Introduction
Varices are dilated, edematous superficial veins
located in the subcutaneous tissue, commonly occurring in pregnant
women, and are typically found in the lower extremities. Pregnancy
is considered a significant contributing factor to the increased
incidence of varicose veins (1,2). In
addition to the lower extremities, varicose veins can also appear
in the hemorrhoidal plexus, vulva, vagina and, less commonly, in
the cervix during pregnancy. The incidence of vulvar varicose veins
in pregnant women exhibited an increase, affecting up to 8% of all
pregnancies (3). The management of
severe vulvovaginal varices presents a challenge in everyday
obstetric practice, often requiring the collaboration of
radiologists, vascular surgeons and obstetrician-gynecologists
(4).
Cervical varices are a rare clinical finding during
pregnancy. To date, only 21 cases have been documented in the
international English-language literature (5). Cervical varices are dilated vascular
structures that can protrude through the dilated endocervical canal
to varying degrees. Their superficial position close to the
epithelium and their dilation, renders them anatomical weak points,
susceptible to rupture, thus potential causes of severe,
life-threatening bleeding during the antenatal period (5). Their pathogenetic mechanisms are not
yet fully understood; however, their incidence appears to be
associated with low placental implantation, an advanced maternal
age, twin pregnancies and exposure to diethylstilbestrol (5,6). Based
on data from the literature, cervical varices may be superficial or
originating from the endocervix, a feature that significantly
affects appearance during a physical examination and imaging
(7). Superficial, os-type varices
are more easily visualized during a speculum examination, as is the
detection of the precise site of bleeding in the case of rupture
(5,7). Internal, endocervix varices are usually
more difficult to detect via speculum examination, and are better
visualized via vaginal ultrasound and Doppler mode (5,7). However
they may also be visible via a speculum examination in the case of
multiple, highly enlarged varices that protrude from the external
os (such as in the case in the present study). Hemorrhagic
endocervical varices are rarely observed in the first trimester of
pregnancy. Cervical varices usually occur in the second or third
trimester of pregnancy and may be associated with fetal loss
following the termination of the pregnancy with a non-viable fetus
(as in the case in the present study) or with pre-term delivery
(6).
The present study describes a rare case of fetal
loss at 21 weeks of gestation due to severe bleeding from ruptured
cervical varices. The authors wish to emphasize the role of
transvaginal ultrasonography and transvaginal Doppler
ultrasonography in the early diagnosis of this condition, aiming to
reduce maternal and perinatal morbidity and mortality.
Additionally, the importance of differentiating bleeding caused by
cervical varices from vaginal bleeding associated with peripheral
placental abruption, particularly in cases complicated by placenta
previa is highlighted.
Case report
The present case report concerns a 26-year-old
primigravida who presented early in the morning to the Emergency
Department of the General Hospital of Trikala, Trikala, Greece, at
21 weeks of gestation, reporting an episode of major vaginal
bleeding at ~1 h prior. The pregnant woman described the bleeding
as heavy, with large blood clots. Her hemodynamic status was
stable, with a blood pressure of 110/70 mmHg and a heart rate of 84
beats per minute, indicating tolerable blood loss severity and
allowing for the performance of all necessary investigations. The
vaginal hemorrhage was not accompanied by pain. The patient had
been followed-up at a private obstetric center, where a low-lying
placenta (placenta previa) was identified via ultrasound during the
first trimester. Nuchal translucency was measured at 1.2 mm, and no
fetal anatomical abnormalities were detected. A previous minor
vaginal hemorrhage (first episode) was reported ~1 month earlier.
According to the patient, the bleeding, attributed by her
obstetrician to peripheral abruption of the placenta previa,
resolved within 1 week following bed rest and oral progesterone
administration. An investigation of her medical history did not
reveal any notable findings, and no evidence of exposure to
diethylstilbestrol was found. This was a singleton pregnancy,
resulting from spontaneous conception.
Upon a gynecological vaginal examination, a large
amount of vaginal bleeding was observed, which obscured a clear
view of the cervix during the examination. An obstetric ultrasound
revealed a normal fetal heart rate, with the amount of amniotic
fluid within normal limits. The placenta was located in an anterior
low position, with no obvious signs of abruption on the ultrasound.
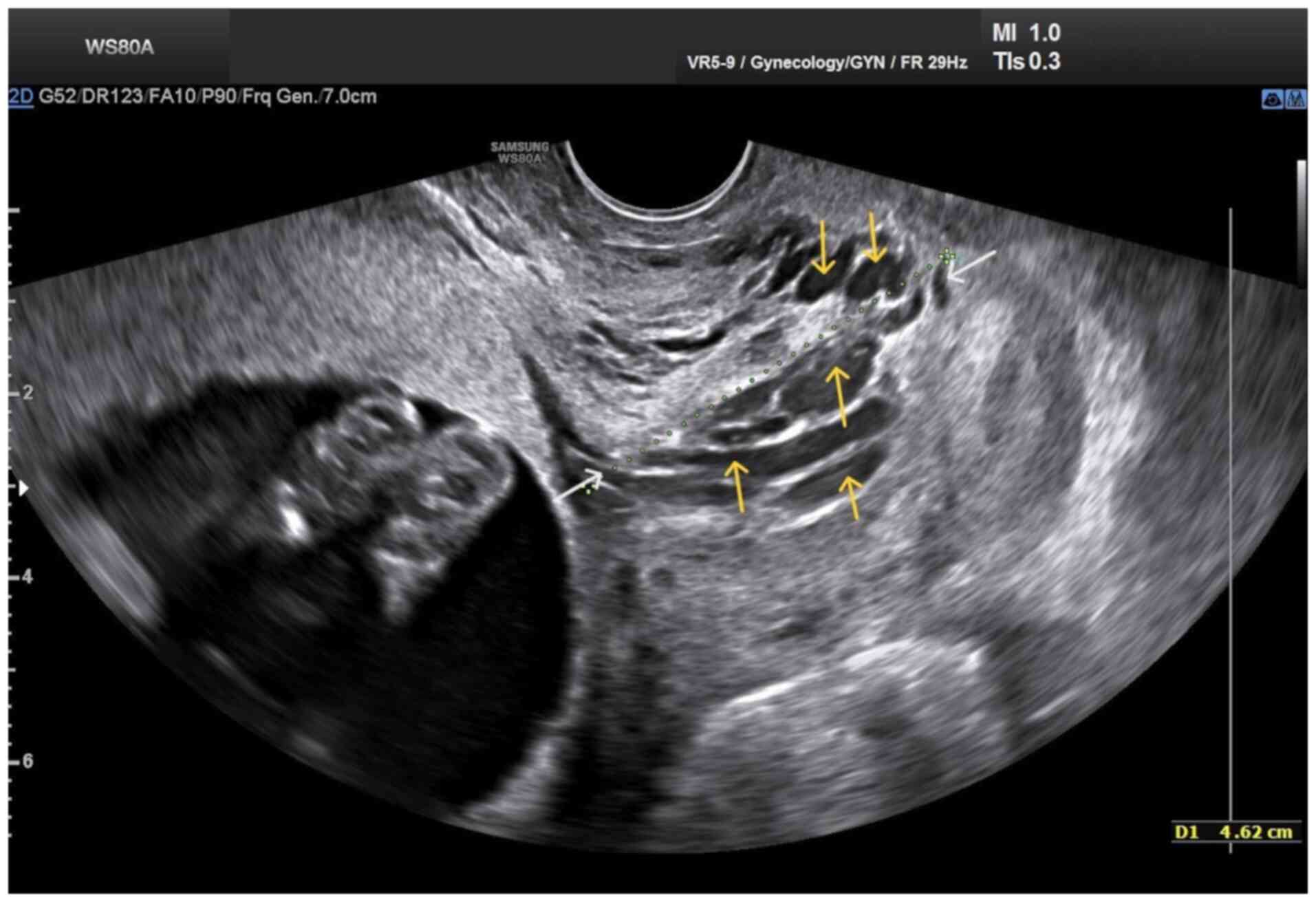
The transvaginal ultrasound revealed a normal cervical length of 46
mm. However, the imaging revealed dilated, elongated structures
protruding through the dilated endocervical canal, which were
characteristic (Fig. 1). A
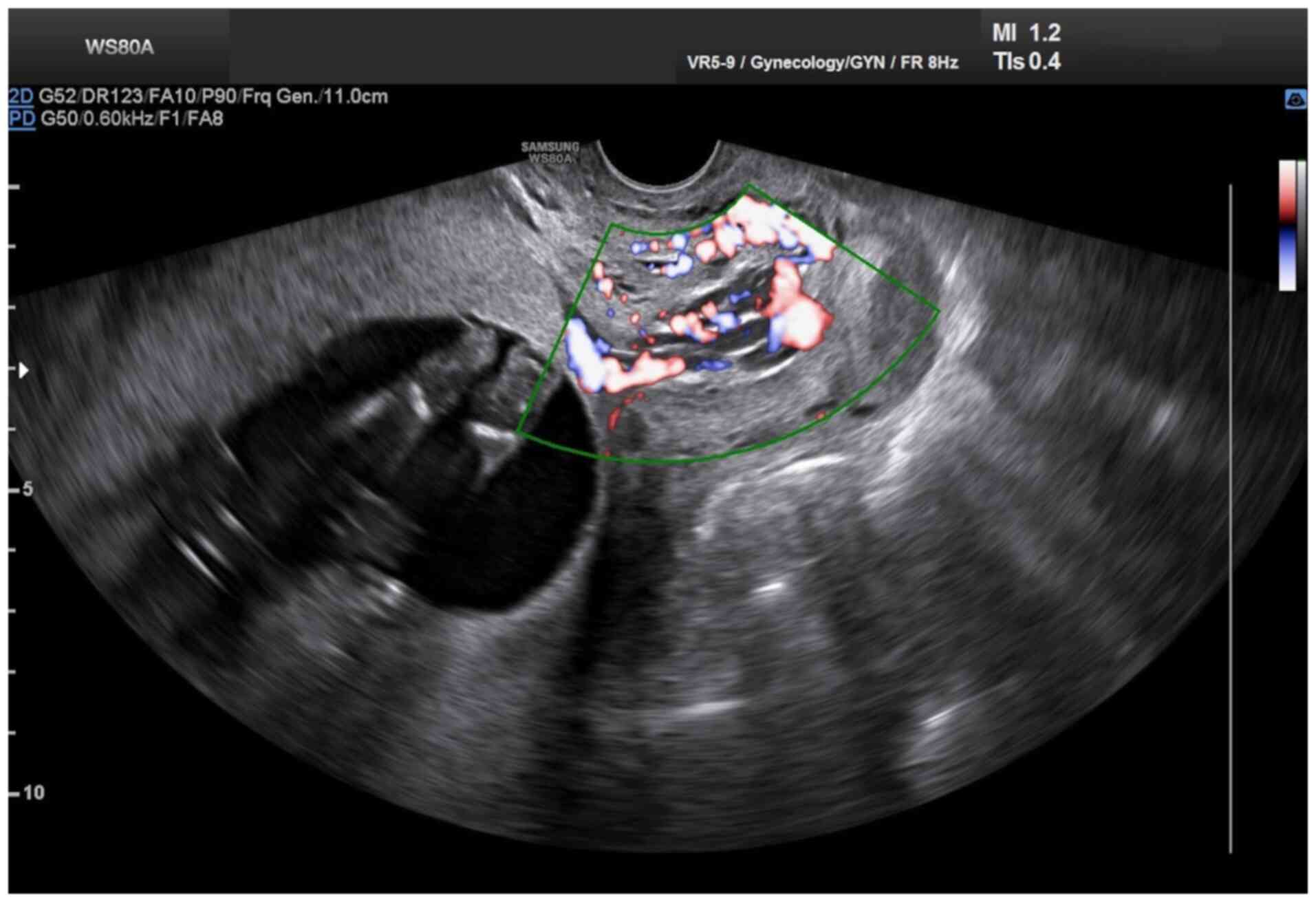
transvaginal Doppler ultrasound of the endocervix demonstrated
dilated, elongated longitudinal structures with increased
vascularization, involving the majority of the cervix. These
findings were consistent with dilated vascular structures (Fig. 2). Due to the ongoing vaginal bleeding
following the admission of the patient to the clinic, a more
thorough vaginal examination was performed under general anesthesia
in the operating room. The operating theatre was adequately
prepared for the possibility of pregnancy termination via
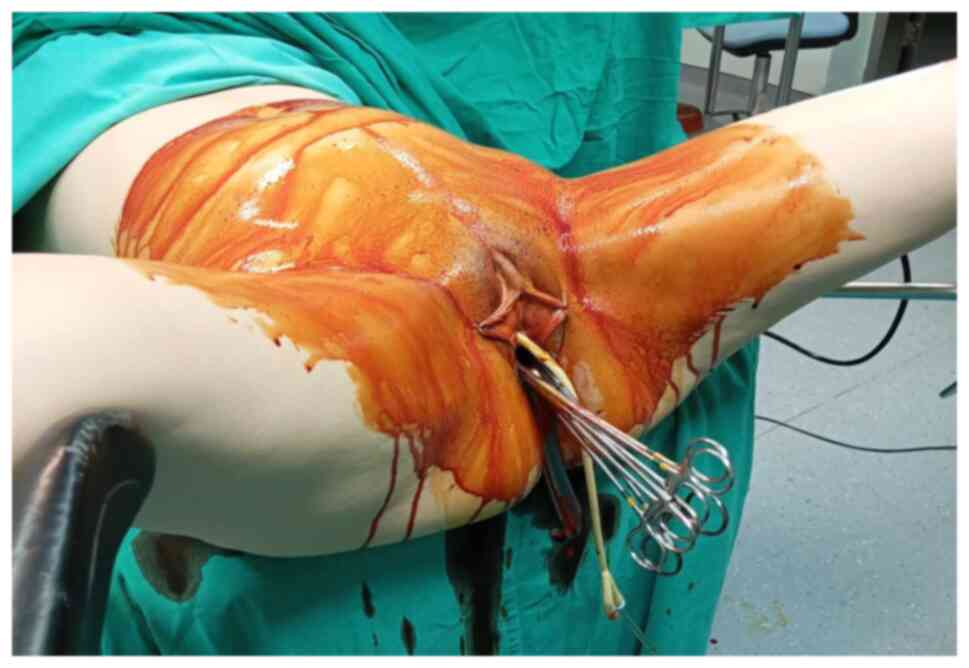
laparotomy in the event of a major hemorrhage. A careful inspection
of the cervix revealed enlarged varicose-like vessels projecting
through the cervical canal up to the external cervical os, which
were actively bleeding (Fig. 3).
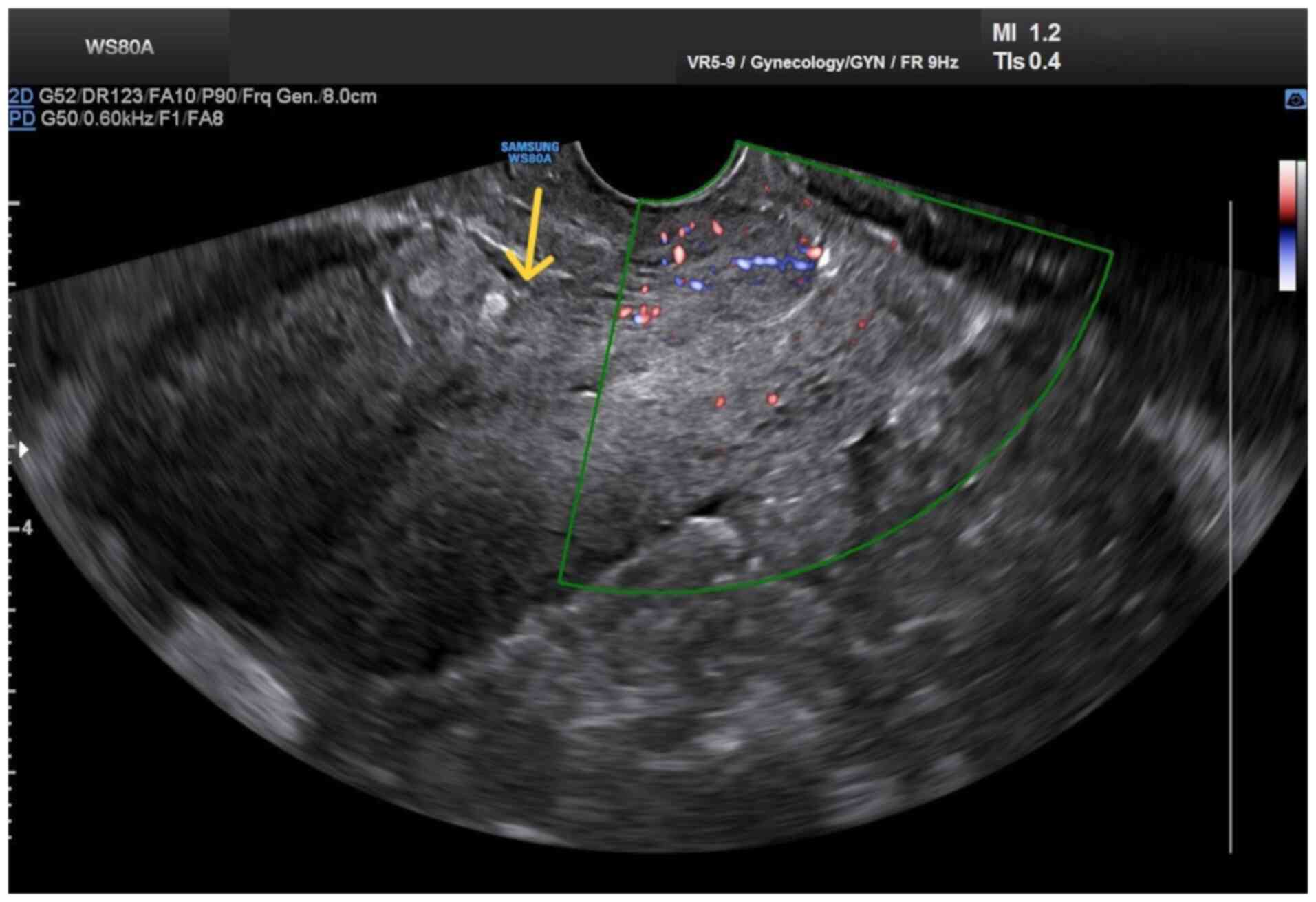
During an attempt to palpate the vascular structures in the cervix,
profuse vaginal bleeding was triggered. To manage the bleeding
temporarily, several hemostatic forceps were applied (Fig. 4).
With the patient in the gynecological laparoscopy
position, an emergency cesarean section was performed. The
umbilical vessels were clipped and the fetus was delivered and
subsequently handed to the neonatologist for assessment, who
unfortunately confirmed its demise shortly thereafter. The placenta
was removed, without any evidence of placenta accreta spectrum
disorder or vascular malformations in the lower uterine segment
near the internal cervical os being observed. However, severe
intraoperative bleeding necessitated the decision to perform a
utero-cervico-vaginal tamponade with gauze packing, along with the
transfusion of 3 units of packed red blood cells and 1 unit of
fresh frozen plasma. Prior to the tamponade, the previously placed
hemostatic forceps were removed. Immediately post-operatively, the
dilated vessels in the endocervix were no longer visible, and no
active bleeding was observed during inspection. For post-operative
hemodynamic stabilization (Table I),
an additional transfusion of 3 units of packed red blood cells was
required. The utero-cervico-vaginal gauze tamponade was removed on
the first post-operative day. Antibiotic treatment was initiated,
with cefuroxime (Mefoxil) administered at a dose of 2 g every 8 h
for 4 days, combined with metronidazole (Flagyl) at 500 mg every 8
h for 2 days. The patient was discharged from the clinic on the 5th
post-operative day. At 20 days thereafter, both the clinical
cervical examination findings (Fig.
5) and transvaginal Doppler ultrasound findings (Fig. 6) were normal. Since then, all
subsequent follow-up assessments have been performed at the private
obstetric center the patient attended before her presentation to
our hospital. At the time of writing the patient is healthy,
without bleeding and has not yet made another attempt at conception
and pregnancy.
 | Table IPre-operative and post-operative
laboratory tests of the patient during her hospitalization at the
clinic. |
Table I
Pre-operative and post-operative
laboratory tests of the patient during her hospitalization at the
clinic.
| Laboratory tests | Pre-operatively | At 6 h after
surgery | 1st post-operative
day | 2nd post-operative
day | 4th post-operative
day | Normal laboratory
values |
|---|
| Ht | 26.6%a,b | 20.8%c | 18.2%d | 25.4% | 25.4% | 37.7-49.7% |
| Hb | 9.7 g/dl | 7.6 g/dl | 6.7 g/dl | 9.2 g/dl | 8.6 g/dl | 11.8-17.8 g/dl |
| WBC |
9.1x103/ml |
16.1x103/ml |
14.4x103/ml |
13.89x103/ml |
7.51x103/ml |
4-10.8x103/ml |
| NEUT | 83.2% | 87.3% | 86.8% | 78.7% | 62.1% | 40-75% |
| PLT |
205x103/ml |
121x103/ml |
107x103/ml |
135x103/ml |
186x103/ml |
150-350x103/ml |
| CRP | 0.06 mg/dl | 0.3 mg/dl | 5.55 mg/dl | 14.55 mg/dl | 2.17 mg/dl | <0.5 mg/dl |
| APTT | 29.8 sec | 27.8 sec | 35.3 sec | 31 sec | 31 sec | 24.0-35.0 sec |
| INR | 0.89 | 0.97 | 1.04 | 1.02 | 1.02 | 0.8-1.2 |
| FIB | 286 mg/dl | 232 mg/dl | 237 mg/dl | 422 mg/dl | 385 mg/dl | 200-400 mg/dl |
| Glu | 76 mg/dl | 133 mg/dl | 69 mg/dl | 81 mg/dl | 90 mg/dl | 75-115 mg/dl |
| U | 30 mg/dl | 29 mg/dl | 22 mg/dl | 25 mg/dl | 24 mg/dl | 10-50 mg/dl |
| Cr | 0.6 mg/dl | 0.6 mg/dl | 0.46 mg/dl | 0.51 mg/dl | 0.49 mg/dl | 0.40-1.10 mg/dl |
| K+ | 4.17 mmol/l | 4.1 mmol/l | 3.24 mmol/l | 3.51 mmol/l | 3.49 mmol/l | 3.5-5.1 mmol/l |
| Na+ | 135 mmol/l | 133 mmol/l | 140.5 mmol/l | 139 mmol/l | 141.7 mmol/l | 136-145 mmol/l |
| B | 0.5 mg/dl | 0.92 mg/dl | 0.48 mg/dl | | | 0.3-1.2 mg/dl |
| SGOT | 28 IU/l | 27 IU/l | 17 IU/l | | | 5-33 IU/l |
| SGPT | 13 IU/l | 14 IU/l | 11 IU/l | | | 10-37 IU/l |
Discussion
The pathogenesis of cervical varices in pregnant
women has not been fully elucidated. Placenta previa is thought to
be the main risk factor. Placenta previa, along with the increased
cervical blood flow that characterizes such cases, appears to be
significantly associated with the development of venous distension
and varices in the area (7). In
addition, prenatal maternal exposure to diethylstilbestrol, which
can cause vascular malformations in the pelvic organs, has been
implicated in the development of cervical varicose veins. Moreover,
the interaction between the uterus and placenta in women exposed to
diethylstilbestrol is well known (8). Furthermore, in vitro
fertilization, the multiple pregnancies frequently resulting from
it, and a maternal age >35 years, which often characterizes
these pregnant women, are additional risk factors for cervical
varices (9). In rare cases, the
development of cervical varices in pregnancy may occur in the
absence of these risk factors (10).
The patient in the present study was 26 years of age and carried a
singleton pregnancy following spontaneous conception. No evidence
suggesting exposure to diethylstilbestrol at the time of the case
was found. In the patient described herein, the only predisposing
risk factor for the development of cervical varices was a low-lying
placenta.
The prenatal diagnosis of cervical varices is based
on a clinical examination, transvaginal ultrasound and magnetic
resonance imaging. The recognition of the clinical features of
cervical varices during pregnancy is of utmost importance for the
accurate diagnosis of this rare clinical entity before major
bleeding occurs due to rupture (11). Bleeding is the predominant symptom
and usually indicates rupture of the cervical varices (12). It is crucial to avoid confusion with
vaginal hemorrhage due to peripheral abruption of a placenta
previa, which often accompanies cervical varices (5). Additionally, the differentiation
between bleeding caused by the rupture of cervical varices and that
caused by vasa previa is of great diagnostic value. Vasa previa
originate from the placenta, whereas cervical varices are of
maternal origin and are not necessarily related to the placenta
(12). A gynecological clinical
examination with careful cervical inspection is thought to be of
considerable help in the diagnosis of cervical varices. However,
unlike transvaginal ultrasound and magnetic resonance imaging, it
is unable to accurately assess the origin, nature, and extent of
cervical varices (12).
Transvaginal ultrasound easily detects the presence
of a placenta previa, which often accompanies cervical varices in
pregnant women. At the same time, it can identify a hypoechoic
structure in the endocervix, which, when examined by Doppler
transvaginal ultrasound, suggests a vascular origin (13). Magnetic resonance imaging, although
not readily available for every pregnant woman with bleeding, is
considered very valuable for accurately visualizing the vessel
distribution in relation to adjacent organs and for excluding other
unforeseen pelvic pathological conditions prior to a planned
cesarean section (12). In the
patient in the present study, the presence of placenta previa and
the onset of a small vaginal hemorrhage in the late first trimester
initially raised the suspicion of possible peripheral placental
abruption. The diagnosis of cervical varices was established by
transvaginal Doppler ultrasonography and a detailed vaginal
examination under anesthesia after the incident of severe vaginal
bleeding in the second trimester. Upon a cervical examination, a
mass of dilated longitudinal vessels with a variceal configuration
was found, originating from the endocervix and protruding up to the
external cervical os, extending mainly toward the posterior
cervical margin (Fig. 3).
Scientific evidence supporting the optimal
management of bleeding caused by cervical varices in pregnancy is
still lacking. The limitation of physical activity, bed rest,
avoidance of sexual intercourse and blood transfusions in cases
where bleeding is accompanied by symptoms of anemia, such as
weakness, orthostatic hypotension, dizziness, or dyspnea are common
conservative therapeutic interventions (12). Additionally, the application of a
cervical pessary is another conservative option to control bleeding
associated with cervical varices during pregnancy. It is believed
that the pressure exerted by the pessary on the cervical tissues
may reduce the width of the varices, thus decreasing the bleeding
caused by their rupture (14).
Furthermore, cervical cerclage can be successfully applied to treat
cervical varicose veins in pregnant women and can lead to a
successful full-term pregnancy, even when applied in cases of
active bleeding from the rupture of cervical varices, as performed
by Poliektov and Kahn (5). The case
described herein differs in the fact that there was no time to
perform conservative measures, since massive bleeding was triggered
only by the attempt to examine the cervix. It is very likely that
any operative maneuvers in the area, such as cervical cerclage,
would also trigger massive bleeding. In cases where a decision is
made to terminate the pregnancy in the first or second trimester,
prophylactic embolization of the uterine artery is considered to
markedly reduce the risk of bleeding from cervical varices, such as
the case described by Lesko et al (15). In the patient in the present study,
the decision to terminate the pregnancy was an emergency medical
option due to massive vaginal bleeding caused by palpation of the
cervical varices. The severe vaginal bleeding in the case in the
present study left no room for consideration of conservative
methods for managing cervical varices, which may have allowed for
the continuation of the pregnancy and its termination by planned
cesarean section or vaginal delivery. The management course used
herein is similar to the one followed in the study by Kumazawa
et al (16), who managed
their case by mechanical pressure of the bleeding varices via
vaginal packing. In their case, mechanical pressure was effective
in stopping the bleeding and prolonging pregnancy for a few more
days, with emergency caesarean section being ultimately performed
(16), similar to the case described
herein. However, the case in the present study differs, as it
demonstrates a more clinically challenging scenario, whereby the
bleeding from varicose veins could not be controlled via mechanical
pressure, leading to the performance of emergency caesarean section
earlier during gestation and allowing no margins to attempt other
conservative treatment options to control the bleeding.
A planned cesarean section is still the preferred
mode of delivery for pregnant women with cervical varices. A
planned cesarean section avoids the rupture of cervical varices and
the triggering of massive vaginal bleeding that can occur during
vaginal delivery (17). A planned
vaginal delivery may be appropriate in isolated cases of cervical
varices, in which the varices may resolve simultaneously with the
separation of a coexisting placenta previa (6,18).
Emergency cesarean section, either associated with or without
emergency hysterectomy, is indicated in cases of massive,
uncontrolled bleeding and is associated with significantly
increased rates of maternal and perinatal morbidity and mortality
(19).
The prognosis is favorable in asymptomatic pregnant
women without bleeding from ruptured cervical varices. Following
the delivery of the fetus, cervical varices resolve spontaneously,
and the risk of recurrence is considered to be low (12). In cases where the rupture of cervical
varices occurs, the bleeding is severe and life-threatening for
both the pregnant woman and the newborn (20). In the patient described herein, the
profuse vaginal bleeding caused by rupture of the cervical varices
resulted in the loss of the fetus after the pregnancy was
terminated by performing a cesarean section. In both the immediate
and late post-operative periods, the findings from clinical
examination and transvaginal Doppler ultrasonography were
normal.
The primary strength of the present case report is
its rarity in the clinical setting, thus its addition to the
literature provides further insight into a lesser known clinical
entity and its management. However, there are limitations that need
to be acknowledged. Namely, the availability of only a single case
somewhat limits the generalizability and applicability of our
findings and conclusions in different clinical settings. Finally,
the absence of long-term follow-up, particularly up to a second
pregnancy and the exploration of recurrence is an additional
limitation that should be acknowledged. The individualization of
diagnostic and treatment approach based on the circumstances of
each patient and the available resources and expertise at hand is
key in achieving the most favorable outcomes.
In conclusion, cervical varices are an extremely
rare clinical entity. The rupture of cervical varices, leading to
massive vaginal bleeding in the second trimester of pregnancy,
often necessitates the termination of the pregnancy via cesarean
section. Cervical varices, particularly when associated with
placenta previa, should be considered in the differential diagnosis
of painless vaginal bleeding in pregnant women. The careful and
skilled use of transvaginal Doppler ultrasonography is deemed to be
invaluable for the early and accurate diagnosis of cervical
varices. Early detection can prevent unnecessary diagnostic
procedures, such as the digital palpation of the cervix, which may
otherwise result in variceal rupture, severe hemorrhage and fetal
loss.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data used in the current study are available
from the corresponding author upon reasonable request.
Authors' contributions
AT and ET participated in the conception and design
of the study and international literature search. IRA and AL were
involved in the conception and design of the study, in the
provision of study materials (such as blood tests, culture test and
imaging) or patient data, in data collection and aggregation and
data analysis and interpretation. IT was involved in the conception
and design of the study, in administrative support, in patient
care, in data collection, in manuscript writing and analysis and
had overall supervision of the manuscript. All authors participated
in the writing of the manuscript, contributed to the revision of
the manuscript, and have read and approved the final version of the
manuscript. All authors (AT, ET, IRA, AL and IT) confirm the
authenticity of all raw data.
Ethics approval and consent to
participate
The present study was conducted according to the
guidelines of the Declaration of Helsinki. Written informed consent
was obtained from the patient.
Patient consent for publication
The patient in the present study provided signed
consent for the publication of her medical case anonymously and any
related images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Raetz J, Wilson M and Collins K: Varicose
veins: Diagnosis and treatment. Am Fam Physician. 99:682–688.
2019.PubMed/NCBI
|
|
2
|
Ismail L, Normahani P, Standfield NJ and
Jaffer U: A systematic review and meta-analysis of the risk for
development of varicose veins in women with a history of pregnancy.
J Vasc Surg Venous Lymphat Disord. 4:518–524.e1. 2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Gavrilov SG: Vulvar varicosities:
Diagnosis, treatment, and prevention. Int J Womens Health.
9:463–475. 2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Giannella L, Montanari M, Delli Carpini G,
Di Giuseppe J and Ciavattini A: Huge vulvar varicosities in
pregnancy: Case report and systematic review. J Int Med Res.
50(3000605221097764)2022.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Poliektov N and Kahn BF: Bleeding cervical
varices in pregnancy: A case report and review of the literature. J
Neonatal Perinatal Med. 15:195–202. 2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Wax JR, Cartin A, Litton C, Conroy K and
Pinette MG: Cervical varices: An unusual source of first-trimester
hemorrhage. J Clin Ultrasound. 46:218–221. 2018.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Tanaka M, Matsuzaki S, Kumasawa K, Suzuki
Y, Endo M and Kimura T: Cervical varix complicated by placenta
previa: A case report and literature review. J Obstet Gynaecol Res.
42:883–889. 2016.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Thorp JM Jr, Fowler WC, Donehoo R, Sawicki
C and Bowes WA Jr: Antepartum and intrapartum events in women
exposed in utero to diethylstilbestrol. Obstet Gynecol. 76:828–832.
1990.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Yoshimura K, Hirsch E, Kitano R and
Kashimura M: Cervical varix accompanied by placenta previa in twin
pregnancy. J Obstet Gynaecol Res. 30:323–325. 2004.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Youssef J, Afolayan V, Mack M and Sze A:
Cervical varicosities, an uncommon cause of third-trimester
bleeding in pregnancy: A case report. Case Rep Womens Health.
38(e00507)2023.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Kurihara Y, Tachibana D, Teramae M,
Matsumoto M, Terada H, Sumi T, Koyama M and Ishiko O: Pregnancy
complicated by cervical varix and low-lying placenta: A case
report. Jpn Clin Med. 4:21–24. 2013.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Peng MY, Ker CR, Lee YS, Ho MC and Chan
TF: Cervical varices unrelated to placenta previa as an unusual
cause of antepartum hemorrhage: A case report and literature
review. Taiwan J Obstet Gynecol. 57:755–759. 2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Kusanovic JP, Soto E, Espinoza J, Stites
S, Gonçalves LF, Santolaya J, Nien JK, Erez O, Sorokin Y and Romero
R: Cervical varix as a cause of vaginal bleeding during pregnancy:
Prenatal diagnosis by color Doppler ultrasonography. J Ultrasound
Med. 25:545–549. 2006.PubMed/NCBI View Article : Google Scholar
|
|
14
|
González-Bosquet E, Grau L,
Ferrero-Martínez S, Hernandez-Saborit A, Rebollo M, Gomez-Chiari M,
Martínez Crespo JM and Gómez-Roig MD: Pessary for management of
cervical varices complicating pregnancy. Obstet Gynecol.
138:482–486. 2021.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Lesko J, Carusi D, Shipp TD and Dutton C:
Uterine artery embolization of cervical varices before
second-trimester abortion. Obstet Gynecol. 123 (2 Suppl
2):S458–S462. 2014.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Kumazawa Y, Shimizu D, Hosoya N, Hirano H,
Ishiyama K and Tanaka T: Cervical varix with placenta previa
totalis. J Obstet Gynaecol Res. 33:536–538. 2007.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Sammour RN, Gonen R, Ohel G and Leibovitz
Z: Cervical varices complicated by thrombosis in pregnancy.
Ultrasound Obstet Gynecol. 37:614–616. 2011.PubMed/NCBI View
Article : Google Scholar
|
|
18
|
Wong CK, Hung CMW, Ng VKS, Yung WK, Leung
WC and Lau WL: Four cases of cervical varices without placenta
praevia: Presentation, diagnosis, managements, and literature
review. J Obstet Gynaecol Res. 48:1997–2004. 2022.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Saedi N, Ghaemi M, Moghadam M, Haddadi M,
Hashemi Z and Hantoushzadeh S: Emergency postpartum hysterectomy as
a consequence of cervical varix during pregnancy; a case report and
literature review. Int J Surg Case Rep. 108(108425)2023.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Park JE, Kim MJ, Kim MK and Kim HM:
Cervical varix with thrombosis diagnosed in the first trimester of
pregnancy. Obstet Gynecol Sci. 62:65–68. 2019.PubMed/NCBI View Article : Google Scholar
|