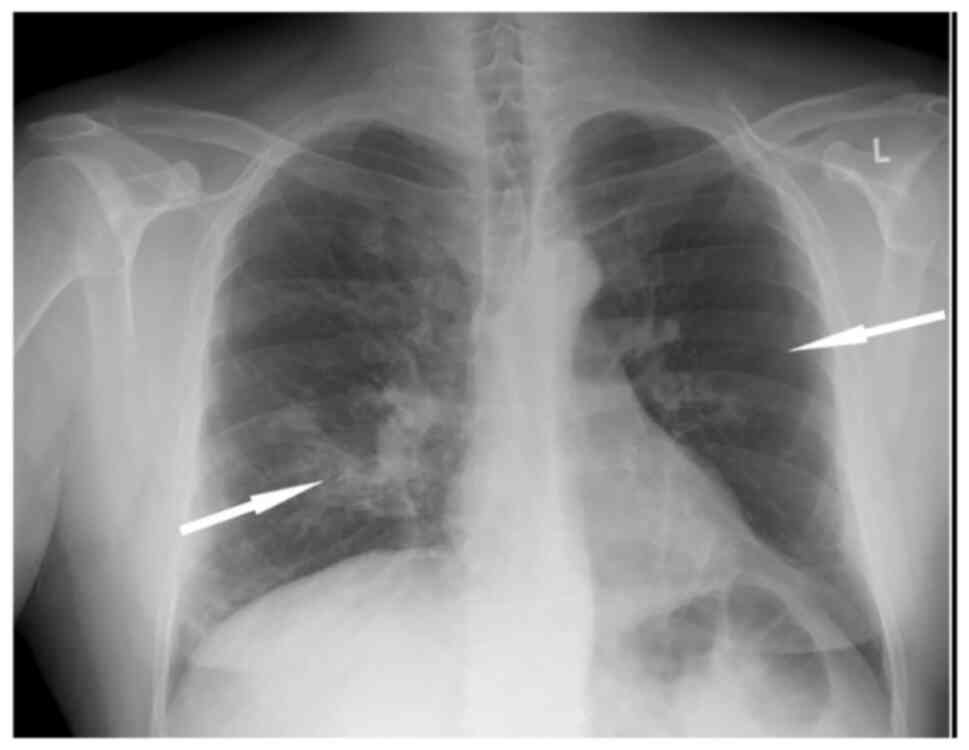
chest X-ray revealed patchy infiltrates in the right lung lower
lobe and a hyperlucent left lung (Fig.
1).
The laboratory analyses included a complete blood
cell count, serum biochemistry and coagulation tests. Notable
laboratory findings included C-reactive protein levels of 133.17
mg/l (normal, <6 mg/l), ferritin levels of 710 ng/ml (normal
range, 150-400 ng/ml) and d-dimer levels of 0.65 µg/ml (normal,
<0.5 µg/ml). The procalcitonin test was negative (0.03 ng/ml;
normal, <0.1 ng/ml).
The patient had a positive detection of severe acute
respiratory syndrome 2 (SARS-CoV-2) nucleic acid in the examined
nasopharyngeal sample using reverse transcription-polymerase chain
reaction (RT-PCR). The patient was unvaccinated against SARS-CoV-2.
He was hospitalized in the COVID-19 unit and was administered
oxygen therapy with a Venturi mask supplying 35% oxygen, along with
prophylactic subcutaneous enoxaparin at a daily dose of 40 mg, and
intravenous dexamethasone at a daily dose of 6 mg, as well as
remdesivir (200 mg on the first day, followed by a daily dose of
100 mg for the following 4 days) (11). The duration of therapy was 5 days for
all agents.
The patient was also advised to continue receiving
the combination of inhaled bronchodilators during his
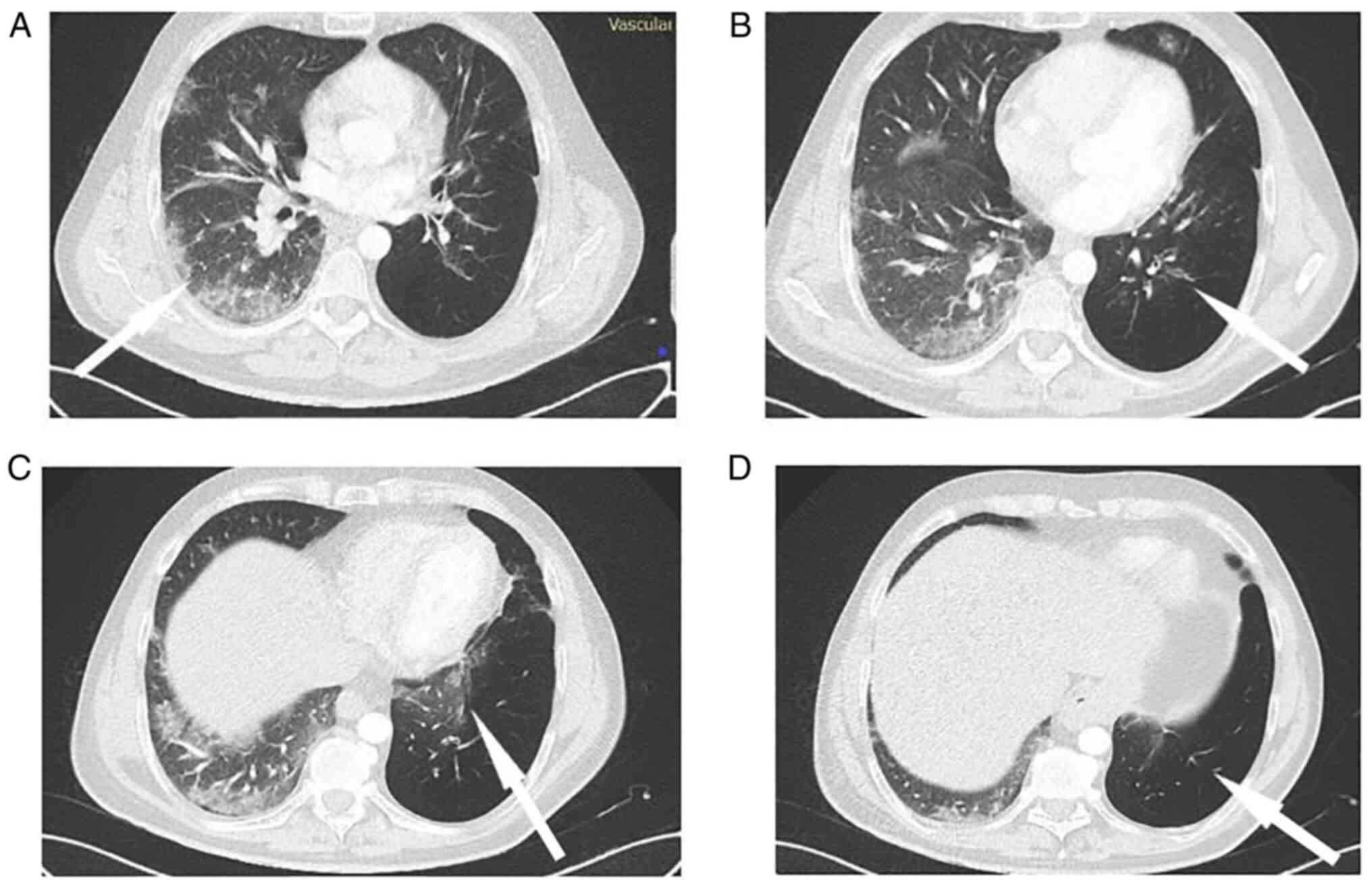
hospitalization. He underwent a computed tomography pulmonary
angiogram, which revealed no pulmonary embolism, and a
high-resolution computed tomography scan of the chest, which
revealed lung infiltrates in all lung fields of the right lung, as
well as a hyperlucent left lung with bronchiectasis and much fewer
lung infiltrates (Fig. 2).
Furthermore, a sputum culture was performed that did not reveal any
microorganisms, and therefore the patient did not receive any
antibiotics.
Following 3 days in the hospital, his fever had
subsided and his oxygen levels had improved. He exhibited a gradual
recovery and was discharged on the 6th day of hospitalization
without the need for supplemental oxygen; a new arterial blood gas
analysis revealed a pO2 of 86 mmHg, a pCO2 of
34 mmHg, pH 7.44 and HCO3- levels of 23.7 mmol/l in room
air.
Discussion
To the best of our knowledge, this is the first
reported case of COVID-19-associated pneumonia in a patient with
Swyer-James-MacLeod syndrome. Since the first cases of COVID-19
were reported, COPD has been linked to a greater likelihood of a
poor prognosis, as measured by the number of hospitalizations and
mortality (12-14).
Chronic inflammation (usually T2) and bronchial remodeling, both of
which are common hallmarks of asthma, may enhance sensitivity to
COVID-19. It has been debated whether asthma increases the chance
of infection; however, new research suggests that the risk is
limited to severe types of the disease (15). A recent study found that individuals
with asthma had a higher risk of hospitalization due to COVID-19
than those without asthma, and that those who had two or more oral
corticosteroid bursts in the preceding 2 years had a higher chance
of ICU admission or mortality, even accounting for vaccination
status (16). However, there are
currently no data available indicating the effects of COVID-19 in
patients with Swyer-James-MacLeod syndrome, at least to the best of
our knowledge.
As regards bronchiectasis, although the findings of
studies on COVID-19 and bronchiectasis are conflicting (17-20),
it should be noted that when making comparisons in patients with
COVID-19 with or without bronchiectasis, the former are more likely
to experience the severe manifestations of the infection, may
require oxygen therapy or hospitalization and may even be more
likely to require admission to an intensive care unit or to succumb
to the disease (17-21).
In the present study, the patient suffered from a syndrome
characterized by an obstructive lung pattern and bronchiectasis,
and required hospitalization and oxygen therapy; fortunately, he
had a favorable outcome.
To the best of our knowledge, there are currently no
data available on the use of bronchodilators in patients with
Swyer-James-MacLeod syndrome and COVID-19-associated pneumonia.
Patients with few or no bronchiectasis have minor symptoms or are
asymptomatic and may remain undiagnosed until adulthood. Adult
patients with this syndrome are frequently diagnosed following a
chest X-ray for other reasons (6).
Furthermore, there is currently no evidence that agents used for
the treatment of COPD or its comorbidities adversely affect the
prognosis of patients with COVID-19. Patients with COPD are
strongly advised to continue their usual treatments, avoiding the
use of nebulizers, particularly if they are not accompanied by a
filter in the expiratory branch (5).
Based on this fact, the patient described herein continued to
receive his usual medication for this obstructive syndrome during
his hospital stay.
Another interesting point is that the patient had a
favorable outcome despite the fact that he was unvaccinated against
COVID-19. It is well established that this is an additional risk
factor for hospitalization and poor outcomes (22). Although there are no data suggesting
that the efficacy of the vaccine in patients with chronic lung
diseases, including Swyer-James-MacLeod syndrome, differs from that
of the general population (5), it
has been reported that airway immune responses to COVID-19
vaccination are the same in patients with COPD and healthy subjects
(23).
In conclusion, the present study describes an
interesting case of COVID-19-associated pneumonia in a patient with
Swyer-James-MacLeod syndrome. Patients with this syndrome are
vulnerable to COVID-19 as are patients with other chronic lung
diseases, requiring oxygen therapy and hospitalization. However, to
the best of our knowledge, there are currently no data available on
the effects of COVID-19 in these patients, their optimal
management, or the role of COVID-19 vaccine in their clinical
course.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
AB and VEG conceptualized the study. AB, VEG, PA,
AG, PP and KT advised on patient care and medical treatment, and
wrote and prepared the draft of the manuscript. PS, NT, GF, SC and
DAS analyzed the data and provided critical revisions. AB and VEG
confirm the authenticity of all the data. All authors contributed
to manuscript revision and have read and approved the final version
of the manuscript.
Ethics approval and consent to
participate
Written informed was obtained from the patient
described herein. A copy of the written consent is available for
review by the editorial office of this journal on request.
Patient consent for publication
Written informed was obtained from the patient for
publication of his data. A copy of the written consent is available
for review by the editorial office of this journal on request.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Cucinotta D and Vanelli M: WHO declares
COVID-19 a pandemic. Acta Biomed. 91:157–160. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He
JX, Liu L, Shan H, Lei CL, Hui DSC, et al: China medical treatment
expert group for Covid-19. Clinical characteristics of coronavirus
disease 2019 in China. N Engl J Med. 382:1708–1720. 2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Muñoz-Rodríguez JR, Gómez-Romero FJ,
Pérez-Ortiz JM, López-Juárez P, Santiago JL, Serrano-Oviedo L and
Redondo-Calvo FJ: COVID-19 SESCAM Network. Characteristics and risk
factors associated with mortality in a multicenter spanish cohort
of patients with COVID-19 pneumonia. Arch Bronconeumol. 57:34–41.
2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Chiner-Vives E, Cordovilla-Pérez R, de la
Rosa-Carrillo D, García-Clemente M, Izquierdo-Alonso JL,
Otero-Candelera R, Pérez-de Llano L, Sellares-Torres J and de
Granda-Orive JI: Short and long-term impact of COVID-19 infection
on previous respiratory diseases. Arch Bronconeumol. 58 (Suppl
1):S39–S50. 2022.PubMed/NCBI View Article : Google Scholar : (In English,
Spanish).
|
|
5
|
Chlapoutakis S, Garmpi A, Trakas N,
Damaskos C and Georgakopoulou VE: Recurrent exacerbations of
chronic obstructive pulmonary disease reveal Swyer-James-Macleod
syndrome in a 63-year-old patient. Cureus.
13(e12601)2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Behrendt A and Lee Y: Swyer-james-macleod
syndrome. In: StatPearls [Internet]. StatPearls Publishing,
Treasure Island, FL, 2022.
|
|
7
|
Chang AB, Masel JP and Masters B:
Post-infectious bronchiolitis obliterans: Clinical, radiological
and pulmonary function sequelae. Pediatr Radiol. 28:23–29.
1998.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tortajada M, Gracia M, García E and
Hernández R: Diagnostic considerations in unilateral hyperlucency
of the lung (Swyer-James-MacLeod Syndrome). Allergol Immunopathol
(Madr). 32:265–270. 2004.PubMed/NCBI View Article : Google Scholar : (In Spanish).
|
|
9
|
Wang JY, Chen KY, Chang YC, Chang YL and
Lee LN: Swyer-James syndrome complicated by lung abscess. J Formos
Med Assoc. 99:252–256. 2000.PubMed/NCBI
|
|
10
|
Soni R and Barnes D: Macleod's syndrome
presenting with spontaneous pneumothorax. Respirology. 4:275–277.
1999.PubMed/NCBI View Article : Google Scholar
|
|
11
|
National Institutes of Health: COVID-19
Treatment Guidelines. Therapeutic Management of Hospitalized Adults
With COVID-19. https://www.covid19treatmentguidelines.nih.gov/tables/therapeutic-management-of-hospitalized-adults/.
Accessed July 19, 2022.
|
|
12
|
Graziani D, Soriano JB, Rio-Bermudez CD,
Morena D, Díaz T, Castillo M, Alonso M, Ancochea J, Lumbreras S and
Izquierdo JL: Characteristics and prognosis of COVID-19 in patients
with COPD. J Clin Med. 9(3259)2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Lippi G and Henry BM: Chronic obstructive
pulmonary disease is associated with severe coronavirus disease
2019 (COVID-19). Respir Med. 167(105941)2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Quaranta VN, Kyriakopoulos C, Liontos A,
Barkas F, Chronis C, Biros D, Athanasiou L, Milionis O, Tsourlos S,
Veliani C, et al: Baseline characteristics and outcome predictors
in patients hospitalized with COVID-19 in the university general
hospital of Ioannina, Greece. Pneumon. 35(9)2022.
|
|
15
|
Liu S, Cao Y, Du T and Zhi Y: Prevalence
of comorbid asthma and related outcomes in COVID-19: A systematic
review and meta-analysis. J Allergy Clin Immunol Pract. 9:693–701.
2021.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Shi T, Pan J, Vasileiou E, Robertson C and
Sheikh A: Public Health Scotland and the EAVE II Collaborators.
Risk of serious COVID-19 outcomes among adults with asthma in
Scotland: A national incident cohort study. Lancet Respir Med.
10:347–354. 2022.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Georgakopoulou VE, Avramopoulos P,
Papalexis P, Bitsani A, Damaskos C, Garmpi A, Gkoufa A, Garmpis N,
Mantzouranis K, Chlapoutakis S, et al: Exacerbation of
bronchiectasis by Pseudomonas putida complicating COVID-19 disease:
A case report. Exp Ther Med. 22(1452)2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Choi H, Lee H, Lee SK, Yang B, Chung SJ,
Yeo Y, Park TS, Park DW, Moon JY, Kim TH, et al: Impact of
bronchiectasis on susceptibility to and severity of COVID-19: A
nationwide cohort study. Ther Adv Respir Dis.
15(1753466621995043)2021.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Guan WJ, Liang WH, Shi Y, Gan LX, Wang HB,
He JX and Zhong NS: Chronic respiratory diseases and the outcomes
of COVID-19: A nationwide retrospective cohort study of 39,420
cases. J Allergy Clin Immunol Pract. 9:2645–2655. 2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Aveyard P, Gao M, Lindson N,
Hartmann-Boyce J, Watkinson P, Young D, Coupland CAC, Tan PS, Clift
AK, Harrison D, et al: Association between pre-existing respiratory
disease and its treatment, and severe COVID-19: A population cohort
study. Lancet Respir Med. 9:909–923. 2021.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Crichton ML, Shoemark A and Chalmers JD:
The impact of the COVID-19 pandemic on exacerbations and symptoms
in bronchiectasis: A prospective study. Am J Respir Crit Care Med.
204:857–859. 2021.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Griffin JB, Haddix M, Danza P, Fisher R,
Koo TH, Traub E, Gounder P, Jarashow C and Balter S: SARS-CoV-2
infections and hospitalizations among persons aged ≥16 years, by
vaccination status-Los Angeles County, California, May 1-July 25,
2021. MMWR Morb Mortal Wkly Rep. 70:1170–1176. 2021.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Southworth T, Jackson N and Singh D:
Airway immune responses to COVID-19 vaccination in COPD patients
and healthy subjects. Eur Respir J. 60(2200497)2022.PubMed/NCBI View Article : Google Scholar
|