Introduction
Approximately 1% of all adult cancers are soft
tissue sarcomas, which are uncommon mesenchymal neoplasms. Synovial
sarcoma is a mesenchymal spindle cell tumor that exhibits variable
epithelial differentiation (1).
Synovial sarcoma typically affects young and middle-aged
individuals, and it has a predilection for the extremities
(2).
Primary pancreatic sarcomas are extremely rare and
typically represent <0.1% of all primary pancreatic malignancies
(3). The patient's age, tumor size,
the number of mitoses, type of translocation and tumor-free
resection margins are among the predictors of prognosis. The
preferred course of treatment is total resection with wide margins,
followed by adjuvant chemotherapy and/or radiotherapy. The overall
survival rate at 5 years is between 36 and 76%, and at 10 years it
is between 20 and 63% (4).
The present study describes a rare case of a primary
spindle cell tumor that developed in the pancreatic head. For the
literature review, a Google Scholar and PubMed literature search
was conducted using the combinations of the following key words
‘synovial sarcoma; spindle cell tumor; pancreatic metastasis;
primary pancreatic tumor’. For the literature review, nine articles
that were associated with the present study were selected from 40
available articles. Table I
summarizes the pathological characteristics and mode of treatment
for the pancreatic primary mesenchymal tumors in the reviewed
cases.
 | Table IPathological characteristics and
management of pancreatic primary mesenchymal tumors in the reviewed
studies. |
Table I
Pathological characteristics and
management of pancreatic primary mesenchymal tumors in the reviewed
studies.
| Author, year | Pancreatic tumor
site | Diagnosis | Treatment | (Refs.) |
|---|
| Makino et al,
2016 | Body | Pancreatic metastasis
from synovial sarcoma | Distal
pancreatectomy | (1) |
| Nagaraju et
al, 2017 | Head | High-grade spindle
cell sarcoma | Laparotomy with
allograft/ pancreatectomy | (3) |
| Luc et al,
2013 | Body | Monophasic Grade II
synovial sarcoma of the pancreas | Distal pancreatectomy
with splenectomy | (4) |
| Malek et al,
2020 | Body, tail | Pancreatic metastasis
from synovial sarcoma | Laparotomy/
splenopancreatectomy | (5) |
| Owen et al,
1997 | Head | Myofibroblastic
differentiation |
Pancreaticoduodenectomy/ without
preservation of the pylorus | (8) |
| Srinivasan et
al, 2008 | Body | Solitary fibrous
tumor | Distal
pancreatectomy | (6) |
| Kim et al,
2014 | Head |
Undifferentiated/unclassified sarcoma | Pylorus-preserving
pancreaticoduodenectomy | (10) |
| Kim et al,
2014 | Head |
Undifferentiated/unclassified sarcoma | Biopsy without
surgical resection | (10) |
| Kim et al,
2014 | Tail |
Undifferentiated/unclassified sarcoma | Biopsy/chemotherapy/
radiotherapy | (10) |
| Kim et al,
2014 | Tail | Solitary fibrous
tumor | Distal
pancreatectomy | (10) |
| Kim et al,
2014 | Body | Solitary fibrous
tumor | Resection | (10) |
| Kim et al,
2014 | Tail | Leiomyosarcoma | Distal
pancreatectomy/ radiotherapy | (10) |
| Kim et al,
2014 | Body | Schwannoma | Excision | (10) |
| Kim et al,
2014 | Body | Schwannoma | Resection | (10) |
| Kim et al,
2014 | Body | Atypical lipomatous
tumor/well-differentiated liposarcoma |
Excision/chemotherapy | (10) |
| Kim et al,
2014 | Tail | Angiomyolipoma | Distal
pancreatectomy | (10) |
| Kim et al,
2014 | Tail | Solid and cystic
hamartoma | Distal
pancreatectomy | (10) |
Case report
Patient information
A 35-year-old male with a known family history of
pancreatic cancer was referred to Hiwa Oncology Hospital
(Sulaimani, Iraq) and presented with left upper quadrant abdominal
pain, aggravated by eating, associated with anorexia, vomiting, and
a weight loss of 20 kg in 1 month (from 98 to 78 kg).
Clinical examination
A physical examination revealed tenderness in the
left quadrant of the abdomen. There was no jaundice or fever, and
the vital signs were normal.
Diagnostic assessment
Liver biochemical tests revealed an increased level
of alanine transaminase (72 IU/l; normal range, 10-50 IU/l);
however, aspartate aminotransferase (22 IU/l; normal range, 10-50
IU/l) and alkaline phosphatase (96 IU/l; normal range 40-130 IU/l)
levels were in the normal, reference range. As regards pancreatic
enzyme levels, amylase levels were normal (39 U/l; normal range,
<100 U/l), whereas lipase levels (169 U/l, normal range: ≤ 60)
were elevated. The leukocyte count was normal
(7.4x109/l; normal range, 4-11x109/l.
Endoscopic ultrasound imaging revealed a bulky heterogeneous
texture of the pancreatic body and tail, diffuse lobularity of the
pancreatic parenchyma, and a honeycomb appearance of the pancreas
with a normal main pancreatic duct. Scanning through the duodenum
revealed an anechoic cystic lesion measuring 22.6x27.6 mm in the
pancreatic head with some solid components in the wall of the cyst
and no communication was observed with the main pancreatic duct
(data not shown; ultrasound images are not available as these were
performed in another center). The findings indicated the presence
of a complex pancreatic solid-cystic lesion.
Therapeutic intervention
The patient underwent a pancreaticoduodenectomy
(Whipple procedure). The pancreatic head, a portion of the small
intestine, the gall bladder and the bile duct were all removed
during the procedure. The resected tumor size was 1.5x1.5 cm. The
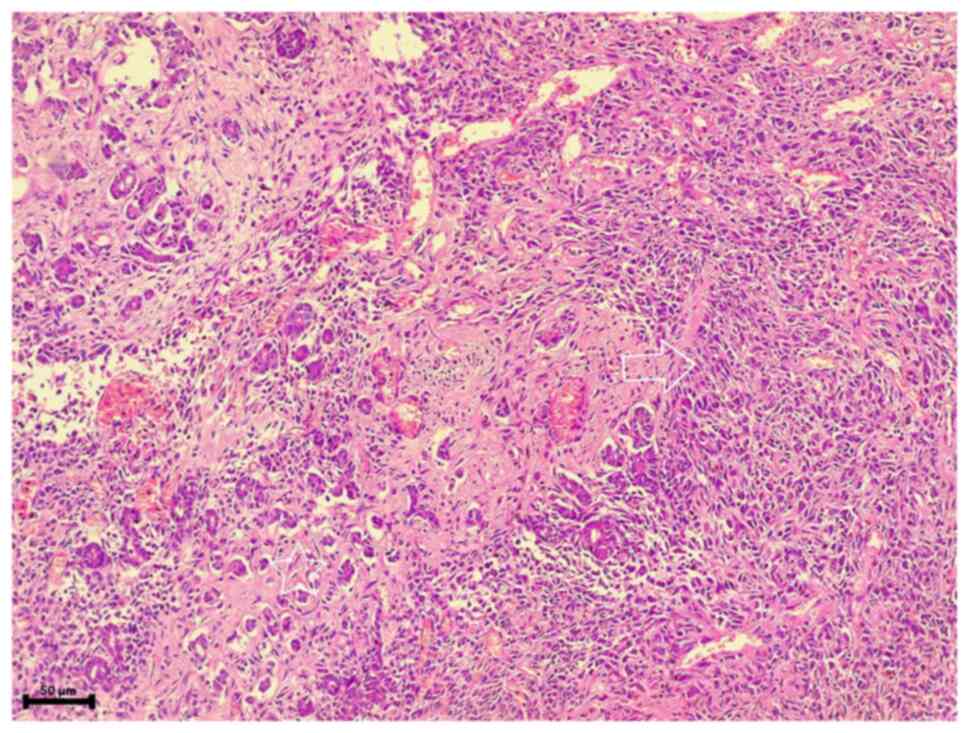
histological examination (performed as described below) revealed a
cellular tumor composed of neoplastic spindle cells with faint
cytoplasm and elongated oval-nuclei, illustrating mild atypia
arranged in a syncytial manner (Fig.
1). The tumor was infiltrative into the surrounding pancreatic
tissue, with the pathological stage of pTI-pN0 Mx. There was no
necrosis, and the tumor mitotic activity revealed sparse mitosis
(<5/50 high-powered field). The immunohistochemistry work-up was
negative for each of the epithelial markers (AE1/AE3), vascular
markers CD34, smooth muscle markers (desmin, smooth muscle actin
and β-catenin), gastrointestinal stromal tumor (CD117), melanoma
marker (HMB45) and progesterone receptor as well. Chromogranin and
synaptophysin staining were negative in Langerhans islet cells and
scattered endocrine cells. Positive stains for TLEI and vimentin
(moderate and diffuse nuclear staining patterns) and negative for
other markers were consistent with synovial sarcoma. No neoadjuvant
or adjuvant therapy was used for the patient, as the patient was
young and the tumor was small, localized and had a low mitotic
rate.
Histopathological staining
procedure
The specimen (3 mm) was fixed in 10%
neutral-buffered formalin for 2-3 days at 25˚C. The DiaPath
Donatello automated processor (Diapath S.P.A.) was used for further
processing the sample through the following steps: Using 10%
neutral-buffered formalin with an average time of 20 min; deionized
water for 10 min; dehydration and fixation by alcohol (70%),
followed by 95 and 99% (each step lasted 1-1:30 min); washing by
three stations of xylene (total 3 h); paraffin wax infiltration
(three stations, each lasted for 1 h).
The Sakura Tissue-Tek embedding system (Sakura
Finetek USA, Inc.) was used for embedding the blocks in paraffin
wax. The tissue sections were then placed through the Sakura
Accu-Cut SRM microtome (Sakura Finetek USA, Inc.). The sections
were floated in a Sakura 1451 water bath at 40-50˚C and placed on
regular glass slides. The DiaPath Giotto autostainer (Diapath
S.P.A.) was used to color the slides with hematoxylin and eosin
stains. The following steps were used: i) Washing the slides with
xylene three times for 7, 7 and 5 min, respectively; ii) using pure
alcohol for 3 min, followed by 90% alcohol for 4 min, 70% alcohol
for 3 min and finally, tap water for 2 min; iii) using hematoxylin
Gill II for 8 min at room temperature (Sigma-Aldrich Hematoxylin
Natural Black 1; Sigma-Aldrich; Merck KGaA); iv) using tap water
for 4 min, followed by ammonia water and tap water for 1 min for
each, and then 70% alcohol for 2 min. Eosin, prepared from
Sigma-Aldrich Eosin-Y disodium salt was used for 5 min at room
temperature, and the slides were then washed with tap water for 1
min. Following that, 70% alcohol was used for 15 sec, 90% for two
min, and 100% three times, each for 3 to 4 min. Finally, xylene was
used in three stations lasting 3, 5 and 4 min, respectively. The
slides were allowed to dry for 5 min before being screened under a
light microscope (Leica microsystems, Germany).
Follow-up
The patient experienced mild surgical site pain
following the procedure. He was discharged from the hospital after
an abdominal ultrasound revealed no notable findings. At 3 months
following the surgery, a computed tomography (CT-scan) and magnetic
resonance imaging (MRI) revealed mild pancreatic duct dilatation
with a 1.5 cm cyst at the site of anastomosis without any obvious
signs of recurrence.
Discussion
A sarcoma is a malignant tumor that develops from
mesenchymal tissue. It is less frequent than carcinoma and affects
mostly adolescents. Synovial sarcomas are malignant soft tissue
tumors of unknown etiology (4,5). These
tumors can appear in a variety of sites and are currently
considered to result from a mutation in mesenchymal cells. Primary
pancreatic sarcomas commonly present as large, high-grade tumors in
the pancreatic head, and they are more common in females than in
males (4). Liposarcoma,
leiomyosarcoma and malignant fibrous histiocytoma are identified as
other types of malignant pancreatic mesenchymal tumors (6). According to the literature, the first
surgical excision of a pancreatic spindle cell sarcoma was likely
performed by Trendelenburg in 1882, and Segre provided the first
pathological descriptions of two cases of pancreatic primary
sarcoma (7,8). Primary pancreatic tumors are relatively
large at presentation. The average size of a primary pancreatic
tumor was reported to be 7.5 cm in the study by Youngwirth et
al (9) and Kim et al
reported a mean tumor size of 5.8 cm in primary pancreatic sarcomas
(10).
The tumor size, high mitotic activity, the
appearance of cellular atypia, or malignant indicative
characteristics are all associated with a poor prognosis. Late
recurrences or metastases are not infrequent (8,11).
Histologically, there are three types of synovial sarcoma,
including monophasic (consisting only of spindle cells) (50-60%),
biphasic (consisting of both epithelial and spindle cell elements
(20-30%) and poorly differentiated (15-20%) (1). The prognosis of both the monophasic and
biphasic histological subtypes has been reported to be the same in
the literature. Moreover, poorly differentiated types have an
aggressive clinical history that often includes early recurrence
and metastasis (12).
Due to the rarity of primary pancreatic mesenchymal
tumors, further attention is required for diagnosis. First, it is
crucial to exclude metastasis from primary tumors originating from
locations outside the pancreas, such as the retroperitoneum, female
genital tract, extremities, or gastrointestinal tract. Second, in
the case that a microscopic examination reveals the malignant
spindle cell components, the possibility of sarcomatoid carcinoma
should be considered (10). Synovial
sarcoma is often portrayed as a heterogeneously enhanced,
well-defined tumor on a contrast-enhanced CT scan-or MRI. However,
as these imaging features are not specifically indicative of
synovial sarcoma, a histological examination is required for the
diagnosis (1). The case described in
the present study was a 35-year-old male, and an endoscopic
ultrasonography revealed a complex solid cystic lesion in the
pancreas.
Thus, histology and immunohistochemistry (IHC)
examinations are used to demonstrate the presence of synovial
sarcoma. Recently, gene expression profiling studies have revealed
overexpression of the transcriptional corepressor, TLE1, in
synovial sarcoma (11,13,14), and
further research discovered that >90% of synovial sarcomas had
moderate-to-strong TLE1 nuclear staining by IHC (11). As in the present study, IHC staining
for TLEI and vimentin was positive, the patient was diagnosed with
synovial sarcoma. The specific genetic abnormality that
characterizes synovial sarcoma is a non-random chromosomal
translocation between the long arm of chromosome 18 and the short
arm of chromosome X; these specific markers are helpful in making a
definitive diagnosis using reverse transcription PCR (2). Therefore, to confirm the diagnosis, the
existence of the SS18-SSX1 or SS18-SSX2 fusion gene needs to be
examined (1). A definite protocol
for treating these lesions is not discussed as there are a few case
reports of primary mesenchymal tumors of the pancreas. Furthermore,
the effectiveness of neoadjuvant or adjuvant chemotherapy or
radiotherapy is also inconclusive due to the rarity of this lesion
and the limited long-term follow-up (10). When deciding whether to remove a
pancreatic tumor surgically, numerous factors are considered. In
the study by Youngwirth et al (9), younger patients, smaller tumors and
lower grades of tumors were associated with more successful
decisions about resection. Therefore, complete resection with wide
margins is the preferred course of treatment, followed by radiation
and/or chemotherapy. Systemic chemotherapy is usually attempted for
unresectable masses (1,4). In the study by Youngwirth et al
(9), only 39.5% of patients had
surgery. Other treatment modalities, such as chemotherapy and
radiation therapy, were only utilized in a small number of cases
and it has been discovered that patients who underwent surgical
resection had a higher chance of survival. A study from the Mayo
Clinic data (15) confirmed the same
outcomes (9). Previous
representative large case series studies have demonstrated that the
5-year overall survival rate of adults with synovial sarcoma ranges
from 57 to 75%. The high application of adjuvant chemotherapy may
be responsible for this relatively improved outcome (12,16,17).
Although Takenaka et al (12)
did not demonstrate a significant difference in survival between
patients receiving adjuvant chemotherapy and those who did not,
this was probably due to the diversity of chemotherapeutic regimens
in each center. Makino et al (1) managed a case of left pelvic and femoral
synovial sarcoma. The patient underwent extensive tumor resection
followed by reconstruction and a constrained complete hip
megaprosthesis, with neoadjuvant adriamycin/ifosfamide (AI) therapy
for four cycles and adjuvant AI therapy for one cycle. Following
regular monitoring, the diagnosis of pancreatic metastases from
synovial sarcoma was confirmed (1).
The patient then received two cycles of adjuvant AI chemotherapy,
followed by two cycles of ifosfamide, carboplatin and etoposide,
with no significant adverse events and no recurrence for 30 months
(1). In the study by Luc et
al (4), no adjuvant therapy was
used after the pancreatic monophasic grade II synovial sarcoma was
diagnosed. They performed a distal pancreatectomy with splenectomy
and found a pathologically poorly differentiated intrapancreatic
tumor that had central necrosis and inflammation (4). Patients in the study by Youngwirth
et al (9) who underwent
surgical resection had smaller tumors and tumors that were poorly
or undifferentiated, similar to the case described herein. Owen
et al (8) concluded that a
pancreatoduodenectomy was an effective treatment for two cases of
large, pathologically malignant stromal tumors that presented in
the head of the pancreas. After 2 and 10 years of follow-up, both
patients were still alive and exhibited no signs of either locally
recurrent disease or distant metastasis (8). Guillou et al demonstrated that
the histological grade (grade 2 vs. 3) of the French Federation of
Cancer Centers (FNCLCC) is the most critical prognostic factor for
survival in patients with synovial sarcoma (18). Youngwirth et al (9) revealed that a worse tumor grade and
patient age were related to decreased adjusted survival in patients
who underwent surgical resection. This is crucial as it
differentiates pancreatic sarcomas from other types of pancreatic
cancer. In addition, they demonstrated a relatively high margin
positivity, which is known as a poor prognostic indicator due to
the size and location of the tumors in the pancreatic head
(9). Margin involvement and lymph
node metastases have been found to be the most significant
prognostic factors in previous studies on pancreatic cancer as a
whole. However, a higher tumor grade has been linked to a lower
overall survival rate in sarcomas (19). Pancreaticoduodenectomy was performed
in the patient described herein. Neoadjuvant or adjuvant therapy
was not used due to four favorable prognostic factors: A small,
localized tumor, a low mitotic rate, and the patient's age.
The major limitations of the present study are the
lack of biomarker evaluation and FDG-PET-CT scan evaluation
reports, as these could not be retrieved. As no standard guideline
was available for primary synovial carcinoma, the patient was
followed-up as a case of pancreatic adenocarcinoma.
In conclusion, pancreatic primary mesenchymal tumors
are extremely rare. Consequently, a diagnosis requires a careful
evaluation. Further investigations, such as IHC examinations are
helpful for a differential diagnosis. Due to the rarity of the
reported cases, information on the clinicopathologic
characteristics and the benefits of different treatment modalities
are limited. Surgical resection is the main method of
treatment.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
KS and OH were the surgeons who performed the
operation. SMA and RMA were the oncologists who managed the case.
AMA was the pathologist who examined the specimen, and was also a
major contributor to the conception of the study. BJM and FA were
major contributors to the conception of the study, as well as in
the literature search for related studies. FHK and DMH were
involved in the literature review, the writing of the manuscript,
as well as in the analysis and interpretation of the patient's
data. MK and BAA were involved in preparing and obtaining the
staining image from histopathological analysis. MK and BAA confirm
the authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from the
patient whose case is presented herein.
Patient consent for publication
Written informed consent was obtained from the
patient whose case is presented herein for the publication of his
data and any related images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Makino Y, Shigekawa M, Kegasawa T, Suda T,
Yoshioka T, Iwahashi K, Ikezawa K, Sakamori R, Yakushijin T,
Kajihara J, et al: A case report of pancreatic metastasis from
synovial sarcoma successfully treated by metastasectomy with
adjuvant chemotherapy. Medicine (Baltimore).
95(e4789)2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Sahara S, Otsuki Y, Egawa Y, Shimizu S,
Yoshizawa Y, Hosoda Y, Suzuki K, Sato Y and Kobayashi H: Primary
synovial sarcoma of the stomach-a case report and review of the
literature. Pathol Res Pract. 209:745–750. 2013.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Nagaraju S, Grethlein SJ, Vaishnav S,
Sharfuddin AA, Powelson JA and Fridell JA: Case report: Primary de
novo sarcoma in transplant pancreas allograft. Transplant Proc.
49:2352–2354. 2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Luc G, Collet D, Reich S, Stanislas S and
Sa-Cunha A: Primary monophasic synovial sarcoma of the pancreas. J
Visc Surg. 150:159–161. 2013.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Malek B, Saida S, Olfa J, Salma K, Maher
S, Riadh C and Khaled R: The management of pancreatic metastasis
from synovial sarcoma of the soft tissue: A case report. Rare
Tumors. 12(2036361320983691)2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Srinivasan VD, Wayne JD, Rao MS and Zynger
DL: Solitary fibrous tumor of the pancreas: Case report with
cytologic and surgical pathology correlation and review of the
literature. JOP. 9:526–530. 2008.PubMed/NCBI
|
|
7
|
Kiefer ED: Carcinoma of the pancreas. Arch
Int Med. 40:1–29. 1927.
|
|
8
|
Owen CH, Madden JF and Clavien PA: Spindle
cell stromal tumor of the pancreas: Treatment by
pancreatoduodenectomy. Surgery. 122:105–111. 1997.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Youngwirth LM, Freischlag K, Nussbaum DP,
Benrashid E and Blazer DG: Primary sarcomas of the pancreas: A
review of 253 patients from the National Cancer Data Base. Surg
Oncol. 27:676–680. 2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Kim JY, Song JS, Park H, Byun JH, Song KB,
Kim KP, Kim SC and Hong SM: Primary mesenchymal tumors of the
pancreas: Single-center experience over 16 years. Pancreas.
43:959–968. 2014.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Baranov E, McBride MJ, Bellizzi AM, Ligon
AH, Fletcher CDM, Kadoch C and Hornick JL: A novel SS18-SSX
fusion-specific antibody for the diagnosis of synovial sarcoma. Am
J Surg Pathol. 44:922–933. 2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Takenaka S, Ueda T, Naka N, Araki N,
Hashimoto N, Myoui A, Ozaki T, Nakayama T, Toguchida J, Tanaka K,
et al: Prognostic implication of SYT-SSX fusion type in synovial
sarcoma: A multi-institutional retrospective analysis in Japan.
Oncol Rep. 19:467–476. 2008.PubMed/NCBI
|
|
13
|
Foo WC, Cruise MW, Wick MR and Hornick JL:
Immunohistochemical staining for TLE1 distinguishes synovial
sarcoma from histologic mimics. Am J Clin Pathol. 135:839–844.
2011.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Tanaka M, Homme M, Yamazaki Y, Ae K,
Matsumoto S, Subramanian S and Nakamura T: Cooperation between
SS18-SSX1 and miR-214 in synovial sarcoma development and
progression. Cancers (Basel). 12(324)2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Zhang H, Jensen MH, Farnell MB, Smyrk TC
and Zhang L: Primary leiomyosarcoma of the pancreas: study of 9
cases and review of literature. Am J Surg Pathol. 34:1849–1856.
2010.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Ferrari A, Gronchi A, Casanova M, Meazza
C, Gandola L, Collini P, Lozza L, Bertulli R, Olmi P and Casali PG:
Synovial sarcoma: A retrospective analysis of 271 patients of all
ages treated at a single institution. Cancer. 101:627–634.
2004.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Spillane AJ, A'Hern R, Judson IR, Fisher C
and Thomas JM: Synovial sarcoma: A clinicopathologic, staging, and
prognostic assessment. J Clin Oncol. 18:3794–3803. 2000.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Guillou L, Benhattar J, Bonichon F,
Gallagher G, Terrier P, Stauffer E, Somerhausen Nde S, Michels JJ,
Jundt G, Vince DR, et al: Histologic grade, but not SYT-SSX fusion
type, is an important prognostic factor in patients with synovial
sarcoma: A multicenter, retrospective analysis. J Clin Oncol.
22:4040–4050. 2004.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Trovik LH, Ovrebo K, Almquist M, Haugland
HK, Rissler P, Eide J, Engellau J, Monge OR, Nyhus AB, Elde IK and
Jebsen NL: Adjuvant radiotherapy in retroperitoneal sarcomas. A
scandinavian sarcoma group study of 97 patients. Acta Oncol.
53:1165–1172. 2014.PubMed/NCBI View Article : Google Scholar
|