Introduction
Gangrenous cellulitis is not uncommonly seen skin
infection in clinical practice. In the past, the leading pathogens
are group B beta-hemolytic Streptococcus and
Pseudomonas (1-3).
Coagulase-negative Staphylococcus (CoNS) may play a critical
role in opportunistic infection when the skin is damaged by trauma,
the implantation of foreign bodies (e.g., permanent pacemakers,
vascular grafts and orthopedic devices), or by the inoculation of
needles (4).
The present study describes the case of a drug
abuser with CoNS infection associated with gangrenous cellulitis.
Physicians need to have a good knowledge of this type of
debilitating skin and soft tissue infection (SSTI). The present
case report is written according to the guidelines of CARE in
2013(5).
Case report
A 40-year-old male with a history of alcohol and
drug addiction visited doctors in the Emergency Department of
MacKay Memorial Hospital, Tamshui branch, Taiwan due to a
persistently high fever for 1 day. He reported the abuse of drugs
via intravenous injection and excessive alcohol consumption over
the past 2 days. Upon arrival to the department, a physical
examination revealed the following: A body temperature of 39.4˚C, a
respiratory rate of 18/min, a heart rate of 115 beats/min and a
blood pressure of 131/75 mm Hg. In addition, generalized skin
gangrene was observed over the trunk (Fig. 1), buttocks and four limbs (Fig. 2A and B). Laboratory tests revealed a white blood
cell count of 6,100/µl, a neutrophil count of 77%; thrombocytopenia
(platelets, 67,000/µl) and elevated C-reactive protein (30.4
mg/dl), creatine kinase (>20,000 IU/l) and D-Dimer (>10,000
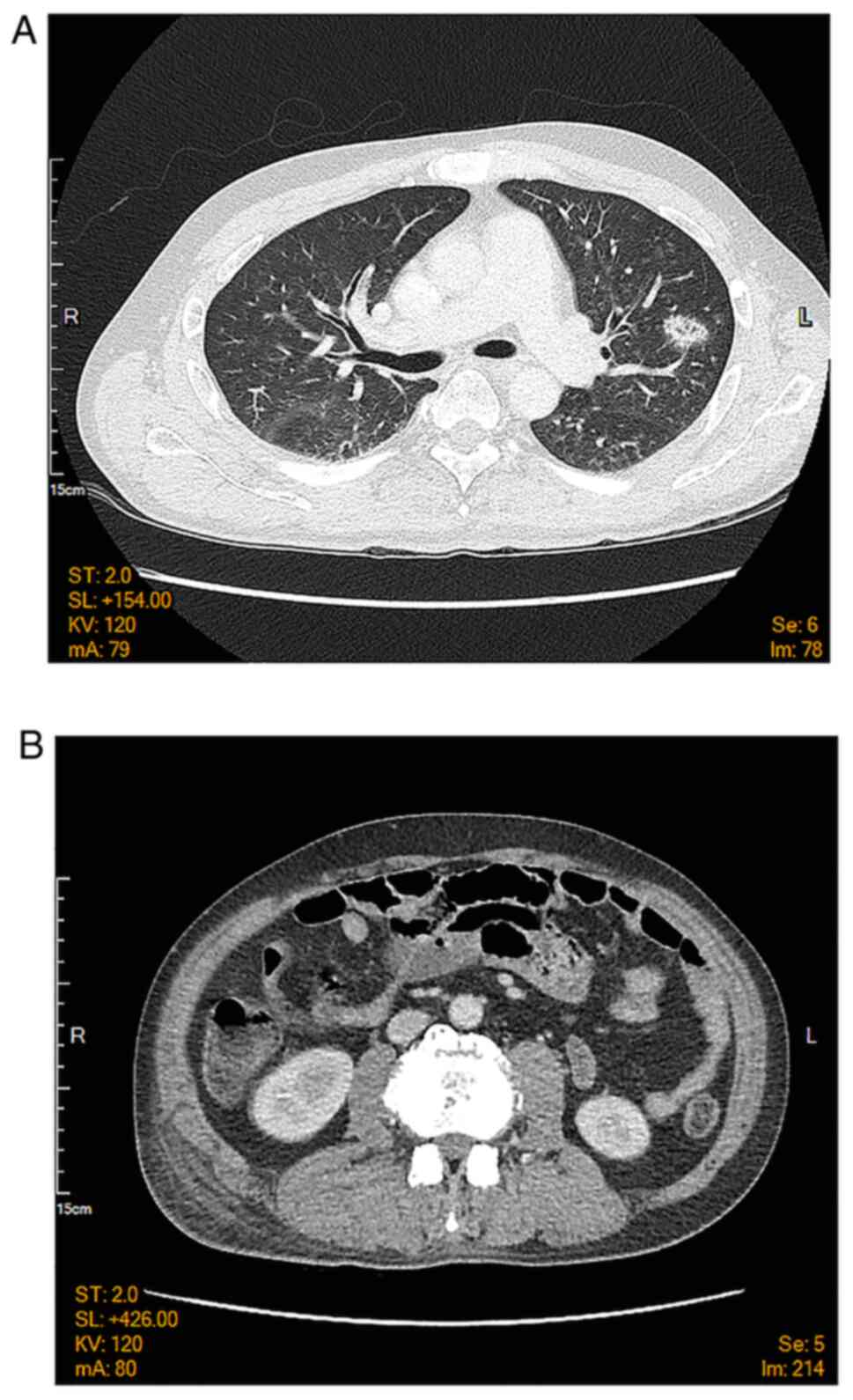
ng/ml) levels. A chest computed tomography scan was arranged to
exclude septic emboli, which revealed multifocal ground-glass
opacities in both lungs and subcutaneous soft tissue and muscle
swelling over the back and buttocks (Fig. 3). An abdominal and cardiac sonography
was performed for the exclusion of other origins of infection.
There was no vegetation of the heart chamber or other significant
findings. The urinary drug screen was positive for ketamine and
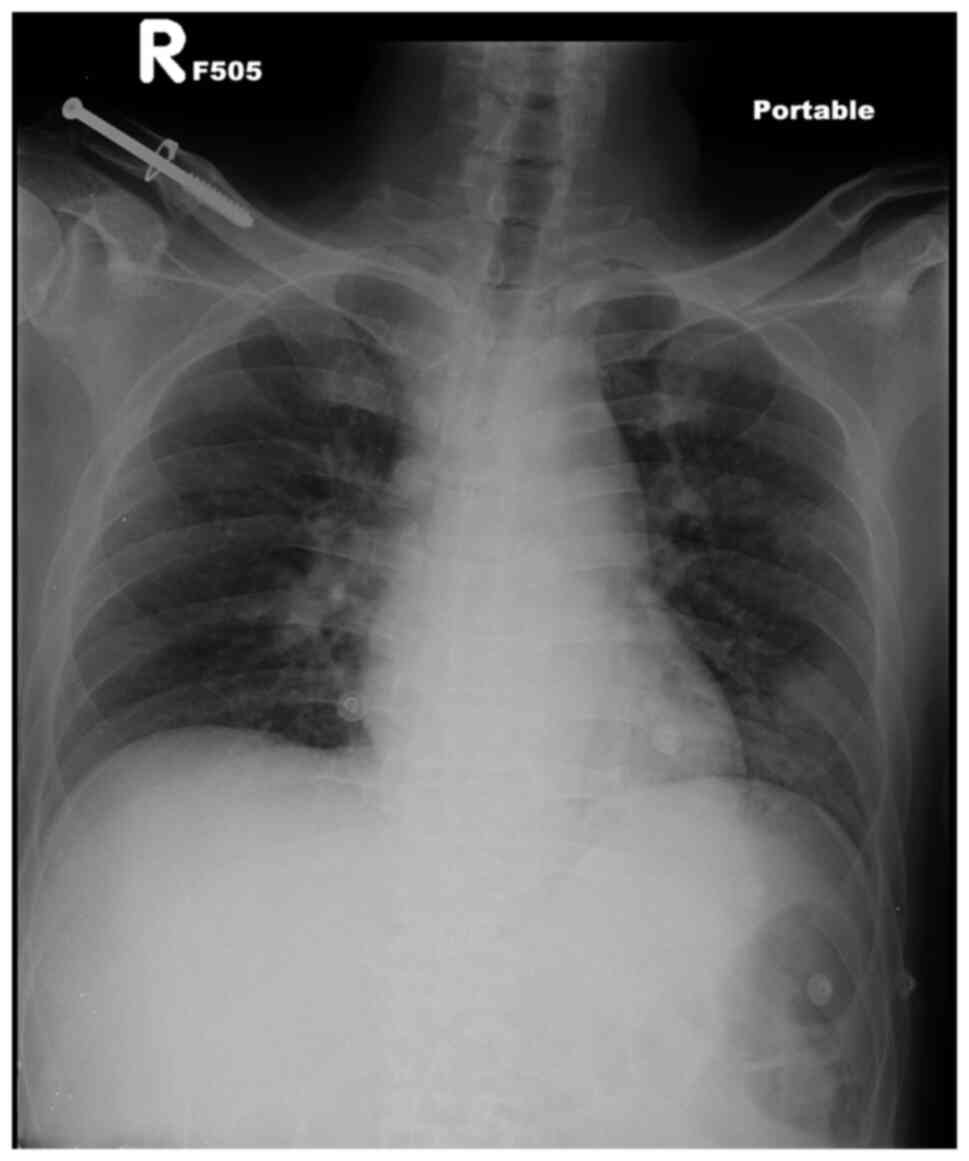
benzodiazepine. A chest X-ray revealed a pneumonia patch over the
left lower lung field (Fig. 4).
Therefore, pneumonia in his left lower lobe and
gangrenous cellulitis were considered the sources of infection. Two
sets of blood culture on day 4 of admission revealed CoNS.
Following 1 week of antibiotics treatment, the blood culture was
sterile. The patient was thus diagnosed with CoNS infection caused
by the venous injection of ketamine.
He was admitted for parenteral antibiotics treatment
with tigecycline (100 mg every 12 h) and meropenem (1,000 mg every
8 h). The plastic surgeon performed serial debridement four times
due to the progressive necrosis of the skin gangrene. Subsequently,
the replacement of the skin on the right foot was performed using
autologous tissue substitute and back rotation fasciocutaneous flap
was conducted. His condition improved gradually following each
debridement session. Finally, he was discharged after ~2 months of
admission.
Discussion
CoNS is present in the normal flora of the cutaneous
ecosystem of human skin, which frequently contaminates blood
culture and occasionally causes diseases. Therefore, it should be
considered as an opportunistic pathogen rather than a contaminant.
CoNS generally has a symbiotic association with its host in the
cutaneous ecosystem. If the cutaneous organ system has been damaged
by trauma, the implantation of foreign bodies (e.g., permanent
pacemakers, vascular grafts and orthopedic devices), or inoculation
by needles, these organisms can cause occasional infection
(4). Predisposing factors for CoNS
infections include an older age, immunosuppression and the implants
of medical devices, which can serve as a nidus for CoNS growth.
Distinguishing the etiological agents from contaminating normal
flora is a crucial clinical challenge to physicians. The diagnosis
of CoNS is based on the clinical judgement of the physician plus a
positive bacterial culture. Repeating another bacterial culture is
reasonable in the case that there is doubt about the collection
method or an increased risk of a contaminated sample (6).
Pathogens that enter the host through venous
ketamine injection can be a reasonable cause of infection, as
described the case in the present study. Long-term alcoholism and
malnutrition may have caused a decline in the immunity of patient
described herein. Polymicrobial Staphylococcus aureus
bacteremia has been noted in 12/58 (20.7%) of necrotizing soft
tissue infections/sacral decubiti and foot gangrene vs. 1/122
(0.8%) of cellulitis/abscesses (P<0.001) (7), and it is significantly much more
frequent in necrotizing infections (7). The most common pathogens found in
diabetic foot infections (both monomicrobial and polymicrobial) are
Staphylococcus aureus (39.7%), Bacteroides fragilis
(30.3%), Pseudomonas aeruginosa (26.0%) and Streptococcus
agalactiae (21.0%) (8). To date,
to the best of our knowledge, there has been no report of local
skin necrosis induced by CoNS infection. Generally, CoNS organisms
are susceptible to the same antibiotics used to treat
methicillin-sensitive Staphylococcus aureus.
Necrotic and gangrenous skin are commonly observed
in daily practice in emergency rooms. Various pathogens occurring
at different sites cause gangrenous cellulitis, which is
characterized by infection with necrosis of the skin and underlying
subcutaneous tissue (9).
In conclusion, gangrenous cellulitis is not an
uncommonly observed symptom in the emergency department. CoNS needs
to be taken into consideration as a pathogen, particularly in
individuals with an older age, are immunosuppressed, or in those
who have implants of medical devices. Analyses using blood cultures
and urine analyses for toxic screening are mandatory in order to
identify the pathogenic cause of infection. Moreover, treatment
with parenteral antibiotics and surgical debridement may be
necessary in such cases, as these treatments were effective in the
patient in the present study. In summary, physicians need to be
aware of the potential pathogenicity of CoNS in SSTI.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
PYC and YJS wrote the draft of the manuscript and
collected the patient data. YJS designed the study and revised it,
and corresponded to the manuscript. CWC analyzed the patient data
and participated in discussions regarding the data. PYC and YJS
confirm the authenticity of all the raw data. All authors have read
and approved the final manuscript.
Ethics approval and consent to
participate
The patient provided written informed consent for
his data to be included in the present study.
Patient consent for publication
The patient provided written informed consent for
the publication of his data and any accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Thame M, Franklin L, Young J, Hall C,
Saunders GL and Williams NP: An unusual presentation of group B
streptococcal sepsis. West Indian Med J. 53:416–419.
2004.PubMed/NCBI
|
|
2
|
Hau T and Förster E: Etiology, diagnosis
and therapy of soft tissue infections. Zentralbl Chir. 115:521–541.
1990.PubMed/NCBI(In German).
|
|
3
|
Haury B, Rodeheaver G, Stevenson T,
Bacchetta C, Edgerton MT and Edlich RF: Streptococcal cellulitis of
the scrotum and penis with secondary skin gangrene. Surg Gynecol
Obstet. 141:35–39. 1975.PubMed/NCBI
|
|
4
|
Kloos WE and Bannerman TL: Update on
clinical significance of coagulase-negative staphylococci. Clin
Microbiol Rev. 7:117–140. 1994.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Gagnier JJ, Riley D, Altman DG, Moher D,
Sox H and Kienle G: CARE Group. The CARE guidelines:
Consensus-based clinical case reporting guideline development.
Dtsch Arztebl Int. 110:603–608. 2013.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Natsis NE and Cohen PR: Coagulase-negative
Staphylococcus skin and soft tissue infections. Am J Clin Dermatol.
19:671–677. 2018.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Khatib R, Sharma M, Johnson LB, Riederer K
and Briski L: Polymicrobial Staphylococcus aureus bacteremia:
Frequency, distinguishing characteristics and outcome. Diagn
Microbiol Infect Dis. 86:311–315. 2016.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Aziz Z, Lin WK, Nather A and Huak CY:
Predictive factors for lower extremity amputations in diabetic foot
infections. Diabet Foot Ankle. 2(7463)2011.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Sharma S and Verma K: Skin and soft tissue
infection. Indian J Pediatr. 68 (Suppl 3):S46–S50. 2001.PubMed/NCBI View Article : Google Scholar
|