Introduction
Acute ischemic stroke (AIS) is one of the primary
triggers of disability, as well as mortality worldwide with a
substantial burden on health systems and families (1-3).
AIS of the posterior circulation as a result of vertebrobasilar
artery occlusions (VBAOs) constitutes 10-20% of all large vessel
occlusions (LVOs) with a mortality rate of almost 90% and most
frequently affecting the basilar artery (BA) (4-8).
The posterior circulation mainly provides blood supply to the main
parts of the brain, such as the brainstem, thalamus and cerebellum
(9).
Intravenous tissue plasminogen activator (t-PA)
administered within 4.5 h of the stroke is currently the recommend
treatment for patients with thrombolytic ischemic strokes (10,11). Of
note, mechanical thrombectomy (MT) for the treatment of acute
thrombolytic ischemic stroke has exhibited favorable outcomes in
both anterior and posterior LVOs (5,12-17).
Almost all studies involving acute VBAO have focused primarily on
prognostic factors, such as the severity of neurologic deficits,
the time of onset to treatment, the location of the occlusion, the
state of collaterals, treatment or management options, as well as
timely reperfusion (18-21).
Prognosis is often poor with a high mortality rate
when early reperfusion is not achieved in patients with basilar
artery occlusion (BAO) (19,22). Thus, MT for patients with BAO has
been shown to be associated with good clinical outcomes with a wide
range of functional attainments (13,22).
Although a few studies have demonstrated that flow reversal, as
well as the patency of the vertebral arteries (VAs) may also affect
the recanalization success, only a few studies have reported MT in
vertebral artery occlusions (VAOs) (5,7,23,24).
Factors associated with a good outcome have not yet been adequately
investigated. Thus, the present study focused on factors associated
with a good prognosis following MT.
Specifically, the precise association between
reperfusion and outcome has not yet been fully established in
patients with BAO and VAO. Thus, the present study describes the
authors' institutional experience on MT for VAOs, as well as
BAOs.
Patients and methods
Patients
The present study retrospectively analyzed a series
of 17 patients with acute VAOs and BAOs treated using MT at the
Department of Neurosurgery, Jiangyin Hospital (Jiangyin, China)
from January, 2017 to December, 2020. The study was approved by the
Research Committee of Jiangyin Hospital. Patients, as well as
relatives were made aware of the intention to include them in a
study during follow-up visits at the outpatient department. Written
informed consents, as well as consents for publication were
obtained from all the patients and the hospital. In all patients,
information such as sex and age, time from admission to the onset
of femoral artery access, the number of thrombi removed, the time
of femoral artery access to recanalization, pre- and post-operative
National Institutes of Health Stroke Scale (NIHSS) scores, pre- and
post-operative thrombolysis in cerebral infarction (TICI) scores,
as well as modified Rankin scale (mRS) scores were documented and
analyzed. All patient information obtained is presented in Table I.
 | Table IClinical data of the 17 patients with
acute ischemic stroke in the posterior circulation who underwent
emergency stent mechanical thrombectomy. |
Table I
Clinical data of the 17 patients with
acute ischemic stroke in the posterior circulation who underwent
emergency stent mechanical thrombectomy.
| | mTICI score | NIHSS score | |
|---|
| Patient no. | Sex | Age (years) | Location of
lesion | NTR | DNT (Min) | TAR- (Min) | Pre-op | Post-op | Pre-op | Post-op (1
week) | mRS (90 days) |
|---|
| 1 | M | 46 | Basilar artery | 4 | 43 | 135 | 0 | 2b | 10 | 6 | 2 |
| 2 | M | 65 | Left vertebral
artery (V1) | 5 | 57 | 310 | 0 | 3 | 10 | 2 | 1 |
| 3 | M | 60 | Left vertebral
artery (V2) | 4 | 47 | 340 | 0 | 1 | 25 | - | 6 |
| 4 | M | 54 | Basilar artery | 5 | 58 | 300 | 0 | 2a | 17 | - | 6 |
| 5 | M | 56 | Left vertebral
artery (V1) | 3 | 42 | 100 | 0 | 1 | 12 | - | 6 |
| 6 | F | 75 | Basilar artery | 2 | 97 | 100 | 0 | 3 | 25 | 8 | 3 |
| 7 | F | 74 | Basilar artery | 3 | 52 | 245 | 0 | 2a | 20 | - | 6 |
| 8 | M | 64 | Basilar artery | 4 | 115 | 170 | 0 | 3 | 20 | 10 | 3 |
| 9 | M | 64 | Left Vertebral
Artery (V4) | 2 | 31 | 180 | 0 | 3 | 16 | 3 | 2 |
| 10 | M | 75 | Basilar artery | 3 | 29 | 156 | 0 | 3 | 26 | 6 | 2 |
| 11 | F | 74 | Basilar artery | 3 | 51 | 188 | 0 | 3 | 19 | 3 | 1 |
| 12 | M | 47 | Left vertebral
artery (V1) | 1 | 29 | 65 | 0 | 3 | 4 | 2 | 1 |
| 13 | M | 70 | Basilar artery | 3 | 361 | 135 | 0 | 3 | 16 | 2 | 1 |
| 14 | M | 57 | Basilar artery | 4 | 61 | 285 | 0 | 2a | 17 | 10 | 4 |
| 15 | M | 54 | Basilar artery | 2 | 81 | 105 | 0 | 3 | 9 | 1 | 0 |
| 16 | M | 34 | Right Vertebral
artery (V1) | 3 | 21 | 120 | 0 | 3 | 15 | 4 | 1 |
| 17 | F | 52 | Basilar artery | 2 | 43 | 91 | 0 | 3 | 12 | 3 | 1 |
Indications and contraindications
The indications for MT included the following: i)
The clinical diagnosis was in line with AIS of the posterior
circulation, the patients were hospitalized within 24 h of onset,
and the presence of neurological deficits related to posterior
circulation ischemia, such as dizziness, gaze disturbance, visual
field defect, visual impairment, coma, etc.; ii) a cerebrovascular
evaluation with computer tomographic angiography (CTA) revealed
that the BA and/or VA was occluded, and a head computer tomography
(CT) scan ruled out intracranial hemorrhage; iii) the patient's
family agreed to an informed consent and signed the surgical
consent form.
The contraindications for MT were the following: i)
A head CT scan indicated the presence of intracranial hemorrhage or
large-area cerebral infarction in the posterior circulation
(>2/3 of the pons or midbrain volume or cerebellar hemisphere
infarction); ii) a history of active bleeding or a tendency to
hemorrhage; iii) severe disability, mRS score >2 points; iv)
severe renal insufficiency; v) the patient had a clear history of
allergies to contrast agents.
Pre-operative evaluation
After the patient was admitted to hospital, a
neurologist completed a physical examination, a neurological
functional assessmen.t as well as NIHSS scoring in the emergency
room. The emergency physician also performed a head CT scan to rule
out intracranial hemorrhage, as well as a head and neck CTA to
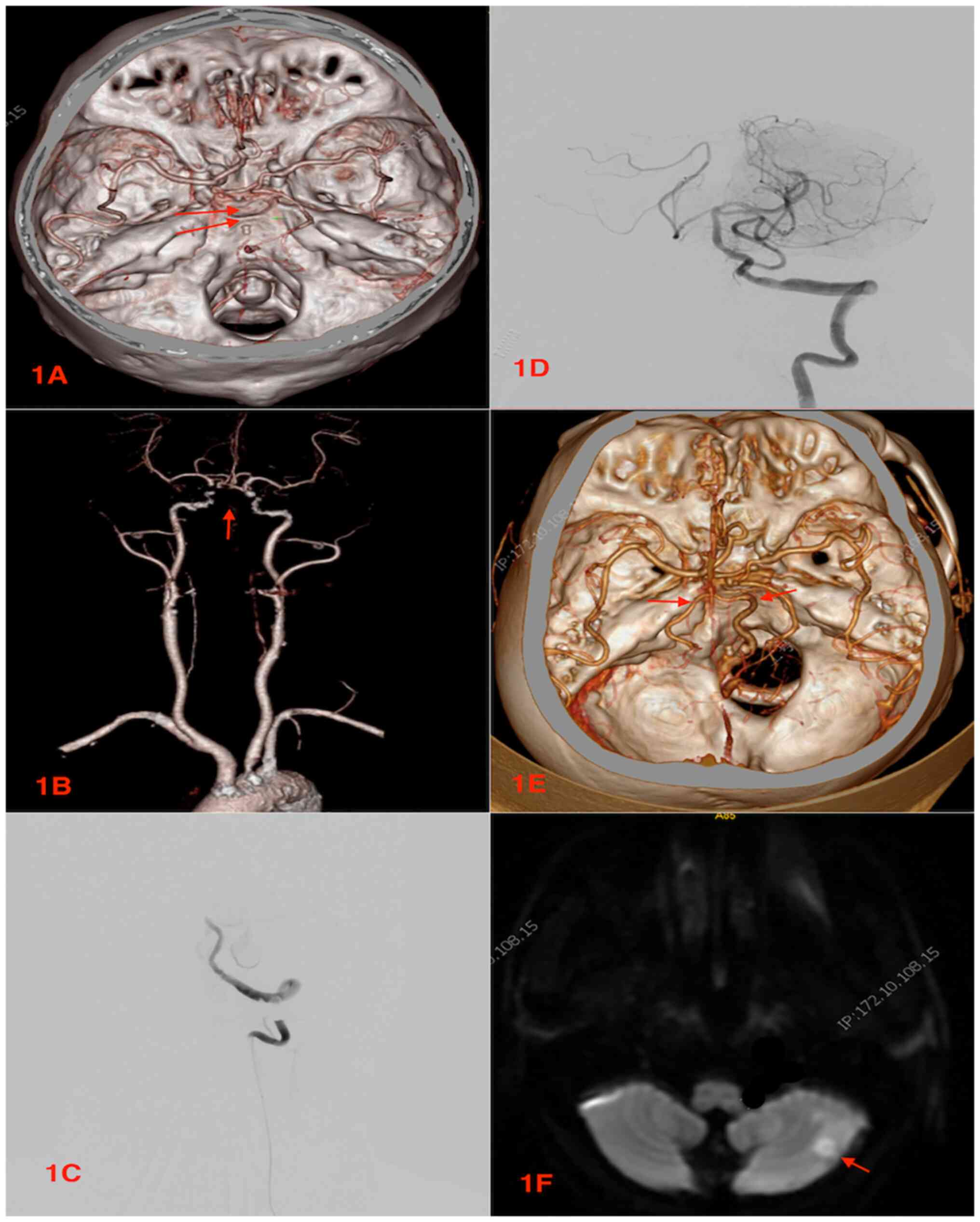
identify BAO (Fig. 1A and B) and/or VAO. In addition, pre-operative
magnetic resonance images (MRIs) were performed in all patients to
detect brainstem infarction. In all patients, the pre-operative CTA
revealed the presence of large vessel occlusion, such as the BAO or
VAO. The time from admission to the onset of femoral artery
puncture/accesses was documented prior to the commencement of
endovascular surgeries.
Anatomical divisions of the
vertebrobasilar artery
The VA is characteristically divided into four
segments, namely V1-V4 (25,26) as follows: V1, also denoted as the
pre-foraminal segment (starts from the subclavian artery to the
transverse foramen of C6); V2, also denoted as the foraminal
segment (starts from the transverse foramen of C6 to the transverse
foramen of C2); V3, also denoted as the atlantic, extradural or
extraspinal segment (starts from C2, where the artery loops, turns
lateral and upwards into the transverse foramen and progresses via
C1 to penetrate the dura; V4, also denoted as the intradural or
intracranial segment (starts from the dura at the lateral border of
the posterior atlanto-occipital membrane to their convergence on
the medulla to constitute the BA) (25,26).
Endovascular procedures
All procures were performed under general
anesthesia. The entire surgical procedures were carried out
strictly as previously described by Luo et al (8). After securing the femoral artery
access, a 6F/8F guide catheters were maneuvered into the BA or the
VAs via the subclavian arteries and initial angiographies performed
to determine the locations of the occlusions (Fig. 1C). Using a coaxial system, 0.21-inch
microcatheters (Rebar microcatheter; Covidien; Medtronic) and
0.014-inch microguide wires (Transend; Stryker) were advanced into
the thrombi as far as the distal ends of the occluded vessels.
Angiographies were then performed to confirm that the distal
vasculars were patent and no pathology was found in the lumen.
In all patients, Solitaire ABs or FRs (EV3
Neurovascular) were utilized for the MT. The solitaire devices were
carefully maneuvered to the occluded segments via microcatheters
and the stent retrievers were unsheathed to allow for complete
expansion through the thrombi. The devices often created bypasses
that restored blood flow across the occluded segments. Again,
angiography was performed to determine the patency of the distal
arteries, after which the fully deployed the solitaire devices were
resheathed. Thrombectomies were performed via the withdrawal of the
solitaire devices and the delivery microcatheters as a single unit.
In the case that the angiography revealed that the occluded
arteries were patent (Fig. 1D), and
blood flow rates were basically normal (TICI 2b and above), the
procedures were then completed.
In the case that the angiography still revealed
stenosis of the BA or VA and the anterior blood flow did not meet a
TICI score of 2b, balloon angioplasty (GatewayTM, Boston Scientific
Corporation) was then first performed. In the case that the
angiography still revealed no patency, the stent placements were
performed to ensure that the flow rates met the TICI score of ≥2b.
In all patients who underwent the MTs, the number of thrombi
removed were documented. In addition, the time from femoral artery
puncture/access to the recanalization of the occluded arteries was
documented.
Post procedure management, efficacy
evaluation and follow-up
Heparin infusion was used during and immediately
after the surgery. Intravenous tirofiban used during the surgery
was also maintained after the surgery. Aspirin (300 mg) and
clopidogrel (300 mg) were administered via the rectal route
immediately after the surgery. All the patients were admitted to
the intensive care unit (ICU) for monitoring and treatment, and
transferred to the general ward after their conditions were stable.
In all patients, immediate post-operative CT scans were performed
to rule bleeding 24 h after the surgery. CTAs were also performed
to confirm recanalization (Fig. 1E).
In addition, post-operative MRIs were performed to assess
infarctions following the procedure (Fig. 1F).
Furthermore, in all patients, the TICI grade was
scored as follows (22,27): 0, no recanalization (no perfusion or
anterograde flow beyond the occlusion site); 1, minimal
recanalization (contrast medium passes the area of occlusion but
fails to opacify the entire cerebral bed distal to the obstruction
during the angiographic run); 2, partial recanalization (2a,
partial filling, <50% of territory visualized; 2b, partial
filling, ≥50% of territory visualized); and 3, complete
recanalization (total reperfusion with normal filling). At the ICU,
the NIHSS scores of all the patients were assessed 7 days after the
surgery.
mRS was also used to evaluate the prognosis of the
patients up to 90 days after the surgery. The mRS scores were
assessed as follows (22,28): 0, no symptoms; 1, no clinically
relevant disability; 2, slight disability (able to look after own
affairs without aid but not to a full extent); 3, moderate
disability (requires some aid but able to walk unaided); 4,
moderately severe disability (unable to attend to own bodily needs
or to walk without aid); 5, severe disability (requires constant
nursing care); and 6, deceased.
Results
Demographic and preoperative
evaluations
A total of 17 patients were included in the present
analysis. Among these, 13 patients were males while 4 were females.
Their ages ranged from 34-75 years, with an average age of 60
years. The time from the onset of admission to the femoral artery
puncture/access was 3.0-8.0 h, with an average time of 5.5 h. The
basic clinical information of the 17 patients is presented in
Table I. In all the patients,
pre-operative MRIs did not reveal brainstem infarction subsequent
to their surgeries.
Anatomical distribution of
lesions
Out of the 17 patients, 11 patients had BAOs while 6
patients had VAOs (Table II). In
addition, out of the 6 patients with VAOs, five occlusions were
observed on the left side, while one occlusion was observed on the
right side. Furthermore, out of the out of the 6 patients with
VAOs, four occlusions were observed at the V1 segment of the VA,
one at the V2 segment and one at the V4 segment. Thus, in the
present study, there were more patients with BAOs than VAOs. More
patients also had V1 occlusions compared to V2 and V4 occlusions.
No patient had a V3 segment occlusion.
 | Table IIStratification of patients as per the
type of artery occluded, recanalization rate and the functional
outcomes of patients. |
Table II
Stratification of patients as per the
type of artery occluded, recanalization rate and the functional
outcomes of patients.
| | mTICI score | mRS score at 90
days |
|---|
| Artery
occluded | No. of
patients | 1-2a | 2b or 3 | 0-2 | 3-5 | 6 |
|---|
| BA | 11 | 3 | 8 | 6 | 3 | 2 |
| VA | 6 | 2 | 4 | 4 | - | 2 |
| Total | 17 | 5 | 12 | 10 | 3 | 4 |
Operative outcomes
After 1-7 times of MT with Solitaire AB, 70.6%
(12/17) of the patients achieved complete recanalization (TICI 2b
or 3); 17.4% (3/17) achieved partial recanalization (TICI 2a),
while 11.7% (2/17) of the patients achieved minimal recanalization
(TICI 1). Out of the 11 patients with BAOs, 72.7% (8/11) achieved a
successful recanalization (TICI 2b or 3), while out of the 6
patients with VAOs, 66.7% (4/6) achieved a successful
recanalization (mTICI 2b or 3). No notable differences in
recanalization (TICI 2b or 3) were observed between the patients
with BAO and VAOs (Table II). The
average time from femoral artery puncture/access to recanalization
was 172 min. No notable differences were observed between the time
from femoral artery puncture/access to recanalization and
prognosis. This may be due to the small sample size of the study.
All the 12 patients who achieved successful recanalization of the
arteries (TICI 2b or 3) survived after their surgery. Out of the 3
patients who achieved partial recanalization (TICI 2a), 1 patient
had severe stenosis of the BA with acute occlusion and balloon
dilation at the stenotic portion resulted in rupture and bleeding
of the BA and subsequently in mortality after the surgery.
The other 2 patients had larger areas of cerebral
infarctions after the surgery, and decompressive craniostomies were
performed to allow for brain expansion, as well as brain hernias
and 1 patient succumbed. The 2 patients with TICI 2a who succumbed
had occlusions in the BA. The 2 patients who achieved minimal
recanalization (TICI 1) succumbed immediately after their
surgeries. These 2 patients had occlusions in the V1 and V2
segments of the VA. All the deceased patients succumbed immediately
after the surgeries (<24 h). The average number of thrombi
removed was three. In addition, the average time from femoral
artery puncture/access to recanalization was 178 min. Thus, an
average time of ~5.5 h from patient admittance to recanalization
with a 70.6% recanalization rate with an overall good functional
outcome of 58.8% at 90 days suggests that, patients whose surgeries
were performed within 5 h of admittance still have hope for
recanalization compared to an initial 1.5 h average time for
recanalization.
Efficacy evaluation and follow-up
outcomes
The average NIHSS score prior to surgery was 15.3,
while the average NIHSS score at 1 week after the surgery was 4.5.
Observationally, there was a marked improvement in patient outcomes
when comparing the NIHSS before surgery to the NIHSS at 1 week
after the surgery. The prognoses of the patients were assessed at
90 days post-surgery using the mRS. A good prognosis was defined as
a mRS score ≤2 (Table II). It was
observed that (Table I) 41.17%
(7/17) of the patients had mRS scores of 0 and 1 (good prognosis).
In addition, 29.41% (5/17) of the patients had mRS scores of 2 and
3 (mild to moderate disability). Furthermore, 5.8% (1/17) of the
patients had mRS scores of 4 and 5 (severely disability), and
23.53% (4/17) of the patients had a mRS score of 6 (deceased).
Out of the 11 patients with BAOs, 54.5% (6/11)
achieved a good functional outcome (mRS 0-2), while out of the 6
patients with VAOs, 66.7% (4/6) achieved a good functional outcome
(mRS 0-2). The overall good functional outcome in the patients was
58.8% (10/17) as per the mRS score range of 0-2 (Table II). In addition, a mortality rate of
23.53% was observed and the causes of death were as a result of
intraoperative procedural complications. At 2 years of follow-up,
the patients with favorable outcomes revealed no further
neurological deficits and massive improvements in their quality of
life. No patients were lost during follow-up.
Discussion
The effectiveness of MT in posterior circulation
stroke is still confronted with uncertainty, notwithstanding the
successful outcomes in large vessel anterior circulation stroke
(6,12,15,16,18,29).
Overall, out of the 17 patients in the present study, BAOs were
observed in 64.7% (11/17) of the patients, while in 35.3% (6/17) of
the patients had VAOs. Furthermore, 70.6% of the patients achieved
recanalization (TICI 2b-3), with 41.17, 29.41 and 29.41% of the
patients attaining a good prognosis, mild to moderate disability
and severely disability, respectively as per the mRS scores. The
overall good functional outcome of the patients was 58.8% (10/17)
as per the mRS score range of 0-2. The patients were predominantly
males with a mean age of 60 years.
Sonig et al (30) reported a series of 12 BAOs treated
with retrievable MT and achieved a successful recanalization (TICI
2b or 3) of 91.7% (11/12) in their patients with a median mRS
scores 2 at discharge and 1 at last follow-up. In addition, Kang
et al (31) demonstrated a
successful reperfusion of 90.3% in patients with acute BAOs who
underwent MT with retrievable stents and achieved a favorable
functional outcome of 46.9% (mRS 0-2) of their patients.
Furthermore, Gory et al (22)
attained 72.2% effective recanalization (TICI 2b or 3) or
reperfusion in their patients with a favorable functional outcome
of 34% (mRS 0-2) and a 2-5% risk of hemorrhage. Baik et al
(18) achieved an overall successful
reperfusion rate of 78% with a favorable clinical outcome of 37% in
their patients.
In the present study, out of the 11 patients with
BAOs, 72.7% (8/11) achieved a successful recanalization (TICI 2b or
3) with a good functional out of 54.5% (6/11) as per the mRS score
range of 0-2. In addition, out of the 6 patients with VAOs, 66.7%
(4/6) achieved a successful recanalization (TICI 2b or 3) with a
functional out of 66.7% (4/6) as per the mRS score range of 0-2.
None of the patients presented with bilateral VAOs or tandem VA-BA
occlusions. Tandem VA-BA occlusions although rare, have been
reported in 16-20% of patients with acute VBAOs (6,18,32).
The initial symptomatology of the patients with
neurological deficits related to posterior circulation ischemia,
was dizziness, gaze disturbance, visual field defect, visual
impairment or coma. A CT scan and CTA were the initial radiological
modalities use in assessing the patient at the emergency after
clinical assessments. A CT scan was used to rule out intracranial
hemorrhage, while CTA was used to detect the BA and VA occlusions.
Nevertheless, magnetic resonance diffusion weighted image is often
the ‘gold standard’ radiological modality for the detection of
ischemic changes in patients with LVO in the posterior circulation
(5,33). Intraoperatively, angiographies are
utilized to confirm occlusions, as well as to assess the patency of
distal arteries.
The NIHSS is a beneficial and realistic means of
assessing stroke severity in patients (5,34). It is
devised to evaluate stroke symptoms associated with the anterior
circulation with more emphasis on the limb, as well as speech
impairments and less focus on cranial nerve symptomatology
(5,35). Nevertheless, patients with LVO in the
posterior circulation can have an NIHSS score of 0, with symptoms
such as headaches, vertigo, as well as nausea only in the prodromal
period. Furthermore, the baseline NIHSS score signifies a clinical
evaluation of the collateral state, as well as thrombus severity
(5,19). Thus, a low NIHSS score upon admission
may be due small thrombi or good collaterals leading to positive
outcomes following MT (5). Gory
et al (36) observed that
patients who present with a high NIHSS score had a poorer prognosis
compared to patients with mild-to-moderate deficits at the time of
treatment, notwithstanding recanalization and thus, they proposed
an NIHSS cut-off value of 13. The present study revealed that the
average NIHSS score prior to surgery was 15.3, while the average
NIHSS score at 1 week after the surgery was 4.5. Thus,
observationally, there was a notable improvement in outcomes when
comparing the NIHSS before surgery to the NIHSS at 1 week after
surgery. These findings are therefore consistent with those of the
previous studies mentioned above.
Solitaire thrombectomy for AIS treatment is
instinctively practical, very auspicious, and is already used in
several institutions (37-39).
Miteff et al (37) revealed
that Solitaire thrombectomy attained a high rate of recanalization
which translated into the good prognosis of patients with acute
stroke caused by proximal occlusion within the cerebral arteries.
Using Solitaire AB, Luo et al (8) achieved an overall recanalization rate
of 89.9%, and 36.2% of their patients achieved a favorable outcome
at 90 days. Furthermore, other studies have demonstrated that, on
average, ~81% of patients often attain a recanalization rate of
~30%, attaining favorable outcomes at 90 days (13,37,40). The
present study used Solitaire AB or FR to treat 17 patients with
BAOs and VAOs and attained a 70.6% recanalization rate with an
overall good functional outcome of 58.8% at 90 days; these finding
are comparable to those of the aforementioned previous studies. The
average number of thrombi removed in the present case series was
three.
Luo et al (8)
indicated that the collateral status prior to MT, as well as the
baseline NIHSS score were independent predictors of mortality at 90
days in patients with acute posterior circulation stroke who
underwent Solitaire AB thrombectomy. Studies have demonstrated that
the reperfusion time is one of the key predictors of a good
prognosis of patients with anterior circulation, as well as
posterior circulation stroke (5,12-14,41).
Nevertheless, other studies have not found any link between the
reperfusion time and good prognosis of patients with posterior
circulation strokes (5,19,42,43).
Baik et al (18) observed a
poor outcome despite the good recanalization rate, which may have
been due to the longer procedural time.
Baik et al (18) observed a mortality rate of 21%. Luo
et al (8) observed a
mortality rate of 24.6% at 90 days. Similar studies observed
mortality rates ranging from 21-33% at 90 days (5,22,30,31).
The present study observed a mortality rate of 23.53% and the
causes of death were intraoperative procedural complications. The
present study anticipated a better prognosis and less or no
mortality in patients with VAOs, as there are two VAs and the
patent one can compensate the occluded one, as compare to BAOs.
Comparatively, MT often results in higher recanalization rates than
t-PA therapy; however, better outcomes with MT are not always
exhibited (12,18,44). The
present study had certain limitations as this was a retrospective
study with small case series, which did not allow for satisfactory
conclusions, as a detailed statistical analysis could not be
performed for the majority of variables; thus, statistical analyses
were not performed. In addition, the study was conducted in a
single hospital. Thus, further prospective studies with larger
sample sizes and several hospitals are warranted to arrive at
satisfactory conclusions.
In conclusion, the present study observed a notable
improvement in patient outcomes comparing the NIHSS before surgery
to the NIHSS at 1 week after surgery. Thus, a lower NIHSS score
prior to MT may be a good prognostic factor. Herein, recanalization
rate of 70.6% with an overall good functional outcome of 58.8% at
90 days was attained, which is comparable to that of previous
studies (as those aforementioned). An average time of ~5.5 h from
patient admittance to recanalization with a 70.6% recanalization
rate and an overall good functional outcome of 58.8% at 90 days
suggests that, patients whose surgeries are performed within 5 h of
admittance, still have hope of recanalization compared to the
initial 1.5 h average time for recanalization.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
XY, YF, JJ, ZX, WM and SAR were involved in the
conception and design of the study, in data acquisition and
follow-up, and in the editing of the manuscript. SAR was involved
in the preparation of the manuscript. All authors have carefully
reviewed the manuscript and have read and approved the final
version. XY and WM confirm the authenticity of all the raw
data.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of Jiangyin Hospital [Approval no. 2016ER (058)] and
written informed consent was obtained from all participants. All
methods were performed in accordance with the relevant guidelines
and regulations.
Patient consent for publication
Written informed consents as well as consents for
publication were obtained from all the patients and the
hospital.
Competing interests
All authors declare that they have no competing
interests.
References
|
1
|
Massari F, Henninger N, Lozano JD, Patel
A, Kuhn AL, Howk M, Perras M, Brooks C, Gounis MJ, Kan P, et al:
ARTS (aspiration-retriever technique for stroke): Initial clinical
experience. Interv Neuroradiol. 22:325–332. 2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Rha JH and Saver JL: The impact of
recanalization on ischemic stroke outcome: A meta-analysis. Stroke.
38:967–973. 2007.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Fargen KM, Meyers PM, Khatri P and Mocco
J: Improvements in recanalization with modern stroke therapy: A
review of prospective ischemic stroke trials during the last two
decades. J Neurointerv Surg. 5:506–511. 2013.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Styczen H, Fischer S, Yeo LL, Yong-Qiang
Tan B, Maurer CJ, Berlis A, Abdullayev N, Kabbasch C, Kastrup A,
Papanagiotou P, et al: Approaching the boundaries of endovascular
treatment in acute ischemic stroke: Multicenter experience with
mechanical thrombectomy in vertebrobasilar artery branch
occlusions. Clin Neuroradiol. 31:791–798. 2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Pazuello GB, de Castro-Afonso LH,
Fornazari VR, Nakiri GS, Abud TG, Monsignore LM, Dias FA,
Martins-Filho RK, Camilo MR, Aléssio-Alves FF, et al: Thrombectomy
for posterior circulation stroke: Predictors of outcomes in a
Brazilian registry. World Neurosurg. 147:e363–e372. 2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Baik SH, Jung C, Kim BM and Kim DJ:
Mechanical thrombectomy for tandem vertebrobasilar stroke:
Characteristics and treatment outcome. Stroke. 51:1883–1885.
2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Boeckh-Behrens T, Pree D, Lummel N,
Friedrich B, Maegerlein C, Kreiser K, Kirschke J, Berndt M, Lehm M,
Wunderlich S, et al: Vertebral artery patency and thrombectomy in
basilar artery occlusions. Stroke. 50:389–395. 2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Luo G, Mo D, Tong X, Liebeskind DS, Song
L, Ma N, Gao F, Sun X, Zhang X, Wang B, et al: Factors associated
with 90-day outcomes of patients with acute posterior circulation
stroke treated by mechanical thrombectomy. World Neurosurg.
109:e318–e328. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Sciacca S, Lynch J, Davagnanam I and
Barker R: Midbrain, pons, and medulla: Anatomy and syndromes.
Radiographics. 39:1110–1125. 2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Memon MZ, Kushnirsky M, Brunet MC, Saini
V, Koch S and Yavagal DR: Mechanical thrombectomy in isolated large
vessel posterior cerebral artery occlusions. Neuroradiology.
63:111–116. 2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Powers WJ, Rabinstein AA, Ackerson T,
Adeoye OM, Bambakidis NC, Becker K, Biller J, Brown M, Demaerschalk
BM, Hoh B, et al: 2018 Guidelines for the early management of
patients with acute ischemic stroke: A guideline for healthcare
professionals from the American heart association/American stroke
association. Stroke. 49:e46–e110. 2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Schonewille WJ, Wijman CA, Michel P,
Rueckert CM, Weimar C, Mattle HP, Engelter ST, Tanne D, Muir KW,
Molina CA, et al: Treatment and outcomes of acute basilar artery
occlusion in the basilar artery international cooperation study
(BASICS): A prospective registry study. Lancet Neurol. 8:724–730.
2009.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Gory B, Eldesouky I, Sivan-Hoffmann R,
Rabilloud M, Ong E, Riva R, Gherasim DN, Turjman A, Nighoghossian N
and Turjman F: Outcomes of stent retriever thrombectomy in basilar
artery occlusion: An observational study and systematic review. J
Neurol Neurosurg Psychiatry. 87:520–525. 2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Giorgianni A, Biraschi F, Piano M,
Mardighian D, Gasparotti R, Frigerio M, Pero G, Quilici L, Crispino
M, Pellegrino C, et al: Endovascular treatment of acute basilar
artery occlusion: Registro endovascolare lombardo occlusione
basilar artery (RELOBA) study group experience. J Stroke
Cerebrovasc Dis. 27:2367–2374. 2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Meinel TR, Kaesmacher J,
Chaloulos-Iakovidis P, Panos L, Mordasini P, Mosimann PJ, Michel P,
Hajdu S, Ribo M, Requena M, et al: Mechanical thrombectomy for
basilar artery occlusion: Efficacy, outcomes, and futile
recanalization in comparison with the anterior circulation. J
Neurointerv Surg. 11:1174–1180. 2019.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Zeng Q, Tao W, Lei C, Dong W and Liu M:
Etiology and risk factors of posterior circulation infarction
compared with anterior circulation infarction. J Stroke Cerebrovasc
Dis. 24:1614–1620. 2015.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Matsumoto H, Nishiyama H, Tetsuo Y,
Takemoto H and Nakao N: Initial clinical experience using the
two-stage aspiration technique (TSAT) with proximal flow arrest by
a balloon guiding catheter for acute ischemic stroke of the
anterior circulation. J Neurointerv Surg. 9:1160–1165.
2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Baik SH, Park HJ, Kim JH, Jang CK, Kim BM
and Kim DJ: Mechanical thrombectomy in subtypes of basilar artery
occlusion: Relationship to recanalization rate and clinical
outcome. Radiology. 291:730–737. 2019.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Singer OC, Berkefeld J, Nolte CH, Bohner
G, Haring HP, Trenkler J, Gröschel K, Müller-Forell W, Niederkorn
K, Deutschmann H, et al: Mechanical recanalization in basilar
artery occlusion: The ENDOSTROKE study. Ann Neurol. 77:415–424.
2015.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Cross DT III, Moran CJ, Akins PT, Angtuaco
EE and Diringer MN: Relationship between clot location and outcome
after basilar artery thrombolysis. AJNR Am J Neuroradiol.
18:1221–1228. 1997.PubMed/NCBI
|
|
21
|
Voetsch B, DeWitt LD, Pessin MS and Caplan
LR: Basilar artery occlusive disease in the New England medical
center posterior circulation registry. Arch Neurol. 61:496–504.
2004.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Gory B, Mazighi M, Blanc R, Labreuche J,
Piotin M, Turjman F and Lapergue B: Mechanical thrombectomy in
basilar artery occlusion: Influence of reperfusion on clinical
outcome and impact of the first-line strategy (ADAPT vs stent
retriever). J Neurosurg. 129:1482–1491. 2018.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Mayer TE, Hamann GF and Brueckmann HJ:
Treatment of basilar artery embolism with a mechanical extraction
device: Necessity of flow reversal. Stroke. 33:2232–2235.
2002.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Clarençon F, Blanc R, Gallas S, Hosseini H
and Gaston A: Thrombectomy for acute basilar artery occlusion by
using double Merci retriever devices and bilateral temporary
vertebral artery flow reversal. Technical note. J Neurosurg.
111:53–56. 2009.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Campero A, Rubino PA and Rhoton AL:
Anatomy of the vertebral artery. In: Pathology and surgery around
the vertebral artery. Springer, Paris, pp29-40, 2011.
|
|
26
|
George B and Cornelius J: Vertebral
artery: Surgical anatomy. Oper Tech Neurosurg. 4:168–181. 2001.
|
|
27
|
Schulz UG and Fischer U: Posterior
circulation cerebrovascular syndromes: Diagnosis and management. J
Neurol Neurosurg Psychiatry. 88:45–53. 2017.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Olavarría VV, Brunser A, Cabral N, Martins
S, Muñoz-Venturelli P, Cavada G and Lavados PM: The distribution of
the modified Rankin scale scores change according to eligibility
criteria in acute ischemic stroke trials: A consideration for
sample size calculations when using ordinal regression analysis.
Contemp Clin Trials Commun. 5:133–136. 2017.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Goyal M, Menon BK, van Zwam WH, Dippel DW,
Mitchell PJ, Demchuk AM, Dávalos A, Majoie CB, van der Lugt A, de
Miquel MA, et al: Endovascular thrombectomy after large-vessel
ischaemic stroke: A meta-analysis of individual patient data from
five randomised trials. Lancet. 387:1723–1731. 2016.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Sonig A, Krishna C, Natarajan SK, Liu J,
Hopkins LN, Snyder KV, Levy EI and Siddiqui AH: Stent
retriever-assisted mechanical thrombectomy for acute basilar artery
occlusion: Single US institution experience. Oper Neurosurg
(Hagerstown). 12:250–259. 2016.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Kang DH, Jung C, Yoon W, Kim SK, Baek BH,
Kim JT, Park MS, Kim YW, Hwang YH, Kim YS, et al: Endovascular
thrombectomy for acute basilar artery occlusion: A multicenter
retrospective observational study. J Am Heart Assoc.
7(e009419)2018.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Cohen JE, Leker RR, Gomori JM, Eichel R,
Rajz G, Moscovici S and Itshayek E: Emergent revascularization of
acute tandem vertebrobasilar occlusions: Endovascular approaches
and technical considerations-confirming the role of vertebral
artery ostium stenosis as a cause of vertebrobasilar stroke. J Clin
Neurosci. 34:70–76. 2016.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Werner MF, López-Rueda A, Zarco FX, Blasco
J, San Román L, Amaro S, Carrero E, Valero R, Oleaga L, Macho JM
and Bargalló N: Value of posterior circulation ASPECTS and
pons-midbrain index on non-contrast CT and CT angiography source
images in patients with basilar artery occlusion recanalized after
mechanical thrombectomy. Radiologia (Engl Ed). 61:143–152.
2019.PubMed/NCBI View Article : Google Scholar : (In English,
Spanish).
|
|
34
|
Chalos V, van der Ende NAM, Lingsma HF,
Mulder MJHL, Venema E, Dijkland SA, Berkhemer OA, Yoo AJ, Broderick
JP, Palesch YY, et al: National institutes of health stroke scale:
An alternative primary outcome measure for trials of acute
treatment for ischemic stroke. Stroke. 51:282–290. 2020.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Kayan Y, Meyers PM, Prestigiacomo CJ, Kan
P and Fraser JF: Society of NeuroInterventional Surgery. Current
endovascular strategies for posterior circulation large vessel
occlusion stroke: Report of the Society of neurointerventional
surgery standards and guidelines committee. J Neurointerv Surg.
11:1055–1062. 2019.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Gory B, Mazighi M, Labreuche J, Blanc R,
Piotin M, Turjman F and Lapergue B: ETIS (Endovascular Treatment in
Ischemic Stroke) Investigators. Predictors for mortality after
mechanical thrombectomy of acute basilar artery occlusion.
Cerebrovasc Dis. 45:61–67. 2018.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Miteff F, Faulder KC, Goh AC, Steinfort
BS, Sue C and Harrington TJ: Mechanical thrombectomy with a
self-expanding retrievable intracranial stent (Solitaire AB):
Experience in 26 patients with acute cerebral artery occlusion.
AJNR Am J Neuroradiol. 32:1078–1081. 2011.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Gao F, Lo WT, Sun X, Mo DP, Ma N and Miao
ZR: Combined use of mechanical thrombectomy with angioplasty and
stenting for acute basilar occlusions with underlying severe
intracranial vertebrobasilar stenosis: Preliminary experience from
a single chinese center. AJNR Am J Neuroradiol. 36:1947–1952.
2015.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Huo X, Gao F, Sun X, Ma N, Song L, Mo D,
Liu L, Wang B, Zhang X and Miao Z: Endovascular mechanical
thrombectomy with the solitaire device for the treatment of acute
basilar artery occlusion. World Neurosurg. 89:301–308.
2016.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Andersson T, Kuntze Söderqvist Å, Söderman
M, Holmin S, Wahlgren N and Kaijser M: Mechanical thrombectomy as
the primary treatment for acute basilar artery occlusion:
Experience from 5 years of practice. J Neurointerv Surg. 5:221–225.
2013.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Lee HN, Kim BT, Im SB, Hwang SC, Jeong JH,
Chung MY, Park JH and Shin DS: Implications of mechanical
endovascular thrombectomy for acute basilar and posterior cerebral
artery occlusion. J Cerebrovasc Endovasc Neurosurg. 20:168–175.
2018.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Kaneko J, Ota T, Tagami T, Unemoto K,
Shigeta K, Amano T, Ueda M, Matsumaru Y, Shiokawa Y and Hirano T:
TREAT Study Group. Endovascular treatment of acute basilar artery
occlusion: Tama-REgistry of acute thrombectomy (TREAT) study. J
Neurol Sci. 401:29–33. 2019.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Munich SA, Vakharia K and Levy EI:
Overview of mechanical thrombectomy techniques. Neurosurgery. 85
(Suppl 1):S60–S67. 2019.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Molina CA, Chamorro A, Rovira À, de Miquel
A, Serena J, Roman LS, Jovin TG, Davalos A and Cobo E: REVASCAT: A
randomized trial of revascularization with SOLITAIRE FR device vs
best medical therapy in the treatment of acute stroke due to
anterior circulation large vessel occlusion presenting within
eight-hours of symptom onset. Int J Stroke. 10:619–626.
2015.PubMed/NCBI View Article : Google Scholar
|