Introduction
Meningiomas are non-glial tumors of the central
nervous system (CNS), accounting for ~37.6% of all intracranial
tumors (1). There is a wide variety
of symptoms in cases of symptomatic meningiomas, arising from the
compression of nearby structures, straight attacks on or immediate
changes in the brain, or due to the barrier of cerebrospinal fluid
pathways or vessels (2).
Meningiomas are neoplasms that commonly occur in the
brain and spine. Specifically, when occurring in the brain, there
are meningothelial cell neoplasms, which commonly attach to the
inner side of the dura matter (3).
The most common anatomical locations of meningiomas
are falcine (18-22%), convexity (20-34%) and parasagittal (3). Ectopic meningiomas in the sphenoid and
middle cranial fossa are more uncommon, and the majority of these
occur in the skull of the head and neck area. Other much rarer
locations involve the mediastinum, retroperitoneum, lungs, pelvis
and extremities (3). Magnetic
resonance imaging (MRI) is the diagnostic tool of choice for the
study of meningiomas, given its higher contrast differentiation and
its general ability to distinguish between intra- and extra-axial
lesions (4).
Although the exact diagnosis of meningiomas with
standard MRI imaging is, in most cases, easily established, there
are unusual depictions of which make the diagnosis challenging.
Furthermore, several other malignant and non-malignant neoplasms
may mimic meningiomas. Thus, imaging findings can be variable.
Intra-diploic meningiomas can exhibit both osteoblastic and
osteolytic lesions; thus, possible differential diagnoses on
computed tomography (CT) and MRI include fibrous dysplasia
metastasis, osteosarcoma and intraosseous hemangioma (5).
In this context, the present study aimed to provide
the radiologist or neurosurgeon with a better view of their various
potential manifestations in order to be able to distinguish these
tumors from the numerous lesions that can imitate their
presentation and, thus, ameliorate the surgical planning. The
present study describes 7 cases of different types of meningiomas.
All the presented lesions had a histological diagnosis of
meningioma. Differential diagnoses needs be tailored to the tumor
sites and imaging data, although it can mainly include
hypervascular tumors.
Case report
Simple atypical meningiomas. Case
1
A 67-year-old, previously healthy male patient,
complained of an unsteady left-sided upper and lower motor weakness
that began 2 weeks before presentation to the Animus Kyanos Stavros
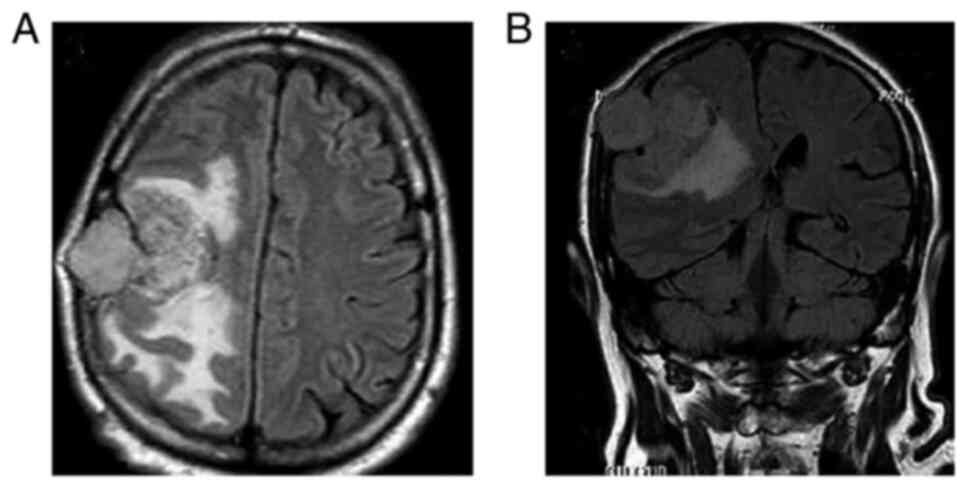
Hospital (Larisa, Greece). An MRI of the brain revealed (Fig. 1) an extra-axial mixed iso-intensity
and hyperintensity mass on the right celebral convexity.
Case 2. A 35-year-old male patient was
admitted to the Animus Kyanos Stavros Hospital, with a complaint of
a 3-month history of left-sided hemiparesis. An MRI (Fig. 2) highlighted a lesion where, before
contrast administration was observed, there was iso-intensity to
slight hypointensity relative to grey matter, and a post-contrast
T1-weighted image identified an extra-axial mass on the right
cerebral convexity. The mass exhibited an avid, homogeneous
enhancement with occasional areas of central necrosis and with the
dural tail sign.
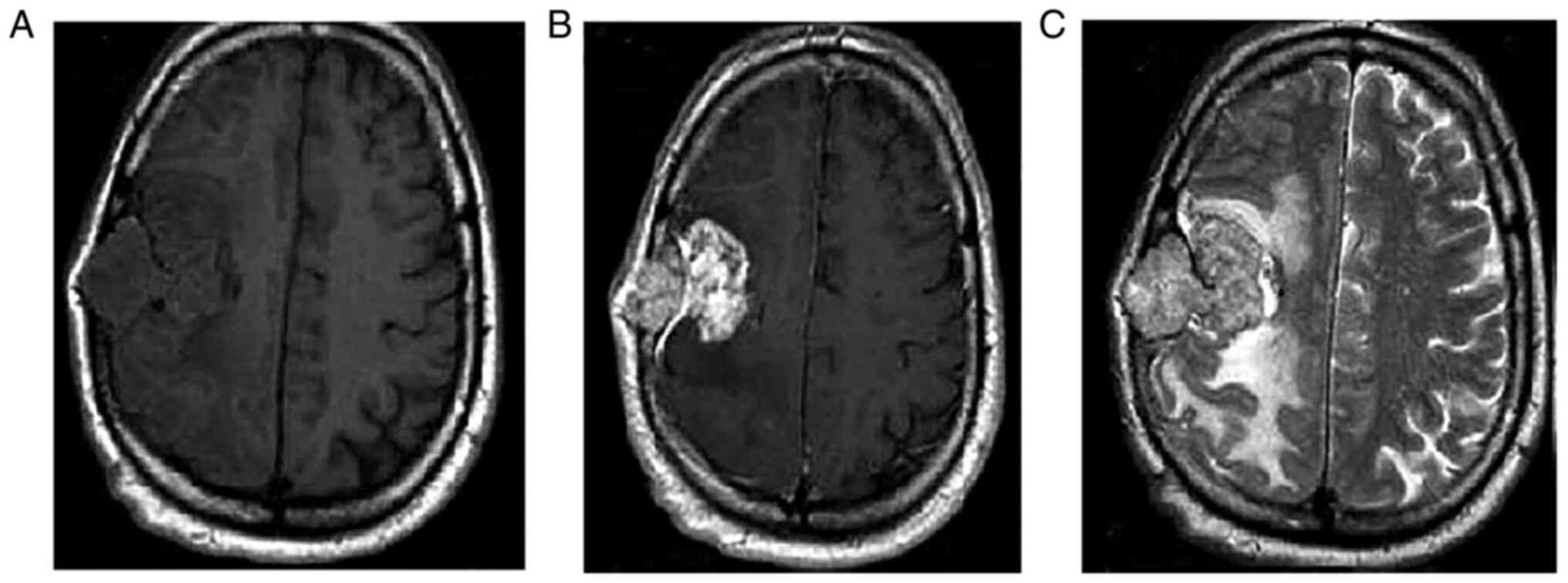
Case 3. A 45-year-old male patient, at 1
month following a head injury, upon a routine examination with an
MRI at the Animus Kyanos Stavros Hospital, was found to have a
small meningioma. In an (A and B) axial diffusion-weighted image
and the corresponding apparent diffusion coefficient map, no
restriction in diffusion or facilitation on the lesion were
observed. An axial T1-weighted image (E) before contrast
administration in axial (G) and coronal (F) T2-weighted images, and
in an axial T2 FLAIR-weighted image (D) and FSPGR with no contrast
(C), revealed an enlargement of the meninga. Following intravenous
contrast administration, an axial T1-weighted image post-contrast
(I) and FSPGR post-contrast (H) revealed a small,
well-circumscribed, extra-axial mass on the left cerebral
convexity. The tumor presented with homogeneous hyperintensity
compared with the gray matter (Fig.
3).
Unusual gigantic extracranial
intracranial parasagittal meningiomas. Case 4
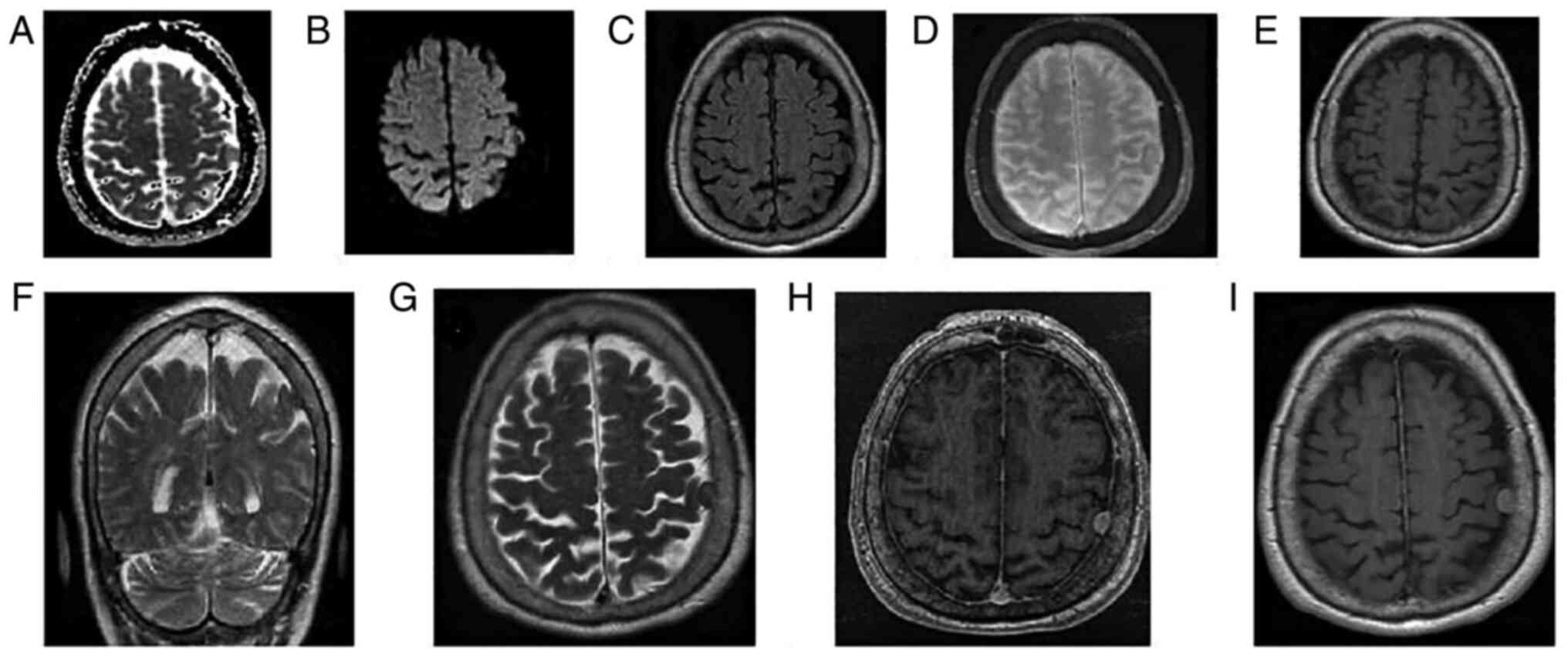
A 67-year old female patient with a known extensive
lesion was admitted to the Animus Kyanos Stavros Hospital, due to a
deterioration of right-sided hemiparesis. The lesion had been
recognized for several years, and the patient had been in a good
clinical condition and had not reported any issues related to it.
However, the findings of the neurological examination did not
reveal any notable findings, apart from mild right hemiparesis. An
MRI revealed a mass lesion wherein the sagittal T1-weighted image
before contrast administration was observed to be iso-intensity to
slight hypo-intensity relative to grey matter (Fig. 4) In sagittal post-contrast
T1-weighted image meningioma demonstrated an avid, homogeneous
enhancement with occasional areas of central necrosis and
calcification that were not enhanced, and with the dural tail sign.
In the coronal post-contrast T1-weighted image, an avid,
homogeneous enhancement was also observed, with occasional areas of
central necrosis and calcification. The T2-weighted image
demonstrated iso-intensity to slight hyperintensity relative to
grey matter and in the axial FLAIR T2, the weighted image in which
the meningioma was relatively hypertense to the brain and
peritumoral brain edema was observed. An axial diffusion-weighted
image and the corresponding apparent diffusion coefficient map
revealed no restriction in diffusion or facilitation in the
tumor.
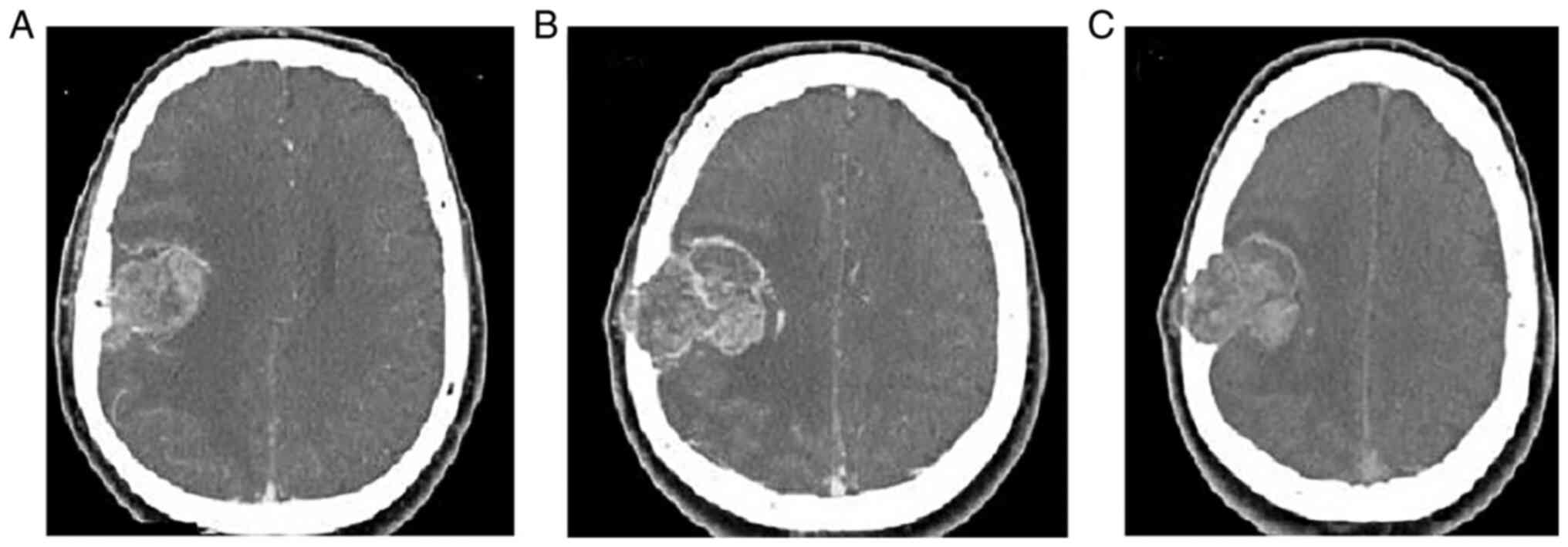
Case 5. A 48-year-old male was admitted to
the Animus Kyanos Stavros Hospital, with a progressive headache
that had been present for 2 months. The axial bone window CT image
revealed the direct tumor infiltration of bone and periosteal
hypervascularity, resulting in benign bone development and a
hyperdensity on a non-contrast CT scan (Fig. 5).
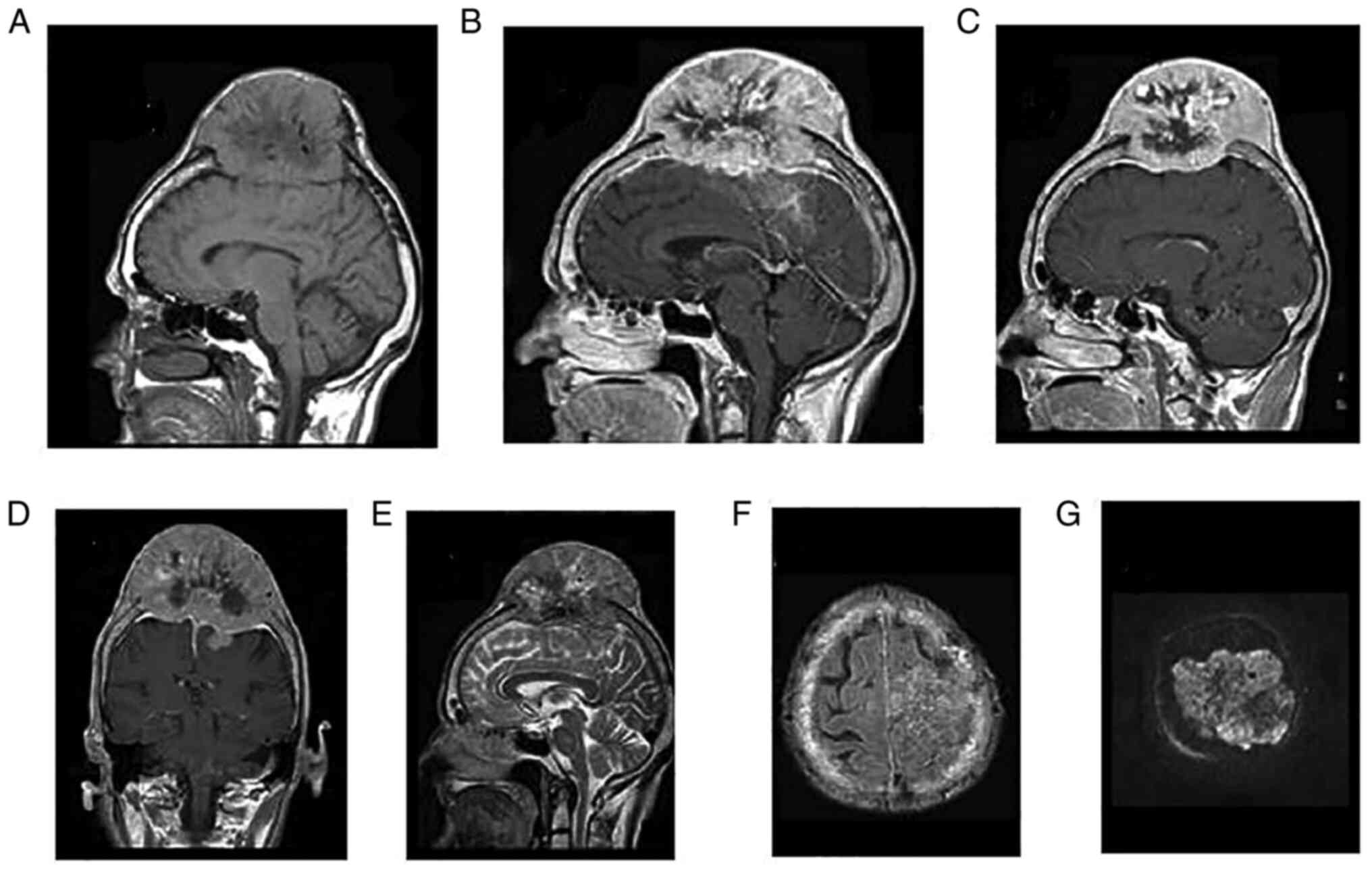
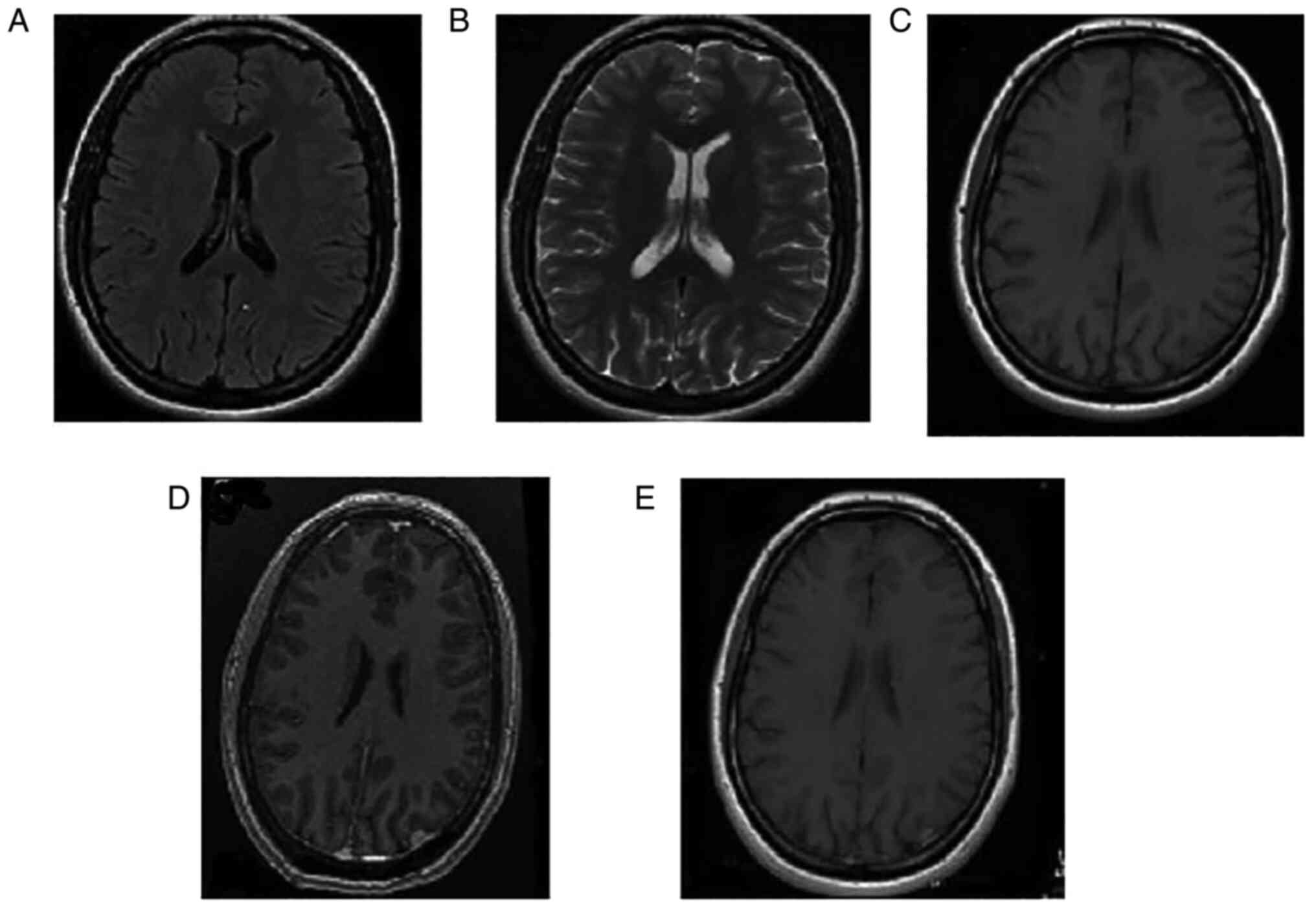
No visible meningiomas. Case 6
A 66-year-old female presented to the Animus Kyanos
Stavros Hospital, complaining of having had a headache for 6
months. She had no prior history of trauma at that location. A
neurological evaluation and laboratory investigations revealed
normal findings. An MRI revealed a small meningioma (Fig. 6), and an axial T1-weighted image (C)
prior to contrast administration in an axial T2-weighted image (A)
and an axial T2 FLAIR-weighted image (B) revealed an enlargement of
the meninga; an axial T1-weighted image post-contrast (E) and FSPGR
post-contrast (D) revealed a small well-circumscribed, extra-axial
tumor on the left cerebral convexity. The mass exhibited
homogeneous hyperintensity in comparison with the gray matter.
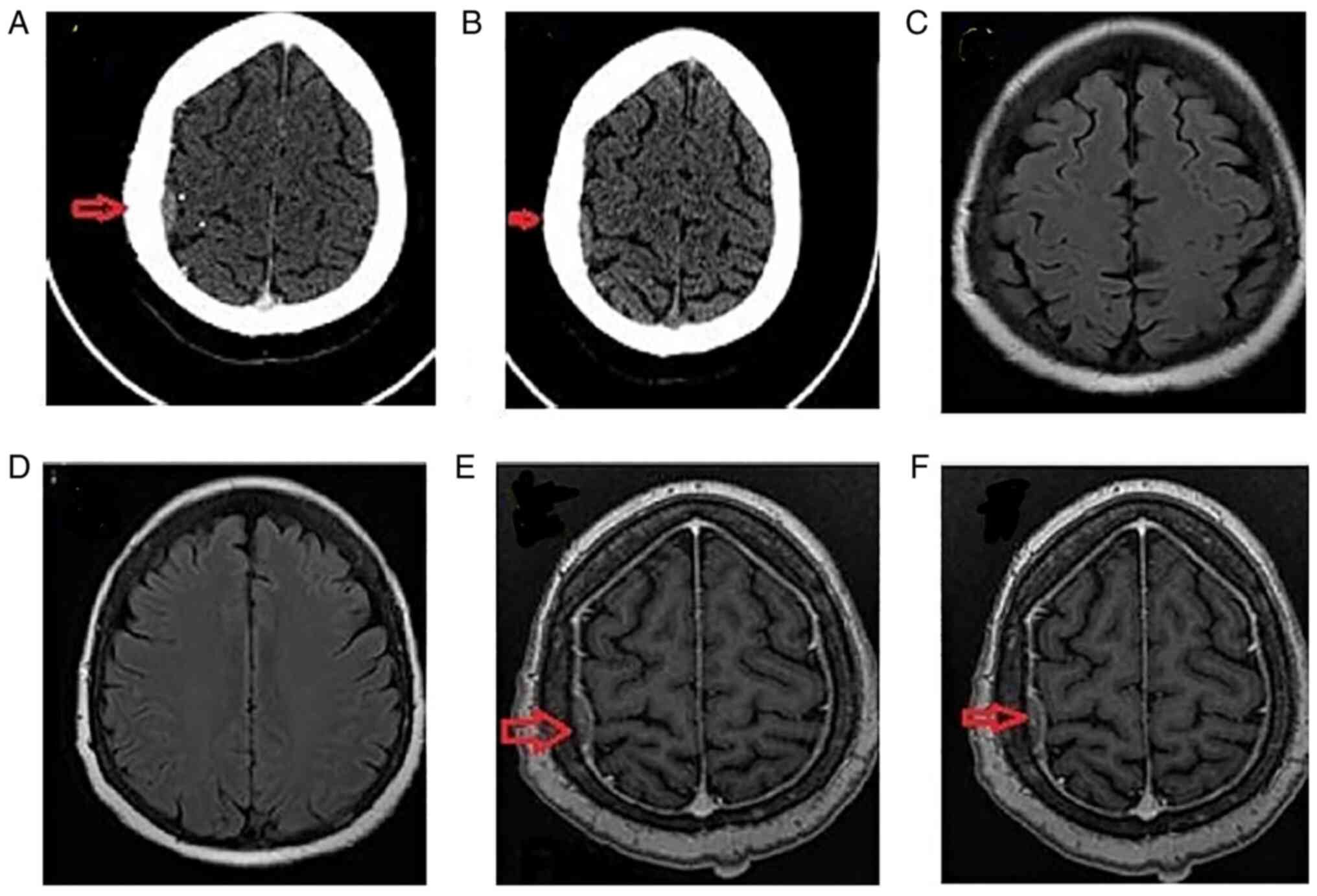
Meningiomas without vascularity. Case
7
A 33-year-old male patient was referred to the
Animus Kyanos Stavros Hospital, by an internal medicine specialist
due to a chronic headache. CT images (Fig. 7) revealed a moderately high-density
tumor with a notable homogeneous enhancement. An MRI (Fig. 7) revealed a poorly defined tumor on
the right cerebral convexity with a mildly hyperintense lesion.
Discussion
Meningiomas are the most frequent type of brain
tumor, accounting for 37.6% of primary brain tumors, with an
adjusted yearly incidence of ~8.3 per 100,000 individuals in the
USA (1,6). Although multiple risk factors have been
identified, the majority of meningiomas develop spontaneously and
are of unknown etiology (7).
According to the World Health Organization (WHO) classification of
the tumors of the CNS, meningiomas can be classified into various
subtypes. Specifically, they are divided into grades I, II and III
according to their histological characteristics (8). Moreover, the majority of meningiomas
are slow-growing benign lesions, although a few exhibit a rapid
growth (9).
Almost 98% of meningiomas are classified as
non-malignant (WHO grades I or II), whereas 2% of these are
classified as malignant. The incidence of meningiomas increases
with age (mainly >65 years of age, more frequently affecting the
African-American population and females more than males (10).
Meningiomas can be detected on any of the exterior
surfaces of the brain and also within the ventricular system, and
they originate from the stromal arachnoid cells of the choroid
plexus (4). They are the second most
common mass lesion of the cerebellopontine angle and can spread
through foramina in the skull base (4). Other locations include the optic nerve
sheath (0.4-1.3% of cases), the choroid plexus (0.5-3% of cases),
the sella turcica, and rarely, outside of the dura with
extracalvarial, calvarial, or both calvarial and extracalvarial
extension, affecting the temporal bone, mediastinum, mandible and
lungs, due to the trapping of the meningocytes or arachnoid cap
cells during head trauma (4).
Meningiomas arise from arachnoid meningothelial
cells. Intracranially, they are extra-axial masses that typically
exhibit iso- to hypointensity on T1-weighted, and iso- to
hyper-intensity on T2-weighted images of the cortex, demonstrating
avid and often homogeneous post-contrast enhancement. Moreover,
there is a strong enhancement that is typically observed following
contrast administration (11).
On diffusion-weighted images as well, meningiomas
can exhibit various intensities; thus, apparent diffusion
coefficient values may differ significantly and may show no
diffusion restraint as compared to the brain tissue (12).
Hyperostosis in the underlying bones, dural tails,
calcification and linear internal flow voids are also frequently
observed in meningiomas. More specifically, the dural tail sign
does not represent a specific finding, as it can also be present in
some metastases, glial tumors and lymphomas, and the latter are not
typically associated with a dural tail to distinguish meningioma
from schwannoma in the cerebellopontine angle (13,14).
Peritumoral brain edema can develop when a
meningioma becomes large (15). The
common MRI signal intensity features comprise an iso-intensity to
modest hypointensity T1-weighted sequence in comparison to grey
matter and iso-intensity to slight hyper-intensity on the T2
sequence. Following contrast administration, meningiomas
traditionally present with avid, homogeneous enhancement with
intermittent areas of central necrosis or calcification. Contrast
can help to identify en plaque meningiomas. Calcification is
typically best demonstrated on a CT scan and an MRI. The dural tail
sign is pathognomonic of meningiomas (16).
Meningiomas may lead to changes in bone, which
include osteolysis and hyperostosis, and are described in 20% of
cases, with the latter being the most common and with the en plaque
form. An enlargement of the skull base foramina can also be present
(13).
Imaging with a CT scan can achieve a good depiction
of the changes in bone associated with meningiomas, which may be
appreciated on an MRI as well. Hyperostosis is the benign bone
development of the direct tumor attachment to the bone and reactive
hyper-vascularity of the periosteum. In 59% of cases, it may be
difficult to discriminate against the hyperostosis of en plaque
from the primary intraosseous meningioma, which is osteoblastic and
may be associated with underlying homogeneous dural enhancement
(17,18). The lack of contrast makes meningioma
less obvious than other lesions on MRI. The majority of tumors may
be identified due to their effects (displacement and edema) on the
adjacent brain. Diagnostic issues arise when the meningiomas are
small and have a minimal mass effect and minimal or no edema. In
these cases, careful attention is required to identify the subtle
anatomic distortion and to proceed to intravenous contrast
administration, which is the key to correct diagnosis (19).
In multiple myeloma (MM), the accumulation of plasma
cells in the CNS or dura is rare. The intracranial manifestation of
MM includes either a diffuse leptomeningeal attachment or, less
often, a single tumor. The involvement of leptomeninges can be
observed as a diffuse enhancement, similar to meningitis, or as
focal masses, mimicking meningiomas (20). Epidural involvement can also be
observed. Several cases of MM with myelomatous meningeal
participation have been described (21,22). The
advanced stage of MM, along with circulating plasma cells,
indicated that malignant cells spread to the meninges through a
hematogenous route. Inappropriately, imaging analyses are often
nonspecific, and the differential diagnosis includes
carcinomatosis, metastasis, plasmacytoma, dural granulocytic
sarcoma and meningitis (23).
In conclusion, the present study provided some
examples of types of meningiomas with wide-range potential
manifestations and imaging variants where the diagnosis is often
challenging. Thus, the reporting radiologist or neurosurgeon needs
to be aware of their alternative presences to differentiate these
tumors from others that can imitate their appearance.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
GF and EL conceptualized the study. VT, GF and EL
advised on patient care and medical treatment, and wrote and
prepared the draft of the manuscript. AAF, PS, NT, PP, KT, VEG, SC,
NM and DAS analyzed the patient data and provided critical
revisions. GF and EL confirm the authenticity of all the data. All
authors contributed to manuscript revision, and have read and
approved the final version of the manuscript.
Ethics approval and consent to
participate
Written informed was obtained from all included
patients.
Patient consent for publication
Written informed was obtained from the patients for
the publication of their data and any accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ostrom QT, Cioffi G, Gittleman H, Patil N,
Waite K, Kruchko C and Barnholtz-Sloan JS: CBTRUS Statistical
Report: Primary brain and other central nervous system tumors
diagnosed in the United States in 2012-2016. Neuro Oncol. 21 (Suppl
5):v1–v100. 2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Buerki RA, Horbinski CM, Kruser T,
Horowitz PM, James CD and Lukas RV: An overview of meningiomas.
Future Oncol. 14:2161–2177. 2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Nur S, Chuang L and Ramaswamy G: Primary
extracranial meningioma of the pelvis: A light microscopic,
immunohistochemical, and ultrastructural study. Gynecol Oncol.
103:745–748. 2006.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Watts J, Box G, Galvin A, Brotchie P,
Trost N and Sutherland T: Magnetic resonance imaging of
meningiomas: A pictorial review. Insights Imaging. 5:113–122.
2014.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Lyndon D, Lansley JA, Evanson J and
Krishnan AS: Dural masses: Meningiomas and their mimics. Insights
Imaging. 10(11)2019.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Fotakopoulos G, Tsianaka E,
Panagiotopoulos V and Fountas K: New developments in management of
meningioma. J Integr Oncol. 4(2)2015.
|
|
7
|
Wiemels J, Wrensch M and Claus EB:
Epidemiology and etiology of meningioma. J Neurooncol. 99:307–314.
2010.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Louis DN, Perry A, Wesseling P, Brat DJ,
Cree IA, Figarella-Branger D, Hawkins C, Ng HK, Pfister SM,
Reifenberger G, et al: The 2021 WHO classification of tumors of the
central nervous system: A summary. Neuro Oncol. 23:1231–1251.
2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Ogasawara C, Philbrick BD and Adamson DC:
Meningioma: A review of epidemiology, pathology, diagnosis,
treatment, and future directions. Biomedicines.
9(319)2021.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Saraf S, McCarthy BJ and Villano JL:
Update on meningiomas. Oncologist. 16:1604–1613. 2011.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Young RJ and Knopp EA: Brain MRI: Tumor
evaluation. J Magn Reson Imaging. 24:709–724. 2006.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Santelli L, Ramondo G, Della Puppa A,
Ermani M, Scienza R, d'Avella D and Manara R: Diffusion-weighted
imaging does not predict histological grading in meningiomas. Acta
Neurochir (Wien). 152:1315–1319; discussion 1319. 2010.PubMed/NCBI View Article : Google Scholar
|
|
13
|
O'Leary S, Adams WM, Parrish RW and
Mukonoweshuro W: Atypical imaging appearances of intracranial
meningiomas. Clin Radiol. 62:10–17. 2007.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Hakyemez B, Yildirim N, Erdoğan C, Kocaeli
H, Korfali E and Parlak M: Meningiomas with conventional MRI
findings resembling intra-axial tumors: Can perfusion-weighted MRI
be helpful in differentiation? Neuroradiology. 48:695–702.
2006.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Toh CH, Siow TY and Castillo M:
Peritumoral brain edema in meningiomas may be related to glymphatic
dysfunction. Front Neurosci. 15(674898)2021.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Whittle IR, Smith C, Navoo P and Collie D:
Meningiomas. Lancet. 363:1535–1543. 2004.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Tokgoz N, Oner YA, Kaymaz M, Ucar M,
Yilmaz G and Tali TE: Primary intraosseous meningioma: CT and MRI
appearance. AJNR Am J Neuroradiol. 26:2053–2056. 2005.PubMed/NCBI
|
|
18
|
Elder JB, Atkinson R, Zee CS and Chen TC:
Primary intraosseous meningioma. Neurosurg Focus.
23(E13)2007.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Smirniotopoulos JG and Jäger HR: Chapter 8
Differential Diagnosis of Intracranial Masses. In: Diseases of the
Brain, Head and Neck, Spine 2020–2023: Diagnostic Imaging
[Internet]. Hodler J, Kubik-Huch RA, von Schulthess GK (eds).
Springer, New York, NY, 2020.
|
|
20
|
Marjanović S, Mijusković Z, Stamatović D,
Madjaru L, Ralić T, Trimcev J, Stojanović J and Radović V II:
Multiple myeloma invasion of the central nervous system. Vojnosanit
Pregl. 69:209–213. 2012.PubMed/NCBI
|
|
21
|
Cerase A, Tarantino A, Gozzetti A, Muccio
CF, Gennari P, Monti L, Di Blasi A and Venturi C: Intracranial
involvement in plasmacytomas and multiple myeloma: A pictorial
essay. Neuroradiology. 50:665–674. 2008.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Petersen SL, Wagner A and Gimsing P:
Cerebral and meningeal multiple myeloma after autologous stem cell
transplantation. A case report and review of the literature. Am J
Hematol. 62:228–233. 1999.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Yi HJ, Hwang HS, Moon SM, Shin IY and Choi
YH: A case of multiple myeloma with brain parenchyme involvement.
Brain Tumor Res Treat. 1:103–106. 2013.PubMed/NCBI View Article : Google Scholar
|