Introduction
Granulomatous mastitis (GM) is a rare inflammatory
condition of the breast that primarily affects women of
childbearing age, often with a history of breastfeeding. GM is
categorized into idiopathic or primary GM and secondary GM
(1,2). It primarily involves the mammary gland,
although in rare cases, it can develop in accessory breast tissue
(2). While the exact cause of GM
remains unclear, the leading hypothesis suggests an autoimmune
origin. Various factors, including medications, diabetes, trauma
and smoking, may trigger the inflammatory response. However, the
strongest associations with GM are pregnancy, lactation and
hyperprolactinemia. The disease accounts for <1% of breast
biopsies (3). Despite being a benign
disease, GM is frequently difficult to detect, as it often
masquerades as breast carcinoma, which is the primary concern at
the clinical stage (4). Its locally
aggressive character causes long-term discomfort and distress for
affected patients. Its non-specific imaging findings can lead to
delayed diagnosis, misinterpretation and potentially unnecessary
invasive procedures. Only a limited number of cases of GM in
axillary breast tissue have been documented (1,2). The
present report describes the case of a 43-year-old female patient
with GM in the accessory breast. The report has been organized
following the CaReL guidelines, and only reliable, peer-reviewed
sources were included, while excluding any untrustworthy references
or data (5,6).
Case report
Patient information
A 43-year-old lactating woman presented to the
Breast Clinic at Smart Health Tower (Sulaymaniyah, Iraq) with a
1-month history of pain in the left axilla and breast. An analysis
of her past medical and surgical history did not reveal any notable
findings. She had a history of four full-term pregnancies and a
cumulative lactation period of 4 years.
Clinical examination
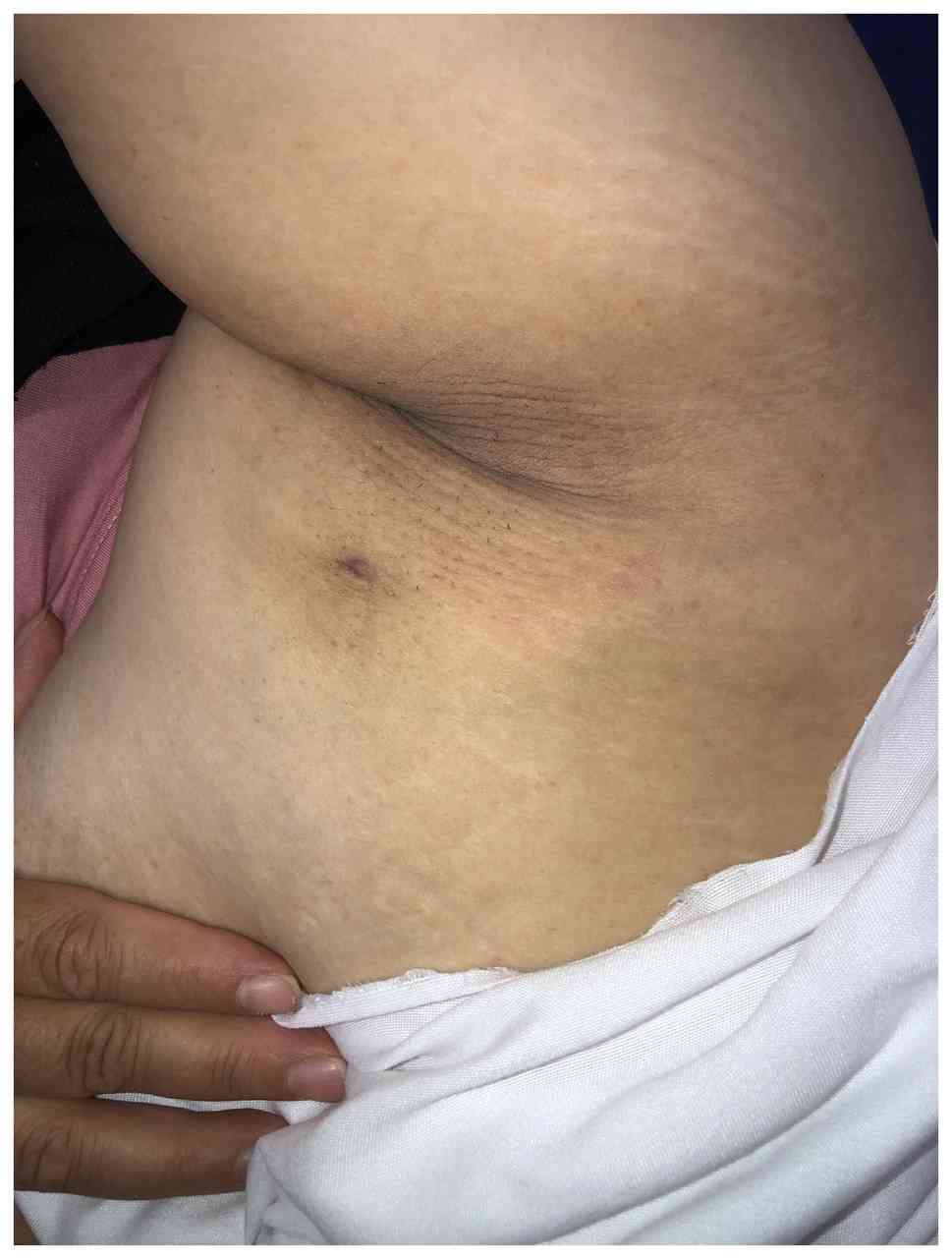
The clinical examination revealed a palpable,
ill-defined area of hardness with a firm consistency and tenderness
upon palpation. Additionally, an axillary breast with a nipple was
noted (Fig. 1).
Diagnostic approach
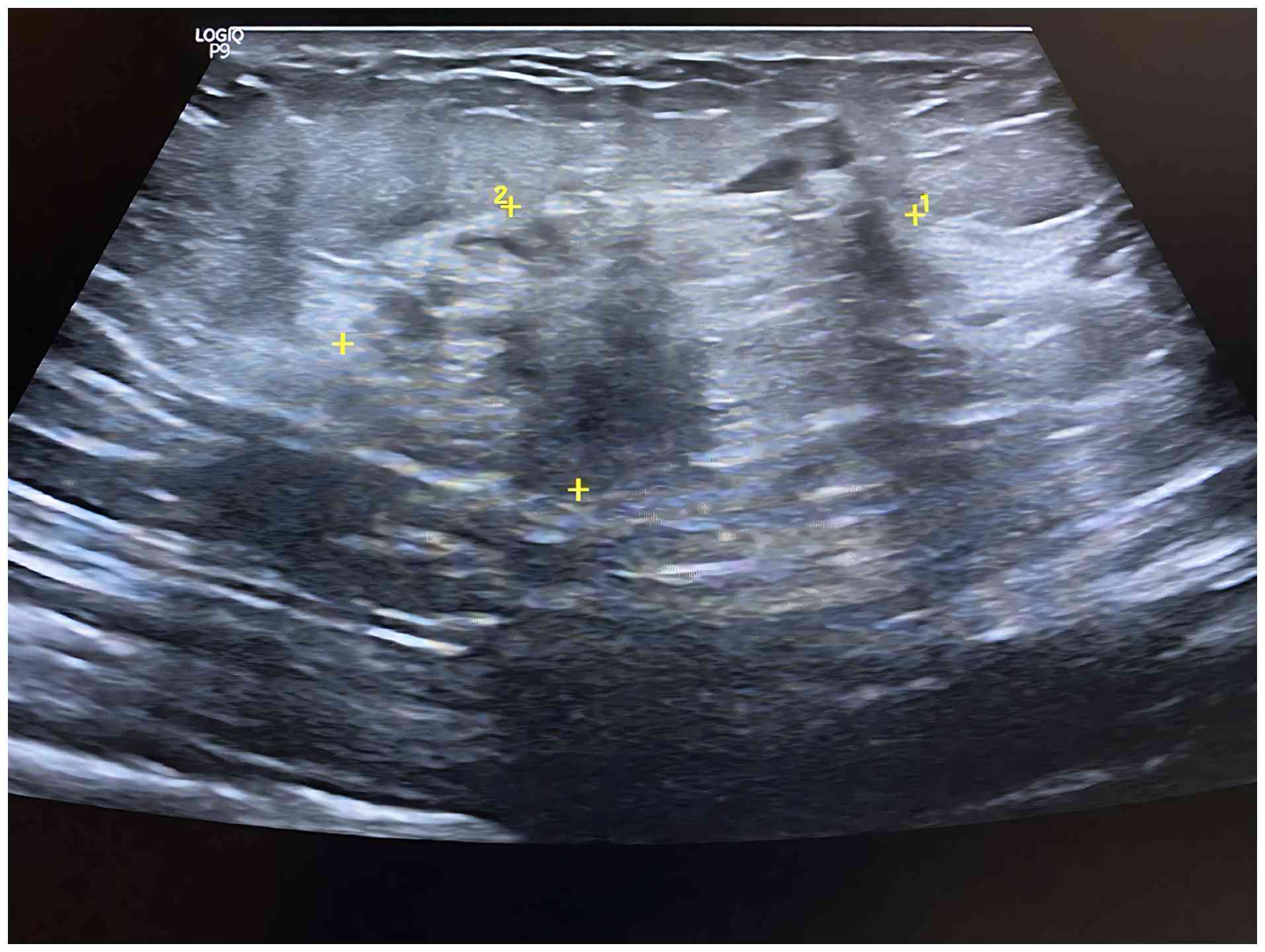
A breast ultrasonography demonstrated bilateral
axillary breast tissue, more prominent on the left side, containing
two distinct heterogeneous collections, the largest measuring 36x9
mm. Mild edema, skin sinuses and non-specific axillary nodes were
also observed. These findings are consistent with chronic mastitis
involving axillary breast tissue (Fig.
2) (1).
Therapeutic intervention
The patient was initially diagnosed with periductal
mastitis and managed medically with a tapering course of oral
corticosteroids (prednisolone 10 mg once daily for 20 days,
followed by 5 mg once daily for an additional 20 days; this was
used to suppress the immune-mediated inflammatory process
underlying GM and to reduce swelling, pain and disease activity),
in combination with amoxicillin (1 g three times daily for 7 days,
to cover potential secondary bacterial infection, which may
complicate the course of GM, particularly when abscesses, fistulae,
or skin involvement are present), cabergoline (0.5 mg once daily
for 2 days, to suppress prolactin secretion) and analgesics
(co-codamol 500 mg, two tablets as needed for pain control). She
demonstrated a good clinical response to this regimen; however, the
condition recurred 1 year later. Following multidisciplinary team
discussion, a wide local excision of the left axillary tail was
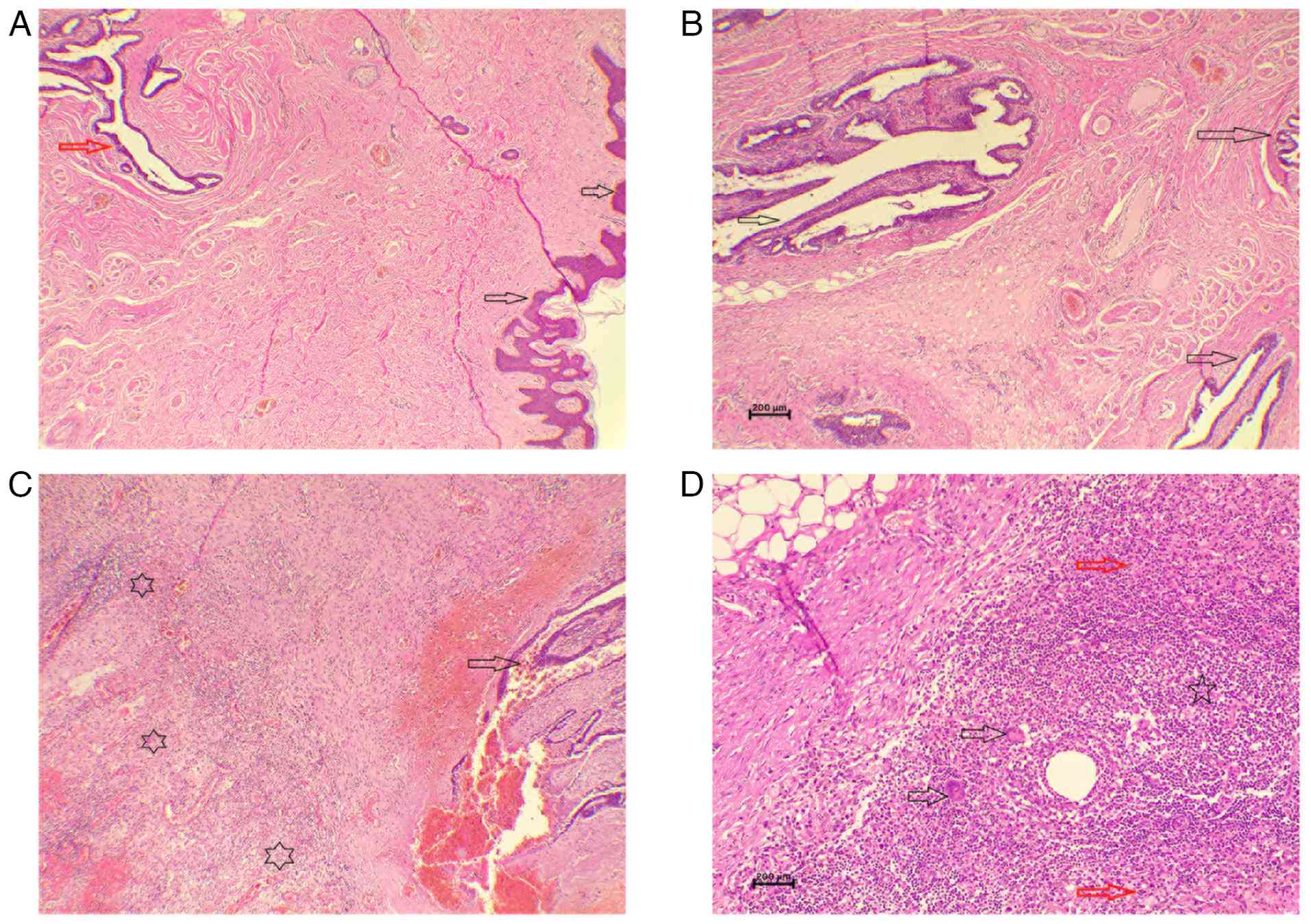
performed. A histopathological analysis of the excised specimen was
performed on 5-µm-thick sections fixed in 10% neutral-buffered
formalin for 24 h, embedded in paraffin, and stained with
hematoxylin and eosin (Bio Optica Co.) for 1-2 min at room
temperature. Examination under a light microscope (Leica
Microsystems GmbH) revealed xanthogranulomatous inflammation
involving the axillary accessory breast tissue, along with benign
lymph nodes showing acute lymphadenitis (Fig. 3).
Follow-up and outcome
At the 2-month follow-up time point, the symptoms of
the patient had markedly improved, with no signs of recurrence. At
the most recent annual follow-up following surgical excision, she
remained in good health and recurrence-free.
Discussion
Accessory breast tissue arises along the embryonic
mammary ridge, extending from the axilla to the pubic region, and
is susceptible to the same pathological conditions as normally
located breast tissue (1). The
frequently reported conditions in accessory breast tissue include
cancer, mastitis, fibroadenomas, phyllodes tumors and fibrocystic
changes (7). The leading hypothesis
regarding the pathogenesis of GM suggests that an autoimmune
response is initiated within the lobules of the breast parenchyma
following ductal injury. This triggers a localized inflammatory
reaction in the connective tissue, promoting the recruitment of
macrophages and lymphocytes, ultimately resulting in a noncaseating
granulomatous response (3).
The influence of ethnicity on GM remains a subject
of debate. Vall et al (3)
reported no specific ethnic predisposition. By contrast, the
studies by Yuan et al (8) and
Deng et al (9) indicated a
higher prevalence of GM in Middle Eastern populations compared to
Western countries. Consistent with the present case, GM
predominantly affects women of reproductive age, particularly those
with a history of breastfeeding. Among the 7 cases reviewed herein,
4 patients had a prior history of breastfeeding, with an average
duration of 22.7 months (Table I)
(1-4,7,10,11).
However, Nakamura et al (7)
and Rajendran et al (10)
documented cases of GM in women without a history of
breastfeeding.
 | Table IRelevant variables of the reviewed
cases. |
Table I
Relevant variables of the reviewed
cases.
| First author, year of
publication | Age, years | Medical history | Use of
contraceptives | No. of
pregnancies | History of
lactation | Duration of lactation
(months) | Affected side | Symptoms | Axillary
involvement | Treatment
approach | Outcome | Follow-up
(years) | (Refs.) |
|---|
| Vall, 2025 | 24 | Unexceptional | No | 1 | Yes | 18 | Left | Erythema, pain and
edema | Yes | Oral corticosteroid
followed by rescue therapy due to poor adherence | A few episodes of
recurrence with subsequent recovery | N/A | (3) |
| Salih, 2024 | 39 | Left breast
granulomatous mastitis | N/A | 3 | Yes | 37 | Right | Right, axillary
discomfort, swelling, redness, fever and chills | Yes | Oral amoxicillin and
clavulanic acid, followed by excisional biopsy | Recovery | 0.5 | (1) |
| Shabani, 2023 | 38 | Unexceptional | No | 2 | Yes | 12 | Right | Painful mass,
thickened skin and warmth | No | Oral
corticosteroid | Recovery | 1 | (11) |
| Nakamura, 2022 | 24 | Unexceptional | N/A | Pregnant at the time
of presentation | No | N/A | Right | Pain and
swelling | Yes | Intravenous
piperacillin, drainage and surgical removal | Recovery | N/A | (7) |
| Oze, 2022 | 42 | Unexceptional | Contraceptive device
after her last child | 5 | N/A | N/A | Right | Swelling, nipple
retraction | Yes | Antibiotic therapy
and wound dressings | Recovery | 0.5 | (4) |
| Alvand, 2022 | 36 | Unexceptional | No | 2 | Yes | 24 | Right | Pain, swelling and
skin thickening | Yes | Prednisone,
naproxen | Recovery | 0.75 | (2) |
| Rajendran, 2019 | 23 | Unexceptional | N/A | 0 | No | N/A | Right | Pain and
swelling | Yes | Oral azithromycin and
oral prednisone | Recovery | N/A | (10) |
Bilateral involvement in GM is rare, as the
condition typically presents unilaterally (1). In the patient in the present study, a
breast ultrasonography identified two distinct heterogeneous
collections within the left axillary breast, accompanied by mild
edema and skin sinuses. These imaging findings were consistent with
the characteristic manifestations of GM, which commonly include
mass formation, skin changes and the development of a sinus tract.
Systemic symptoms, such as fever, remain uncommon in GM cases
(1). Among the cases reviewed
herein, all were unilateral, with fever reported in only 1 patient.
Pain was the reported symptom in 6 cases, whereas erythema was
observed in only 2 cases.
The diagnosis of GM requires a well-coordinated
multidisciplinary approach involving clinicians, radiologists and
pathologists, as demonstrated in the present case report. This is
particularly critical given that cases with clinical deviance or
coexistence with breast cancer have been reported, increasing the
risk of misdiagnosis. Multidisciplinary collaboration not only
helps to avoid such errors, but also facilitates earlier
preoperative diagnosis and ensures the appropriate use of
corticosteroid therapy in selected patients (8,12). Due
to the absence of specific clinical or radiological
characteristics, imaging findings may be non-specific. Mammography
often reveals asymmetric density, while an ultrasound may detect
irregular, heterogeneous masses suggestive of abscesses. However,
these features are not unique to GM and can mimic other breast
pathologies (1).
Although no standardized treatment exists for GM to
date, at least to the best of our knowledge, steroids are
frequently used to reduce lesion size. However, their use is
associated with adverse effects, such as weight gain,
hyperglycemia, Cushing syndrome and opportunistic infections
(7). Additionally, patient
non-adherence can compromise treatment efficacy. Vall et al
(3) reported a case in which poor
adherence led to multiple recurrences, ultimately necessitating
rescue therapy. While the studies by Alvand et al (2) Rajendran et al (10) and Oze et al (4) reported favorable outcomes with
conservative management, the lack of long-term follow-up in these
cases raises concerns about the sustained efficacy and reliability
of conservative treatment strategies.
A previous meta-analysis of 138 cases undergoing
surgery and 358 cases with steroid therapy revealed improved
outcomes with surgery (complete response: 90.6 vs. 71.8%;
recurrence: 6.8% vs. 20.9%) (13).
Combining surgery with steroids further improved results, with a
94.5% complete response rate and a 4.0% recurrence rate (13). A conservative approach was initially
employed for the patient in the present study; however, recurrence
occurred after 1 year. By contrast, wide local excision of the
axillary tail achieved a favorable outcome, with no recurrence
observed at the one-year follow-up.
The case described herein enriches the existing body
of knowledge by elucidating the presentation, complex diagnosis,
treatment options and favorable outcomes of GM in accessory breast
tissue, guiding clinicians in recognizing and managing this rare
condition effectively. However, it is worth mentioning that a
longer period of monitoring would strengthen this report and the
conclusions drawn significantly.
In conclusion, GM can occur in accessory breast
tissue. While corticosteroids may provide favorable short-term
results, they do not necessarily prevent recurrence, whereas
surgical management may offer more durable long-term outcomes.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
ZDH and AMS were major contributors to the
conception of the study, as well as to the literature search for
related studies. HOA, MKA and HHF were involved in the literature
review, in the design of the study, and in the writing of the
manuscript. SOA, SLT, MMA and FHK were involved in the literature
review, in the design of the study, in the critical revision of the
manuscript, analyzing patient data, and the processing of the
table. LRAP was the radiologist who assessed the case. AMA was the
pathologist who performed the diagnosis of the case. FHK and MMA
confirm the authenticity of all the raw data. All authors have read
and approved the final manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from the
patient for their participation in the present study.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the present case report and any
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Salih AM, Pshtiwan LR, Latif S, Ali HO,
Abdullah AM, Baba HO, Hama JI, Hassan SH, Hassan MN, Mohammed SH,
et al: Granulomatous mastitis in accessory breast tissue: A rare
presentation and surgical management. Biomed Rep.
20(62)2024.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Alvand S, Hessami A, Kiani L, Makhmalbaf
AO and Elahi A: Uncommon location of idiopathic granulomatous
mastitis: A case report: Uncommon Location of IGM. Arch Breast
Cancer. 9:320–324. 2022.
|
|
3
|
Vall E, Araya V, Tortajada L, Escobedo V,
Nogueiras R and Del Riego J: Idiopathic granulomatous mastitis
after mRNA vaccination against COVID-19: A possible association?
BJR Case Rep. 11(uaae048)2025.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Oze KR, Yehouenou Tessi RT, Mendes P,
Allali N, Chat L and El Haddad S: Granulomatous mastitis: A case
report. SAGE Open Med Case Rep.
10(2050313X221146671)2022.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Abdullah HO, Abdalla BA, Kakamad FH, Ahmed
JO, Baba HO, Hassan MN, Bapir R, Rahim HM, Omar DA, Kakamad SH, et
al: Predatory publishing lists: A review on the ongoing battle
against fraudulent actions. Barw Med J. 2:26–30. 2024.
|
|
6
|
Prasad S, Nassar M, Azzam AY,
García-Muro-San José F, Jamee M, Sliman RKA, Evola G, Mustafa AM,
Abdullah HO, Abdalla BA, et al: CaReL Guidelines: A consensus-based
guideline on case reports and literature review (CaReL). Barw Med
J. 2:13–19. 2024.
|
|
7
|
Nakamura J, Tanaka F, Ohtaka K, Sato K and
Iyama A: A rare case of granulomatous mastitis in the accessory
axillary breast of a pregnant woman successfully treated by
surgery. Eur J Breast Health. 18(195)2022.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Yuan QQ, Xiao SY, Farouk O, Du YT,
Sheybani F, Tan QT, Akbulut S, Cetin K, Alikhassi A, Yaghan RJ, et
al: Management of granulomatous lobular mastitis: An international
multidisciplinary consensus (2021 edition). Mil Med Res.
9(20)2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Deng Y, Xiong Y, Ning P, Wang X, Han XR,
Tu GF and He PY: A case management model for patients with
granulomatous mastitis: A prospective study. BMC Women's Health.
22(143)2022.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Rajendran D, See CB, Wan WM and Teik CY:
Chronic granulomatous mastitis with axillary lymphadenopathy in a
nulliparous woman. Med J Malaysia. 74:564–565. 2019.PubMed/NCBI
|
|
11
|
Shabani S, Sadeghi B, Zarinfar N and
Sarmadian R: Idiopathic granulomatous mastitis: A case report and
literature review. Clin Case Rep. 11(e7819)2023.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Salih AM, Latif S, Ali RM, Pshtiwan LR,
Ali HO, Abdullah AM, Salih KM, Hassan SH, Nasralla HA, Hussein BO
and Kakamad FH: Granulomatous mastitis co-existing with breast
cancer: A case report and mini-review of the literature. World Acad
Sci J. 7(101)2025.
|
|
13
|
Lei X, Chen K, Zhu L, Song E, Su F and Li
S: Treatments for idiopathic granulomatous mastitis: Systematic
review and meta-analysis. Breastfeed Med. 12:415–421.
2017.PubMed/NCBI View Article : Google Scholar
|