Introduction
Thyroid tumors are uncommon among the pediatric
population, representing ~0.7% of all childhood cancers (1). Despite this rarity, thyroid cancer is
the most prevalent type of endocrine malignancy among children, and
its incidence increases with age, reaching its peak between 15 and
19 years of age (2). Among the
different types of thyroid cancer, papillary thyroid carcinoma
(PTC) is the most frequently diagnosed, accounting for ~80-90% of
all pediatric thyroid cancer cases (3). Although PTC is rare in children, it
often presents with more extensive lymph node involvement and a
higher likelihood of distant metastases than in adults, making
early detection and appropriate treatment crucial.
Several risk factors have been found to be
associated with the development of thyroid cancer, including
Hashimoto's thyroiditis, genetic disorders such as multiple
endocrine neoplasia type 2, Carney's syndrome, Werner's syndrome
and DICER1 syndrome, iodine deficiency, as well as exposure to
ionizing radiation, particularly during childhood (1). These risk factors highlight the
importance of the careful monitoring of individuals with relevant
medical histories. Pediatric thyroid cancer is often initially
discovered as a neck mass, typically without accompanying symptoms,
which can result in a range of progression stages at the time of
diagnosis. Although rare, thyroid cancer in children can be easily
mistaken for other non-thyroid conditions, such as abscesses,
malformations, ectopic thymus, thyroglossal duct cysts and various
tumors. This misdiagnosis can lead to delays in appropriate
treatment, highlighting the importance of considering thyroid
cancer in the differential diagnosis of pediatric neck masses
(2).
PTC subtypes include classic, solid, follicular and
diffuse sclerosing variants. In children, particularly those aged
<10 years, the classic papillary morphology often observed in
adults may be absent. These tumors can be unencapsulated and widely
invasive throughout the thyroid, displaying a follicular and solid
architecture with unique nuclear features and abundant psammoma
bodies (4).
The present study describes two rare cases of PTC in
pediatric patients with no notable medical or family history of
thyroid cancer, both of whom underwent total thyroidectomy without
complications. Furthermore, the present study aimed to contribute
valuable information to the current body of literature through a
detailed review of the existing information. The present case
report was written in accordance with the CaReL guidelines. Only
reliable, peer-reviewed sources were used while excluding any
untrustworthy references or data (5,6).
Case report
Case 1. Patient information
A 9-year-old girl presented to the Head and Neck
Clinic at Smart Health Tower (Sulaymaniyah, Iraq) with a painless
anterior neck swelling that had been present for four weeks. She
had no significant family, medical, or surgical history.
Clinical findings. The patient was vitally
stable. Upon examination, the thyroid gland was firm and enlarged,
with palpable cervical lymph nodes.
Diagnostic approach. Laboratory
investigations revealed normal thyroid function. The
thyroid-stimulating hormone (TSH) level was 3.3 uIU/ml (normal
range, 0.8-6.0 uIU/ml), the calcitonin was 0.724 pg/ml (normal
range, up to 9.82 pg/ml), the anti-thyroglobulin level was elevated
at 373 IU/ml (normal range, <115 IU/ml) and the serum calcium
level was normal at 9.62 mg/dl (normal range, 8.8-10.8 mg/dl). A
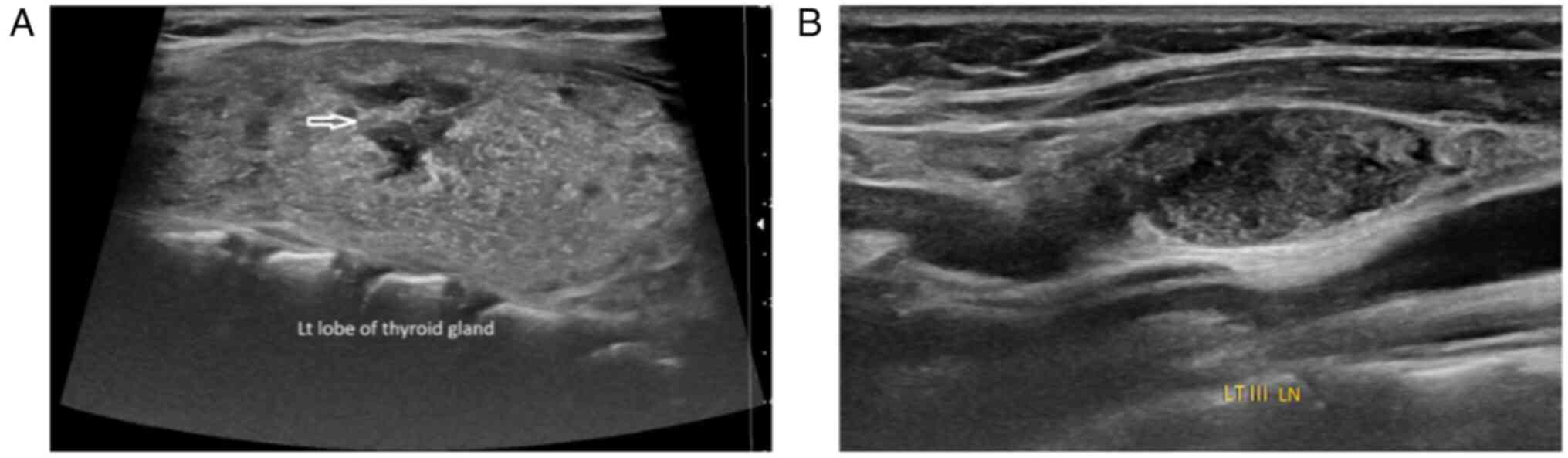
neck ultrasound (US) revealed a mildly enlarged thyroid gland with
heterogeneous parenchymal texture, and multiple irregular
hypoechoic lesions were noted in both lobes, primarily on the left
and diffuse microcalcifications in both lobes. Suspicious lymph
nodes were identified around the gland, the largest measuring 17x8
mm. They were also identified in the right cervical groups I, II,
III and IV, the largest measuring 22x6 mm, and the left groups II,
III, IV, and V, the largest measuring 20x9 mm (Fig. 1). Fine-needle aspiration cytology
(FNAC) under ultrasound guidance was suggestive of PTC.
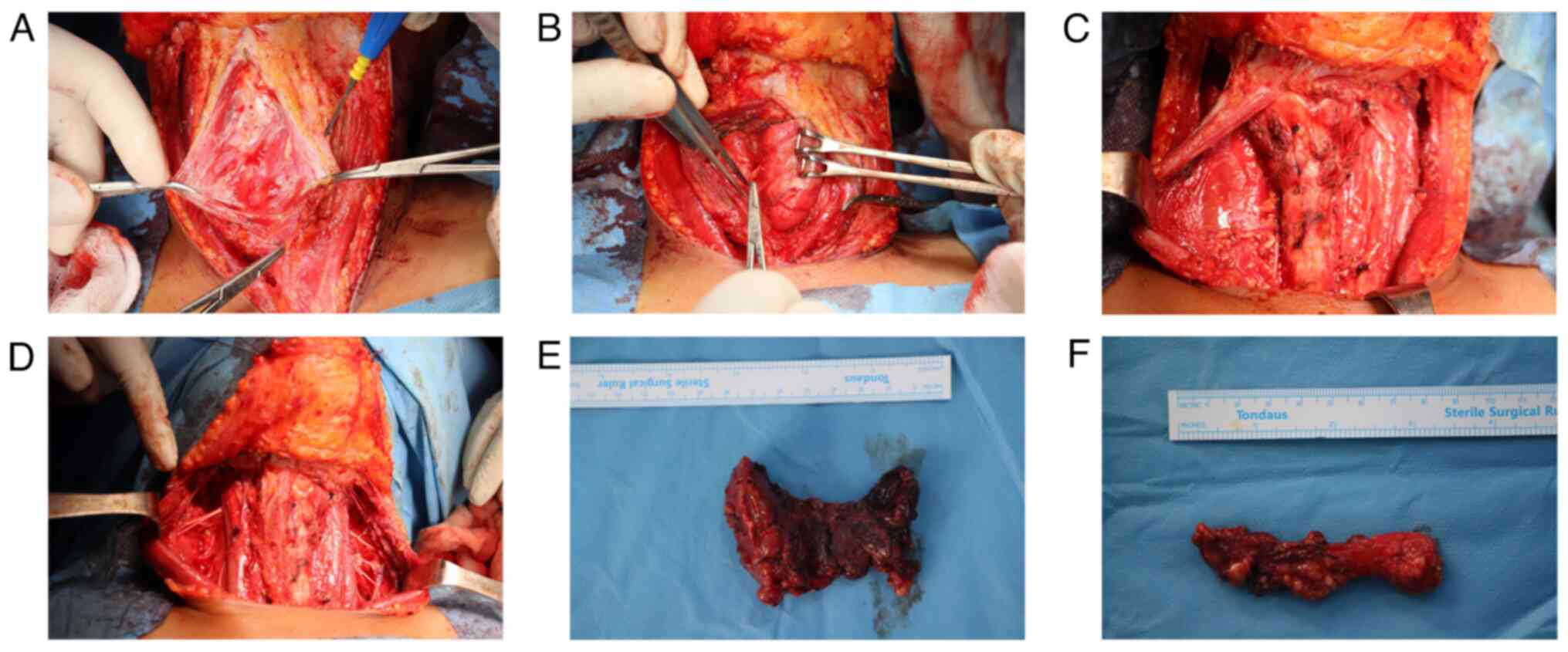
Therapeutic intervention. Under general
anesthesia, the patient underwent a total hyroidectomy with
bilateral central and lateral neck dissection (levels I to V). Both
recurrent laryngeal nerves were preserved, hemostasis was achieved,
and the wound was closed in layers (Fig.
2). Post-operatively, the patient remained stable. A
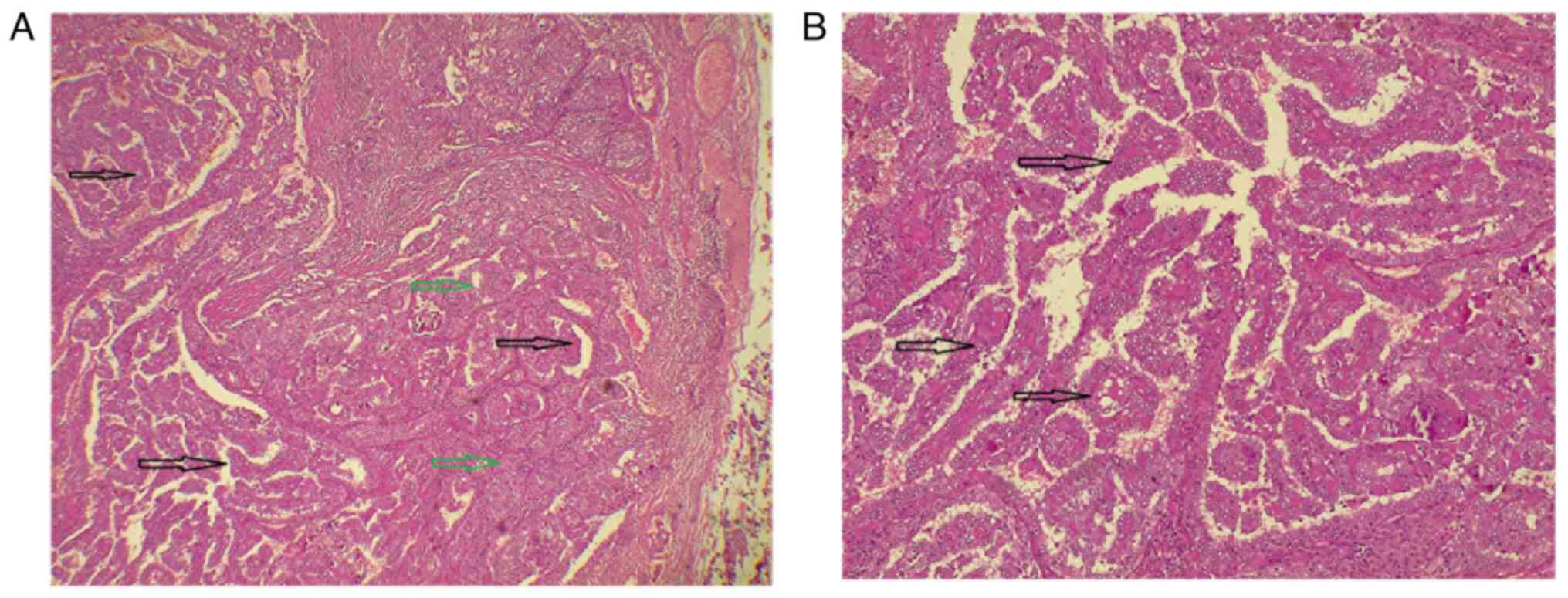
histopathological examination (HPE) was performed. Tissue samples
were fixed in 10% neutral-buffered formalin at room temperature for
24 h, processed and embedded in paraffin. Sections of 5 µm
thickness were prepared, stained with hematoxylin and eosin (Bio
Optica Co.) for 1-2 min at room temperature, and subsequently
examined using a light microscope (Leica Microsystems GmbH). The
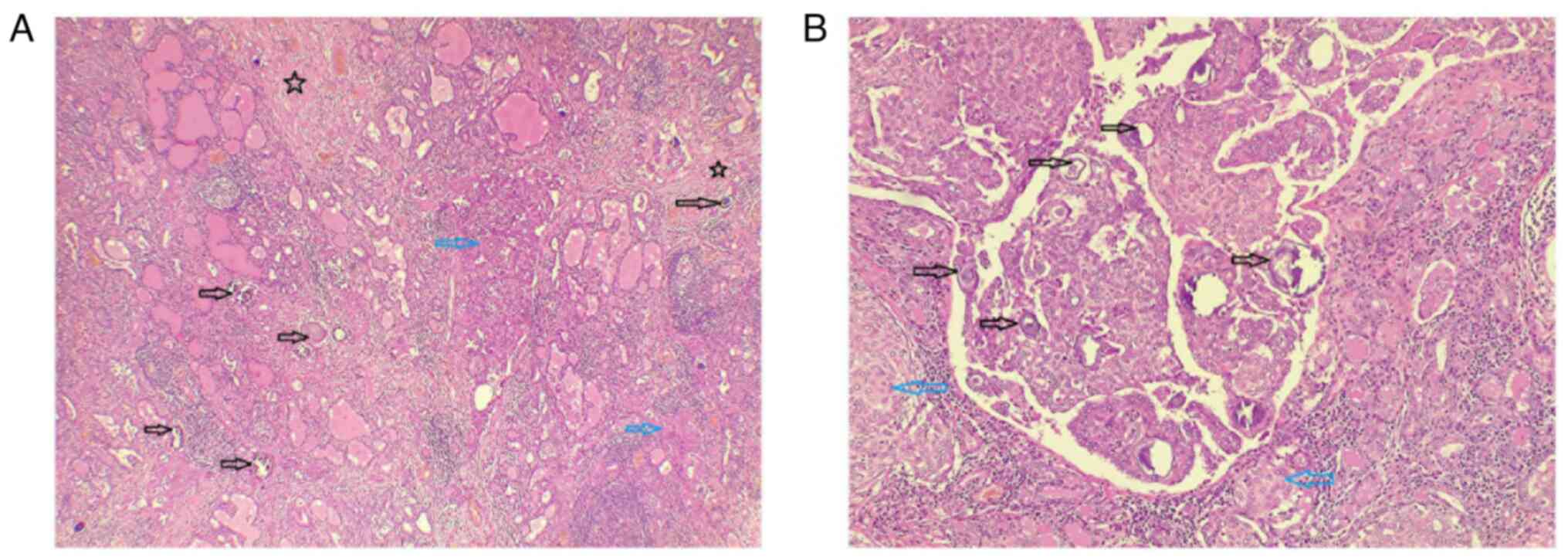
HPE revealed a multifocal, well-differentiated diffuse sclerosing
type PTC involving the right lobe, isthmus and left lobe, with the
largest lesion measuring 55 mm in the left lobe (Fig. 3). Of the 181 lymph nodes examined, 70
were positive for metastasis, including the Delphian lymph nodes
(9/9), right central group (8/9), left central group (5/14), right
lateral group (6/45) and left lateral group (8/104).
Follow-up. The patient recovered without
complications and was discharged (at almost 1 week following her
presentation to the hospital). with prescribed thyroid medication
and a scheduled follow-up appointment. She was referred for
radioactive iodine treatment and will have regular follow-ups to
monitor for any signs of recurrence.
Case 2. Patient information
A 9-year-old girl presented to the Head and Neck
Clinic at Smart Health Tower (Sulaymaniyah, Iraq) with right-sided
neck swelling that had been gradually enlarging over the past year.
She had no accompanying symptoms or notable medical, surgical, or
family history. There was also no history of irradiation or
consanguinity.
Clinical findings. Upon examination, the
thyroid gland was firm and enlarged at the right lobe, with
palpable cervical lymph nodes.
Diagnostic approach. Upon a laboratory
investigation, thyroid function tests were normal; the TSH level
was 2.77 uIU/ml (normal range, 0.8-6.0 uIU/ml), the free T4 level
was 16.62 Pmol/l (normal range, 12.8-27 Pmol/l), the calcitonin
level was 3.56 pg/ml (normal range, up to 9.82 pg/ml), the
thyroglobulin level was 2.53 ng/ml (normal range, 3.5-77 ng/ml) and
the normal serum calcium level was 9.35 mg/dl (normal range,
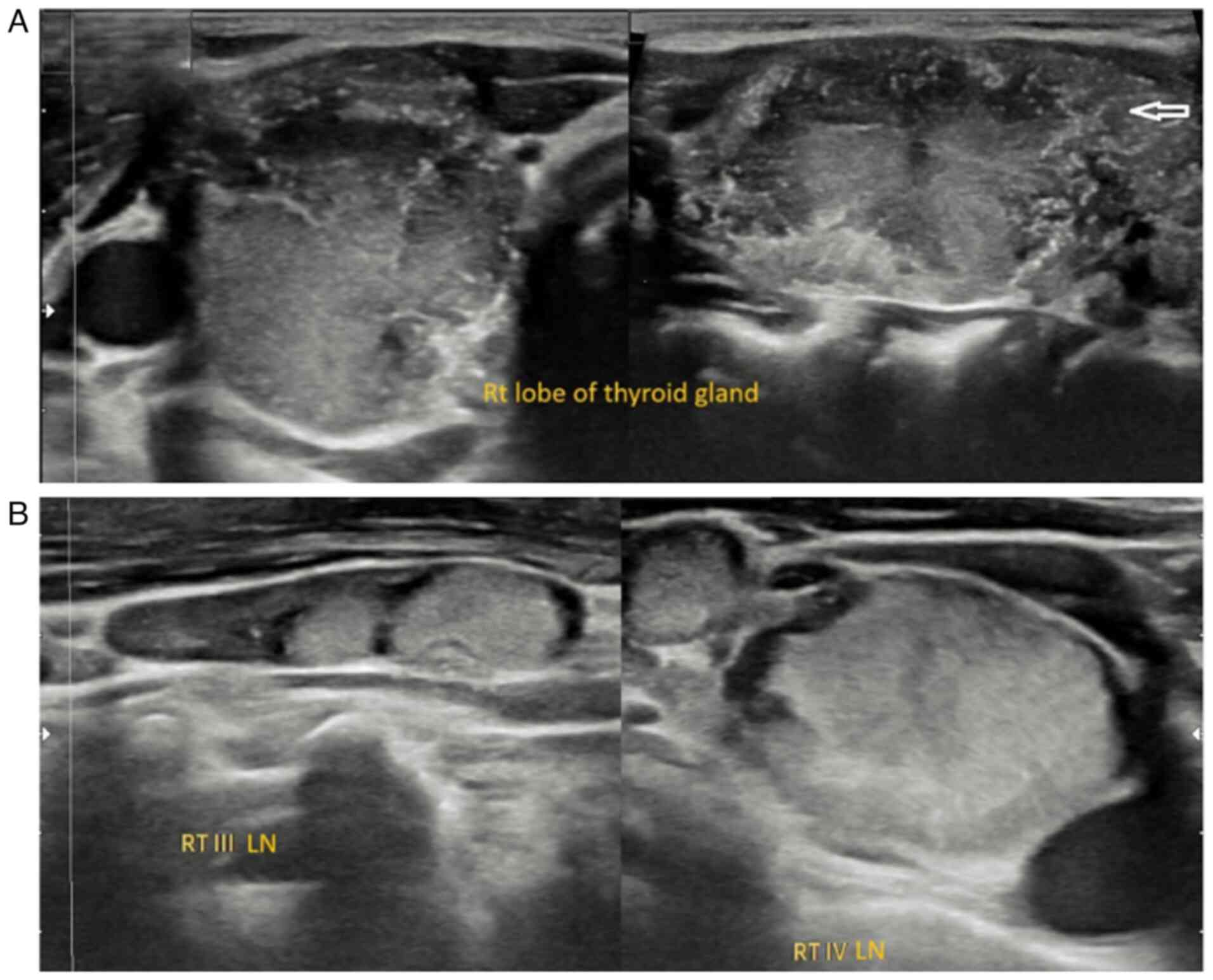
8.8-10.8 mg/dl). The neck US revealed a large, irregular outline,
hypervascular, heterogenously hypoechoic nodule measuring 37x19x19
mm, occupying the majority of the right lobe, mainly mid-upper
third with microcalcification, classified as a highly suspicious
nodule Thyroid Imaging, Reporting And Data System (TI-RADS)
5(7). This was associated with
suspicious pathological cervical lymph nodes in the right group II,
III and IV, the largest measuring 24x5 mm. In the left thyroid
lobe, there were a few small micronodules (Fig. 4). The patient underwent FNAC under US
guidance for the right TR5 nodule, and the cellular findings
confirmed PTC.
Therapeutic intervention. Following a
thorough discussion within a multidisciplinary team, the patient
underwent a total thyroidectomy with bilateral central and right
lateral neck dissection under general anesthesia. Both recurrent
laryngeal nerves were preserved. Hemostasis was achieved and the
wound was closed in layers. The post-operative course was
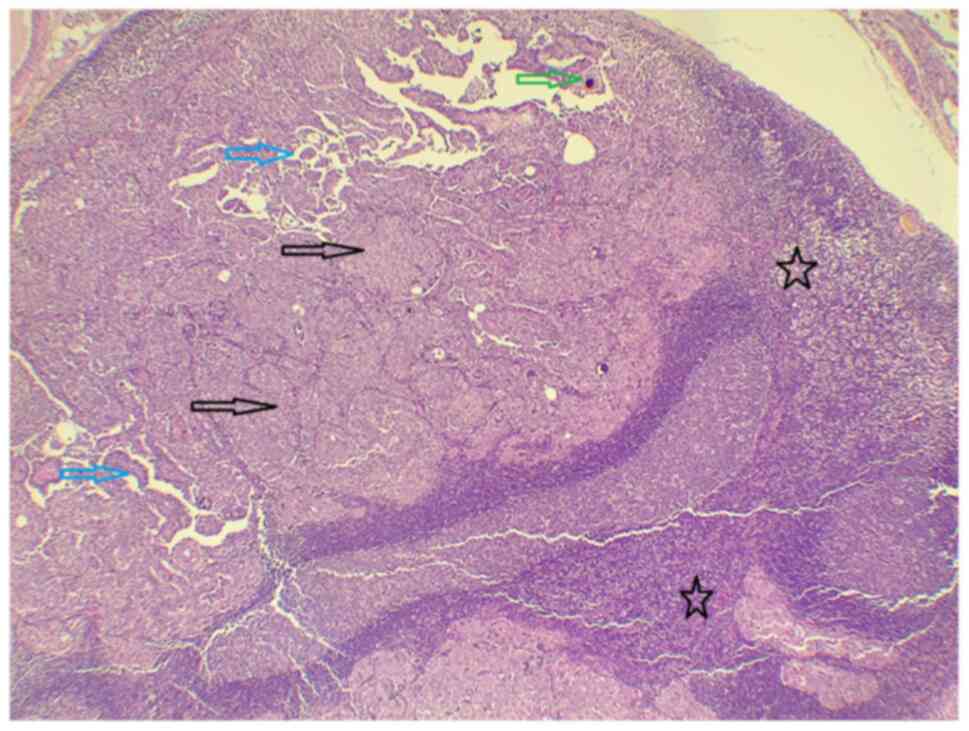
uneventful, with stable vital signs. A HPE (performed as described
above for Case 1) confirmed a unifocal, well-differentiated
conventional PTC in the right lobe (Fig.
5). Lymph node involvement was noted in 17 out of 72 nodes,
which exhibited infiltration by malignant epithelial cells forming
papillary structures: Delphian (0/2), right central (8/15), left
central (1/17) and right lateral (8/38) (Fig. 6).
Follow-up. The patient exhibited an
uneventful postoperative recovery and was discharged (at almost 1
week following her presentation to the hospital) on thyroid hormone
replacement therapy with a scheduled follow-up. She was referred
for adjuvant radioactive iodine therapy and enrolled in a
structured surveillance program to monitor for disease recurrence.
There was no clinical or radiological evidence of recurrence at the
three-year follow-up.
Discussion
PTC, particularly among prepubertal patients, is
considered rare. When compared with adult PTC, pediatric patients
with PTC often present with relatively more advanced-stage tumors
with a notable female predominance. However, pediatric patients
with PTC, if properly treated, have an improved prognosis compared
with older patients with PTC (2,8). This
was evident in the patients described herein, as the first case
exhibited multifocality, with the largest lesion measuring 55 mm,
accompanied by metastasis in 70 lymph nodes. The second case also
exhibited signs of local advancement as the tumor was 37 mm in
size, and 17 lymph nodes had been invaded. A literature search was
performed on the PubMed and Google Scholar database, covering the
period from January, 2017 to February, 2025. The search used
combinations of the following key words: ‘papillary thyroid
carcinoma’, ‘papillary thyroid cancer’, ‘thyroid neoplasm’,
‘pediatric’ and ‘prepubertal’. Only articles published in the
English language and reporting individual prepubertal PTC cases
were considered. From this search, 9 relevant cases were identified
and were included in a mini-review of the literature (2,3,8-14).
In line with the current body of literature and indicative of
advancement, 7 out of 9 (77.77%) cases exhibited multifocality, and
8 (88.88%) cases had lymph node involvement (Table I).
 | Table IFundamental characteristics of the
reviewed cases. |
Table I
Fundamental characteristics of the
reviewed cases.
| Age, years | Sex | Med. history | Family history | Location | Size in rad.
(mm)a | Multifocality | Lymph node
involvement | Hist. variant | Mutations | Dist. Met. | Surgical
approach | Radioactive iodine
therapy | Other adjuvant
therapy | Recurrence | Outcome | Follow-up, years | (Refs.) |
|---|
| 11 | F | Autoimmune
thyroiditis | Hypothyroidism and
vitiligo | Right thyroid
lobe | 45 | Yes | Yes | Diffuse
sclerosing | N/A | None | Total thyroidectomy
and central compartment lymphadenectomy | Yes | Suppressive
levothyroxine therapy | None | Alive | 0.3 | (3) |
| 8 | M | Unremarkable | Unremarkable | Right thyroid
lobe | 100 | Yes | Yes | Conventional | N/A | None | Total
thyroidectomy | No | Thyroxine | None | Alive | 4 | (2) |
| 15 | F | β-Thalassemia, acute
pancreatitis, transaminitis, Fanconi-like syndrome & secondary
amenorrhea | Unremarkable | Right thyroid
lobe | 59 | Yes | Yes | Conventional | N/A | None | Total thyroidectomy
and central compartment neck dissection | Yes | Levothyroxine | Yes | N/A | 2 | (11) |
| 17 | M | Unremarkable | N/A | Thyroglossal
duct | 65 | No | No | Conventional | N/A | None | Extended Sistrunk
procedure and total thyroidectomy | No | Thyroid Hormone
Suppression Therapy | No | Alive | 0.5 | (12) |
| 5 | M | Peripheral
cyanosis | N/A | N/A | 20 | No | Yes | Conventional | N/A | Lungs | Total thyroidectomy
& cervical lymph node excision | Yes | None | Yes | Died | 5.5 | (13) |
| 11 | F | Unremarkable | N/A | N/A | N/A | Yes | Yes | Diffuse
sclerosing | N/A | Lungs | Total thyroidectomy
& lymph node dissection | N/A | N/A | N/A | Alive | N/A | (10) |
| 12 | M | Hyperthyroidism | N/A | N/A | N/A | Yes | Yes | Conventional | N/A | Lungs | Total
thyroidectomy | Yes | None | Yes | | 0.5 | (9) |
| 13 | F | Unremarkable | Thyroid
carcinoma | Right thyroid
lobe | 40 | Yes | Yes | Conventional | N/A | Lungs | Total thyroidectomy
and bilateral central compartment lymph node excision | Yes | None | Yes | N/A | N/A | (14) |
| 7 | F | Unremarkable | N/A | Bilateral lobes of
the thyroid | R=35 L=18 | Yes | Yes | Conventional | ETV6/NTRK3
fusion | None | Total thyroidectomy
and bilateral cervical lymph node dissections | Yes | None | No | Alive | N/A | (8) |
| Mean: 11±3.84 | F: 5/9 M:4/9 | 5/9 | 2/9 | | | 7/9 | 8/9 | C: 8/9 D: 1/9 | 1/9 | 4/9 | TT: 9/9 | 6/9 | 4/9 | 4/9 | A: 5/9 D: 1/9 | | |
The most common sites of metastasis are the lungs,
bones and brain. Long-distance metastasis was present in 4 (44.44%)
of the reviewed cases, all in the lungs. The primary treatment for
lung metastases in thyroid cancer is radioactive iodine therapy,
which can achieve complete radiographic resolution and provide
long-term survival benefits for patients (9). The most significant predictors of
recurrence are lymph node involvement, multiple thyroid nodules at
presentation, and papillary or papillary-follicular histology.
Recurrence rates are higher in children (35-45%) compared to adults
(5-20%) (2). In the present study,
among the reviewed cases, 4 patients (44.44%) experienced
recurrence, all with lymph node involvement. Thyroid cancer is
generally more common among females than males, with an overall
ratio of ~1 male to every 3.6 females. However, in children aged
<10 years, this difference becomes less pronounced, with a
male-to-female ratio of ~1.25:1. The incidence of thyroid cancer
peaks between the ages of 15 and 19 years, with the average age at
diagnosis being 16 years (2). The
patients in the present case report were both 9 years of age, and
the mean age of diagnosis was 11±3.84 for the reviewed cases.
The majority of children with PTC are typically
diagnosed after noticing symptoms such as an enlarging thyroid
nodule or a persistent neck lymph node. The diagnostic process
often involves a physical exam, thyroid US, fine-needle biopsy,
and, if deemed necessary, a diagnostic hemithyroidectomy (10). A distinct subtype, pediatric diffuse
sclerosing PTC, such as that observed in case 1 in the present
study, is characterized by extensive infiltration, resulting in
enlargement of the affected thyroid lobe or the entire gland, often
with palpable cervical lymphadenopathy. This variant is frequently
associated with microcalcifications, making FNAC essential for
definitive diagnosis (3). The
primary imaging modality for evaluating neck swelling in children
is ultrasonography. Features suggestive of thyroid malignancy
include hypoechogenicity, an irregular outline, a subcapsular
location and type III nodular vascularization (both peri-nodular
and intra-nodular), which are strongly associated with an increased
likelihood of malignancy in pediatric patients. FNAC remains the
cornerstone of the diagnostic workup for thyroid nodules in
children, providing a minimally invasive and reliable method for
evaluating malignancy risk (15).
The 2009 ATA guidelines for adult thyroid cancer recommend staging
all patients with differentiated thyroid carcinoma (DTC) according
to the AJCC TNM classification. Within this framework, children are
categorized as stage I if no distant metastases are present and
stage II if distant metastases exist (4). Notably, the stage I group is highly
heterogeneous, encompassing children with a solitary intrathyroidal
lesion, those with extensive locoregional disease and cervical
lymph node involvement, as well as those with only microscopic PTC
(4).
In recent years, it has become widely accepted that
a total thyroidectomy is necessary for all pediatric PTC cases,
along with the surgical removal of any affected lymph nodes when
feasible, as it has been found that the absence of total
thyroidectomy is one of the most significant risk factors for
recurrence (10). A point of
surgical debate is whether to perform a central compartment lymph
node dissection, as it is associated with a higher risk of
hypoparathyroidism. This risk needs to be carefully balanced
against the potential for disease progression. Preserving the
recurrent laryngeal nerves, as accomplished in both cases, is
crucial, as damage can lead to vocal cord paralysis. Therefore, the
surgery needs to be performed by experienced professionals
(10). Children generally have a
longer life expectancy than adults; thus, it is crucial to
carefully evaluate the long-term impacts of thyroid cancer
treatment in pediatric patients. Radioiodine therapy, while
effective, is associated with risks of complications, such as
dysfunction of the salivary and lacrimal glands (the most common
side effects), reductions in fertility for both males and females,
bone marrow suppression and an increased risk of developing
secondary cancers (3). A lower
socioeconomic status and diagnostic delays can limit access to
timely care and specialized diagnostics, leading to more advanced
disease at presentation with greater nodal involvement and the need
for aggressive treatment. In pediatric PTC, where multifocality and
nodal spread are common, such factors further increase recurrence
risk and complicate management.
Future advances in PTC should rely on precision
medicine with molecular profiling for targeted therapy, AI-assisted
diagnostics to improve early detection, and liquid biopsy for
non-invasive monitoring. Studying heterogeneous nuclear
ribonucleoprotein C is also critical, as its expression levels have
been linked to tumor mutational burden (16). Selective radioactive iodine and
minimally invasive surgery support treatment de-escalation in
patients who are considered low-risk, while global collaborations
are vital to reduce disparities and refine pediatric-specific
guidelines that balance survival with long-term quality of
life.
A key limitation of the present study was the
absence of comprehensive genetic or molecular profiling, such as
assessment of BRAF, RAS, RET/PTC, or other kinase fusions, which
are increasingly recognized as critical for risk stratification,
prognosis and targeted therapy selection in pediatric PTC. The lack
of this information limits the ability to associate molecular
alterations with clinical outcomes and hinders personalized
treatment planning.
In conclusion, PTC in prepubertal children is
uncommon. Total thyroidectomy with adjuvant radioiodine therapy may
provide favorable outcomes; however, management needs to be
carefully individualized, and current evidence is limited to small
case series, underscoring the need for larger studies.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
FHK and AMS were major contributors to the
conception of the study, as well as to the literature search for
related studies. MMA, HAA and AAQ were involved in the conception
and design of the study, literature review and in the writing of
the manuscript. KMS, SFA, ZBN, SHH and ANQ were involved in the
literature review, in the design of the study, in the critical
revision of the manuscript, and in the processing of the table. AJQ
was the radiologist who assessed the case. AMA was the pathologist
who performed the diagnosis of the case. FHK and SHH confirm the
authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from the
parents of the patients for their participation in the present
study.
Patient consent for publication
Written informed consent was obtained from the
parents of the patients for the publication of the present case
report and any accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Martucci C, Crocoli A, De Pasquale MD,
Spinelli C, Strambi S, Brazzarola P, Morelli E, Cassiani J, Mancera
J, Luengas JP, et al: Thyroid cancer in children: A multicenter
international study highlighting clinical features and surgical
outcomes of primary and secondary tumors. Front Pediatr.
10(914942)2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Tirkaso BH, Mulugeta GA, Belete TD and
Melak MM: Papillary thyroid carcinoma in an 8-year-old Ethiopian
child: A case report with literature review. SAGE Open Med Case
Rep. 12(2050313X241248392)2024.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Szwarkowska M, Kaleta K, Jurek A,
Kujdowicz M, Taczanowska-Niemczuk A, Kiszka-Wiłkojć A, Maślanka M,
Górecki W, Starzyk J, Januś D, et al: Occult thyroid cancer in
autoimmune thyroiditis: Lymph node ultrasound as the sole
diagnostic indicator of malignancy in a pediatric case of papillary
thyroid carcinoma. Children (Basel). 12(194)2025.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Francis GL, Waguespack SG, Bauer AJ,
Angelos P, Benvenga S, Cerutti JM, Dinauer CA, Hamilton J, Hay ID,
Luster M, et al: Management guidelines for children with thyroid
nodules and differentiated thyroid cancer. Thyroid. 25:716–759.
2015.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Abdullah HO, Abdalla BA, Kakamad FH, Ahmed
JO, Baba HO, Hassan MN, Bapir R, Rahim HM, Omar DA, Kakamad SH, et
al: Predatory publishing lists: A review on the ongoing battle
against fraudulent actions. Barw Med J. 2:26–30. 2024.
|
|
6
|
Prasad S, Nassar M, Azzam AY, José FG,
Jamee M, Sliman RK, Evola G, Mustafa AM, Abdullah HO, Abdalla BA,
et al: CaReL guidelines: A consensus-based guideline on case
reports and literature review (CaReL). Barw Med J. 2:13–19.
2024.
|
|
7
|
Tessler FN, Middleton WD, Grant EG, Hoang
JK, Berland LL, Teefey SA, Cronan JJ, Beland MD, Desser TS, Frates
MC, et al: ACR thyroid imaging, reporting and data system
(TI-RADS): White paper of the ACR TI-RADS committee. J Am Coll
Radiol. 14:587–595. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Otsubo R, Mussazhanova Z, Akazawa Y, Sato
A, Matsuda K, Matsumoto M, Yano H, Matsuse M, Mitsutake N, Ando T,
et al: Sporadic pediatric papillary thyroid carcinoma harboring the
ETV6/NTRK3 fusion oncogene in a 7-year-old Japanese girl: A case
report and review of literature. J Pediatr Endocrinol Metab.
31:461–467. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Thirumala V, O'Souji C and Thirumala S:
Bilateral pulmonary metastases of papillary thyroid carcinoma in a
12-year-old child-A case report and review of the literature.
Radiol Case Rep. 15:799–802. 2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Verburg FA, Van Santen HM and Luster M:
Pediatric papillary thyroid cancer: Current management challenges.
Onco Targets Ther. 28:165–175. 2016.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Choleva L and Wilkes M: Papillary Thyroid
carcinoma in a pediatric patient with β-thalassemia. JCEM Case Rep.
1(luad131)2023.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Blaseg NA and Munson PD: Papillary thyroid
carcinoma arising in a thyroglossal duct cyst in a pediatric
patient. J Pediatr Surg Case Rep. 66(101790)2021.
|
|
13
|
Aladily TN, Khader M, Bustami N and Samara
OA: Papillary thyroid carcinoma in a 5-year-old child, mimicking
lymphoma in presentation. Avicenna J Med. 11:103–106.
2021.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Soydal Ç and Özkan E: A child with
papillary thyroid carcinoma: Role of radioactive iodine therapy in
pediatric patients. In: Thyroid and Parathyroid Diseases: A
Case-Based Guide. pp415-418, 2019.
|
|
15
|
Regmi PR, Amatya I, Paudel S and Kayastha
P: Papillary carcinoma of thyroid in a child, rare but aggressive:
A case report. Journal of Institute of Medicine Nepal. 43:102–104.
2021.
|
|
16
|
Shi Y, Wang Y, Zhang W, Niu K, Mao X, Feng
K and Zhang Y: N6-methyladenosine with immune infiltration and
PD-L1 in hepatocellular carcinoma: Novel perspective to
personalized diagnosis and treatment. Front Endocrinol (Lausanne).
14(1153802)2023.PubMed/NCBI View Article : Google Scholar
|