Introduction
Brain abscess (BA) constitutes 1-8% of all
intracerebral tumors (1). Even
though there has been immense progress made in diagnostic and
treatment techniques, BA remains one of the reasons for unfavorable
outcomes (2,3). However, modern neurosurgical
techniques, such as the use of neuronavigation in brain surgical
procedures, as well as non-invasive, accurate radiological
techniques, such as magnetic resonance spectroscopy, and more
targeted antibiotic therapy have succeeded in leading to notable
improvements in the surgical outcomes of patients with BA (1,4).
Primary or hematogenous extended abscesses more
frequently have an odontogenic or cardiogenic origin or are
observed in immunocompromised patients and are usually located at
the edge of gray and white matter (5). Over the past 15 years, the frequency of
primary BAs has decreased, while the frequency of post-traumatic or
post-operative (secondary) BAs has increased (6).
However, to the best of our knowledge, there is
currently no data available concerning the suitable therapeutic
management for BA, probably due to the low incidence. Moreover, to
the very best of our knowledge, no consensus or randomized
therapeutic trials have been published comparing the surgical
outcomes of patients with primary and secondary BA (7).
The present study thus aimed to address this gap in
the literature by comparing the surgical outcomes of patients with
primary and secondary BA, in order to determine the factors related
to unfavorable outcomes.
Patients and methods
Patients and data collection
The present retrospective study included 32 patients
with BA who underwent surgery in a local institution (University
Hospital of Larissa, Larissa, Greece) between February, 2013 and
December, 2023. The Institutional Review Board (IRB) of the
University of Thessaly, Greece, the School of Medicine, and the
School of Health Sciences approved its IRB Number, 2697/15-01-2024,
finalized by the 38th General Assembly on January 28, 2023. The
present study was in line with the Declaration of Helsinki (1995;
as revised in Edinburgh 2000). Written informed was obtained from
all the included patients or their next-of-kin or the parents/legal
guardians prior to the surgery.
These patients were separated into two groups as
follows: Group A (primary abscess) and group B (secondary or
iatrogenic-related abscess). Additional classifications in group B
were made following the neurosurgical intervention: Traumatic brain
injury (TBI), tumors, edema and intracranial hematoma (ICH).
Data collection was carried out on the basis of the
following inclusion criteria: Patients aged >8 years that
underwent a surgical procedure for primary or secondary BA
(following neurosurgical interventions: TBI, tumors, edema and ICH)
detection. The exclusion criteria consisted of clinical and
laboratory signs of severely reduced liver and kidney function,
immunosuppressive patients, impaired gastrointestinal absorption,
pregnancy, or the suspicion of resistant causative bacterial
strains. The participants were categorized based on the following
clinical or radiographical data retrieved from the medical archives
when available: Sex, age, Glasgow Coma Scale (GCS) upon admission,
diabetes, hypertension, alcohol use, drug abuse, history of
surgical procedures [external ventricular drain (EVD) and the site
of craniotomy/decompressive craniectomy (DC) in one site or
bilateral], and the timing of intravenous (IV) antibiotic treatment
prior to neurosurgical intervention (Table I). The clinical and radiographic data
were collected according to the clinical presentation (headache,
neurological deficit, or fever) and brain imaging (computed
tomography or magnetic resonance imaging), which was consistent
with a BA, according to the hospital radiologist.
 | Table IBaseline demographic characteristics
of the patients in the present study. |
Table I
Baseline demographic characteristics
of the patients in the present study.
| Parameters | All patients, n=32
(100%) | Group A, n=16
(50%) | Group B, n=16
(50%) | P-value |
|---|
| Age, mean ± SD
(years) | 55.3±16.7 | 54.6±16 | 55.9±17 | 0.720 |
| Sex (male), n
(%) | 23 (71.8) | 12 (37.5) | 11 (34.3) | 0.694 |
| GCS score upon
admission, mean ± SD | 11.4±2.5 | 11.3±2.7 | 11.5±2.4 | 0.741 |
| Diabetes mellitus, n
(%) | 4 (12.5) | 3 (9.3) | 1 (3.1) | 0.285 |
| Hypertension, n
(%) | 11 (34.3) | 6 (18.7) | 5 (15.6) | 0.710 |
| Alcohol use, n
(%) | 5 (15.6) | 2 (6.2) | 3 (9.3) | 0.626 |
| Drugs abuse, n
(%) | 1 (3.1) | 0 (0) | 1 (3.1) | 0.310 |
| History of surgical
procedure | | | | |
|
EVD | 1 (3.1) | 0 (0) | 1 (3.1) | 0.310 |
|
Site of
craniotomy/DC | | | | <0.05 |
|
One
site, n (%) | 14 (43.7) | 0 (0) | 14 (43.7) | 0.283 |
|
Bilateral,
n (%) | 2 (6.2) | 0 (0) | 2 (6.2) | 0.144 |
| Time of IV treatment
before intervention, mean ± SD (days) | 10.0±6.6 | 15.9±3.9 | 4.1±1.3 | <0.05 |
All patients received IV antibiotic therapy
according to the antibiogram for antimicrobial susceptibility. The
follow-up ranged from 1 to 10 years, commencing on the day of
hospital discharge, and was the same in both groups.
The primary outcome was the GCS score at 1 month
following neurosurgical intervention, and the secondary outcomes
were fever duration, hospital stay, intensive care unit stay,
mortality and cure (Table II).
 | Table IIOutcomes of the patients following
treatment. |
Table II
Outcomes of the patients following
treatment.
| Parameter | All patients, n=32
(100%) | Group A, n=16
(50%) | Group B, n=16
(50%) | P-value |
|---|
| GCS after
neurosurgical intervention, mean ± SD | 12.4±3.5 | 12.0±3.8 | 12.7±3.2 | 0.595 |
| Fever duration, mean
± SD (days) | 9.3±9.4 | 9.2±6.2 | 9.3±11.9 | <0.05 |
| Hospital stay, mean ±
SD (days) | 58.2±8.25 | 63.4±3.8 | 53.0±8.2 | <0.05 |
| ICU stay, mean ± SD
(days) | 13.1±13.2 | 14.2±14.5 | 12.0±12.2 | 0.661 |
| Mortality, n (%) | 5 (15.6) | 0 (0) | 5 (15.6) | <0.05 |
| Cured, n (%) | 27 (84.3) | 16(50) | 11 (34.3) | <0.05 |
Statistical analysis
The Statistical Package for the Social Sciences ver.
11 (SPSS, Inc.) was used for all statistical analyses. The
assessment of the normality of the allocation of variables was
carried out using the Shapiro-Wilk test, while Fisher's exact test
was performed for the categorical variables. The Mann-Whitney U
test was used for the evaluation of continuous data. Multivariate
linear regression analysis was performed in order to examine the
effects of multiple variables on the dependent variable. It was
possible to use receiver operating characteristic (ROC) analysis to
ascertain the utility of surgery for the primary vs. the secondary
BA as a predictor of adverse outcomes (mortality). A P-value
<0.05 was considered to indicate a statistically significant
difference.
Results
In total, 32 patients who underwent surgical
procedures for BAs with primary or secondary detection were
registered in the present study. These patients were separated into
two groups as follows: Group A (16 patients, 50%) with a primary
abscess and group B (16 patients, 50%) with a secondary abscess. Of
the 32 included patients, 23 (71.8%) were males, and the median age
was 55.3 years (range, 9-82 years). The baseline demographic
characteristics of the study participants are presented in Table I. The microorganisms isolated from
the tissue biopsied during surgery are presented in Table III.
 | Table IIIIsolated microorganisms in biopsy of
the patients operated on for abscess. |
Table III
Isolated microorganisms in biopsy of
the patients operated on for abscess.
| Microorganism | Group A, n=16 | Group B, n=16 |
|---|
| Acinetobacter
baumannii, n(%) | 1 (3.1) | 5 (15.6) |
| Enterococcus,
n (%) | 1 (3.1) | 2 (6.2) |
| Candida auris,
n (%) | 1 (3.1) | 3 (9.3) |
| Bacteroides
fragilis | 2 (6.2) | 0 (0) |
| Klebsiella
pneumoniae, n (%) | 3 (9.3) | 4 (12.5) |
| Streptococcus
intermedius, n (%) | 1 (4.3) | 6 (18.7) |
| Streptococcus
constellatus, n (%) | 2 (6.2) | 0 (0) |
|
Propionibacterium, n (%) | 5 (15.6) | 4 (12.5) |
| Serratia, n
(%) | 1 (3.1) | 3 (9.3) |
| Staphylococcus
aureus, n (%) | - | 6 (18.7) |
Univariate analysis revealed that there was a
statistically significant difference between the two groups with
respect to the following parameters: EVD and bilateral
craniotomy/DC; the timing of IV treatment initiation prior to the
intervention; and fever duration (P<0.05, Table IV).
 | Table IVUnivariate analysis for
mortality. |
Table IV
Univariate analysis for
mortality.
| Parameters | Survivors n=27 | Non-survivors,
n=5 | P-value |
|---|
| Age, mean ± SD
(years) | 55.5±17.3 | 59.2±13.3 | 0.604 |
| Sex (male), n
(%) | 1 (3.1) | 4 (12.5) | 0.660 |
| GCS score of
admission, mean ± SD | 11.4±2.7 | 11.2±1.0 | 0.249 |
| Diabetes mellitus,
n (%) | 3 (9.3) | 1 (3.1) | 0.581 |
| Hypertension, n
(%) | 10 (31.2) | 1 (3.1) | 0.461 |
| Alcohol use, n
(%) | 5 (15.6) | 0 (0) | 0.295 |
| Drugs abuse, n
(%) | 1 (3.1) | 0 (0) | 0.662 |
| History of surgical
procedure | | | |
|
EVD | 0 (0) | 1 (3.1) |
<0.05 |
|
Site of
craniotomy/DC | | | |
|
One
site, n (%) | 11 (34.3) | 3 (9.3) | 0.425 |
|
Bilateral,
n (%) | 0 (0) | 2 (6.2) |
<0.05 |
| Time of IV
treatment prior to intervention, mean ± SD (days) | 11.1±6.6 | 4.2±1.7 |
<0.05 |
| GCS after
neurosurgical intervention, mean ± SD | 12.4±3.7 | 12.4±2.5 | 0.748 |
| Fever duration,
mean ± SD (days) | 6.5±5.8 | 24.2±11.6 |
<0.05 |
| Hospital stay, mean
± SD (days) | 57.9±7.7 | 59.8±11.7 | 0.959 |
| ICU stay, mean ± SD
(days) | 11.6±12.9 | 21.2±13.8 | 0.189 |
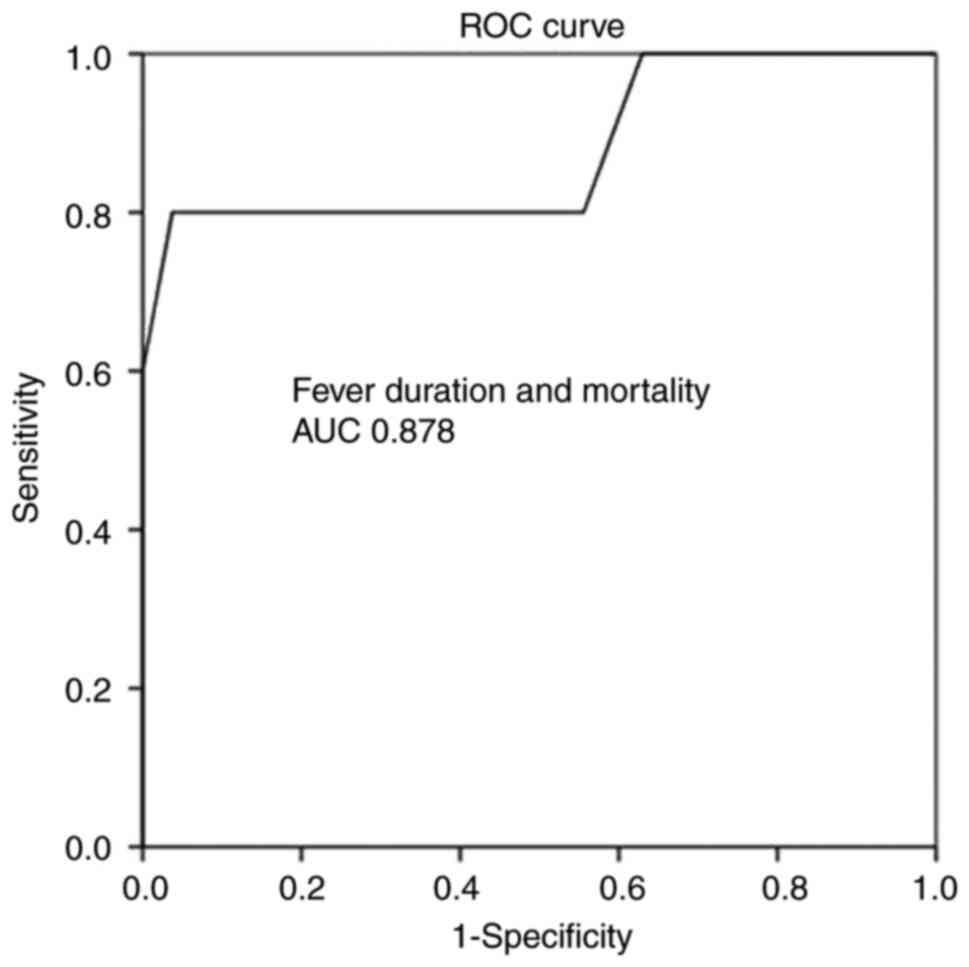
Multivariate linear regression analysis (Table V) disclosed that all aforementioned
parameters were associated with mortality. More specifically, ROC
analysis for IV treatment initiation prior to intervention
demonstrated that an interval of 21 days prior to the surgical
procedure had better dispersion (97% sensitivity and 100%
specificity) as evaluated by an area under the curve (AUC) standard
error (SE) of 0.815 (0.085) and P<0.05, as shown in Table VI and Fig. 1. In addition, ROC analysis for fever
duration revealed that an interval of 2.5 days following the
surgical intervention had a better dispersion (100% sensitivity and
93% specificity), as indicated by an AUC (SE) of 0.878 (0.109) and
P<0.05 (Table VI and Fig. 2).
 | Table VMultivariate linear regression
analysis for mortality. |
Table V
Multivariate linear regression
analysis for mortality.
| | | 95% CI for
Exp(B) |
|---|
| Parameter | P-value | Exp(B) | Lower | Upper |
|---|
| Surgical
procedure | | | | |
|
EVD |
<0.05 | -0.300 | -1.108 | -0.143 |
|
Site of
craniotomy/DC | | | | |
|
Bilateral,
n (%) |
<0.05 | 0.603 | 0.569 | 1.239 |
| Time of IV
treatment prior to the intervention, mean ± SD (days) |
<0.05 | -0.312 | -0.026 | -0.008 |
| Fever duration,
mean ± SD (days) |
<0.05 | 0.701 | 0.021 | 0.031 |
 | Table VIROC analysis for absorption. |
Table VI
ROC analysis for absorption.
| Parameters | Area | Std. error | 95% CI,
lower-upper | P-value |
|---|
| Surgical
procedure | | | | |
|
EVD | 0.600 | 0.155 | 0.297-0.90 | 0.484 |
|
Site of
craniotomy/DC | | | | |
|
Bilateral,
n (%) | 0.700 | 0.154 | 0.399-1.000 | 0.161 |
| Time of IV
treatment prior to intervention, mean ± SD (days) | 0.815 | 0.085 | 0.648-0.981 |
<0.05 |
| Fever duration,
mean ± SD (days) | 0.878 | 0.109 | 0.665-1.000 |
<0.05 |
Discussion
In the present study, patients who underwent
surgical procedures for BA with secondary detection had a more
favorable outcome compared with those that presented with primary
BA. In other words, patients who underwent surgery for a BA, EVD
treatment, or a bilateral craniotomy had worse outcomes. In
addition, the timing of IV treatment prior to the intervention and
fever duration were independent outcome predictors. Notably,
patients had a better outcome if the IV treatment commenced 21 days
prior to the surgical intervention. Moreover, if the fever
persisted for 2.5 days post-operatively, this was a good prognostic
factor for patient outcomes.
BA constitutes a highly controversial and
challenging entity, even in sophisticated healthcare facilities
with ample resources, and is associated with high mortality and
morbidity rates (2,3). A multidisciplinary approach is
mandatory, as is long-term follow-up, particularly in environments
with limited resources where the BA incidence is higher (8). However, although in low- and
middle-income countries (LMICs) BA accounts for 8% of all
intercranial masses and this figure declines to only 2% for
higher-middle-income countries (HMICs), primary BA in the child
population is very common in LMICs, while in HMICs only sporadic
cases have been reported (9).
Another major difference between LMICs and HMICs is the surgical
procedure, as in the former settings, the majority of cases are
treated via burr hole aspiration (9).
Major procedures, such as craniotomy or craniectomy
have been reported in a number of studies (10-13).
In a previous cohort study, only one patient was treated via burr
hole aspiration (10). According to
the current guidelines, antimicrobials should be withheld until
aspiration or the excision of BA in patients without severe disease
if neurosurgery can be carried out within 24 h following the
radiological diagnosis (10). In the
patient sample in the present study, however, the surgical removal
of the BA was usually preceded by antibiotic therapy, as the
majority of the patients were referred to the clinic following an
ENT (ear, nose and throat) consultation and had been receiving
antimicrobial medication for days or weeks. Hakan et al
(14) reported a significant
association between a high fever (>38.5˚C) and mortality.
According to the available literature, a poor
prognosis of patients with BA is more likely in immunocompromised
patients, as well as in those with a history of diabetes and a low
GCS score (7). In general, patients
presenting with a lower GCS score have a poorer prognosis and often
develop fatal complications (1,3). In the
present study, there was no association between diabetes and GCS at
the time of admission.
Despite the surgical management of BA, antibiotics
are very efficient in both the early and late periods (1,3). The
limited efficacy of antibiotics, mainly after the incapsulated
stage, is due to the failure to achieve the sufficient therapeutic
absorption of the antibiotic into the abscess cavity (1,3). On the
other hand, the implications of long-term antibiotic use, such as
increased liver and kidney burden, intestinal microbiome disorders,
side-effects and effects on the immune system, constitute major
concerns, particularly in patients with BA (1,3). In
addition, antibiotic resistance, which is a global issue, enhances
the susceptibility to secondary infections and has negative effects
on the microbiota and health (1,3). Similar
to all these reports, in the present study, management with
antibiotics was one of the main parameters associated with
favorable outcomes. More precisely, it was found that IV antibiotic
administration 21 days prior to the surgical removal of the BA was
related to improved outcomes.
In extant literature, fever is the most commonly
reported symptom of BA (15). In the
present study, a fever duration exceeding 2.5 days post-operatively
was related to a poor response to treatment and thus with an
unfavorable outcome.
The present study had several limitations that
should be noted when interpreting the reported findings. The main
limitation stems from its retrospective nature, which increased the
risk of possible errors in collecting and interpreting the data
from the clinical history, such as seizures or steroid
administration. In addition, another limitation was that all
patients were treated with IV antibiotics and there was no control
group.
In conclusion, currently, BA is still considered a
highly complex pathological entity with different
pathophysiological aspects to be considered to treat their
catastrophic sequelae. A multidisciplinary approach involving a
combination of often multiple surgical procedures and a prolonged
antibiotic administration may improve the functional outcomes of
patients if the underlying pathology does not preclude this
possibility. The present study revealed that patients who underwent
surgical procedures for BA with secondary detection had a more
favorable outcome compared with those with primary BA and a history
of EVD treatment and/or bilateral craniotomies. In addition, it was
found that the timing of IV treatment initiation prior to the
intervention and fever duration could predict the outcomes of
patients. Thus, patients had a better outcome if the IV treatment
commenced 21 days prior to the surgical intervention. Moreover, if
the fever persisted for not >2.5 days following the surgery,
this was a good prognostic factor for patient outcomes.
Aspects that are still controversial and should be
assessed further through high-quality studies include the
following: The surgical approach for major craniotomies or DCs with
full excision of BA or minimal image-guided stereotactic
aspiration, the duration of IV antibiotic medication (6-8 weeks),
when to switch to oral antibiotics, and for how long.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
CG and GF conceptualized the study. CG, KP, GC, TS,
PS, ΝΤ, AK, VEG, GF and KNF made a substantial contribution to data
interpretation and analysis, and wrote and prepared the draft of
the manuscript. CG and GF analyzed the data and provided critical
revisions. CG and GF confirm the authenticity of all the raw data.
All authors contributed to manuscript revision, and have read and
approved the final version of the manuscript.
Ethics approval and consent to
participate
The Institutional Review Board (IRB) of the
University of Thessaly, Greece, the School of Medicine, and the
School of Health Sciences approved its IRB Number, 2697/15-01-2024,
finalized by the 38th General Assembly on January 28, 2023. The
present study was in line with the Declaration of Helsinki (1995;
as revised in Edinburgh 2000). Written informed was obtained from
all the included patients or their next-of-kin or the parents/legal
guardians prior to the surgery.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Sharma BS, Gupta SK and Khosla VK: Current
concepts in the management of pyogenic brain abscess. Neurol India.
48:105–111. 2000.PubMed/NCBI
|
|
2
|
Lu CH, Chang WN and Lui CC: Strategies for
the management of bacterial brain abscess. J Clin Neurosci.
13:979–985. 2006.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Takeshita M, Kagawa M, Izawa M and
Takakura K: Current treatment strategies and factors influencing
outcome in patients with bacterial brain abscess. Acta Neurochir
(Wien). 140:1263–1270. 1998.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Salah M and Shalaby A: Computed
tomography-guided stereotactic surgery in the management of brain
lesions: A single-center experience. Surg Neurol Int.
14(184)2023.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Frazier JL, Ahn ES and Jallo GI:
Management of brain abscesses in children. Neurosurg Focus.
24(E8)2008.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Carpenter J, Stapleton S and Holliman R:
Retrospective analysis of 49 cases of brain abscess and review of
the literature. Eur J Clin Microbiol Infect Dis. 26:1–11.
2007.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Muzumdar D, Jhawar S and Goel A: Brain
abscess: An overview. Int J Surg. 9:136–144. 2011.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Ooi SZY, Sichimba D, Dalle DU,
Higginbotham G, Takoutsing BD, Bankole NDA, Egiz A, Kotecha J, de
Koning R, Nguembu S, et al: Management and outcomes of paediatric
intracranial suppurations in low- and middle-income countries: A
scoping review. Front Surg. 8(690895)2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Nathoo N, Narotam PK, Nadvi S and van
Dellen JR: Taming an old enemy: A profile of intracranial
suppuration. World Neurosurg. 77:484–490. 2012.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Bodilsen J, D'Alessandris QG, Humphreys H,
Iro MA, Klein M, Last K, Montesinos IL, Pagliano P, Sipahi OR,
San-Juan R, et al: European society of clinical microbiology and
infectious diseases guidelines on diagnosis and treatment of brain
abscess in children and adults. Clin Microbiol Infect. 30:66–89.
2024.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Fotakopoulos G, Gatos C, Georgakopoulou
VE, Lempesis IG, Spandidos DA, Trakas N, Sklapani P and Fountas KN:
Role of decompressive craniectomy in the management of acute
ischemic stroke (review). Biomed Rep. 20(33)2024.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Fotakopoulos G, Tsianaka E, Siasios G,
Vagkopoulos K and Fountas K: Posttraumatic hydrocephalus after
decompressive craniectomy in 126 patients with severe traumatic
brain injury. J Neurol Surg A Cent Eur Neurosurg. 77:88–92.
2016.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Fotakopoulos G, Tsianaka E, Vagkopoulos K
and Fountas KN: According to which factors in severe traumatic
brain injury craniectomy could be beneficial. Surg Neurol Int.
7(19)2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Hakan T, Ceran N, Erdem I, Berkman MZ and
Göktaş P: Bacterial brain abscesses: An evaluation of 96 cases. J
Infect. 52:359–366. 2006.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Rosenfeld EA and Rowley AH: Infectious
intracranial complications of sinusitis, other than meningitis, in
children: 12-year review. Clin Infect Dis. 18:750–754.
1994.PubMed/NCBI View Article : Google Scholar
|