Introduction
Kaposi sarcoma (KS) is an atypical multicentric
tumor that mainly originates in the skin of the lower extremities.
It can occur in four clinical forms, including classic KS, endemic
KS, human-acquired immunodeficiency syndrome-related epidemic KS
(AIDS-related KS) and transplantation-associated KS (1). This tumor commonly consists of
proliferating spindle cells and capillary vessels, presenting as
multiple vascular tumors, and may develop as cutaneous lesions,
invasive lymph nodes, or visceral tumors (2). The human immunodeficiency virus (HIV),
human herpesvirus-8 (HHV-8) and immunosuppressive treatment all
play a role in the development of KS (1,3,4). The more susceptible sex is usually
males in their 70 and 80s (5). The
simultaneous occurrence of several different tumors, such as a
primary tumor with a metastatic tumor or a metastatic tumor with an
inflammatory lesion has been previously reported as the association
of KS with several malignant diseases like lymphomas, leukemias and
multiple myeloma. However, its co-existence with a solid tumor,
such as renal cell carcinoma (RCC), is extremely rare (6,7). Based
on the literature and to the best of our knowledge, there are only
three reports available to date that mention this finding (7-9).
RCC represents a heterogenous group of cancers originating from
renal tubular epithelial cells. Its incidence increases according
to age and the male sex (10). The
present study reports a rare case of synchronous classic KS and
clear cell RCC in a 69-year-old male patient with no chronic
disease or history of surgical intervention.
Case report
Patient information
A 69-year-old man was referred by a dermatologist to
the Hiwa Oncology Hospital (Sulaimani, Iraq) after presenting with
painful, purplish nodular lesions on the dorsal aspect of his hands
and feet for a duration of 2 months (Fig. 1).
Clinical findings
He had no chronic medical illnesses or prior
surgical interventions. He had used various prescribed topical
agents, such as trichloroacetic acid (TCA) solution and topical
steroids without any response.
Diagnostic assessment
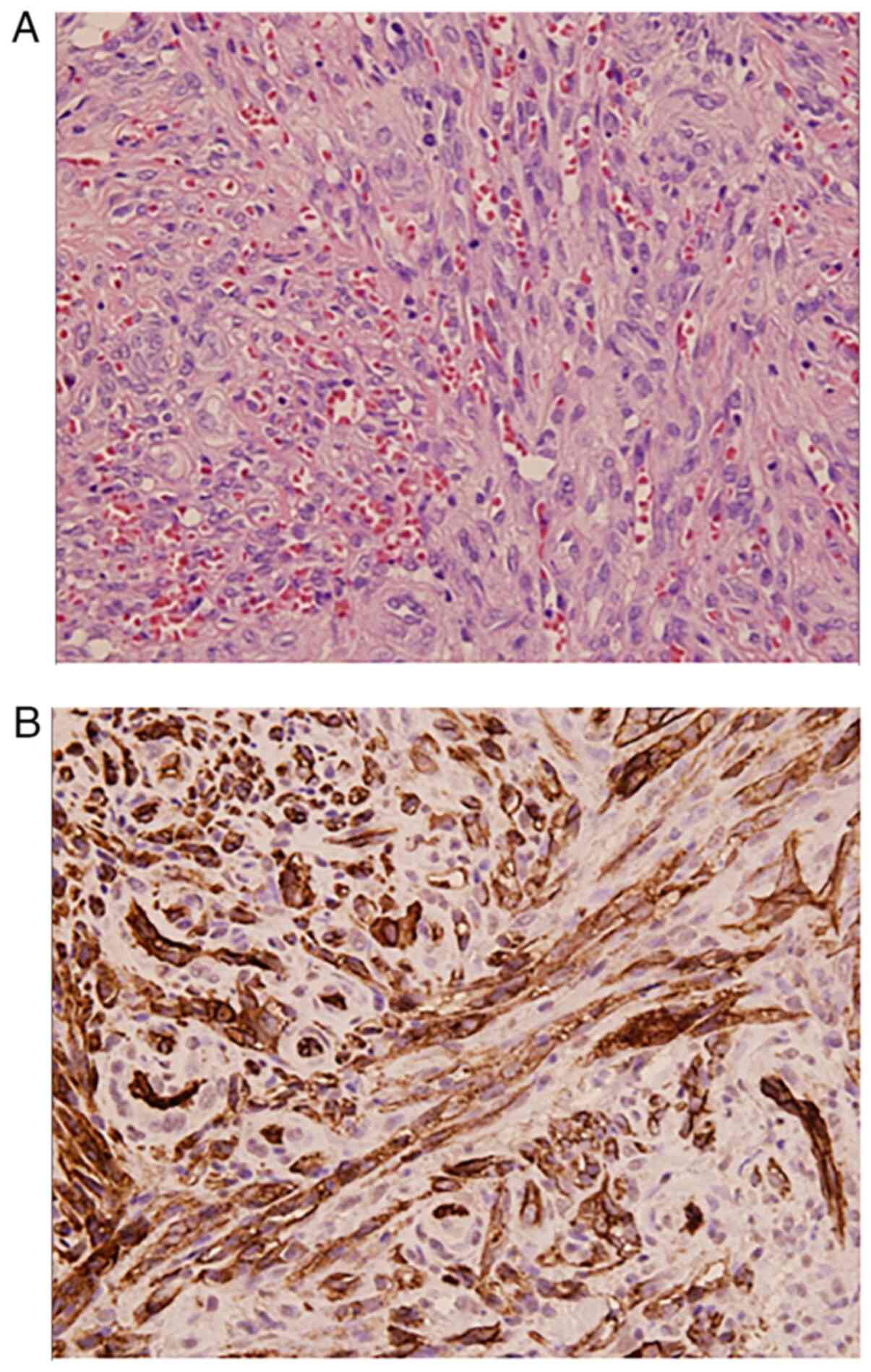
An excisional biopsy of one of the lesions revealed
a nodular dermal lesion with numerous vascular channels and
interlacing spindle cells. Immunohistochemical examinations
(previously conducted by another center) revealed a positive
reaction to CD31 (Fig. 2). He was
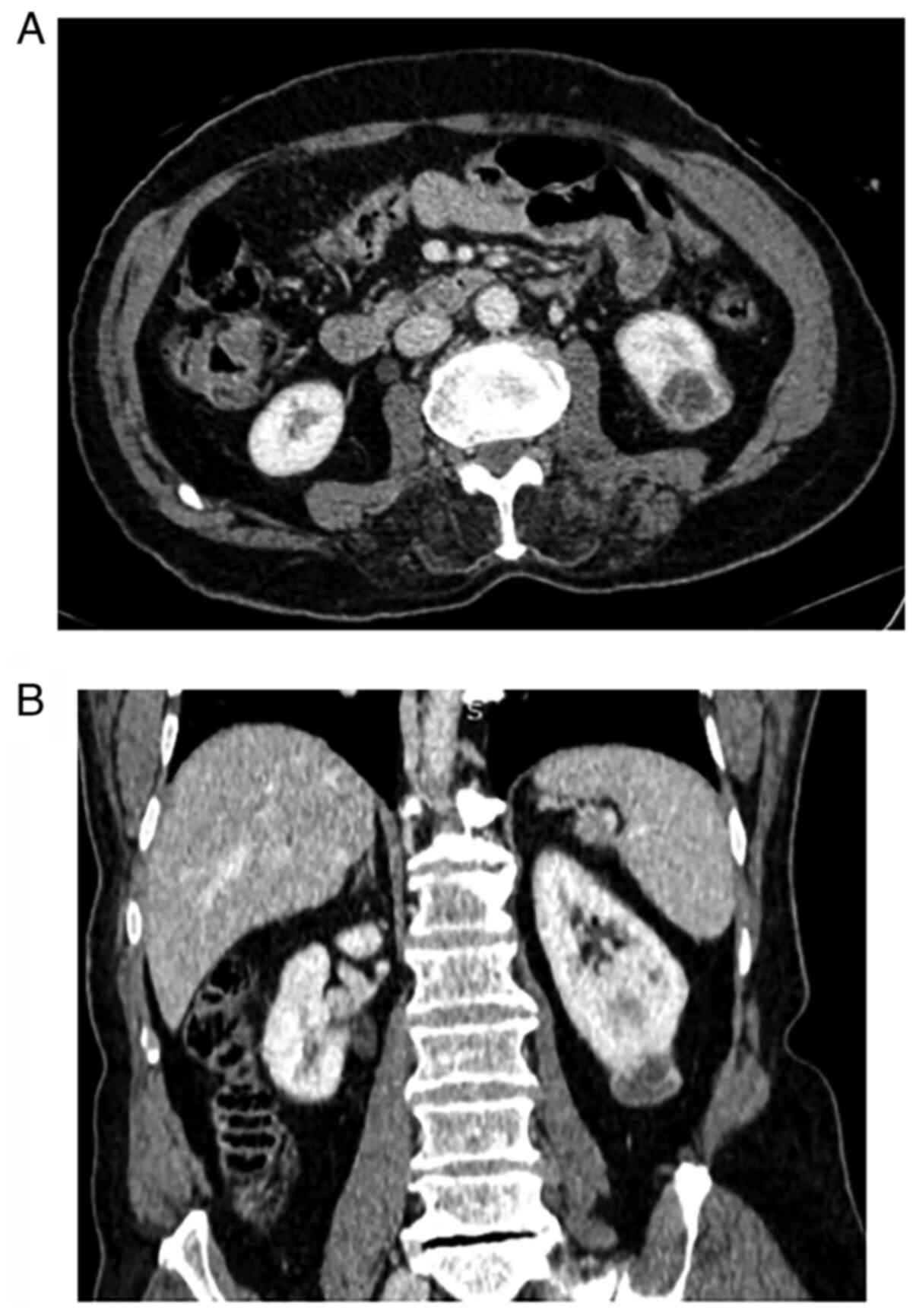
referred to an oncology center. After a metastatic workup, a 2.5 cm
enhancing mass was found in a contrast-enhanced CT of the abdomen,
suggesting RCC or metastasis (Fig.
3).
Therapeutic intervention
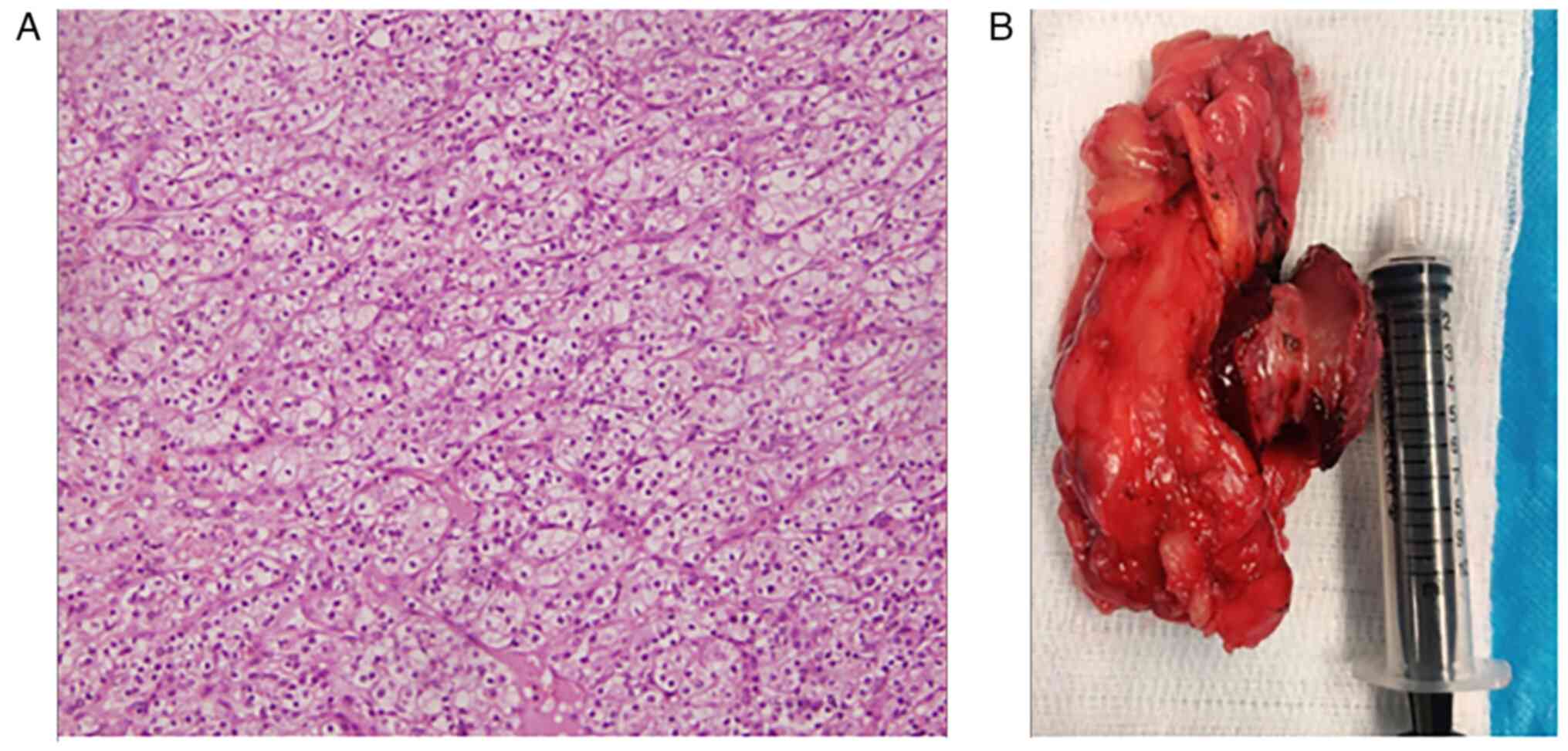
A partial nephrectomy was performed, and the
histopathological examinations (previously conducted by another
center) were in line with clear cell RCC with a pathological stage
of pT1a (Fig. 4). The patient then
received six cycles of paclitaxel (100 mg/m2)
intravenously every 14 days, along with topical imiquimod (5%)
three times weekly. He responded to the treatment, and the skin
lesions disappeared (Fig. 5).
Follow-up
The post-operative period was uneventful. After 1
year, his follow-up imaging revealed no recurrent renal mass.
Discussion
The dermatologist, Moritz Kaposi, was the first to
report several cases of KS in elderly males and described it as a
multifocal pigmented sarcoma of the skin (11). KS is a rare neoplasm that develops
from endothelial cells and is classified into four epidemiological
forms: Classic KS, endemic KS, AIDS-related KS and
transplantation-associated KS (1).
Classic KS most commonly occurs in elderly male patients of Arabic,
Southern European, and Jewish ancestry. Individuals who were born
in countries where classic KS is prevalent are therefore at a
higher risk of developing KS (4). In
some African countries, KS has been known for decades prior to the
emergence of HIV (12). This form is
known as endemic, and it is much more aggressive than the classic
form. AIDS-related KS commonly occurs in HIV-affected homosexual
males (12).
It has been revealed that a significant association
exists between immunosuppression and KS (1). Another study reported that the
incidence of KS was 200-fold higher in recipients of organ
transplants in comparison to the general population (11). The exact etiology of KS has yet to be
understood; however, infection with HHV-8 is strongly related to
the neoplasm, and it has been reported in >95% of KS cases of
all epidemiological forms (13). It
can affect the coding of the factors and cytokines that regulate
cellular proliferation, immune responses and apoptosis, inducing
the transformation of endothelial cells (1). It is worth mentioning that in the
present case report, the patient was free from any chronic or
acquired disease, and his past surgical and medical treatment was
also negative. For this reason, the three forms of endemic KS,
AIDS-related KS and transplantation-associated KS were excluded.
The patient described herein was an elderly male and compatible
with the criteria of classic KS, in which the majority of the
classic KS cases are elderly males.
Classic KS usually appears as painless, bluish-red
demarcated lesions on the distal parts of the lower extremities,
and histologically the lesions are often similar to granulated
tissue. In the majority of cases, the lesions grow gradually and
merge to form large plaques. On some occasions, solitary lesions
can form nodular and brownish-red tumors (14). The KS in the present study manifested
as painful, purplish nodular lesions on the dorsal aspects of the
hands and feet.
In the literature, the association of KS with
various diseases and cancers has been discussed (4,7,15). Multicentric Castleman disease (MCD)
refers to a lymphoproliferative disorder that is associated with
secondary B-cell lymphoma development. It has recently been
revealed that a subclass of this disorder is linked to
KS-associated herpesvirus (KSHV), in which KSHV infection can be
found in almost all HIV-associated cases of MCD and 50% of
HIV-negative patients (4). Several
scholars have mentioned the concurrence of KS and psoriasis, which
presents a diagnostic challenge due to the resemblance between the
lesions of both conditions (15,16).
Furthermore, another epidemiological study revealed a high risk of
KS in patients with psoriasis (17).
Magri et al (13) also
reported a rare case of KS following severe acute respiratory
syndrome coronavirus 2 (SARS-CoV-2) infection in an 83-year-old
female patient. They considered that various cofactors may have
been involved in the development of KS, including steroid
administration, older age, and infection with SARS-CoV-2(13). Synchronous tumors in the same
individual are regarded as a subject of interest with the hope of
shedding light on the factors that are involved in promoting the
neoplastic process or identifying criteria that place an individual
at risk of developing various malignancies. The biological
mechanisms behind the association of KS with different malignancies
have not yet been well-established, although some individuals may
be susceptible to some common initiators of malignant alterations
(18). An association of KS with
multiple types of cancer, such as leukemia, multiple myeloma,
thymoma, non-Hodgkin's lymphoma, Hodgkin's lymphoma and malignant
melanoma has been reported (14).
Iscovic et al (19) conducted
a study on 1,000 Jewish patients with classic KS and found that 61
cases were affected by a second neoplasm, and increasing risks of
non-Hodgkin's lymphoma and cutaneous malignant melanoma were
detected. The simultaneous appearance of KS and RCC is a very
infrequent condition (7). To the
best of our knowledge, only three such cases have been published to
date. The first one was reported by Giatrakou et al
(7), in which the case was affected
by classic KS and two coexistent kidney tumors: Clear cell RCC and
chromophobe RCC. The case was recovered from the KS after the
removal of the kidney tumors (7).
The second case was synchronous KS and RCC in a non-infected HIV
homosexual male who was managed by tumor resection (8). In addition, another case of synchronous
AIDS-related KS with renal cell adenocarcinoma in a 42-year-old
homosexual male was reported (9).
The present case is the first report of synchronous classic KS and
clear cell RCC, followed by the case of Giatrakou et al
(7).
Both KS and RCC are vascular tumors, and their
pathogenesis is commonly affected by an angiogenic factor known as
vascular endothelial growth factor (VEGF). A complete response of
KS was observed after sorafenib, an inhibitor of VEGF receptors,
was administered for the treatment of metastatic renal cancer
(7,20). This reinforces that there is a common
therapeutic and pathogenetic pathway between these two neoplasms,
and VEGF plays a significant role in their oncogenesis (7). KS can be easily suspected depending on
the clinical manifestations; however, a clinical diagnosis alone is
not sufficient. A histopathological diagnosis remains the standard
method for the confirmation of KS, although this needs to be
performed by an experienced pathologist (21). The treatment strategy for KS commonly
depends on several factors, including skin lesion number, disease
extension, symptoms, comorbidities, and the rate of tumor growth.
Thus, the management of KS can be ranged from local therapy for
cutaneous disease to systemic therapy in cases with visceral and
symptomatic lesions. For the treatment of localized skin lesions, a
number of options like ionizing radiation, cryotherapy,
photodynamic therapy and surgical excision have been frequently
used. However, in aggressive cases involving the skin, lymph nodes,
and visceral organs, chemotherapy is a necessary option (22). Cytotoxic chemotherapy has been
reported as the treatment of choice for KS. DNA-damaging agents,
such as doxorubicin and paclitaxel are in the first line of
treatment (21). In the case
described herein, after conducting a partial nephrectomy, the case
was administered six cycles of paclitaxel every 2 weeks with
topical imiquimod (5%) three times weekly, and the patient
completely responded to the treatment.
In conclusion, synchronous KS with clear-cell RCC is
a rare finding. Clear-cell RCC can be found incidentally during the
workup of the KS. Their simultaneous appearance may be triggered by
the common enhancing angiogenic factor, VEGF.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
RB was a major contributor to the conception of the
study, and the surgeon who managed the case. HOA and FHK were
involved in the design of the study, literature search and review
of studies for the inclusion of related studies, and in the
drafting of the manuscript. BS was the oncologist who performed the
oncological analysis. BAA, IA, RSA and RKA were involved in the
literature review, in the design of the study, the critical
revision of the manuscript, and the processing of the figures. RB
and BS confirm the authenticity of all the raw data. RJR and SHT
were the radiologists who performed the assessment of the subjects'
Kaposi sarcoma and renal cell carcinoma. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from the
patient.
Patient consent for publication
Written informed consent was taken from the patient
for the publication of any related information and images or
illustrations.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Agbaht K, Pepedil F, Kirkpantur A, Yilmaz
R, Arici M and Turgan C: A case of Kaposi's sarcoma following
treatment of membranoproliferative glomerulonephritis and a review
of the literature. Ren Fail. 29:107–110. 2007.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Mitsuyasu RT, Colman MF and Sun NC:
Simultaneous occurrence of Hodgkin's disease and Kaposi's sarcoma
in a patient with the acquired immune deficiency syndrome. Am J
Med. 80:954–958. 1986.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Cheung MC, Pantanowitz L and Dezube BJ:
AIDS-related malignancies: Emerging challenges in the era of highly
active antiretroviral therapy. Oncologist. 10:412–426.
2005.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Boshoff C and Weiss RA: Epidemiology and
pathogenesis of Kaposi's sarcoma-associated herpesvirus. Philos
Trans R Soc Lond B Biol Sci. 356:517–534. 2001.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Moore A, Peretz I, Yosef L, Goldstein DA,
Goldvaser H, Horn S, Edel Y and Zer A: Potential association
between Kaposi sarcoma and gout: An exploratory observational
study. Sarcoma. 2020(8844970)2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Paksoy N: Simultaneous occurrence of
Kaposi sarcoma and tuberculosis; Kaposi sarcoma and lymphoma in the
same lymph node: A report on two HIV-positive patients from
Zimbabwe. Rev Soc Bras Med Trop. 52(e20180188)2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Giatrakou S, Leodara V, Siatelis A,
Papadavid E, Theodoropoulos K, Safioleas K, Stamatakos M and
Stavrianeas NG: P91 clearance of non AIDS-Kaposi sarcoma after
removal of coexistent clear cell renal cell and chromophobe renal
cell carcinomas. Melanoma Res. 20:e81–e82. 2010.
|
|
8
|
Meuthen I, Vossbeck H, Marx FJ, Hummerich
W and Saborowski F: Kaposi's sarcoma and renal cell carcinoma in a
male homosexual without detectable HIV infection-case report and
review of the literature. Onkologie. 18:151–154. 1995.
|
|
9
|
Azón-Masoliver A, Moreno A, Gatell JM and
Mascaró JM: Renal cell adenocarcinoma associated with AIDS-related
Kaposi's sarcoma. AIDS. 4:818–819. 1990.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Hsieh JJ, Purdue MP, Signoretti S, Swanton
C, Albiges L, Schmidinger M, Heng DY, Larkin J and Ficarra V: Renal
cell carcinoma. Nat Rev Dis Primers. 3(17009)2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Cesarman E, Damania B, Krown SE, Martin J,
Bower M and Whitby D: Kaposi sarcoma. Nat Rev Dis Primers.
5(9)2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Beral V, Peterman TA, Berkelman RL and
Jaffe HW: Kaposi's sarcoma among persons with AIDS: A sexually
transmitted infection? Lancet. 335:123–128. 1990.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Magri F, Giordano S, Latini A and
Muscianese M: New-onset cutaneous Kaposi's sarcoma following
SARS-CoV-2 infection. J Cosmet Dermatol. 20:3747–3750.
2021.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Iscovich J, Boffetta P, Franceschi S,
Azizi E and Sarid R: Classic Kaposi sarcoma: Epidemiology and risk
factors. Cancer. 88:500–517. 2000.PubMed/NCBI
|
|
15
|
Brambilla L, Genovese G, Tourlaki A and
Della Bella S: Coexistence of Kaposi's sarcoma and psoriasis: Is
there a hidden relationship? Eur J Dermatol. 28:320–325.
2018.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Yoo J, Jo M, Kim MS, Choi KH, Park HJ and
Jue MS: Hidden pictures of Kaposi's sarcoma in psoriatic lesions: A
diagnostic challenge. Ann Dermatol. 28:749–752. 2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Hemminki K, Liu X, Ji J, Sundquist J and
Sundquist K: Kaposi sarcoma and Merkel cell carcinoma after
autoimmune disease. Int J Cancer. 131:E326–E328. 2012.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Safai B, Miké V, Giraldo G, Beth E and
Good RA: Association of Kaposi's sarcoma with second primary
malignancies: Possible etiopathogenic implications. Cancer.
45:1472–1479. 1980.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Iscovich J, Boffetta P and Brennan P:
Classic Kaposi's sarcoma as a first primary neoplasm. Int J Cancer.
80:173–177. 1999.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Ardavanis A, Doufexis D, Kountourakis P
and Rigatos G: A Kaposi's sarcoma complete clinical response after
sorafenib administration. Ann Oncol. 19:1658–1659. 2008.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Schneider JW and Dittmer DP: Diagnosis and
treatment of Kaposi sarcoma. Am J Clin Dermatol. 18:529–539.
2017.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Passarelli A, Galdo G, Pellegrino T,
Roviello G, Aieta M, Aviello G and Conca R: Therapeutic management
of a symptomatic Kaposi's sarcoma patient with renal failure
undergoing haemodialysis: A case report. Dermatol Reports.
14(9113)2021.PubMed/NCBI View Article : Google Scholar
|