Introduction
The vulvar lesions described to date exhibit a wide
range of morphologies. Among these, some are neoplastic, displaying
malignant features and carrying a significant risk of morbidity,
while others are non-neoplastic or benign neoplasms (1). Primary vulvar adenocarcinomas are rare
occurrences (2). Mesenchymal lesions
of the vulva may manifest as locally specific to the vulvar region
or as non-specific soft tissue neoplasms, which occur more
frequently at sites other than the vulva. Local mesenchymal lesions
confined to the lower genital tract include fibroepithelial stromal
polyps of the vulva, cellular angiofibroma, angiomyofibroblastoma,
superficial angiomyxoma and aggressive angiomyxoma (3).
Fibroepithelial stromal polyps of the female genital
tract were initially described as a distinct clinical entity by
Norris and Taylor (4) in the early
1960s. This lesion is benign and typically occurs in women of
reproductive age, more frequently in the vagina than in the cervix
and vulva (5). Fibroepithelial
stromal polyps of the vulva typically present as solitary polypoid
stromal lesions covered by normal squamous epithelium (6). Their size is usually not >5 cm,
although in rare cases, they may reach sizes of up to 20 cm and may
weigh >1 kg (7). The pathogenesis
of vulvar fibroepithelial polyps is largely unknown; however,
hormonal stimulation and chronic inflammation are considered major
predisposing risk factors (8).
The present study describes the case of a patient of
vulvar fibroepithelial polyp, emphasizing the rarity of this
clinical entity. Additionally, it addresses the clinical, imaging
and histological diagnostic approach to these lesions, highlighting
the necessity of surgical resection and the importance of
differentiating them from malignant vulvar lesions.
Case report
A 44-year-old female patient of reproductive age
presented at the Outpatient Gynecological Clinic of the General
Hospital of Trikala, Trikala, Greece. She reported that the sole
reason for her visit was the presence of a small tumor on her
vulva, which was not associated with neither pain nor tenderness.
The patient only reported experiencing mild discomfort in her
external genitalia. No history of trauma or friction injury to the
vulvar area was reported, and there were no clinical signs of
vulvar infection or inflammation. The patient could not recall when
the polyp first appeared; however, she had stated that over the
past year, she noted an increase in its size, prompting her to
consult a gynecologist. Her menstrual cycle was reported as normal,
she had a normal hormonal status, typical of a pre-menopausal woman
of her age and no abnormal findings were noted from the last Pap
smear test, which had been conducted 2 years prior as part of her
gynecological screening. As regards her obstetric history, she had
three lower-segment cesarean deliveries. Additionally, the patient
reported a medical history of hypothyroidism, which was effectively
controlled with appropriate medical treatment. She reported no
other chronic or metabolic disorders.
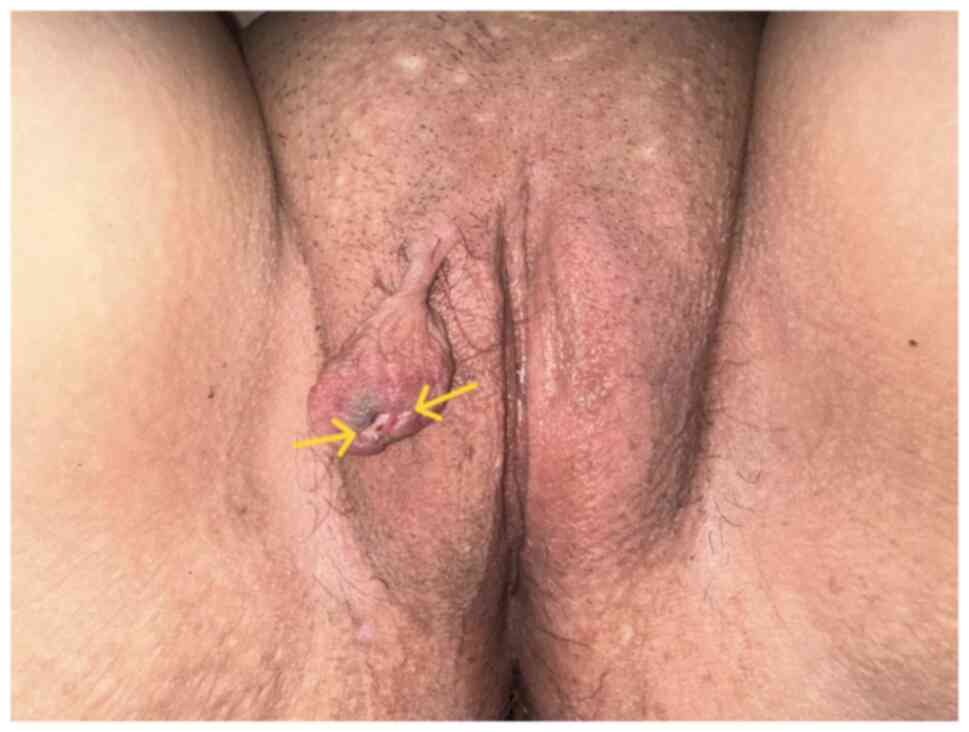
Upon a clinical examination, a painless pedunculated
tumor was noted at the external genitalia, with a maximal diameter
of ~5 cm including the pedicle. The tumor originated from the upper
section of the anterior surface of the right labium majus, near the
clitoris. It exhibited density on palpation and was covered with
normal skin, displaying ulcerative lesions (Fig. 1). No abnormal findings were observed
during a clinical and transvaginal ultrasound examination of the
internal genitalia. The Pap smear test conducted at that time as
part of preventive screening yielded normal results. The levels of
inflammatory markers and tumor markers were within normal
laboratory values (Table I).
 | Table IThe results of laboratory tests that
were performed during the pre-operative assessment of the
patient. |
Table I
The results of laboratory tests that
were performed during the pre-operative assessment of the
patient.
| Laboratory tests | Preoperative
values | Laboratory reference
values |
|---|
| Ht | 34.1% | 37.7-49.7% |
| Hb | 10.6 g/dl | 11.8-17.8 g/dl |
| PLT |
331x103/ml |
150-350x103/ml |
| WBC |
6.76x403/ml |
4-10.8x103/ml |
| NEUT | 49.8% | 40-75% |
| APTT | 27.4 sec | 24.0-35.0 sec |
| INR | 1.05 | 0.8-1.2 |
| CRP | 0.1 mg/dl | 0.5 mg/dl |
| Glu | 88 mg/dl | 75-115 mg/dl |
| Cr | 0.83 mg/dl | 0.40-1.10 mg/dl |
| CEA | 2.26 ng/ml | <5 ng/ml |
| CA125 | 21.3 U/ml | ≤35 U/ml |
| CA15-3 | 17.6 U/ml | 0.0-31.3 U/ml |
| CA15-9 | 14.9 U/ml | 0.0-37 U/ml |
Based on the clinical findings, a fibroepithelial
polyp of the vulva was suspected and the patient was scheduled for
surgery after obtaining her informed consent. In the operating
room, under spinal anesthesia, the wide excision of the
pedunculated tumor was performed, followed by suturing of the
surgical wound.
The collected surgical specimens were sent to the
Histopathology Laboratory of the Hospital (Anatomic Pathology
Laboratory of the General Hospital of Trikala) for further
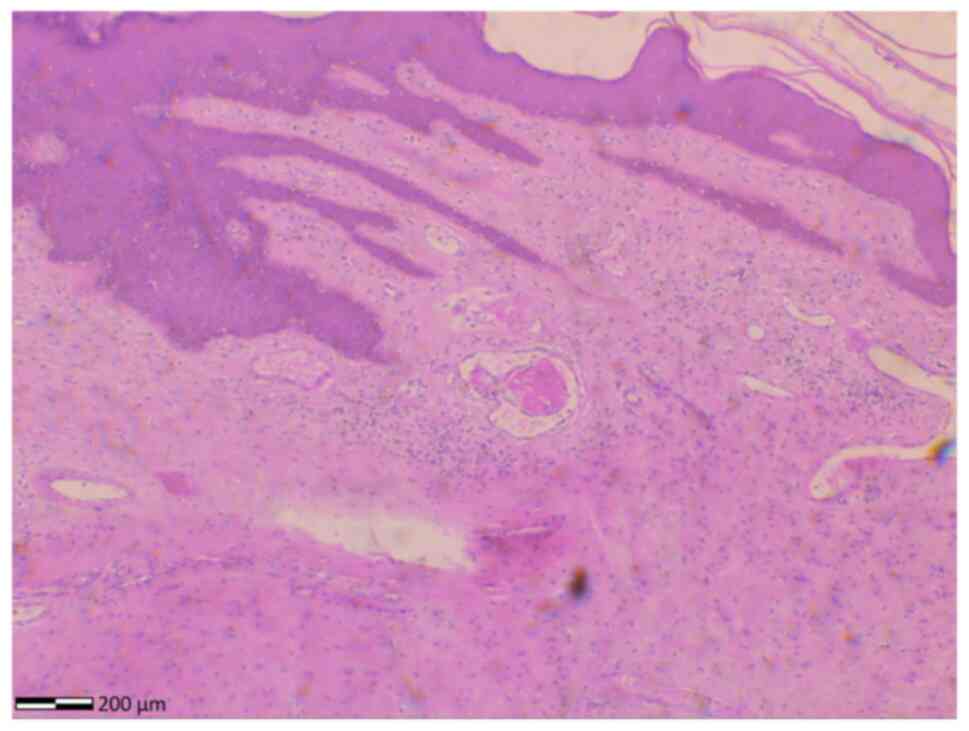
assessment. The pathological examination of the surgical specimen
macroscopically revealed a polypoidal stromal lesion extending to
the epidermis, with the presence of several blood vessels.
Microscopic analysis was performed utilizing hematoxylin and eosin
staining. As per the Laboratory's routine protocol, specimens were
embedded in paraffin cubes and 5-mcm-thick sections were obtained
for analysis. A buffered, 10% formalin solution was utilized as a
fixative medium, for 36 h at room temperature. Hematoxylin and
eosin staining 0.5% alcohol (Diachel A.E.) was applied for 12 min
at room temperature. All microscopic examinations were performed
using a LEICA DM2000 optical microscope (Leica Microsystems GmbH).
The microscopic examination revealed spindle-shaped and stellate
cells without atypia or mitoses, collagen deposition, congestion
and localized thrombosis of the stromal vessels. In addition,
epidermis with hyperplasia and hyperkeratosis was observed and no
dysplastic epithelial lesions were observed (Fig. 2).
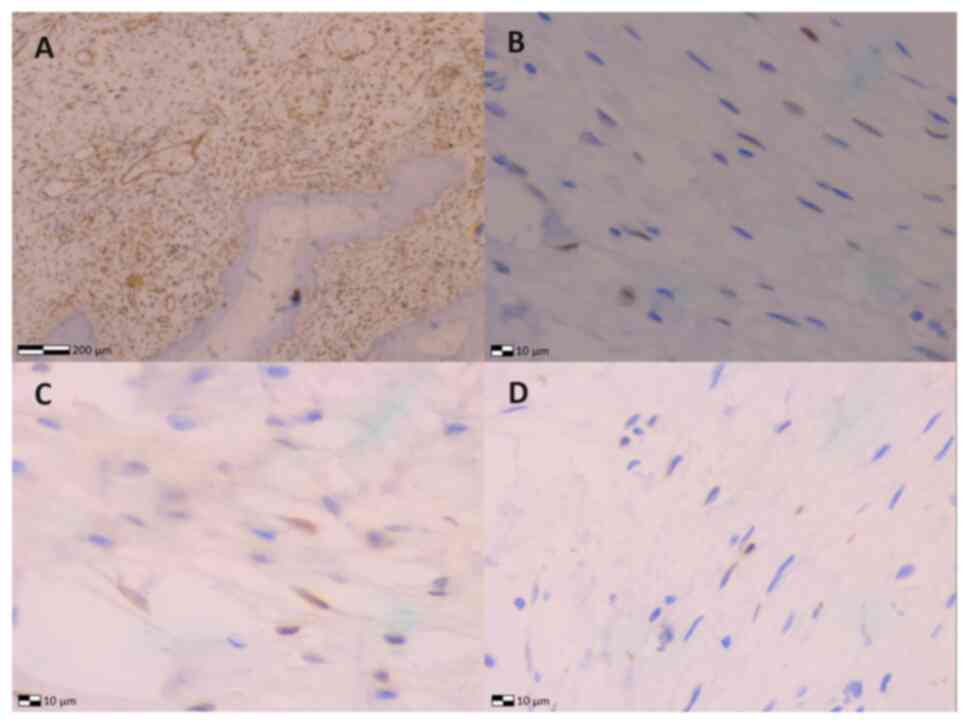
The specimens were also subjected to
immunohistochemical analysis. Paraffin-embedded sections 4µm thick
were collected and dewaxed for 40 min at 70˚C. Subsequently, they
were placed sequentially in BOND™ Dewax solution, 100% v/v ethanol
solution and BOND™ wash solution. Heat-induced epitope retrieval
(HIER) was performed via the use of BOND™ Epitope Retrieval ER1
Solution, (pH 7) for estrogen receptor (ER), progesterone receptor
(PR), Vimentin (VIM) and Ki67 for 20 min at 100˚C. The block
peroxide kit (Bond; Leica Biosystems) was used for 5 min. Antibody
dilution was performed with a proprietary Leica (Bond; Leica
Biosystems) solution as follows: Dilution for ER (M3643; Agilent
Technologies, Inc.) was 1:40, for PR (M3569; Agilent Technologies,
Inc.) was 1:100, for VIM (M0725; Agilent Technologies, Inc.) was
1:100 and for Ki67 (F0788; Agilent Technologies, Inc.) was 1:20.
All antibodies were incubated for a period of 30 min in total. In
particular, the post-primary kit (Bond; Leica Biosystems) was used
for a duration of 10 min at an incubation temperature of 100˚C.
Subsequently, a secondary detection kit polymer (Bond; Leica
Biosystems) was used for a duration of 10 min and the DAB kit
(Bond; Leica Biosystems) for 10 min to facilitate visualization.
Hematoxylin was applied for 5 min as a counterstain at room
temperature and the sections were dehydrated, mounted and
coverslipped. The resulting slides were examined under the same
LEICA DM2000 optical microscope (Leica Microsystems GmbH). The
specimen exhibited positivity for vimentin (VIM), estrogen
receptors (ER), progesterone receptors (PR) and Ki67 (Fig. 3).
The post-operative course of the patient was
uneventful, and the patient was discharged from the clinic on the
first post-operative day. At 6 months post-operatively, no
recurrence of the fibroepithelial polyp was observed at its
extraction site from the vulva. The patient was advised to
follow-up with annual visits to the gynecological clinic at the
General Hospital of Trikala.
Discussion
The diagnosis of vulvar fibroepithelial polyps
presents significant challenges. Ultrasound findings, magnetic
resonance imaging findings and detailed histological analysis need
to be combined with the clinical presentation of the tumor, which
is typically non-specific (9). Small
fibroepithelial polyps of the vulva (<5 cm) are often
asymptomatic and are incidentally discovered during gynecological
examinations. In other cases, patients may report their presence
when seeking medical attention at a later stage. In rare cases of
large fibroepithelial polyps (>5 cm), symptoms are more likely
to occur, with bleeding being the most frequent clinical
manifestation. Additionally, ulcerative lesions and signs of
inflammation, often accompanied by varying degrees of secondary
infection, may be associated with large vulvar fibroepithelial
polyps (10,11). A single case report of a patient with
sepsis attributed to a huge ulcerative and inflammatory
fibroepithelial polyp of the vulva has been documented in the
international literature (12). In
the patient in the present study, the small size of the polyp
(<5 cm) with the presence of a thick pedicle without signs of
vascular obstruction or torsion (Fig.
1) did not explain the presence of ulcerative lesions due to
insufficient blood supply. Therefore, considering the absence of
trauma to the vulvar region, the presence of ulcerative lesions on
the surface of the tumor raised strong suspicion regarding the
possibility of malignancy. Benign vulvar fibroepithelial polyps can
often be mistaken for malignant tumors due to their diverse
morphological features (13).
Malignant vulvar lesions that should be included in the
differential diagnosis of fibroepithelial polyps include aggressive
angiomyxoma, angiomyofibroblastoma, sarcoma, superficial cervical
and vaginal myofibroblastoma, cellular angiofibroma, perineurioma,
botryoid rhabdomyosarcoma, and squamous cell carcinoma (8,14).
Contemporary imaging modalities can markedly aid in
the pre-operative diagnosis of vulvar fibroepithelial polyps,
particularly when they are of substantial size. An ultrasound is
considered a first-line imaging modality, being more accessible and
cost-effective than computed tomography and magnetic resonance
imaging (5). An ultrasound can
detect the presence of soft tissue within the mass and, depending
on the location of the fibroepithelial polyp in the vulvar region,
and it can exclude the presence of a hernia containing omentum or
intestine (11). Doppler
ultrasonography may reveal a central hypoechoic mass of varying
dimensions with increased peripheral vascularity (15). Additionally, findings from magnetic
resonance imaging, such as stromal hypodense areas on T2-weighted
scans and linear hyperdense areas on T1 images, are suggestive of
vulvar fibroepithelial polyps (16).
In 2019, Yoo et al (14)
reported that contrast-enhanced diffusion-weighted magnetic
resonance imaging can aid in differentiating vulvar fibroepithelial
polyps from other vulvovaginal stromal tumors. In the patient
described herein, given the small size of the tumor, ultrasound and
magnetic resonance imaging were not deemed necessary as part of the
preoperative evaluation. Based on the clinical findings, it was
decided to proceed with the wide surgical excision of the lesion
followed by histological examination of the tumor.
Accurate histological analysis of vulvar
fibroepithelial polyps is crucial for diagnosis. Microscopic
examination of the tumor is essential for distinguishing vulvar
fibroepithelial polyps from malignant vulvar lesions (17). Histologically, vulvar fibroepithelial
polyps exhibit a cellular stromal component with a central vascular
core, covered by overlying benign squamous epithelium. The hallmark
of vulvar fibroepithelial polyps is the presence of stellate and
multinucleated stromal cells, typically located at the
epithelium-stroma interface. These cells express estrogen and
progesterone receptors, react to desmin, and occasionally to smooth
muscle fiber actin (18,19). In the patient in the present study, a
histological examination ruled out the presence of vulvar
malignancy. The immunohistochemical analysis of the tumor was
performed to confirm its differentiation from malignant vulvar
lesions. In the case of the patient described herein, the
importance of wide surgical excision of the lesion and the
necessity of accurate histological diagnosis are emphasized, as the
risk of local recurrence varies for these tumors (18).
Total surgical resection is the preferred treatment
option for vulvar fibroepithelial polyps, particularly for those
that are large in size. Cryotherapy or cauterization may be
considered ideal treatment modalities for small polyps (20,21).
Timely and proper surgical treatment, accompanied by definitive
histological diagnosis, is considered to significantly contribute
to the radical management of vulvar fibroepithelial polyps and to
the management of anxiety in these patients (22). Although not common, local recurrence
can be observed, particularly in cases where the polyp resection is
incomplete (23). In the patient in
the present study, there was no evidence of local recurrence at 6
months post-operatively. To ensure the early detection of potential
future recurrence, the patient was advised to undergo regular
follow-up with annual visits to the outpatient gynecological clinic
of the General Hospital of Trikala.
In conclusion, fibroepithelial stromal polyps of the
vulva are rare benign mesenchymal tumors that typically occur in
women of reproductive age. Following the wide surgical excision of
the vulvar lesion, confirmation of the diagnosis through meticulous
microscopic histological examination of the surgical specimen is
necessary in all cases. Furthermore, the presence of non-traumatic
ulcerative lesions on the surface of the polyp, even in cases where
tumors are small in size, should raise clinical suspicion of vulvar
malignancy, prompting the implementation of immunohistochemical
assessment of the tumor to definitively differentiate it from
vulvar malignancies.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data used in the current study are available
from the corresponding author upon reasonable request.
Authors' contributions
All authors (ET, AT, IRA, EX, AZ, EK, AC, AL, ES, MM
and IT) participated in the preparation of the manuscript. ET, AT,
EX and AZ participated in the acquisition, analysis, or
interpretation of the patient's data, in the drafting of the
manuscript, and agree to be accountable for all aspects of the
work, will review the final version to be published. IRA, EK, AC
and AL were involved in the conception and design of the study, in
the provision of study materials or patient data, in data
collection and aggregation, and in data analysis and
interpretation. ES and MM were involved in the provision of study
materials (immunohistochemical analysis, histological images), and
in data collection and aggregation. IT made substantial
contributions to the conception or design of the study,
acquisition, analysis, or interpretation of data, drafting of the
manuscript, critical review of the manuscript for important
intellectual content, and agrees to be accountable for all aspects
of the work. IT also reviewed the final version to be published and
supervised the study. EK, AL and IT confirm the authenticity of all
the raw data.
Ethics approval and consent to
participate
The present study was conducted according to the
guidelines of the Declaration of Helsinki. Written informed consent
was obtained from the patient.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the present case report and any
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Kelekçi KH, Özyurt S, Özkan B, Karaca Ş,
Karakuzu A and Bilgin İ: The impact of inflammatory and infectious
diseases of vulvar on quality of life. J Menopausal Med.
22:131–138. 2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Desouki MM and Fadare O: Primary
adenocarcinomas of the vulva and related structures: An enigmatic
and diverse group of tumors✰. Semin Diagn Pathol.
38:71–84. 2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Chapel DB, Cipriani NA and Bennett JA:
Mesenchymal lesions of the vulva. Semin Diagn Pathol. 38:85–98.
2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Norris HJ and Taylor HB: Polyps of the
vagina. A benign lesion resembling sarcoma botryoides. Cancer.
19:227–232. 1966.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Bozgeyik Z, Kocakoc E, Koc M and Ferda
Dagli A: Giant fibroepithelial stromal polyp of the vulva: Extended
field-of-view ultrasound and computed tomographic findings.
Ultrasound Obstet Gynecol. 30:791–792. 2007.PubMed/NCBI View
Article : Google Scholar
|
|
6
|
Nucci MR and Fletcher CD: Vulvovaginal
soft tissue tumours: Update and review. Histopathology. 36:97–108.
2000.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Chan MM, Yong TT and Sittampalam K: Giant
labial fibroepithelial stromal polyp. Malays J Pathol. 35:91–94.
2013.PubMed/NCBI
|
|
8
|
Kurniadi A, Rinaldi A, Yulianti H, Bazar
AR, Prasetyawati RD and Tjandraprawira KD: Multiple vulvar giant
fibroepithelial polyps: A rare case occurrence. Case Rep Obstet
Gynecol. 2022(5712925)2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Andrew MS and Poon C: A rare case of a
giant vulvarfibroepithelial stromal polyp. J Pediatr Adolesc
Gynecol. 35:501–504. 2022.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Avila J, Nicol K, Hewitt GD and Matson SC:
Vulvar fibroepithelial polyps in a female adolescent: A case
report. J Pediatr Adolesc Gynecol. 30:595–597. 2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Dura MC, Aktürk H, Sungur GŞ and Alsalamin
WOI: A giant fibroepithelial polyp of the vulva. Cureus.
15(e39152)2023.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Amin A, Amin Z and Al Farsi AR: Septic
presentation of a giant fibroepithelialpolyp of the vulva. BMJ Case
Rep. 2018(bcr2017222789)2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Navada MH, Bhat PR, Rao SV and G N: Large
fibroepithelial polyp of vulva. Case Rep Dermatol Med.
2011(273181)2011.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Yoo J, Je BK, Yeom SK, Park YS, Min KJ and
Lee JH: Giant fibroepithelial stromal polyp of the vulva:
Diffusion-weighted and conventional magnetic resonance imaging
features and pathologic correlation. J Pediatr Adolesc Gynecol.
32:93–97. 2019.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Smet C, Gomes TG, Silva L and Matias J:
Giant fibroepithelial vulvar polyp in a pregnant woman. BMJ Case
Rep. 14(e236106)2021.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Kato H, Kanematsu M, Sato E, Ito N, Furui
T and Hirose Y: Magnetic resonance imaging findings of
fibroepithelialpolyp of the vulva: Radiological-pathological
correlation. Jpn J Radiol. 28:609–612. 2010.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Bahadur A, Mundhra R, Heda A and Singh A:
Large vulvar fibroepithelial polyp and review of differentials. BMJ
Case Rep. 17(e259389)2024.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Pharaon M, Warrick J and Lynch MC:
Fibroepithelial stromal polyp of the vulva: Case report and review
of potential histologic mimickers. Int J Gynecol Pathol. 37:e1–e5.
2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Kurniawati EM, Djunaidi F and Kurniasari
N: Giant fibroepithelial polyps of the vulva in a woman with
uterine myoma and primary infertility: A case report and literature
review. Am J Case Rep. 23(e933198)2022.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Rexhepi M, Trajkovska E, Besimi F and
Rufati N: Giant fibroepithelial polyp of vulva: A case report and
review of literature. Pril (Makedon Akad Nauk Umet Odd Med Nauki).
39:127–130. 2018.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Ogura N, Inagaki M, Yasuda R, Yoshida S
and Maeda T: A vaginal fibroepithelial stromal polyp: A case report
with magnetic resonance images. BJR Case Rep.
8(20210189)2022.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Korkontzelos I, Mpourazanis G, Goshi F,
Vogiatzis R, Theodorou DJ, Korkontzelou PD, Balassi E,
Georgakopoulou VE and Papamitsou T: Giant ulcerated fibroepithelial
stromal polyp of the vulva: A case report. Cureus.
15(e40017)2023.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Ostör AG, Fortune DW and Riley CB:
Fibroepithelial polyps with atypical stromal cells (pseudosarcoma
botryoides) of vulva and vagina. A report of 13 cases. Int J
Gynecol Pathol. 7:351–360. 1988.PubMed/NCBI View Article : Google Scholar
|