Introduction
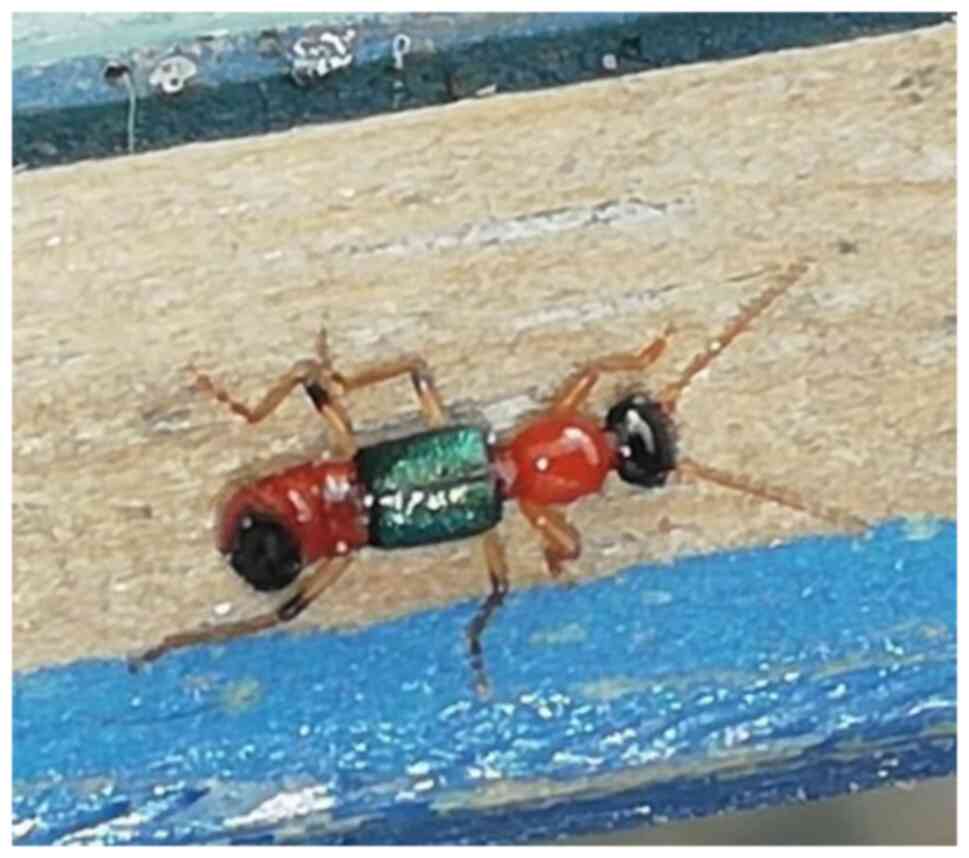
The genus Paederus belongs to the order
Coleoptera, the family Polyphaga and the sub-families
Staphylinoidea, Staphylinidae and Paedrinae (Fig. 1) (1).
They predominantly inhabit tropical zones, and frequently appear in
seasons of rain and high humidity (2). At least 600 species of Paederus
have been described worldwide, of which 20-30 have been associated
with Paederus dermatitis (2,3). A database termed EncicloVida, developed
by the National Commission for the Knowledge and Use of
Biodiversity (CONABIO), indicates that Mexico has 20 species of the
genus Paederus: Paederus antiquus,
cantoniensis, cordovensis, currax,
curticeps, erythroderus, femoralis,
filicornis, grandis, laetipes, laetus,
mexicanus, neotropicus, rufitarsis,
salvini, signaticornis, tempestivus,
testaceitarsis, ustus, yucateca (https://enciclovida.mx/especies/76243-paederus;
accessed March 27, 2023). The laetus and
signaticornis species have previously been found to produce
skin lesions in humans (1). It is
not known whether the other species that inhabit Mexico can cause
dermatitis. They have the ability to produce a substance known as
Pederin, a toxic substance present in the insect's hemolymph, which
is more potent than cobra venom (4).
Pederin (C25 H45 O9 N) is an amide
with two tetrahydropyran rings (5).
When Pederin comes in contact with the skin of an individual, it
can block cellular mitosis by inhibiting protein and DNA synthesis,
causing a type of irritant contact dermatitis (5). Contact with this insect can lead to
several clinical manifestations that range from mild erythema to
ulcerative lesions with associated infections. This injury is not
caused by a bite or sting, but rather by the accidental brushing or
crushing of the insect over an exposed area of the human body
(4,5). If not adequately treated, these
manifestations can spread and create complicated cases of
cellulitis and systemic affectation (4). Pederin has been identified to be
produced by Gram-negative endosymbiotic bacteria of the
Pseudomonas genus, which are in part responsible for the
associated infections (6,7).
In general, the management of these patients is
based on the administration of topical steroids, oral antimicrobial
cycles and antihistamines (8,9). To
date, to the best of our knowledge, there are no large randomized
controlled trials available to guide the therapy for Paederus
dermatitis. There is a preclinical trial with guinea pigs, where
linear dermatitis (or dermatitis linearis) induced by
Paederus was managed with fluocinolone, or potassium
permanganate with calamine, the latter being more effective
(10). Despite the preclinical
precedent of the efficacy of potassium permanganate for this type
of dermatitis, there are no reports yet available that demonstrate
its use in humans with this condition, at least to the best of our
knowledge.
The present study describes the case of an
individual affected by contact with the Paederus sp. insect,
where potassium permanganate (Vikút antiseptic
solution®, Grupo Salypro de Mexico S.A. de C.V.) was
used as part of the treatment.
Case report
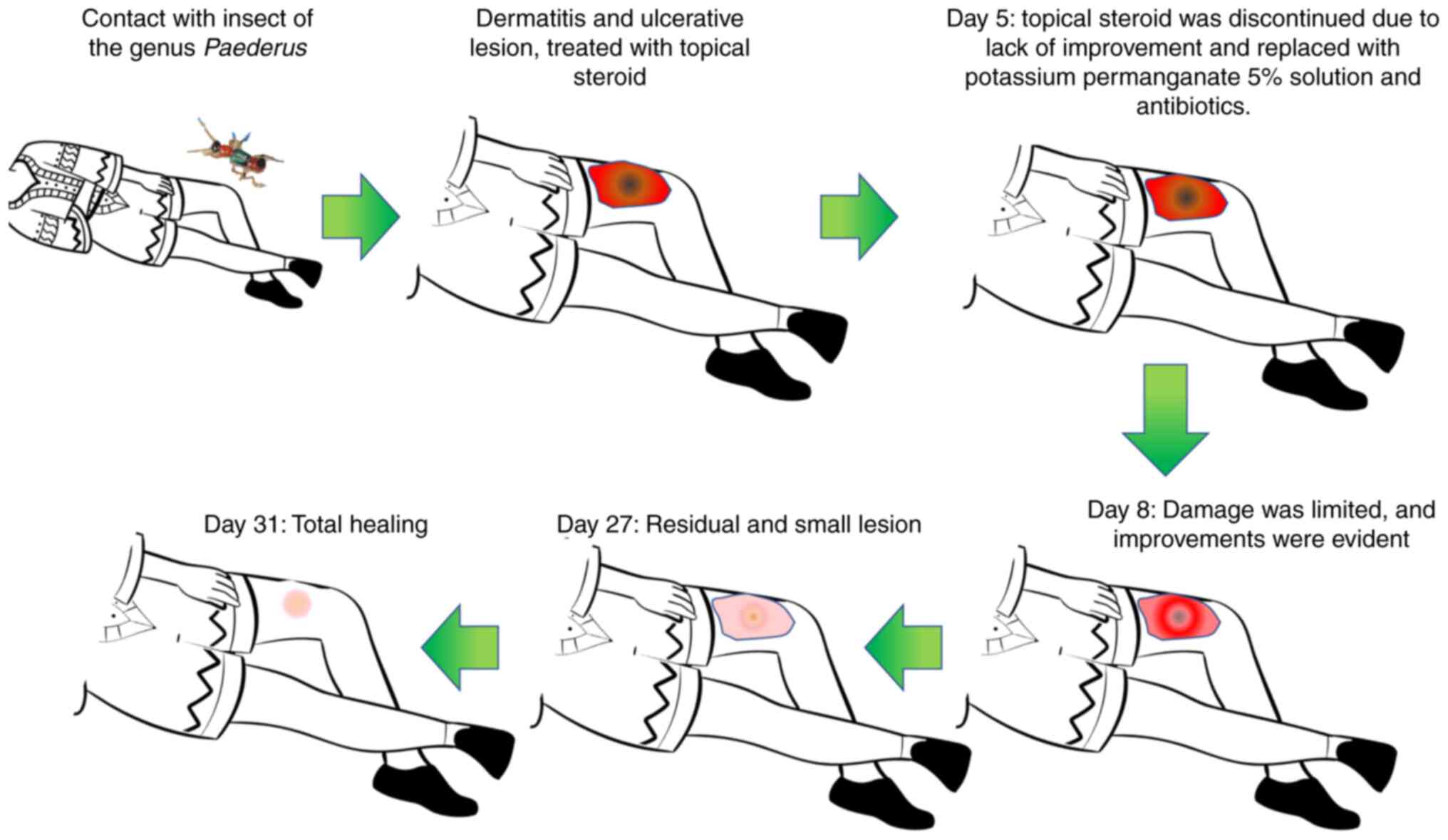
The present study describes the case of a
59-year-old male, with no history of diabetes or hypertension, with
the important precedent of vitiligo and known allergy to pollen.
The patient had come into contact with the insect popularly known
as ‘Panchos or Cuereres’ (Paederus sp.) on his right thigh,
while he was sleeping, in the city of Colima, Mexico, located in
the western part of the Mexican Republic. Initially, the patient
presented itching, heat sensation and local erythema in the place
of contact. Within hours, this evolved into a papular lesion which
grew to 2 cm in diameter. At 24 h after contact with the insect,
the lesion evolved into a blister, and the patient requested care
at a private medical center (‘CEDA Centro de Educación en Diabetes
y Autocontrol’, Colima, Colima, Mexico). Therapy was initiated with
a topical steroid (fluocinolone acetonide) cream, twice a day. At
72 h of evolution, perilesional blisters were formed, and the
initial diameter of the erythematous area expanded to ~7 cm. On the
4th day post-contact, the lesion became ulcerative at the center
and dermic necrosis was observed. It progressively grew in
diameter, and a perilesional dermatitis began to spread on the
medial and lateral side of the patient's thigh. Topical steroid
treatment was suspended on the 5th day, and management based on two
daily applications of potassium permanganate for 4 weeks was
initiated, with two weekly doses of benzathine penicillin of
1,2000,000 UI (intramuscular administration), with 400 mg ibuprofen
every 8 h in the case that the patient felt pain. The 5% potassium
permanganate solution used was a commercial presentation for
topical application (Vikút antiseptic solution®, Grupo
Salypro de Mexico S.A. de C.V.), which also contains the following
ingredients: Salicylic acid, benzoic acid, ethanol and distilled
water.
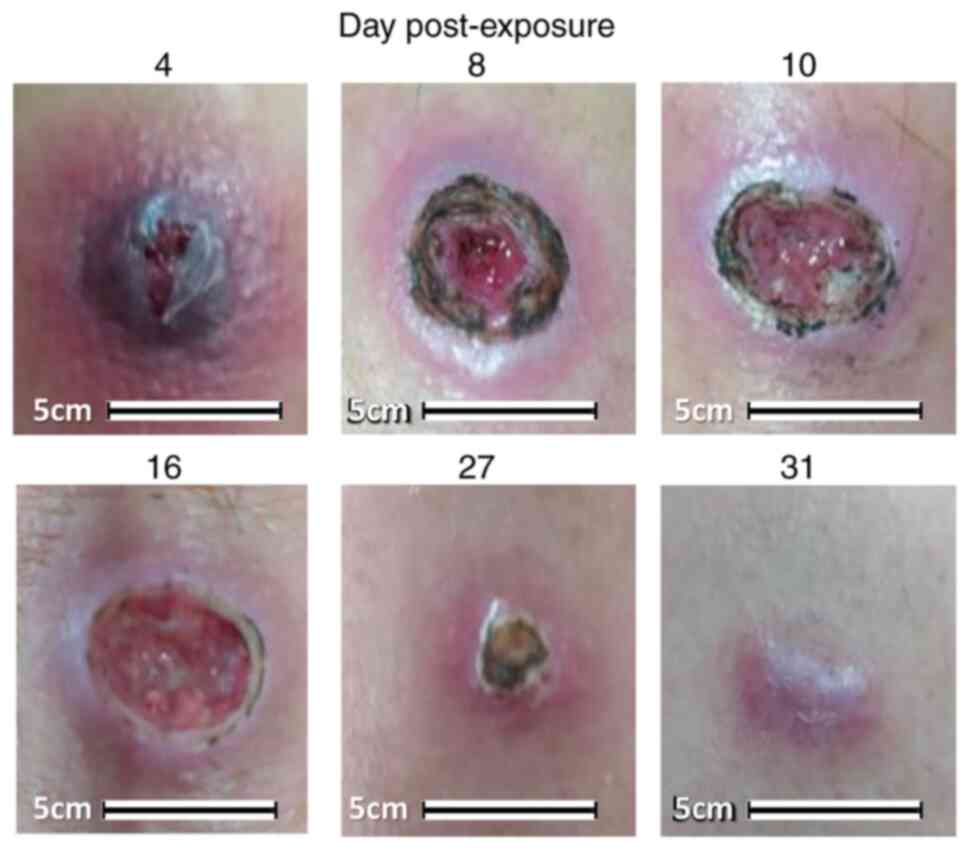
At 72 h following the initiation of treatment with
potassium permanganate, the patient had a follow-up consultation,
and he exhibited an attenuation of the damage to his skin and a
marked improvement in the lesions. After 4 weeks, the healing
process was completed, with only a hypopigmented blot remaining at
the point of contact (Figs. 2 and
3).
Discussion
Outbreaks of Paederus dermatitis have been reported
in Australia, Malaysia, Sri Lanka, Nigeria, Kenya, Iran, Central
Africa, Uganda, Okinawa, Sierra Leone, Argentina, Brazil, Peru,
Venezuela, Ecuador and India. In Mexico, there are two confirmed
species that can cause this type of dermatitis and although they
are widely distributed in the country, Paederus dermatitis in
Mexico is rarely identified; therefore, reports of this type are
limited (3). Several treatments are
available for Paederus dermatitis, including topical steroids,
cycles of oral antimicrobials and antihistamines (8,9).
However, research on the therapy of this type of dermatitis is
limited; thus, further research is required in this matter in order
to provide other treatment options.
Potassium permanganate is obtained by the
electrolytic oxidation of manganese (11). In the medical field, it is used as a
potent oxidant that affects the cellular wall of pathogens, thus
providing its functions as a substance of mineral origin with broad
antimicrobial activity (12,13). It is a bactericide and fungicide, and
it can also affect viruses. Furthermore, it favors the formation of
collagen and granulation tissue, both critical components in the
process of wound healing (12).
The use of potassium permanganate has been described
over the past decades for the management of various types of wounds
(12,14). In the case presented herein, its
effectiveness in the management of dermatitis linearis was
observed, secondary to contact with an insect of the
Paederus genus, which is a relatively common ailment, and it
is even endemic in several countries worldwide (15). Information about the management of
this type of dermatitis is limited, apart from what is related to
the use of topical steroids, oral anti-inflammatories, antibiotics
and antihistamines (4). Potassium
permanganate has been previously shown as capable of accelerating
the healing process of ulcers of diverse characteristics, such as
those in the diabetic foot (12). In
the unique clinical case presented herein, potassium permanganate
and antibiotics were used simultaneously; thus, it is not possible
to determine whether a monotherapy would have produced a similar
result. For this reason, further preclinical and clinical trials
are required in the future.
In conclusion, potassium permanganate solutions
(such as Vikút®), in conjunction with antibiotics and
anti-inflammatories, may be of great benefit for the treatment of
dermatitis or ulcerative lesions caused by insects of the
Paederus genus. However, further research is required to
determine the detailed effects.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed in the current
study are available from the corresponding author upon reasonable
request.
Authors' contributions
IDE, ALE, IPRS and JGE designed the study and wrote
the manuscript. YSMG, ADLB, MLMF, KILA and MAMH visited the patient
and were in charge of clinical follow-up. IDE and YSMG confirm the
authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
The present study (registered 2020-04-07) was
approved by the Ethics Committee of the School of Medicine of the
Universidad de Colima, Mexico, and written informed consent was
obtained from the participant. All procedures performed in the
present protocol were in accordance with the Declaration of
Helsinki.
Patient consent for publication
The patient provided his written informed consent
for the publication of his clinical case, keeping his identifying
information hidden.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Qadir SNR, Raza N and Rahman SB:
Paederus dermatitis in Sierra Leone. Dermatol Online J.
12(9)2006.PubMed/NCBI
|
|
2
|
Krinsky WL: Chapter 9-beetles
(Coleoptera). In: Medical and Veterinary Entomology. Mullen
GR and Durden LA (eds). 3rd edition. Academic Press, pp129-143,
2019.
|
|
3
|
Macias-Alonso B and Rodríguez-Castellanos
MA: Contact dermatitis due to Paederus. Dermatol Rev Mex.
63:402–406. 2019.
|
|
4
|
Ghoneim KS: Human dermatosis caused by
vesicating beetle products (Insecta), cantharidin and paederin: An
overview. World J Med Med Sci. 1:1–26. 2013.
|
|
5
|
Nasir S, Akram W, Khan RR, Arshad M and
Nasir I: Paederus beetles: The agent of human dermatitis. J
Venom Anim Toxins Incl Trop Dis. 21(5)2015.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Kellner RLL: Molecular identification of
an endosymbiotic bacterium associated with pederin biosynthesis in
Paederus sabaeus (Coleoptera: Staphylinidae). Insect
Biochem Mol Biol. 32:389–395. 2002.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Chamankar B, Maleki-Ravasan N, Karami M,
Forouzan E, Karimian F, Naeimi S and Choobdar N: The structure and
diversity of microbial communities in Paederus fuscipes
(Coleoptera: Staphylinidae): From ecological paradigm to
pathobiome. Microbiome. 11(11)2023.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Pagotto B, Plafnik R, Castillo A, Cionci
J, Abad ME, Cabanilas MS and Larralde M: Contact Paederus
dermatitis in a 12 years old boy. Arch Argent Pediatr. 111:e66–e68.
2013.PubMed/NCBI View Article : Google Scholar : (In Spanish).
|
|
9
|
Pierce JW, Rittman B and Raybould JE: Case
report: Paederus dermatitis in the returning traveler. Am J
Trop Med Hyg. 98:1523–1525. 2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Fakoorziba MR, Eghbal F, Azizi K and
Moemenbellah-Fard MD: Treatment outcome of Paederus
dermatitis due to rove beetles (Coleoptera: Staphylinidae) on
guinea pigs. Trop Biomed. 28:418–424. 2011.PubMed/NCBI
|
|
11
|
McBeath ST, Wilkinson DP and Graham NJD:
Advanced electrochemical oxidation for the simultaneous removal of
manganese and generation of permanganate oxidant. Environ Sci Water
Res Technol. 6:2405–2415. 2020.
|
|
12
|
Delgado-Enciso I, Madrigal-Perez VM,
Lara-Esqueda A, Diaz-Sanchez MG, Guzman-Esquivel J, Rosas-Vizcaino
LE, Virgen-Jimenez OO, Kleiman-Trujillo J, Lagarda-Canales MR,
Ceja-Espiritu G, et al: Topical 5% potassium permanganate solution
accelerates the healing process in chronic diabetic foot ulcers.
Biomed Rep. 8:156–159. 2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Anderson I: Should potassium permanganate
be used in wound care? Nurs Times. 99(61)2003.PubMed/NCBI
|
|
14
|
Hill E and Thomas J: Potassium
permanganate ulcers of the vagina. Obstet Gynecol. 18:747–752.
1961.PubMed/NCBI
|
|
15
|
Neamin G, Negga A, Mukemil H, Mengistu B
and Rahel Y: Paederus dermatitis outbreak in addis ababa,
ethiopia: A case-control study. J Environ Public Health.
2021(8892785)2021.PubMed/NCBI View Article : Google Scholar
|