Introduction
Darier disease is a rare, often misdiagnosed genetic
disorder inherited in an autosomal dominant pattern. It was
initially described by Darier and White in 1889. Sporadic cases are
estimated to occur in approximately half of the instances, with the
condition exhibiting high penetrance, >95%. Darier disease
typically begins in childhood and continues into adolescence,
leading to the formation of small papules, primarily in the
seborrheic regions, including the scalp, the areas behind the ears
and temples, the back of the neck, the front of the torso and skin
folds. Additionally, the involvement of the palms, soles, nails and
mucous membranes may occur. Over time, these areas may become
covered with scales and yellowish or brown crusts characterized by
hyperkeratosis. The papules do not always develop within hair
follicles, but frequently cluster together, forming wart-like
lesions covered with keratotic crusts. Nonetheless, there are
instances where symptoms may not appear until the sixth or seventh
decade of life, with localized Darier disease being a clinical
variant that was first identified by Kreibich in 1906 (1-3).
A mutation in the ATPase sarcoplasmic/endoplasmic
reticulum Ca2+ transporting 2 (ATP2A2) gene located on
chromosome 12q23-24 is attributed to the pathogenesis of Darier
disease due to a malfunction of the endoplasmic reticulum
Ca²+ ATPase pump. This malfunction leads to defective
calcium storage within the aforementioned organelle. Consequently,
this disruption impairs the normal processing of junctional
proteins, such as desmoplakins, leading to acantholysis (4).
The present study describes a sporadic case of
Darier disease localized only to the breast. The validity of the
references in the present case report was confirmed, and the case
report was written according to CaReL guidelines (5,6).
Case report
Patient information
A 35-year-old female sought medical attention at
Smart Health Tower, Ranya, Iraq on August 14, 2024, due to a right
nipple lesion that had persisted for approximately one month. She
delivered two children via cesarean section, both of whom were
breastfed for a combined duration of 3 years and 2 months. Her past
medical history was unremarkable, apart from a family history of
lung cancer in her paternal aunt.
Clinical findings
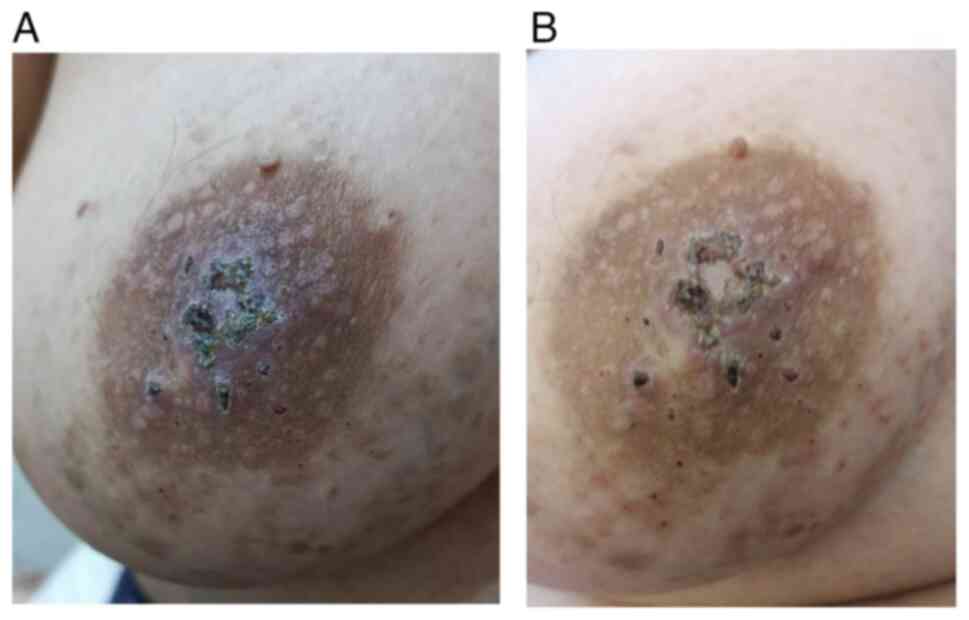
There were multiple small brown to black firm nipple
lesions causing nipple destruction, associated with multiple small
red, non-tender skin lesions in the areolar region and the lower
part of the breast (Fig. 1).
Diagnostic approach
The breast ultrasound revealed homogenous background
echotexture with a fibroglandular pattern, normal morphology, and
no solid masses or distortion in either breast. The breasts had
normal skin thickness and contours, and non-specific axillary lymph
nodes were observed. The right nipple was not visible and the
ulcerated areola complex was suggestive of nipple adenoma. Tissue
diagnosis was obtained from the right nipple lesion by incisional
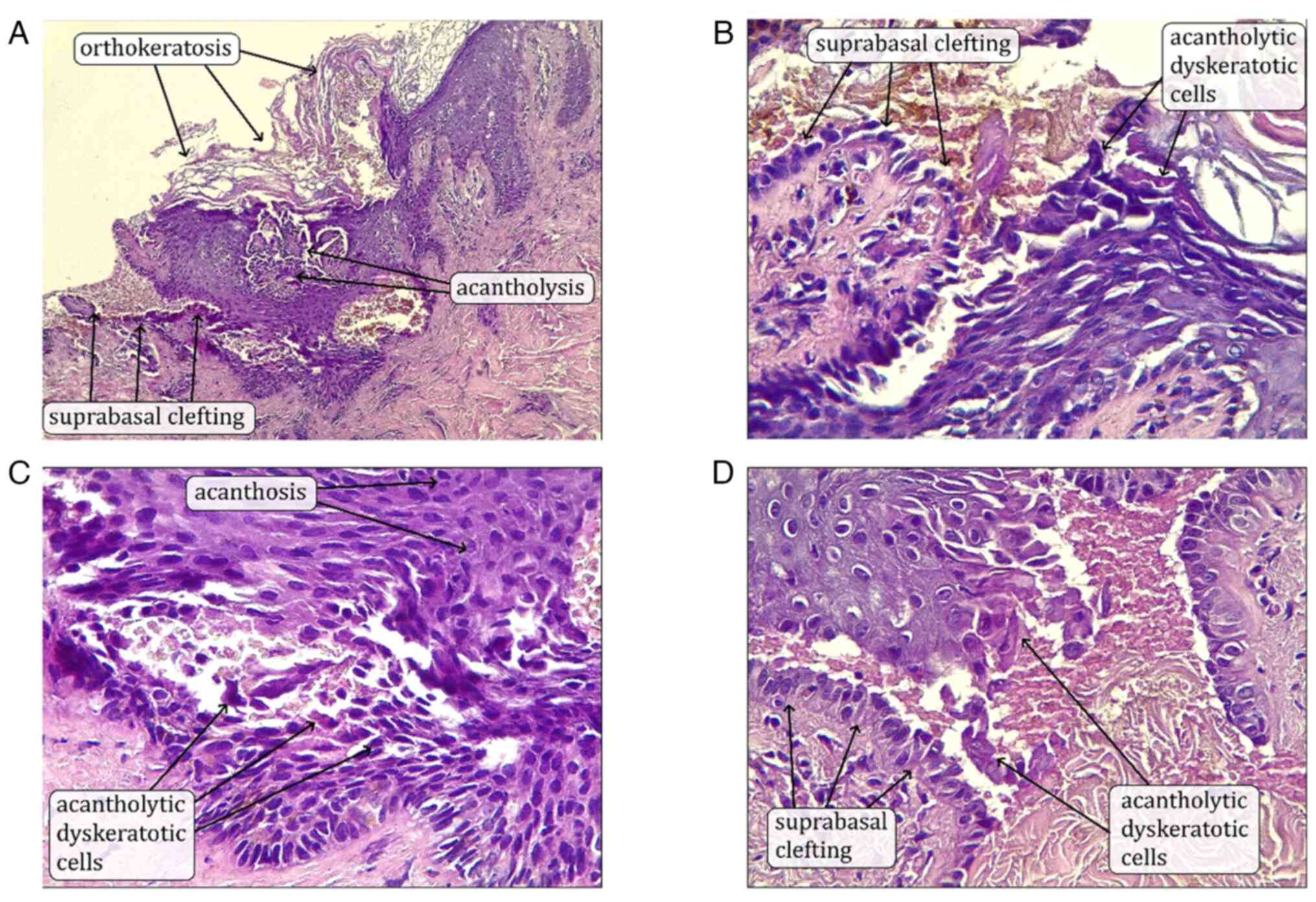
biopsy. The histopathological examination was performed in the
following manner; The sections used were paraffin-embedded and
sectioned to a thickness of 5 µm. Fixation was performed using 10%
neutral-buffered formalin at room temperature for 24 h. Hematoxylin
and eosin (H&E) staining (from Bio Optica) was used with
hematoxylin staining carried out for 5 min and eosin staining for 2
min, both at room temperature. The slides were observed and imaged
using a light microscope (Leica Microsystems GmbH). The results
revealed a small amount of acantholytic cells and papillary-like
configuration within the epidermis; no conclusive evidence of
malignancy was observed, and a diagnosis of Darier disease
localized to the breast was made (Fig.
2). The patient was advised to undergo ATP2A2 gene analysis to
support the diagnosis; however, the test was not performed.
Therapeutic intervention
The patient was administered high-dose oral Costus
medication to reduce inflammation at a dose of three capsules (each
containing 250 mg Costus extract) taken twice daily, totaling 1,500
mg per day. This treatment was maintained for a period of 6 months,
after which the dose was gradually tapered based on the clinical
response and tolerance of the patient. Her dermatologist
recommended emollient lotion to relax and hydrate her skin, topical
fusidic acid cream 2% to control and prevent further skin
infection, and oral isotretinoin 20 mg once daily to minimize
hyperkeratosis and smoothen papules. The patient was instructed to
wear sunscreen and avoid sun exposure. For monitoring clinical
improvement, follow-up appointments were planned on a regular
schedule.
Follow-up
The patient is still undergoing regular checkups and
is in good health without any health issues. Although routine
baseline and follow-up laboratory tests, including liver function
tests (LFTs) and lipid profile were recommended, the patient
declined to proceed with these investigations. Following 3 months
of isotretinoin use, the medication was gradually tapered and
discontinued due to the desire of the patient to conceive in the
following 6 months. Furthermore, the teratogenic risks associated
with the use of isotretinoin were clearly explained, and
appropriate pregnancy prevention counseling was provided.
Currently, the condition of the patient remains stable, with no
signs of progression or new complications.
Discussion
Darier disease is a hereditary condition
characterized by abnormal keratinization of the skin. Apart from
skin manifestations, it may also manifest with non-dermal symptoms,
including psychiatric conditions, such as intellectual disability,
epilepsy, or bipolar disorder (1).
However, the patient in the present study did not complain of any
psychiatric issues, and there were no such complaints in the review
of the literature as regards localized drier disease, apart from a
5-year-old female with Darier disease localized to the vulva;
however, it is worth mentioning that the epilepsy and mental
impairment she was suffering from were attributed to a
cardiopulmonary arrest event earlier in her life rather than Darier
disease itself (7). The outcomes of
localized Darier disease across the referenced studies were
generally favorable with either complete resolution or significant
improvement, particularly when appropriate topical treatments were
applied. However, one case did report relapse following treatment
discontinuation (Table I) (2,3,7-9).
This can be explained by the proposed pathogenesis of localized
Darrier disease, which is due to genetic mosaicism, as previously
mentioned by Takagi et al (1); these mutations arise during zygotic
division. It presents as a rash with either macular or linear
patterns, confined to a specific body area, resembling an epidermal
nevus distribution (1). Only a
limited number of confirmed cases of localized Darier disease have
been reported, at least to the best of our knowledge. For instance,
Fitzgerald and Lewis-Jones (2)
reported the case of a 59-year-old female patient who presented
with plaque over each areola consisting of numerous crusted,
brownish papules, which were confirmed as Darier disease on
histopathological examination. When it is confined to the areola
with no other parts of the body affected, it can easily be
misdiagnosed, as was the case with the patient in the present
study; this was only diagnosed following a histopathological
examination. The opposite was reported by Spizuoco et al
(4), where a patient presented with
widespread, merging, keratotic, crusted, and papular lesions
located in the scalp, forehead, back and chest, in addition to her
left nipple being affected. She was diagnosed with Darier disease;
however, later on, a biopsy of the nipple lesion revealed
confirmatory findings of Paget's disease, necessitating a detailed
approach and considering possible differential diagnosis (4). The other differentials include
Hailey-Hailey disease, Paget's disease, Seborrheic dermatitis,
epidermodysplasia verruciformis and acanthosis nigricans
necessitating histopathological examination for confirming query
cases, which shows the stratum corneum with disorganized
hyperproliferation and keratotic plug formation, accompanied by the
presence of parakeratosis. In regions where suprabasal cleavage
occurs, there is a notable presence of acantholytic cells along
with atypical keratinocytes, which manifest as corps ronds and
grains. These pathological features are distributed throughout the
affected tissue, reflecting disruptions in cellular adhesion and
differentiation (1). The case in the
present study underwent breast ultrasound to detect any underlying
mass or tumor, as it is important to exclude breast cancer in such
cases as breast cancer is one of the leading causes of mortality
and morbidity worldwide (10).
 | Table ICharacteristics of the patients with
localized Darier disease identified in the literature. |
Table I
Characteristics of the patients with
localized Darier disease identified in the literature.
| First author, year of
publication | No. of patients | Sex | Age (years) | Family history of
Darier disease | Localization | Presentation | Comorbidities | Treatment | Outcome | Follow-up
(months) | (Refs.) |
|---|
| Fitzgerald, 1997 | 1 | F | 59 | No | Both breasts | Plaque over each
areola consisting of numerous crusted, brownish papules. | Asthma, angina,
hypothyroidism and cervical spondylosis | - | Significant
improvement, but appearance of multiple small palmar pits and
V-shaped notching of the distal ends of several of the nails | Unspecified | (2) |
| Salopek, 1993 | 1 | F | 5 | No | Vulva | Red-brown, 1-2-mm
papules coalesced to form confluent plaques over the vulvar and
perivulvar skin in a bilateral, symmetric distribution. The surface
of the papules was rough and somewhat warty, with a few lesions
revealing superficial erosions. In the left groin was an ulcerated,
crusted papule. | Mentally impaired and
suffered from epilepsy secondary to aspiration-induced
cardiopulmonary arrest at age ten months | Antifungals for
possible candidiasis, and corticosteroids for diaper dermatitis,
without much success. Barrier cream was lastly used. | Spontaneous
resolution | 3 | (7) |
| Barrett, 1989 | 1 | F | 43 | No | Vulva | Pruritic lesion. | - | Mild corticosteroid
cream | Complete
resolution | 3 | (8) |
| Linder, 2016 | 1 | F | 71 | No | Inframammary and
presternal area | Several symmetrically
distributed, small, very itchy, partly excoriated red papules
surrounded by an erythematous halo. The lesions were 4-8 mm in
diameter. | - | Daily 0.1% adapalene
cream | Complete
resolution | Unspecified | (3) |
| O'Malley, 1997 | 4 | M | 21 | No | Right side of the
chest | Asymptomatic linear
group of yellow-brown keratotic papules for five years. | - | No treatment
received | - | - | (9) |
| | | M | 37 | No | Left side of the
abdomen | Linear group of
discrete, warty, brown papules. | - | 0.1% tretinoin
cream | Complete
resolution | 4 | |
| | | M | 36 | No | Right axilla | Brown, keratotic
papules anteriorly and a macerated, vegetative, erythematous
plaque. | - | - | - | - | |
| | | F | 35 | No | Posterior aspect of
right leg, right arm and the right side of trunk. | Rough, yellowish
papules . | - | A 2-year course of
treatment with a combination of vitamin A cream and betamethasone
valerate | The eruption cleared,
but it gradually returned after the treatment was discontinued | 24 | |
Currently, no validated curative treatments exist;
the majority of cases are managed symptomatically. Providing
lifestyle guidance is crucial in mitigating exacerbating factors,
including high humidity, elevated temperatures, excessive sweating,
mechanical irritation, exposure to ultraviolet rays, pregnancy,
childbirth, and surgical interventions. In the present case, 20 mg
of daily isotretinoin was used, which is frequently employed in
treating Darier disease and is highly effective. However, the use
of this drug is associated with several side-effects; thus, a
number of patients undergo only intermittent therapy or, in some
cases, discontinue treatment altogether, particularly for females
wishing to conceive (1).
Additionally, in vitro studies have
demonstrated that treating cultured keratinocytes with the three
medications prednisolone, cyclosporine, and retinoids can alleviate
the suppression of ATP2A2 gene expression following ultraviolet
irradiation (1,11). This suggests the potential
therapeutic efficacy of these drugs in managing the condition.
However, in instances where Darier disease is localized, topical
options can offer fewer side-effects with similar outcomes; for
example, in their study, Linder et al (3) used 0.1% adapalene cream for Darier
disease localized to the inflammatory region, which resulted in
complete resolution of the skin lesions. Furthermore, O'Malley
et al (9) reported similar
results with topical tretinoin, resulting in a complete resolution
in 4 months involving the right axilla in one of their four cases.
In another case reported by Salopek et al (7), antifungal treatment and corticosteroids
were used without notable efficacy; however, later on, a barrier
cream resulted in a good outcome. Observation or treatment with
mild corticosteroid and barrier creams can be considered for
localized forms of Darier disease (1,3,7,9).
The present study had certain limitations which
should be mentioned. A limitation of the present study is the
unavailability of ultrasound images, laboratory tests (including
LFTs and lipid profile tests), ATP2A2 gene analysis, and other
supporting investigations to confirm the underlying cause of Darier
disease.
In conclusion, Darier disease may present as a
localized unilateral breast lesion, characterized by multiple
small, firm brown to black lesions on the nipple, leading to nipple
destruction.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
LRAP and AMS were the major contributors to the
conception of the study, as well as in the literature search for
related studies. HHF, DSH and FHK were involved in the literature
review, in the writing of the manuscript, and in the analysis and
interpretation of the patient's data. SLT, KKM, DAO and KAN were
involved in the literature review, in the design of the study, in
revision of the manuscript and in the processing of the figures.
LRAP, SLT and AMS were involved in treating and examining the
patient. LRAP and FHK confirm the authenticity of all the raw data.
All authors have read and approved the final manuscript.
Ethics approval and consent to
participate
The patient provided written informed consent to
participate and publish any related data in the present study.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the present case report and any
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Takagi A, Kamijo M and Ikeda S: Darier
disease. J Dermatol. 43:275–279. 2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Fitzgerald DA and Lewis-Jones MS: Darier's
disease presenting as isolated hyperkeratosis of the breasts. Br J
Dermatol. 136(290)1997.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Linder D, Marinello E, Donisi PM, Salmaso
R, Zattra E and Zampetti A: Inframammary dermatitis: A case of
localized late-onset Darier's disease. Case Rep Dermatol.
8:189–192. 2016.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Spizuoco A, Jain RD, Stockton T, Kessler
SE and Hamacher KL: Mammary Paget disease in Darier disease: Beware
the wolf in sheep's clothing. Am J Dermatopathol. 34:449–451.
2012.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Abdullah HO, Abdalla B, Kakamad FH, Ahmed
JO, Baba HO, Nasih M, Bapir R, Rahim HM, Omar D, Kakamad SH, et al:
Predatory publishing lists: A review on the ongoing battle against
fraudulent actions. Barw Med J. 2:26–30. 2024.
|
|
6
|
Prasad S, Nassar M, Azzam AY,
García-Muro-San José F, Jamee M, Sliman RK, Evola G, Mustafa A,
Abdullah HQ, Abdalla B, et al: CaReL guidelines: A Consensus-based
guideline on case reports and literature review (CaReL). Barw Med
J. 2:13–19. 2024.
|
|
7
|
Salopek TG, Krol A and Jimbow K: Case
report of Darier disease localized to the vulva in a 5-year-old
girl. Pediatr Dermatol. 10:146–148. 1993.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Barrett JF, Murray LA and MacDonald HN:
Darier's disease localized to the vulva. Case report. Br J Obstet
Gynaecol. 96:997–999. 1989.PubMed/NCBI View Article : Google Scholar
|
|
9
|
O'Malley MP, Haake A, Goldsmith L and Berg
D: Localized Darier disease: Implications for genetic studies. Arch
Dermatol. 133:1134–1138. 1997.PubMed/NCBI
|
|
10
|
Mingomataj E, Krasniqi M, Dedushi K,
Sergeevich KA, Kust D and Qadir AA: Cancer publications in one year
(2023): A Cross-sectional study. Barw Med J. 2:3–11. 2024.
|
|
11
|
Mayuzumi N, Ikeda S, Kawada H and Ogawa H:
Effects of drugs and anticytokine antibodies on expression of
ATP2A2 and ATP2C1 in cultured normal human keratinocytes. Br J
Dermatol. 152:920–924. 2005.PubMed/NCBI View Article : Google Scholar
|