Introduction
Achieving profound pulpal anaesthesia during
endodontic treatment, particularly in mandibular molars with
symptomatic irreversible pulpitis (SIP), remains a persistent
clinical challenge. Inferior alveolar nerve block (IANB), although
routinely employed, demonstrates a high failure rate in such cases,
with reported success rates ranging from 19 to 56% owing to the
heightened inflammatory state of the pulp (1,2).
Achieving effective anaesthesia in cases of SIP in
the mandibular molars, particularly with an IANB, is challenging
due to a combination of physiological and anatomical factors.
Severe inflammation in SIP releases mediators, such as
prostaglandins and bradykinin, which sensitize pulpal nociceptors,
lowering the pain threshold and causing hyperalgesia. This makes
the nerves hyper-responsive, reducing the efficacy of local
anaesthetics (3). Additionally, the
acidic environment in inflamed tissues lowers the pH level,
hindering the dissociation of anaesthetics, such as lidocaine, into
their active form, thus impairing nerve membrane penetration and
sodium channel blockade. Inflamed nerves may also express more
sodium channels, which further resisting anaesthesia (4). Anatomically, mandibular molars pose
challenges owing to potential accessory innervation from nerves,
such as the mylohyoid, lingual or long buccal nerves, which may not
be fully blocked by a standard IANB (3). Collectively, these factors make
profound anaesthesia difficult to achieve in patients with SIP.
Several strategies have been explored to improve
anaesthetic outcomes, including supplemental techniques
(intraosseous, intraligamentary and buccal infiltrations) and the
use of different anaesthetic agents or volumes (5). While a considerable success rate has
been documented for intraosseous injections, this technique not
only requires specialized apparatus, but also incurs significant
expenses and has the potential to inflict damage on root
structures, induce systemic complications, provoke pain and result
in post-injection discomfort (6).
Intrapulpal injections are associated with significant pain and
require pulp exposure (5).
Cryotherapy, a non-pharmacological modality
involving the application of cold, is a promising adjunctive
strategy. It induces local vasoconstriction, reduces oedema,
reduces nerve conduction velocity and elevates the pain threshold
through nociceptor desensitization (7). However, the potential risks associated
with cryotherapy, such as transient tissue sensitivity or
discomfort from cold application, should be considered, although
these are typically minimal with controlled application (7). Previous studies have demonstrated that
intraoral cryotherapy can improve the success rate of IANB, and
reduce intraoperative and post-operative pain during endodontic
procedures (7-10).
For instance, Gopakumar et al (11) evaluated the anaesthetic efficacy of
Endo-Ice spray and intrapulpal ice sticks as adjuncts to IANB in
patients with SIP, finding that both methods significantly reduced
pain and improved anaesthesia success, with ice packs exhibiting
superior outcomes. Moreover, mechanistic investigations have
demonstrated that cooling can suppress capsaicin-sensitive pain
receptors and modulate inflammatory pathways, offering a plausible
biological rationale for its analgesic effects in inflamed pulp
tissues (7,8).
Although previous studies have separately
investigated buccal ice packs or intrapulpal ice application as
adjuncts to IANB (9,10), the combined use of surface and
intrapulpal cryotherapy to maximize analgesic efficacy in patients
with SIP has not yet been explored in a single randomized
controlled trial (RCT), at least to the best of our knowledge. The
present study aimed to address this gap by evaluating the efficacy
of cryotherapy as a supplemental aid to IANB in patients with SIP
undergoing endodontic treatment, with the primary outcome being the
anaesthesia success rate (defined as no or mild pain during
treatment), and the secondary outcome being pain scores during
access opening and cleaning/shaping. By providing a non-invasive,
chairside approach to enhance anaesthesia and reduce pain,
cryotherapy holds significant clinical relevance for improving
patient comfort and procedural outcomes in endodontic practice,
particularly for challenging SIP cases. The null hypothesis was
that cryotherapy would not enhance IANB efficacy compared with
conventional IANB alone.
Patients and methods
Trial design
The present study was a single-centre,
parallel-group RCT with a 1:1 allocation conducted at the
Department of Conservative Dentistry and Endodontics, J N Kapoor
D.A.V. Dental College and Hospital, adhering to the Consolidated
Standards of Reporting Trials (CONSORT) guidelines 2025(12). The trial employed a 1:1 allocation
ratio, comparing two interventions: Group I (IANB with 2%
lignocaine alone) and group II (IANB with 2% lignocaine
supplemented with cryotherapy). The study period spanned from
April, 2023 to January, 2025. Ethical approval for the present
study was obtained from the Ethics Committee of J N Kapoor D.A.V.
Dental College and Hospital, Yamunanagar, India (F/EC/21/0018). The
study was conducted in strict accordance with the principles
outlined in the Declaration of Helsinki and in compliance with all
relevant guidelines and regulations governing human research
ethics. Each patient provided written informed consent prior to
participation. The trial was registered in the Clinical Trials
Registry of India CTRI/2023/03/050746 (https://ctri.nic.in/Clinicaltrials/pmaindet2.php?EncHid=ODEzMzU=&Enc=&userName=)
(Clinicaltrials.gov). Prior to the
commencement of patient recruitment, informed consent was obtained
from the patients following a detailed explanation of the
objectives of the study, as well as the procedures, risks and
benefits. No modifications were made following trial
registration.
Selection of participants
Eligibility criteria included patients aged 18-40
years with fully erupted mandibular first molars that exhibited
complete root development. The diagnosis of SIP was established
based on both clinical and diagnostic findings, consistent with the
American Association of Endodontists (AAE) guidelines (13). Clinically, patients presented with a
history of sharp, spontaneous pain, lingering thermal sensitivity
lasting >30 sec following cold stimulus, and referred pain.
Diagnostic confirmation was obtained using cold testing
(Endo-Frost, Coltene), in which a prolonged and exaggerated
response indicated pulpal inflammation. Additionally, all included
teeth exhibited positive responses to electric pulp testing (EPT),
confirming pulpal vitality. Pre-operative pain intensity was
required to exceed 54 mm on the Heft-Parker visual analogue scale
(VAS, 170 mm scale), indicating moderate to severe pain (13). This threshold was selected based on
the Heft-Parker VAS classification, where scores >54 mm
correspond to moderate to severe pain, ensuring the inclusion of
patients with clinically significant pain levels that challenge
anaesthetic efficacy in SIP cases. This cut-off aligns with that of
previous studies (14,15) and facilitates the meaningful
evaluation of the effects of cryotherapy on pain management in
highly symptomatic patients.
Dental anxiety was also assessed pre-operatively
using Corah's Dental Anxiety Scale-Revised (DAS-R), which yields a
total score ranging from 4 to 20(16). The scores were categorized as
follows: ≤8, mild anxiety; 9-12, moderate anxiety; 13-14, high
anxiety; and 15-20, severe anxiety or dental phobia. Only patients
with DAS-R scores >9 were included to ensure a uniform level of
moderate-to-high dental anxiety, as anxiety is known to lower pain
thresholds and can affect the success of local anaesthesia.
Including this criterion helped standardize the psychological
factors affecting the anaesthetic response across participants.
The exclusion criteria included patients with
systemic health conditions, a history of analgesic intake within 12
h prior to the procedure, non-vital teeth (negative to EPT),
radiographic evidence of periapical pathology, such as widened
periodontal ligament space or periapical radiolucency, patients
with psychological or behavioural issues, a history of previous
endodontic treatment and a history of chronic pain. A total of 133
patients were screened; 60 patients who met all the inclusion
criteria were enrolled after obtaining written informed
consent.
Interventions and comparator
Participants were randomly assigned to two groups
(n=30 teeth each) as follows: i) Group I (the control): In this
group, patients received IANB with 3.6 ml 2% lignocaine
hydrochloride (Xylocaine®) and epinephrine (1:100,000)
using a standardized technique (17). The injection site was located
three-quarters of the distance along an imaginary line extending
from the midpoint of the coronoid notch to the deepest part of the
pterygomandibular raphe. A 27-gauge needle (31 mm) was used, and
the syringe barrel was positioned at the contralateral premolar or
molar region. After approximately two-thirds of the needle length
was advanced, and bone contact was achieved, negative aspiration
was confirmed. The entire volume was slowly deposited at a rate of
1 ml/min. During needle withdrawal, a few drops were deposited to
anaesthetize the lingual soft tissues and facilitate rubber dam
clamp placement.
ii) Group II (experimental group): This group
received the same IANB technique with a volume of 3.6 ml of 2%
lignocaine and epinephrine (1:100,000) as group I. In addition,
cryotherapy was administered post-anaesthesia using Endo-Frost
spray (Coltene) on the occlusal, buccal and lingual surfaces for 2
sec each, followed by the intrapulpal application of sterile ice
sticks (6 mm in diameter and 3 cm in length) for 4 min after access
cavity preparation and pulp chamber deroofing. Sterile ice sticks
were prepared and stored in a digital freezer (Gellvann). The
temperature of the ice sticks was monitored using a digital freezer
thermometer to ensure consistency, maintaining a range between -4
and 0˚C to prevent thermal injury. Following access cavity
preparation and pulpal exposure, the ice sticks were gently placed
inside the pulp chamber using sterile tweezers and maintained in
contact for 4 min. Care was taken to monitor any signs of patient
discomfort or tissue sensitivity during application.
Root canal treatment, including access cavity
preparation, cleaning, shaping and irrigation, was standardized for
both the groups. Access cavities were prepared using a high-speed
airotor handpiece with Endo Access burs (Dentsply Sirona) under
water cooling. Working length was determined using an electronic
apex locator (Root ZX II, J. Morita) and confirmed
radiographically. Cleaning and shaping were performed using
ProTaper Gold rotary instruments (Dentsply Sirona) using a
crown-down technique. Irrigation was performed with 3% sodium
hypochlorite (Prime Dental Products Pvt. Ltd.) using side-vented
irrigation needles (NaviTip, Ultradent Products Inc.), followed by
a final rinse with 17% EDTA (MD-Cleanser, Meta Biomed) and
distilled water.
At 20 min following IANB administration, the
effectiveness of local anaesthesia was verified using both
subjective and objective criteria. Subjective signs included
numbness of the lower lip and tongue, confirming anaesthesia of the
inferior alveolar and lingual nerves. Objective testing involved
EPT (D640 Digitest II Pulp Vitality Tester, Parkell) at two
intervals (2 min apart) and a cold stimulus test using a cotton
pellet moistened with Green Endo-Ice spray (Coltene/Whaledent Inc.)
applied for 5 sec. Only teeth that exhibited no response to either
the EPT or the cold test were included. Patients who exhibited a
positive response to either test were excluded from the study and
received supplemental intrapulpal or intraligamentary injections.
During treatment, pain was recorded using the Heft-Parker VAS,
categorized as 0 mm (no pain), <54 mm (mild pain), 54-114 mm
(moderate pain) and >114 mm (severe pain). Successful
anaesthesia was defined as no or mild pain (VAS ≤ 54 mm) during
access and cleaning/shaping. Moderate to severe pain was considered
a failure, and such cases were managed with supplemental
anaesthesia.
Outcomes
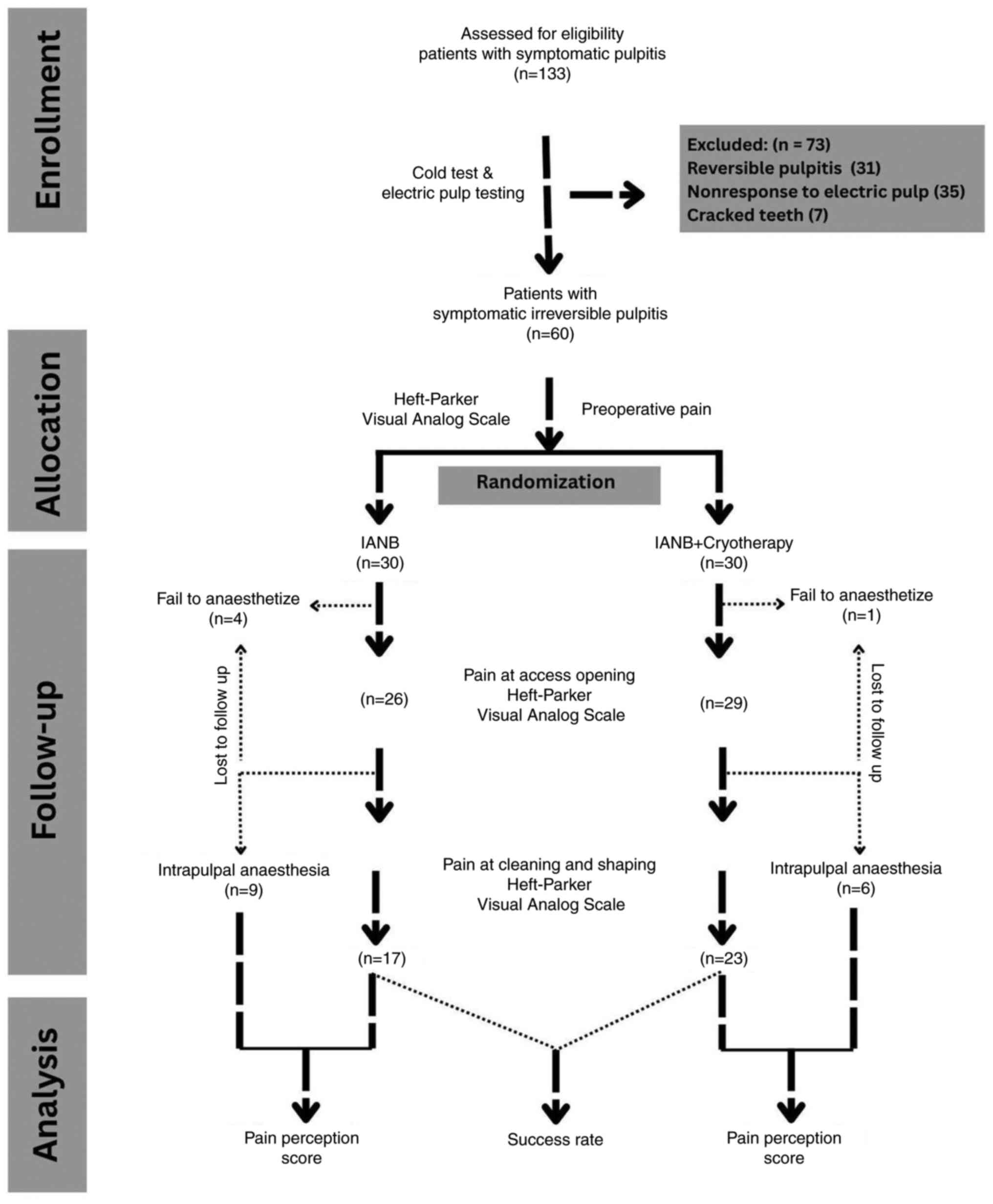
A total of 4 patients in the control group and
patient in the experimental group withdrew during follow-up due to
failure to anaesthesia. Thus, 26 patients in the control and 29
patients in the experimental group completed all study visits
(T1-T3) and were included in the final analysis. The primary
outcome was the success rate of anaesthesia, defined as the
percentage of patients reporting no to mild pain (≤54 mm on the
Heft-Parker VAS) during access opening and cleaning/shaping. The
secondary outcome was the pain score recorded on the Heft-Parker
VAS during these procedures.
Data management and harms
The data were stored in a secure password-protected
database with anonymized participant IDs. Only the principal
investigator and statistician accessed the final data set. For the
present study, one interim analysis was conducted at 50% enrolment
to assess the safety and preliminary efficacy, as planned in the
protocol. The Data Monitoring Committee (DMC), J N Kapoor D.A.V.
Dental College and Hospital, reviewed the primary endpoint (adverse
event rate) using a Haybittle-Peto boundary (P<0.001) to control
for type I errors. No significant harm was observed (P>0.001 for
severe adverse events), and the futility criteria (conditional
power <20%) were not met, allowing the study to continue to
completion as planned.
Sample size estimation
The sample size was determined using G*Power
software (version 3.1.9.2, Heinrich-Heine-Universität Düsseldorf,
Germany) with an alpha error of 5% and statistical power of 80%.
Based on an effect size of 0.70 from a previous study (14), and a projected attrition rate of 10%
in each group, 60 patients (30 per group) were deemed sufficient to
detect a clinically significant difference in anaesthesia success
rates.
Randomization
The personnel who enrolled participants and those
who assigned them to the interventions did not have access to the
random allocation sequence. Patients were randomly divided into the
experimental or control group using a computer-generated sequence
(random.org) with a block randomization method (block
size of four) to ensure balanced allocation. The principal
investigator was blinded to the randomization process to prevent
bias, and allocation concealment was maintained using sequentially
numbered opaque sealed envelopes that were opened only on the day
of the procedure.
Blinding
The blinding of the operator and participants was
not feasible due to the nature of cryotherapy intervention.
However, the outcome assessor responsible for recording the
Heft-Parker VAS scores was blinded to the group allocation to
reduce bias.
Statistical analysis
An intention-to-treat (ITT) analysis was performed
to account for dropouts; however, primary results are reported for
per-protocol completers. Data were entered into a Microsoft Excel
spreadsheet and analysed using Stata Statistical Software Release
18 (StataCorp, LP). The normality of the data distribution was
assessed using the Shapiro-Wilk test, with confirmation via Q-Q
plots. The data were found to be normally distributed. Data were
summarized using descriptive statistics: quantitative variables
(e.g., Heft-Parker VAS scores) and are reported as the mean ±
standard deviation (SD), and qualitative variables (e.g., success
rates) are presented as numbers and percentages. The intergroup
comparisons of pain score were performed using an independent
t-test and intragroup comparisons of the mean pain score were
performed using repeated measures ANOVA with the Bonferroni post
hoc test. The chi-square test was used to compare anaesthesia
success rates between the groups, with a significance level of
0.05. All analyses followed the intention-to-treat principle and
included all randomized participants in the final analysis.
Results
The CONSORT flow diagram is presented in Fig. 1. The study results demonstrated the
baseline comparability (Table I) of
group I and group II, with the mean ages of the patients being
32.8±6.20 and 32.6±6.31 years, respectively (P=0.9), and a
non-significant sex distribution, with each group consisting of 15
males (25%) and 15 females (25%).
 | Table IDescriptive analysis of the study
groups. |
Table I
Descriptive analysis of the study
groups.
| Parameters | Group I | Group II | Statistical
value | P-value |
|---|
| Age (years), mean ±
SD | 32.8±6.20 | 32.6±6.31 | 0.123 | NSa |
| Male, n (%) | 15 (25%) | 15 (25%) | 0 | NSb |
| Female, n (%) | 15 (25%) | 15 (25%) | | |
The pre-operative pain scores were similar between
the groups (99.17±15.57 vs. 95.33±18.56, P=0.39) (Table II). This demonstrated that both
groups were comparable at baseline. Group II exhibited
significantly lower pain during access opening compared with group
I (20.60±29.90 vs. 41.43±43.10, P=0.03), although not during
cleaning and shaping (17.73±24.06 vs. 26.95±36.72, P=0.27)
(Table II). Intragroup analysis via
repeated measures ANOVA confirmed a significant pain reduction over
time in both groups (Table III).
Post hoc analysis with the Bonferroni test revealed significant
pain reductions from preoperative to access opening and
cleaning/shaping in both groups (P=0.0003), with greater reductions
in group II (Table IV), but no
notable difference between cleaning/shaping and later stages. The
overall anaesthesia success rate was higher in group II (79.3%,
23/29) than in group I (65.3%, 17/26) (P=0.247), indicating that
cryotherapy enhanced IANB efficacy in patients with SIP; however,
this difference between the groups was not significant (Table V).
 | Table IIIntergroup comparison of Heft-Parker
VAS pain scores at different time intervals using an independent
t-test. |
Table II
Intergroup comparison of Heft-Parker
VAS pain scores at different time intervals using an independent
t-test.
| Pain | Group | No. of patients | Mean ± SD | Stats | P-value |
|---|
| Pre-operative
(T0) | Group I | 30 | 99.17±15.57 | 0.86 | 0.39 |
| | Group II | 30 | 95.33±18.56 | | |
| Access opening
(T1) | Group I | 26 | 41.43±43.10 | 2.10 | 0.04a |
| | Group II | 29 | 20.60±29.90 | | |
| Cleaning and
shaping (T2) | Group I | 26 | 26.95±36.72 | 1.11 | 0.27 |
| | Group II | 29 | 17.73±24.06 | | |
 | Table IIIIntragroup comparison of Heft-Parker
VAS pain scores at different time intervals (T0, T1 and T2) using
repeated measures ANOVA. |
Table III
Intragroup comparison of Heft-Parker
VAS pain scores at different time intervals (T0, T1 and T2) using
repeated measures ANOVA.
| Groups | Pre-operative
(T0) | Access opening
(T1) | Cleaning and
shaping (T2) | Statistical
value | P-value |
|---|
| Group I | 99.17±15.57 | 41.43±43.10 | 26.95±36.72 | 38.07 | 0.001a |
| Group II | 95.33±18.56 | 20.60±29.90 | 17.73±24.06 | 95.8 | 0.001a |
 | Table IVPost-hoc analysis with the Bonferroni
test for pairwise comparison of Heft-Parker VAS pain scores at
three different time intervals (T0, T1 and T2) in both the
groups. |
Table IV
Post-hoc analysis with the Bonferroni
test for pairwise comparison of Heft-Parker VAS pain scores at
three different time intervals (T0, T1 and T2) in both the
groups.
| | Group I | Group II |
|---|
| Pairwise group
comparison | Mean
difference | 95% CI | P-value | Mean
difference | 95% CI | P-value |
|---|
| T0 vs. T1 | 57.74 | -78.61 to
-36.86 | 0.0003a | 74.73 | -89.88 to
-59.57 | 0.0003a |
| T0 vs. T2 | 72.22 | -93.09 to
-51.34 | 0.0003a | 77.60 | -92.75 to
-62.44 | 0.0003a |
| T1 vs. T2 | 14.48 | -35.35 to 6.39 | 0.6864 | 2.87 | -18.023 to
12.28 | 0.9989 |
 | Table VOverall success rate of anaesthesia
in both the groups. |
Table V
Overall success rate of anaesthesia
in both the groups.
| Parameters | Group I (n=26) | Group II
(n=29) | Chi-squared
test | P-value |
|---|
| Successful
anaesthesia | 17 (65.3%) | 23 (79.3%) | 1.34 | 0.247a |
| Unsuccessful
anaesthesia requiring supplemental intrapulpal/intraligamentary
injections | 09 (34.7%) | 06 (20.7%) | | |
Discussion
Effective pain management remains the cornerstone of
successful endodontic therapy, with the ability to achieve profound
anaesthesia, often serving as a critical measure of clinical
competence. IANB is the gold standard for anesthetizing mandibular
teeth during endodontic procedures. However, achieving adequate
anaesthesia in teeth with SIP presents a significant challenge
owing to the acute inflammatory state of the pulp. Inflammation in
SIP leads to an increased expression of tetrodotoxin-resistant
sodium channels on nociceptors, which are less responsive to local
anaesthetics, reducing the success rate of IANB by up to eight-fold
(18). This physiological barrier,
combined with other factors, such as patient anxiety, inaccurate
injection techniques and anatomical variations, has prompted the
exploration of supplementary methods to enhance the efficacy of
IANB (5). Despite these efforts, no
technique has achieved complete pulpal analgesia, underscoring the
need for innovative approaches to improve pain control during
endodontic treatments.
The present study utilized a volume of 3.6 ml of 2%
lidocaine for IANB, based on the findings presented in the study by
Aggarwal et al (19), who
reported a higher success rate with this dosage compared to 1.8 ml
in patients with SIP and reported similar success rates with 2%
lidocaine, 4% articaine and 0.5% bupivacaine. This choice of
anaesthetic volume aligns with the aim of the study of optimizing
the efficacy of IANB as a baseline for comparison with cryotherapy.
Cryotherapy was administered to the experimental group (group II)
using a combination of refrigerant spray (Endo-Frost, Coltene) and
intrapulpal ice sticks. Cryotherapy has been explored in
endodontics in various forms, including cold saline irrigation and
intraoral ice packs, with evidence suggesting that it can mitigate
postoperative pain and enhance anaesthetic outcomes (9,20). For
instance, it has been demonstrated that cold saline irrigation
significantly reduces postoperative pain in teeth with vital pulps,
likely by reducing inflammation and pulpal nerve activity (21).
In the present study, group II (cryotherapy)
demonstrated significantly lower mean pain scores than group I
(control) during access opening (P<0.001), indicating that
cryotherapy effectively enhanced the efficacy of IANB at this stage
of treatment. However, during cleaning and shaping, while group II
exhibited a lower mean pain score, the difference was not
statistically significant (P>0.05). This non-significant
difference may be attributed to the transient nature of the
analgesic effects of cryotherapy, as the cooling-induced nociceptor
desensitization and reduced pulpal blood flow likely diminish over
time (7). The intrapulpal ice
application, administered for 4 min immediately following access
cavity preparation, may have exerted its maximum effect during the
initial stages of treatment, with the cryoanesthetic effect waning
by the time cleaning and shaping commenced, typically 10-15 min
later in the procedure. This temporal limitation is consistent with
prior studies, such as Vera et al (22), which noted that the effects of
cryotherapy are most pronounced within a short window
post-application due to tissue rewarming and restoration of normal
neural conduction. Additionally, the mechanical stimulation and
irrigation during cleaning and shaping may further activate
sensitized nociceptors in inflamed pulp tissue, potentially
counteracting the residual cryotherapy effect (21). These factors likely explain the lack
of a significant difference at this later stage, suggesting that
supplemental cryotherapy applications or alternative adjunctive
techniques may be necessary to maintain analgesia throughout the
entire endodontic procedure.
The present study experienced a higher dropout rate
in the control group (4 patients) compared with the experimental
group (1 patient), primarily due to anaesthesia failure, raising
the possibility of skewed outcomes. However, the use of an ITT
analysis, alongside the primary per-protocol analysis of completers
(26 control and 29 experimental patients), helped mitigate
potential bias by including all randomized participants in the
final analysis.
Cryotherapy induces vasoconstriction and diminishes
cellular metabolism by restricting biochemical processes, which
reduces the extent of tissue injury, consequently reducing the
oxygen requirements of cells and curtailing the production of free
radicals within tissues. The vasoconstrictive response yields
anti-edematous effects, whereas analgesia is attained following a
decrease in temperature due to the inhibition of nerve endings
resulting from the application of cold stimuli (7). The magnitude of the vasoconstriction
reaches its peak at a temperature of 15˚C, and research has
indicated that a reduction in body temperature diminishes
peripheral nerve conduction; notably, at ~7˚C, there is a total
deactivation of myelinated A delta fibres, whereas the
non-myelinated C-fibres become inactive at ~3˚C (23).
Overall, in the present study, group II achieved a
higher success rate of anaesthesia than group I, with a
statistically significant difference. These findings are consistent
with those of Topçuoğlu et al (24), who reported that preoperative
intraoral ice pack application for 5 min significantly improved
IANB success rates in patients with SIP. Similarly, Gopakumar et
al (11) evaluated the effect of
intraoral cryotherapy using ice sticks and refrigerant spray, and
found that both methods significantly reduced pain and improved
IANB outcomes in SIP cases, with ice packs showing superior
results, as observed in the present study.
The application of Endo-Frost refrigerant spray
(-50˚C), composed of propane, butane and isobutane, in combination
with intrapulpal ice sticks for 4 min, likely contributed to the
observed pain reduction in group II. Vera et al (22) suggested that the optimal duration of
cryotherapy varies by tissue type, with 4-5 min being sufficient to
achieve therapeutic effects without causing damage in areas with
minimal muscle and fat, as in intraoral applications. The 4-min
duration for intrapulpal ice application used in the present study
was selected based on this evidence, as it balances the need for
effective nociceptor desensitization and reduced pulpal blood flow
with the prevention of thermal injury to pulpal or surrounding
tissues. This duration is further supported by practical
considerations, as preliminary testing indicated that 4 min allowed
consistent cooling of the pulp chamber without patient discomfort
or procedural delays, aligning with findings from Gopakumar et
al (11), who used a similar
duration for intrapulpal ice application. By contrast, Koteeswaran
et al (25) found no
significant difference between IANB alone and IANB with cryotherapy
using Endo-Ice spray (-26.2˚C) and intrapulpal ice. This
discrepancy may be attributed to the lower temperature of
Endo-Frost (-50˚C) used in the present study, which likely produced
a more pronounced cryoanesthetic effect compared to Endo-Ice,
facilitating deeper tissue cooling and greater pain reduction.
The physiological mechanisms of cryotherapy provide
the rationale for its effectiveness. Cold application extracts heat
from the tissue, causing vasoconstriction and reducing local
inflammation, thereby mitigating oedema and inflammation (7). Goodis et al (26) reported that tooth cooling decreased
pulpal blood flow, which can eliminate pain perception in some
cases. Additionally, cryotherapy reduces the adherence of
leukocytes to capillary endothelial walls and decreases endothelial
dysfunction (7). According to Van't
Hoff's law, a 10˚C decrease in tissue temperature reduces local
enzyme activity and cellular metabolism by 2-3-fold, minimizing
tissue damage (7). Furthermore,
cryotherapy disrupts nerve conduction by causing myelin sheath
deterioration and axonal degeneration, raising the nociceptive
threshold, and slowing pain signal transmission (19). Cold also inactivates oral vanilloid
receptors, which are upregulated during inflammation and are
sensitive to capsaicin, further reducing pain perception (27). These mechanisms likely explain why
patients often use cold (e.g., ice or cold water) to alleviate
acute pulpal pain, a clinical observation supported by prior
literature (28,29). Collectively, these factors likely
contributed to the significant pain reduction observed in group II
compared with group I during endodontic treatment.
Demographic variables (pre-operative pain, age and
sex) were comparable between the two groups, indicating that these
factors did not influence the study outcomes. Consequently, the
null hypothesis that there would be no difference in IANB efficacy
between group I and group II was rejected. The superior performance
of the cryotherapy group underscores its potential as a
non-invasive, chairside technique to enhance IANB efficacy in SIP
cases.
Previous studies evaluating cryotherapy as an
adjunct to IANB in patients with SIP have provided valuable
insight, but are not without potential biases (9,11,15). A
number of studies, including those examining buccal ice packs or
intrapulpal ice application, often faced challenges with blinding
due to the sensory nature of cold application, which may introduce
placebo effects or patient reporting bias, particularly when
subjective pain scales like the Heft-Parker VAS were used (11,30).
Additionally, small sample sizes in some trials may have limited
statistical power, potentially overestimating or underestimating
the efficacy of cryotherapy. Variability in patient selection
criteria, such as inconsistent preoperative pain thresholds or
inclusion of patients with differing levels of dental anxiety,
could further confound results, as these factors influence pain
perception and anaesthesia outcomes (15,31).
These methodological limitations highlight the need for more robust
study designs, such as larger sample sizes and the use of sham
cryotherapy or objective pain assessment methods, to minimize bias
and enhance the reliability of findings in future research.
The findings of the present study suggest several
clinical implications for integrating cryotherapy into the
management of SIP in endodontic practice. First, cryotherapy, using
a combination of cold spray and intrapulpal ice application, can
serve as an effective adjunct to inferior alveolar nerve block
anaesthesia, particularly for patients with severe pre-operative
pain. This approach enhances patient comfort during initial
treatment stages, potentially improving procedural efficiency and
patient cooperation in challenging cases. Second, in settings where
immediate root canal therapy is not available, such as emergency
departments or rural clinics, cryotherapy could provide temporary
pain relief by reducing pulpal inflammation and nerve sensitivity,
acting as a bridge to definitive treatment while referrals are
arranged. Third, by decreasing inflammation and nerve
responsiveness, cryotherapy may help reduce post-operative pain,
potentially lowering the need for analgesics and supporting a
smoother recovery. Incorporating cryotherapy into standard
protocols for managing symptomatic irreversible pulpitis offers a
non-invasive, cost-effective strategy to improve anaesthesia
outcomes and patient experience. However, further research is
required to establish standardized protocols, including optimal
timing and frequency of cryotherapy application, to ensure
consistent benefits across diverse clinical settings.
Despite these promising results, the present study
has several limitations. The small sample size (n=60) may limit the
generalizability of the findings, necessitating larger trials to
confirm the efficacy of cryotherapy. Additionally, the lack of
blinding for both operators and patients due to the nature of
cryotherapy application introduces a potential for bias, which
could have influenced pain reporting. Future studies could mitigate
this limitation by implementing sham cryotherapy, such as using a
non-cooled spray or room-temperature sticks, to blind participants
and operators while maintaining the procedural appearance of
cryotherapy application. Additionally, employing objective pain
assessment methods, such as pulpal nerve stimulation or
physiological monitoring (such as heart rate variability), could
further reduce bias in pain reporting. Variations in operator skill
during cryotherapy application or differences in pulp chamber
anatomy across patients may have also influenced the consistency of
the effects of cryotherapy, as these factors could affect the
precision of ice stick placement or the extent of cooling achieved.
These strategies would enhance the robustness of future trials
evaluating the efficacy of cryotherapy in endodontic pain
management.
In conclusion, cryotherapy, as a supplementary
technique, significantly enhances the efficacy of IANB in patients
with SIP, particularly during access opening, offering a simple and
non-invasive method to reduce pain and improve patient comfort. The
higher anaesthesia success rate compared to conventional IANB alone
underscores its potential as a valuable adjunct in endodontic
practice. However, larger, well-controlled studies are required to
validate these findings and address the limitations of the present
study, ensuring the consistent integration of cryotherapy into
standard protocols for managing SIP.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author. The present randomized
controlled trial is registered as.
Author's contributions
SK and PB conceptualized the study, designed the
methodology and drafted the initial manuscript. SK and RKB
contributed to data collection, performed the clinical intervention
and critically revised the manuscript for intellectual content. RKB
and VG conducted the statistical analysis, interpreted the data,
and contributed to manuscript drafting. SG and SDG participated in
the study design, patient recruitment and data interpretation,
ensuring clinical relevance. SG and SDG managed data acquisition,
including patient assessments and CPAP compliance monitoring. SK
and SDG confirm the authenticity of all the raw data. and confirm
the authenticity of data, and finalized the manuscript for
submission. All authors reviewed, and have read and approved the
final manuscript and agree to be accountable for all aspects of the
work, ensuring its accuracy and integrity.
Ethics approval and consent to
participate
Ethical approval for the present study was from the
Ethics Committee of J N Kapoor D.A.V. Dental College and Hospital,
Yamunanagar, India (F/EC/21/0018). The study was conducted in
strict accordance with the principles outlined in the Declaration
of Helsinki and in compliance with all relevant guidelines and
regulations governing human research ethics. Each patient provided
written informed consent prior to participation.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests
Use of artificial intelligence tools
During the preparation of this work, AI tools were
used to improve the readability and language of the manuscript or
to generate images, and subsequently, the authors revised and
edited the content produced by the AI tools as necessary, taking
full responsibility for the ultimate content of the present
manuscript.
References
|
1
|
Falatah AM, Almalki RS, Al-Qahtani AS,
Aljumaah BO, Almihdar WK and Almutairi AS: Comprehensive strategies
in endodontic pain management: an integrative narrative review.
Cureus. 15(e50371)2023.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Thangavelu K, Kannan R and Kumar NS:
Inferior alveolar nerve block: Alternative technique. Anesth Essays
Res. 6:53–57. 2012.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Fowler S, Drum M, Reader A and Beck M:
Anesthetic success of an inferior alveolar nerve block and
supplemental articaine buccal infiltration for molars and premolars
in patients with symptomatic irreversible pulpitis. J Endod.
42:390–392. 2016.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Ueno T, Tsuchiya H, Mizogami M and
Takakura K: Local anesthetic failure associated with inflammation:
verification of the acidosis mechanism and the hypothetic
participation of inflammatory peroxynitrite. J Inflamm Res.
1:41–48. 2008.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Meechan JG: Supplementary routes to local
anaesthesia. Int Endod J. 35:885–896. 2002.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Kanaa MD, Whitworth JM and Meechan JG: A
prospective randomized trial of different supplementary local
anesthetic techniques after failure of inferior alveolar nerve
block in patients with irreversible pulpitis in mandibular teeth. J
Endod. 38:421–425. 2012.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Fayyad DM, Abdelsalam N and Hashem N:
Cryotherapy: A new paradigm of treatment in endodontics. J Endod.
46:936–942. 2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Algafly AA and George KP: The effect of
cryotherapy on nerve conduction velocity, pain threshold and pain
tolerance. Br J Sports Med. 41:365–369. 2007.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Elheeny AAH, Sermani DI, Saliab EA and
Turky M: Cryotherapy and pain intensity during endodontic treatment
of mandibular first permanent molars with symptomatic irreversible
pulpitis: A randomized controlled trial. Clin Oral Investig.
27:4585–4593. 2023.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Ahmad MZ: Effects of intracanal
cryotherapy on postoperative pain in necrotic teeth with
symptomatic apical periodontitis: A randomized controlled clinical
trial. Front Dent Med. 6(1543383)2025.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Gopakumar R, Jayachandran M, Varada S,
Jayaraj J, Ezhuthachan Veettil J and Nair NS: Anesthetic efficacy
of Endo-Ice and intrapulpal ice sticks after inferior alveolar
nerve block in symptomatic irreversible pulpitis: A randomized
controlled study. Cureus. 15(e42135)2023.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Hopewell S, Chan AW, Collins GS,
Hróbjartsson A, Moher D and Schulz KF: CONSORT 2025 statement:
Updated guideline for reporting randomised trials. Lancet: April
14, 2025 (Epub ahead of print). doi:
10.1016/S0140-6736(25)00672-5.
|
|
13
|
Glickman GN: AAE consensus conference on
diagnostic terminology: Background and perspectives. J Endod.
35:1619–1620. 2009.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Heft MW and Parker SR: An experimental
basis for revising the graphic rating scale for pain. Pain.
19:153–161. 1984.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Gupta R and Prakash P: Cryotherapy as an
adjunct to inferior alveolar nerve block in symptomatic
irreversible pulpitis: A randomised controlled clinical trial. IP
Indian J Conserv Endod. 7:16–23. 2022.
|
|
16
|
Ronis DL, Hansen CH and Antonakos CL:
Equivalence of the original and revised dental anxiety scales. J
Dent Hyg. 69:270–272. 1995.PubMed/NCBI
|
|
17
|
Malamed SF: Handbook of Local Anesthesia.
6th edition. Elsevier, St. Louis, pp225-252, 2014.
|
|
18
|
Kistner K, Zimmermann K, Ehnert C, Reeh PW
and Leffler A: The tetrodotoxin-resistant Na+ channel Na(v)1.8
reduces the potency of local anesthetics in blocking C-fiber
nociceptors. Pflugers Arch. 459:751–763. 2010.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Aggarwal V, Singla M and Miglani S:
Comparative evaluation of anesthetic efficacy of 2% lidocaine, 4%
articaine, and 0.5% bupivacaine on inferior alveolar nerve block in
patients with symptomatic irreversible pulpitis: A prospective,
randomized, double-blind clinical trial. J Oral Facial Pain
Headache. 31:124–128. 2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Keskin C, Özdemir Ö, Uzun İ and Güler B:
Effect of intracanal cryotherapy on pain after single-visit root
canal treatment. Aust Endod J. 43:83–88. 2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Almohaimede A and Al-Madi E: Is intracanal
cryotherapy effective in reducing postoperative endodontic pain? An
updated systematic review and meta-analysis of randomized clinical
trials. Int J Environ Res Public Health. 18(11750)2021.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Vera J, Castro-Nuñez MA, Troncoso-Cibrian
MF, Carrillo-Varguez AG, Méndez Sánchez ER and Rangel-Padilla JA:
Effect of cryotherapy duration on experimentally induced connective
tissue inflammation in vivo. Restor Dent Endod.
48(e29)2023.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Belitsky RB, Odam SJ and Hubley-Kozey C:
Evaluation of the effectiveness of wet ice, dry ice, and cryogenic
packs in reducing skin temperature. Phys Ther. 67:1080–1084.
1987.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Topçuoğlu HS, Arslan H, Topçuoğlu G and
Demirbuga S: The effect of cryotherapy application on the success
rate of inferior alveolar nerve block in patients with symptomatic
irreversible pulpitis. J Endod. 45:965–969. 2019.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Koteeswaran V, Ballal S, Natanasabapathy V
and Kowsky D: Efficacy of Endo-Ice followed by intrapulpal ice
application as an adjunct to inferior alveolar nerve block in
patients with symptomatic irreversible pulpitis-a randomized
controlled trial. Clin Oral Investig. 23:3501–3507. 2019.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Goodis HE, Winthrop V and White JM: Pulpal
responses to cooling tooth temperatures. J Endod. 26:263–267.
2000.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Laureano Filho JR, de Oliveira e Silva ED,
Batista CI and Gouveia FM: The influence of cryotherapy on
reduction of swelling, pain and trismus after third-molar
extraction: A preliminary study. J Am Dent Assoc. 136:774–778; quiz
807. 2005.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Babes A, Amuzescu B, Krause U, Scholz A,
Flonta ML and Reid G: Cooling inhibits capsaicin-induced currents
in cultured rat dorsal root ganglion neurones. Neurosci Lett.
317:131–134. 2002.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Bleakley CM and Hopkins JT: Is it possible
to achieve optimal levels of tissue cooling in cryotherapy? Phys
Ther Rev. 15:344–350. 2010.
|
|
30
|
Bazaid DS and Kenawi LMM: The effect of
intracanal cryotherapy in reducing postoperative pain in patients
with irreversible pulpitis: A randomized control trial. Int J
Health Sci Res. 8:83–88. 2018.
|
|
31
|
Karunakar P, Solomon RV, Kumar BS and
Reddy SS: Evaluating the pain at site, onset of action, duration
and anesthetic efficacy of conventional, buffered lidocaine, and
precooled lidocaine with intraoral cryotherapy application in
patients with symptomatic irreversible pulpitis: A clinical study.
Conserv Dent Endod. 27:1228–1233. 2024.PubMed/NCBI View Article : Google Scholar
|