Introduction
Mantle cell lymphoma (MCL) is a mature B-cell
neoplasm derived from the mantle zone of lymphoid follicles and is
typically composed of small- to medium-sized monomorphic cells. Its
diagnostic characteristics include the t(11;14)(q13;q32)
translocation and cyclin D1 overexpression, the former causing the
latter (1,2). MCL usually involves the lymph nodes;
however, extranodal involvement is also common, particularly in
Waldeyer's ring and the gastrointestinal tract, spleen and bone
marrow. Other organs that may be affected include the skin,
endocrine glands, lungs and central nervous system, with these
sites most commonly affected by relapsing disease (1). In addition, a wide variety of
extranodal lesions, such as submandibular duct and endobronchial
lesions, have been reported in recent years (3,4).
However, in rare cases, extranodal MCL has arisen in the ocular
adnexa, soft tissue and heart. The present study report the case of
a patient with MCL, which demonstrated metachronous extranodal
recurrence in the conjunctiva, soft tissue and right atrium. The
clinical characteristics of the disease at each site, as well as
the treatment course are described.
Case report
A 75-year-old male patient with a history of
systemic MCL presented with right cervical and supraclavicular
lymph node swelling, and was referred to the Osaka General Hospital
of West Japan Railway Company in July, 2018. His MCL was first
diagnosed 10 years prior (December, 2007), and remission had been
achieved with chemotherapy, involving rituximab, cyclophosphamide,
vincristine, doxorubicin and dexamethasone. A physical examination
did not reveal any other superficial lymph node swelling. The
performance status of the patient was categorized as 0 according to
the Eastern Cooperative Oncology Group performance status scale.
Laboratory examinations revealed a white blood cell count of
4.2x109/l, a hemoglobin concentration of 13.5 g/dl, a
platelet count of 209x109/l, a lactate dehydrogenase
level of 191 U/l (reference range, 106-211 U/l) and a soluble
interleukin-2 receptor level of 405 U/ml (reference range, 145-519
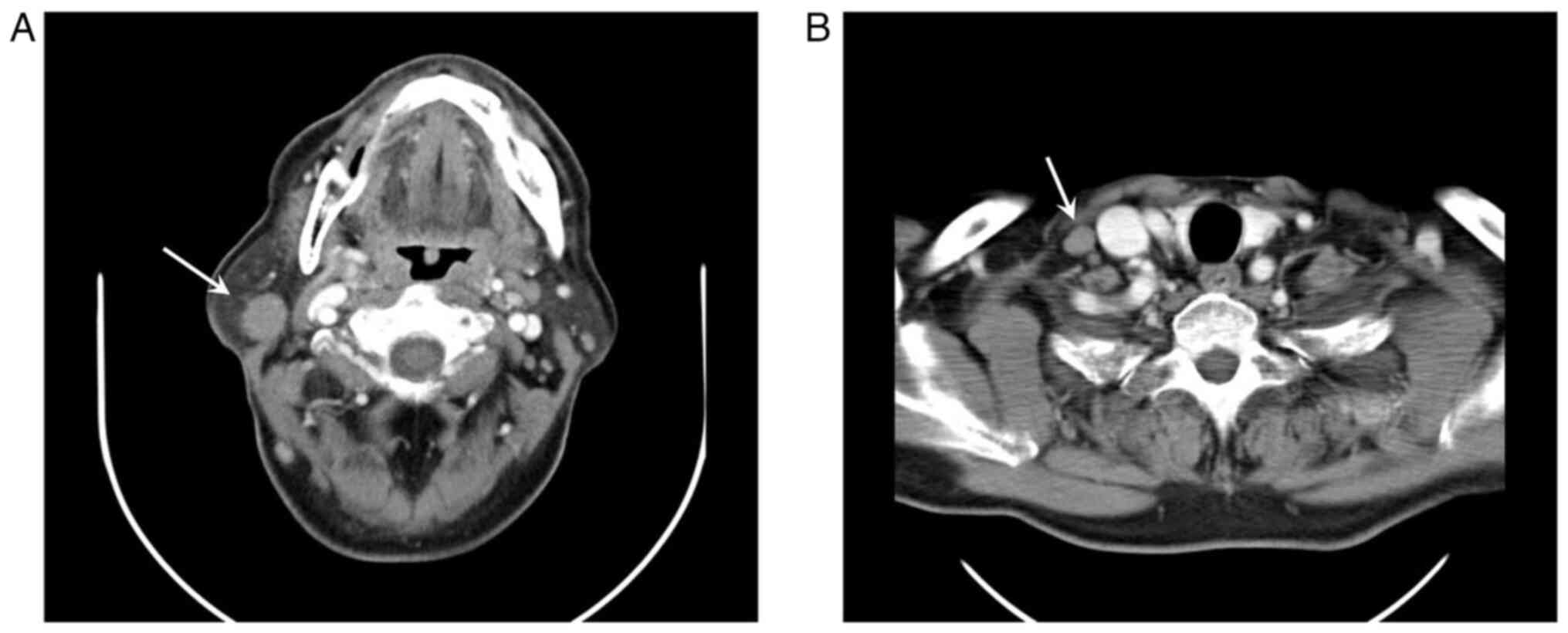
U/ml). On a computed tomography (CT) scan, cervical and
supraclavicular lymph node swelling were observed (Fig. 1); however, no disease, including
splenomegaly, was found at other sites. A biopsy of the swollen
cervical lymph node demonstrated the massive proliferation of
monotonous lymphoid cells with irregular nuclear contours. The mass
blocks were fixed in a solution containing 10% formaldehyde
(Yuaikasei Co., Ltd.) in 0.01 M phosphate-buffered saline (Muto
Pure Chemicals Co., Ltd.) for 2 h at room temperature. Following
fixation, the tissue blocks were loaded into the
Tissue-Tek® TEC 6 (Sakura Finetek Japan Co., Ltd.) and
subsequently embedded in paraffin. Formalin-fixed paraffin-embedded
sections were cut (3-µm-thick) using a YAMATO REM-710 microtome
(Yamato Kohki Industrial Co., Ltd.). The subsequent dewaxing
process included sequential treatments with xylene, anhydrous
ethanol, a decreasing concentration gradient of ethanol, and water.
Following this, the sections were immersed in hematoxylin staining
solution (Muto Pure Chemicals Co., Ltd.) for 5 min at room
temperature and then differentiated with 0.3% acid alcohol before
being incubated with 0.6% ammonia for 1 min at room temperature.
Eosin staining solution (Muto Pure Chemicals Co., Ltd.) was applied
for 3 min, followed by dehydration with ethanol and xylene.
Finally, the samples were mounted with neutral gum to prepare the
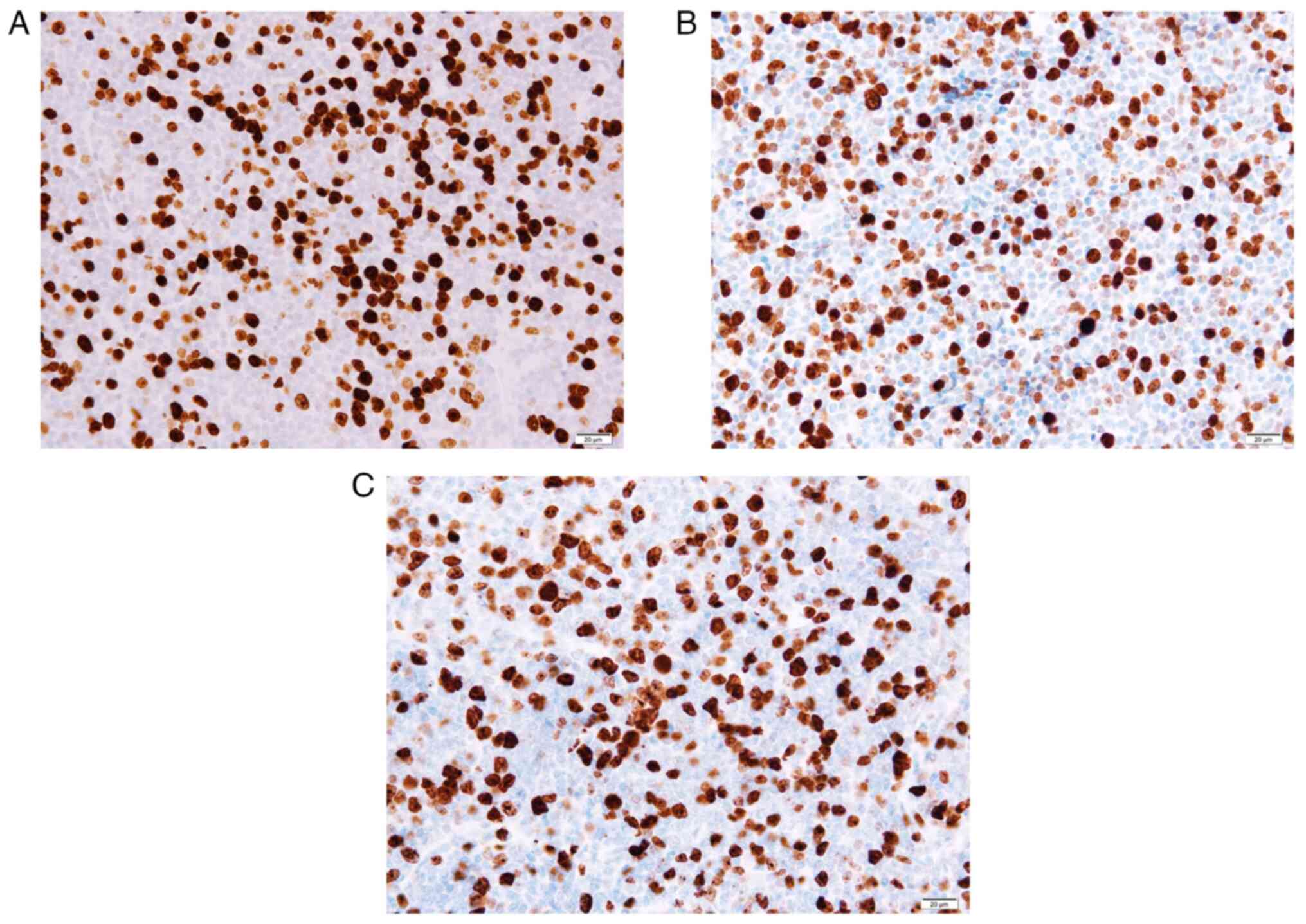
slides. Immunohistochemical staining revealed that the lymphoid
cells were positive for Bcl-2 (cat. no. 413141; Nichirei
Biosciences, Inc.), CD5 (cat. no. 413251; Nichirei Biosciences,
Inc.), CD79a (cat. no. 413161; Nichirei Biosciences, Inc.), CD20
(cat. no. 760-2531; Roche Diagnostics) and cyclin D1 (cat. no.
413521; Nichirei Biosciences, Inc.) and negative for CD10 (cat. no.
413261; Nichirei Biosciences, Inc.) and CD3 (cat. no. 413591;
Nichirei Biosciences, Inc.). Ki-67 (cat. no. 760-4286; Roche
Diagnostics) staining stained >20% of the cells with varying
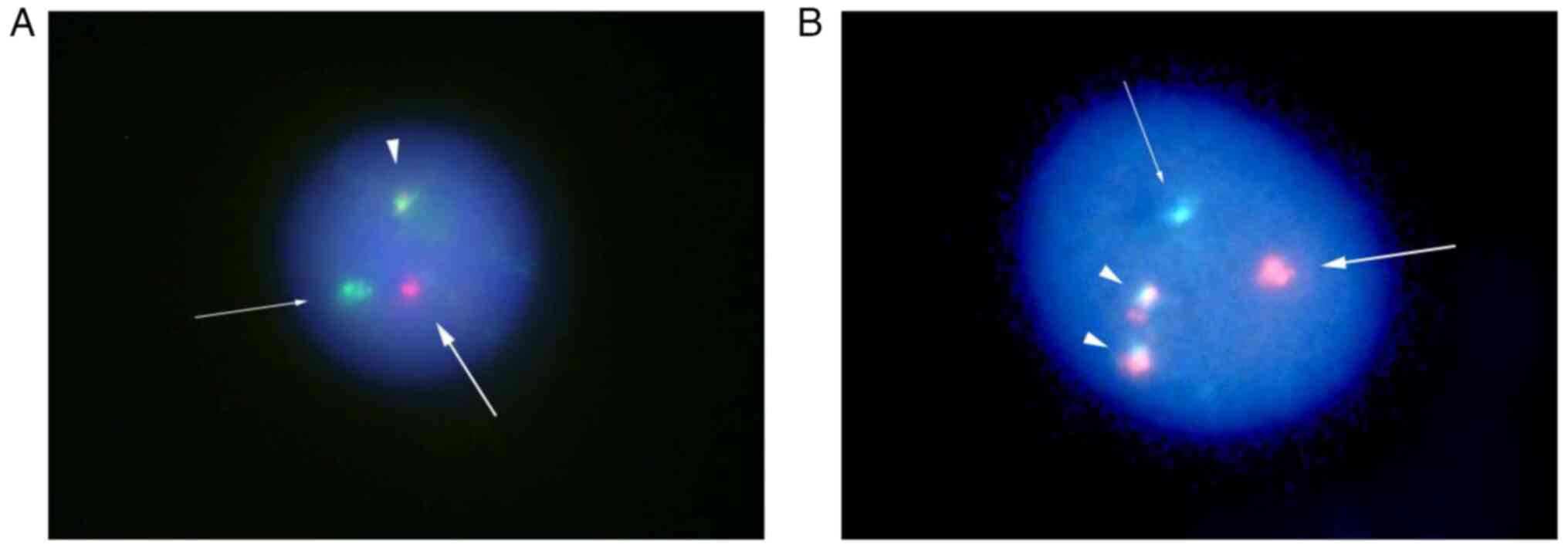
intensity (Fig. 2). Fluorescence
in situ hybridization (FISH) analysis was not performed due
to a lack of tissue samples. A pathological diagnosis of relapse of
known MCL was made. A bone marrow examination did not demonstrate
any evidence of bone marrow invasion. At this time, the MCL
international prognostic index (MIPI) score of the patient was
calculated as ~5.9954, indicating that he was in the intermediate
risk group (5). Since the patient
had stage II disease, he was subjected to radiotherapy. Volumetric
modulated arc therapy (2 Gy x 20 fractions) resulted in complete
remission. At 1 year following radiotherapy (October, 2019), he
presented with right conjunctival swelling. No ophthalmological
symptoms other than discomfort, such as pain, vision loss,
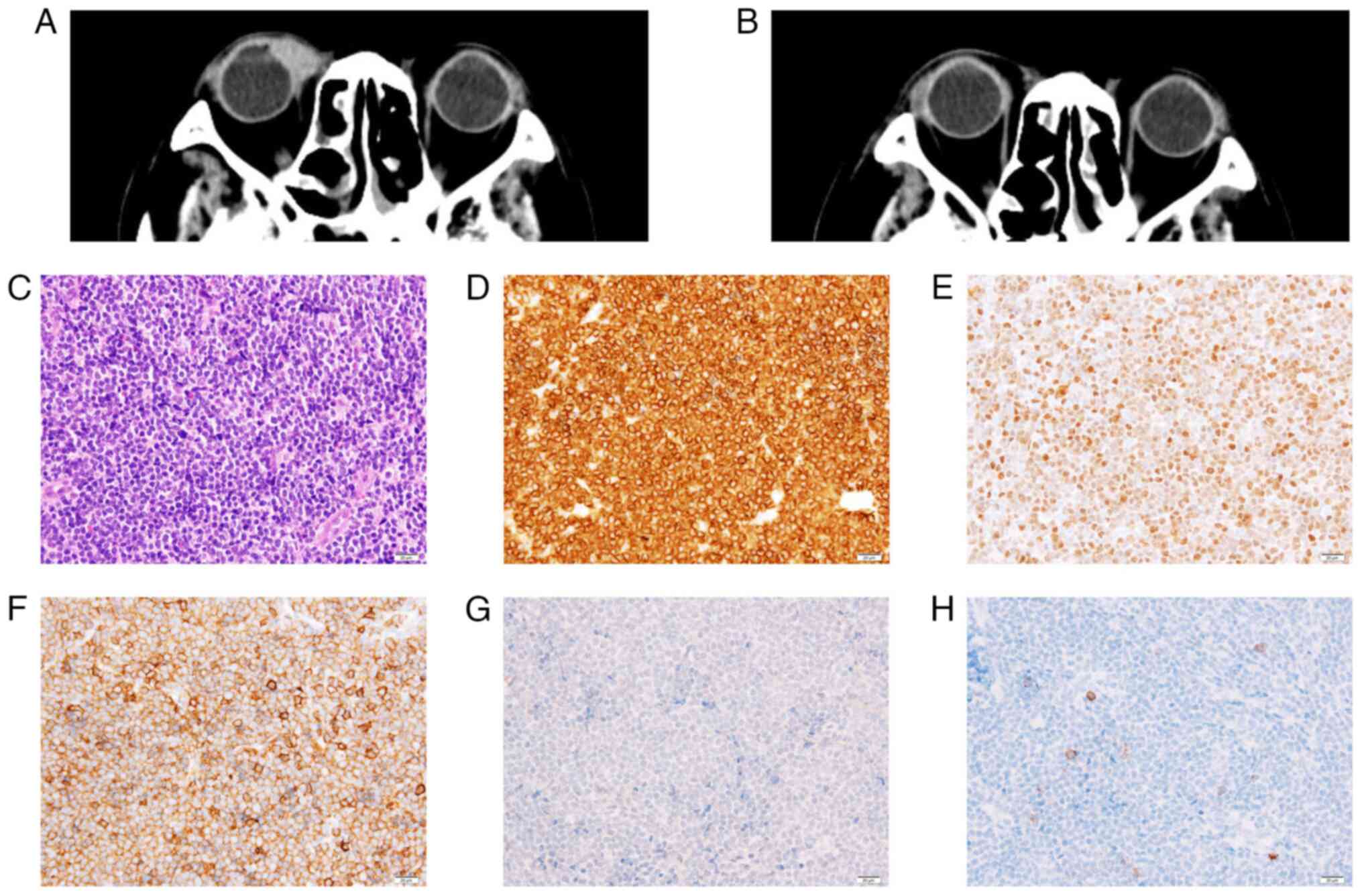
exophthalmos, or epiphora, were observed. A CT scan demonstrated an
enlarged right conjunctiva. An excisional biopsy of the conjunctiva
was performed, which revealed the diffuse infiltration of
monotonous lymphocytes. Phenotypically, they were positive for CD5,
Bcl-2, Ki-67 and cyclin D1, but negative for CD10 and CD23 (cat.
no. 413611; Nichirei Biosciences, Inc.), and these findings
confirmed the diagnosis of relapsed MCL (Figs. 2 and 3). Bone marrow aspiration, a whole-body CT
scan and fluorodeoxyglucose-positron emission tomography (FDG-PET)
did not identify any other disease. The patient was commenced on
external-beam radiotherapy (2 Gy daily up to 40 Gy in 4 weeks),
which led to complete remission.
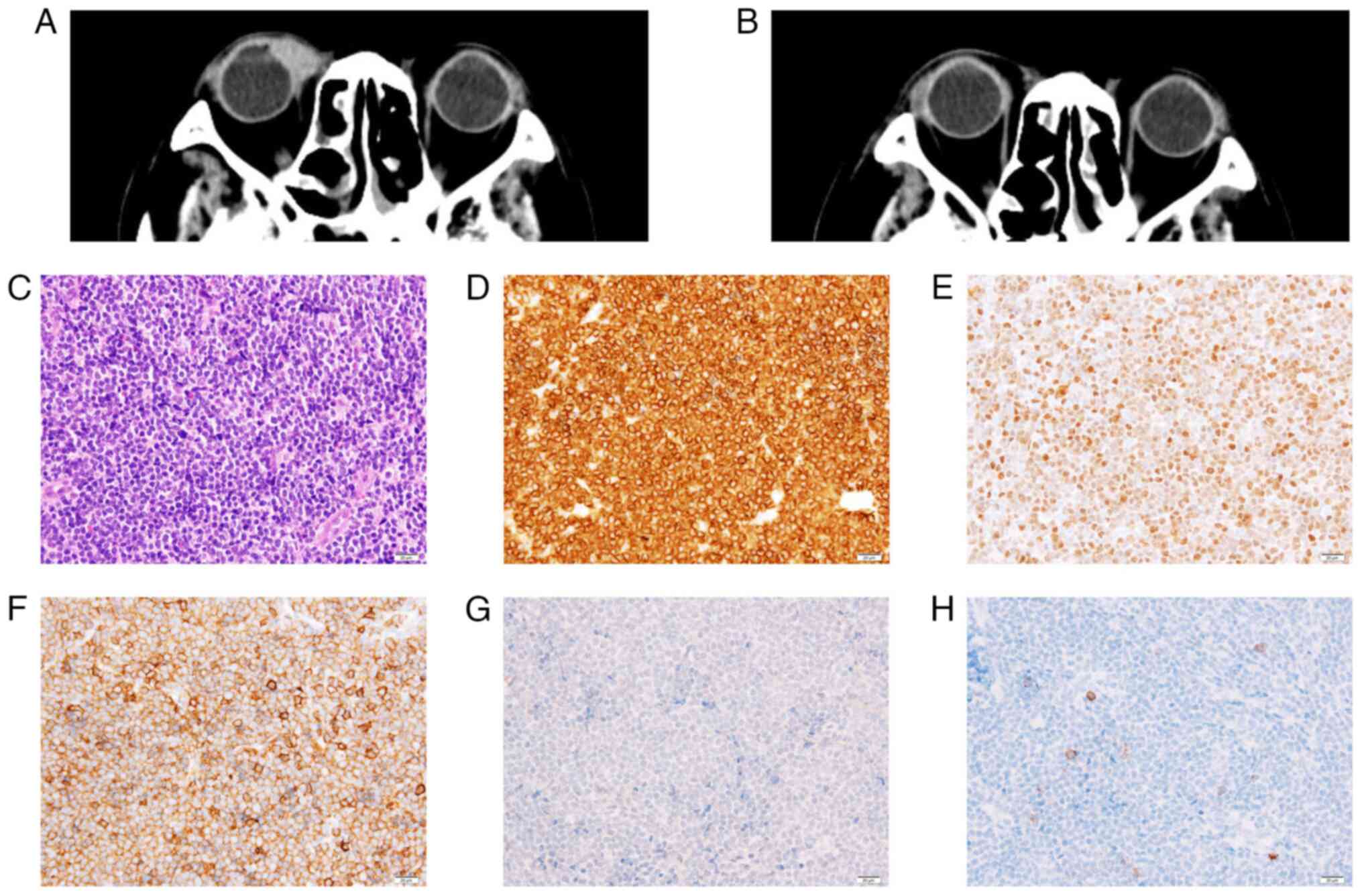 | Figure 3(A) Computed tomography scan
illustrating a mass in the right orbit. (B) Following radiotherapy,
the mass disappeared. (C) The conjunctival mass was composed of
diffuse, dense sheets of atypical cells (hematoxylin and eosin
staining; magnification, x400). The abnormal cells were
immunopositive for (D) Bcl-2 (magnification, x400), (E) cyclin D1
(magnification, x400), and (F) CD5 (magnification, x400), and
negative for (G) CD10 (magnification, x400), and (H) CD23
(magnification, x400). |
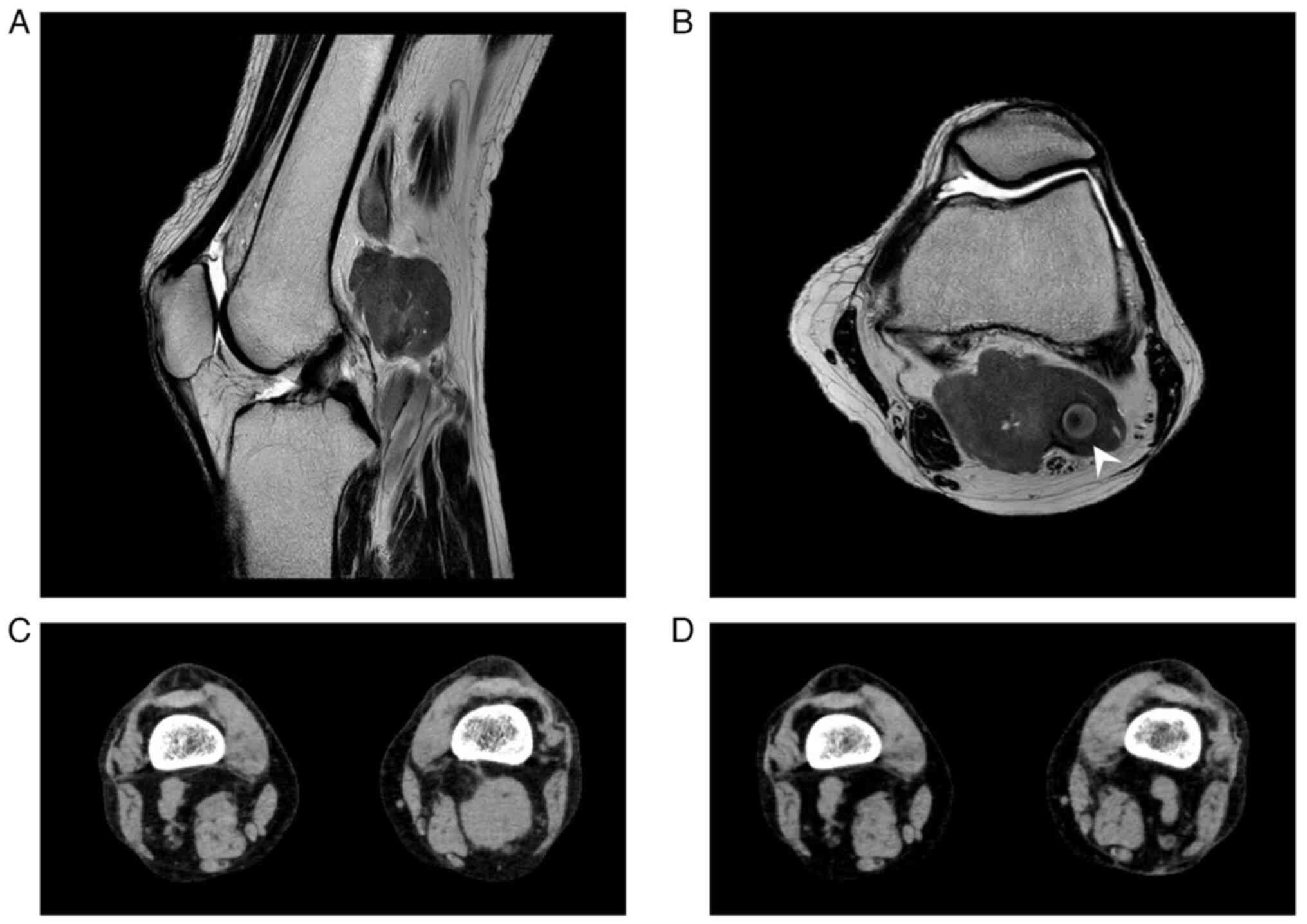
In February, 2022, the patient complained of a
painless mass in the left popliteal fossa. Magnetic resonance
imaging (MRI) of the left knee revealed a lesion of 54x34 mm in
size localized in the popliteal fossa, which exhibited intermediate
signal intensity on T1- and T2-weighted images (Fig. 4). A surgical biopsy of the popliteal
mass was performed and demonstrated the same pathological findings
as the previous examination of the conjunctival mass, and Ki-67
staining produced a positive result (Fig. 2). FISH of interphase nuclei detected
CCND1/IGH fusion signals using CCND1/IGH fusion probe (Vysis
IGH/CCND1 XT Dual Color, Dual Fusion FISH Probe kit; Abbott
Molecular Inc.) in 949 of the 1,000 analyzed cells (Fig. 5). Hence, the patient was diagnosed
with recurrent MCL. FDG-PET revealed FDG accumulation in the
popliteal mass, and a bone marrow examination revealed no evidence
of bone marrow involvement; therefore, the disease was diagnosed as
stage I. Since the disease had recurred twice, chemotherapy was
suggested as a suitable therapeutic strategy; however, the patient
preferred radiotherapy. Thereafter, external-beam radiotherapy (2
Gy x 20 fractions) was performed, resulting in complete remission,
which lasted for 2 years.
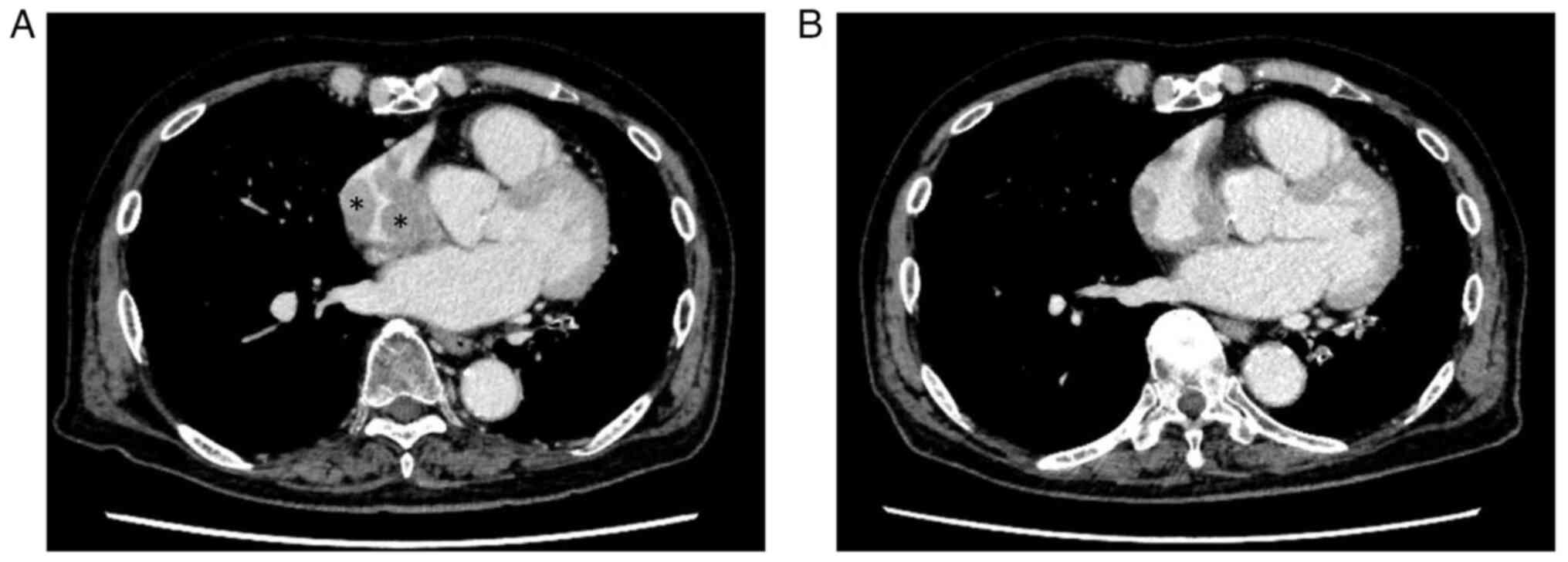
Although the patient remained well for ~2 years
following radiotherapy for the popliteal mass (January, 2025), he
subsequently developed swollen preauricular and cervical lymph
nodes. A CT scan demonstrated no abnormal findings in the
conjunctiva or popliteal fossa; however, a right atrial mass was
newly found in addition to the swollen preauricular and cervical
lymph nodes (Fig. 6). An FDG-PET
scan also demonstrated positivity at the same sites. Although
transthoracic echocardiography was performed, the right atrial mass
could not be detected. An electrocardiography demonstrated a sinus
rhythm with supraventricular premature contraction; i.e., there was
no change from previous examinations. FISH of the bone marrow cells
of the patient using the CCND1/IGH fusion probe revealed fusion
signals in 12 interphase nuclei out of 1,000 analyzed cells
(Fig. 5). Therefore, a diagnosis of
recurrent MCL was made, and the disease was staged as stage IV.
Since the bone marrow examination had confirmed the presence of
recurrent disease, no re-biopsy of the lymph nodes was performed.
The patient was commenced on ibrutinib therapy (140 mg/day), and
the swollen preauricular and cervical lymph nodes shrank rapidly.
In addition, a CT scan demonstrated a significant reduction in the
size of the right atrial mass within 4 months (Fig. 6). The patient continues to exhibit a
partial remission and is currently receiving ibrutinib
monotherapy.
Discussion
The present study described the case of a patient
with MCL; the patient presented with metachronous extranodal
recurrences, involving the conjunctiva, soft tissue and right
atrium. The conjunctival and soft-tissue lesions were
pathologically evaluated by re-biopsies, and radiotherapy was
beneficial. The most recent recurrence, involving the right atrium,
was successfully treated with a tyrosine kinase inhibitor.
Ocular adnexal lymphoma is considered to be
relatively rare, accounting for ~3% of extranodal non-Hodgkin
lymphomas. On the other hand, lymphoma is one of the most common
malignancies in the ocular adnexa, accounting for up to 55% of all
primary malignancies in the orbit (6). As for the pathological subtype,
according to the largest published study of ocular adnexal lymphoma
(involving 353 cases), MCL is rare and comprises only 5% of ocular
adnexal lymphomas (7). In these
cases, secondary MCL affected the ocular adnexal region more
commonly (63%) than primary (37%) MCL (7). As regards the therapeutic strategy,
localized ocular adnexal lymphoma is generally treated with
external-beam radiotherapy, while systemic disease is treated with
chemoimmunotherapy alone or combined with radiotherapy.
Radiotherapy is the standard treatment for isolated conjunctival
lymphoma and this results in 5-year local control rates >80%.
Although the optimal radiotherapy dose is unclear, doses >35 Gy
exacerbate post-treatment toxicity and morbidity, while low,
fractionated doses alleviate them (8). Concerning the survival rate, a previous
study suggested that the 5-year disease-specific survival rates of
patients with primary ocular adnexal MCL, systemic MCL with
involvement of the ocular adnexa and relapsed systemic MCL in the
ocular adnexal region did not differ (5-year disease-specific
survival rate, 38%) (9). Although
the disease recurred at different extranodal sites from the
previous lesion in the case presented herein, administering
radiotherapy at a dose of 40 Gy resulted in long-term local control
since the disease only recurred in the conjunctiva.
As regards soft-tissue lymphoma, it is characterized
by the disease growing within the soft tissue, which includes the
connective tissue, adipose tissue and skeletal muscle. In a
previous study, it reported to account for ~0.1% of all malignant
lymphomas, although that study was limited to primary soft-tissue
lymphomas (10). In a recent study,
Trutzer and Lossos (11) described 4
cases of relapsed MCL affecting the soft tissue of the extremities.
These 4 cases represented 0.85% of the MCL cases treated at their
institution, highlighting the rarity of such cases (11). As regards diagnosis, several studies
have suggested the usefulness of MRI for diagnosing soft-tissue
lymphoma, e.g., lymphomas were found to be uniformly enhanced,
exhibiting high signal intensity on T2-weighted imaging and
intermediate intensity on T1-weighted images (12,13). On
the other hand, a previous review that included both the
abovementioned case series and previously reported cases described
inconsistent MRI results (13). In
the case in the present study, the internal MRI signals of the left
popliteal fossa tumor were homogenous, and the tumor demonstrated
intermediate signal intensity on T1-weighted images; however, the
fact that the signal intensity of the tumor was not high on
T2-weighted images was atypical. Therefore, it was considered that
pathological diagnosis based on re-biopsy is preferable for
improving the accuracy of diagnosis.
As for cardiac lymphoma, a single-center analysis of
cardiac lymphoma was recently reported (14). Lymphomatous involvement in the heart
was only found in 6 patients (1.5%; 5 patients with diffuse large
B-cell lymphoma and 1 patient with B-cell lymphoma) among 394
patients who underwent echocardiography prior to chemotherapy
(14). However, transthoracic
echocardiography only has 60% sensitivity for detecting cardiac
involvement (15), and in the case
present herein, the cardiac mass could not be detected using
echocardiography; hence, it was hypothesized that the actual
incidence of the disease may be higher than reported. Concerning
pathological diagnosis, it has been reported that diffuse large
B-cell lymphoma, T-cell lymphoma and Burkitt lymphoma are the most
common pathological diagnoses, in that order (16). There have been several reported cases
of cardiac MCL similar to the present case report; Futela et
al (17), who cited data from
Surveillance, Epidemiology and End Results, mentioned the rarity of
cardiac MCL. Anatomically, it has been reported that the right
atrium, which was also affected in the case presented herein, is
the most common location for cardiac MCL (15,18). In
addition, Kudo et al (18)
demonstrated that surgery is desirable to avoid the risk of a
pulmonary embolism caused by the mass since cardiac lymphoma most
frequently involves the right atrium. In the case in the present
study, a CT scan only demonstrated the thickening of the right
atrial wall; therefore, the continuation of ibrutinib treatment was
possible without the concern of causing the mass to become
dislodged as it shrank, resulting in rapid, safe and successful
treatment. It is suggested that a therapeutic strategy including
ibrutinib should be considered for the treatment of patients with
cardiac MCL, particularly elderly patients and/or patients with a
poor performance status, for whom surgery is not indicated.
Finally, as regards pathological evaluations, the
positivity rate of Ki-67 immunohistochemistry is an independent
prognostic factor distinct from the four MIPI factors, and a
prognostic index that includes the Ki-67 positivity rate has also
been proposed (5). In addition,
aggressive MCL is characterized by rapid progression, frequent
extranodal disease and a high Ki-67 positivity rate (19). In the case presented herein, although
the Ki-67 positivity rate did not increase over time, which would
suggest clonal evolution, Ki-67 positivity had been consistently
observed since 2018, when a pathological evaluation became
possible. The main limitation of the present case report was that
it was not possible to demonstrate the possibility of clonal
evolution through metachronous recurrence using FISH or Ki-67
positivity. However, it is considered that careful surveillance,
including for the possibility of extranodal recurrence, is
necessary when Ki-67 positivity is present, as demonstrated in the
present case report.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
MM and DA designed the study. MM wrote the original
manuscript. DM and SN performed the laboratory analysis of the
specimens of the patient described in the study. DM, SN and KRK
conducted a critical literature review, and also contributed to the
acquisition, analysis and interpretation of the patient's data;
they also contributed to the drafting of the Discussion section.
MM, DA and KRK confirm the authenticity of all the raw data. All
authors have read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
The present study was conducted in accordance with
the ethical standards of the Declaration of Helsinki 1964 and its
later amendments. Written informed consent was obtained from the
patient for his participation in the present case report.
Patient consent for publication
Written informed consent was obtained from the
patient for the case information and images to be published in the
present case report.
Competing interests
All authors declare that they have no competing
interests.
References
|
1
|
Klapper W, Ferry JA, Hermine O, Li S,
Lossos IS, Medeiros LJ, Naresh KN, Rosenquist R, Rule S and
Stilgenbauer S: Mantle cell lymphoma. In: WHO classification of
tumours. Vol 11. 5th edition. International Agency for Research on
Cancer, Lyon, pp446-452, 2024.
|
|
2
|
Siebert R and Aukema SM: Mature B- and
T-cell neoplasms and Hodgkin lymphoma. In: Cancer Cytogenetics:
Chromosomal and Molecular Genetic Aberrations of Tumor Cells. Heim
S and Mitelman F (eds). 4th editioin. Wiley Blackwell, Hoboken, NJ,
pp252-331, 2015.
|
|
3
|
Muscelli S, Shah SS and Bigcas JL:
Extranodal manifestation of mantle cell lymphoma in the
submandibular duct: A case report and review of literature.
Otolaryngol Case Rep. 26(100498)2023.
|
|
4
|
Ding YZ, Tang DQ and Zhao XJ: Mantle cell
lymphoma with endobronchial involvement: A case report. World J
Clin Cases. 10:2604–2609. 2022.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Hoster E, Dreyling M, Klapper W,
Gisselbrecht C, van Hoof A, Kluin-Nelemans HC, Pfreundschuh M,
Reiser M, Metzner B, Einsele H, et al: A new prognostic index
(MIPI) for patients with advanced-stage mantle cell lymphoma.
Blood. 111:558–565. 2008.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Kirkegaard MK: Ocular adnexal lymphoma:
Subtype-specific clinical and genetic features. Acta Ophthalmol.
100 (Suppl 270):S3–S37. 2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ferry JA, Fung CY, Zukerberg L, Lucarelli
MJ, Hasserjian RP, Preffer FI and Harris NL: Lymphoma of the ocular
adnexa: A study of 353 cases. Am J Surg Pathol. 31:170–184.
2007.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tanenbaum RE, Galor A, Dubovy SR and Karp
CL: Classification, diagnosis, and management of conjunctival
lymphoma. Eye Vis (Lond). 6(22)2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Knudsen MKH, Rasmussen PK, Coupland SE,
Esmaeli B, Finger PT, Graue GF, Grossniklaus HE, Khong JJ, McKelvie
PA, Mulay K, et al: Clinicopathological features of ocular adnexal
mantle-cell lymphoma in an international multicenter cohort. JAMA
Ophthalmol. 135:1367–1374. 2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Travis WD, Banks PM and Reiman HM: Primary
extranodal soft tissue lymphoma of the extremities. Am J Surg
Pathol. 11:359–366. 1987.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Trutzer IM and Lossos IS: Relapsed mantle
cell lymphoma manifesting with soft tissue tumors of the
extremities: University of Miami experience and review of the
literature. Ann Hematol. 103:4581–4588. 2024.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Chun CW, Jee WH, Park HJ, Kim YJ, Park JM,
Lee SH and Park SH: MRI features of skeletal muscle lymphoma. AJR
Am J Roentgenol. 195:1355–1360. 2010.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Spinnato P, Chiesa AM, Ledoux P, Kind M,
Bianchi G, Tuzzato G, Righi A and Crombé A: Primary soft-tissue
lymphomas: MRI features help discriminate from other soft-tissue
tumors. Acad Radiol. 30:285–299. 2023.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Ebina T, Sano Y, Hirabayashi M, Tsurumi T,
Watanabe M, Furukawa M, Matsuo W, Nagasawa H, Hirose H, Horii M, et
al: Echocardiographic findings of malignant lymphoma with cardiac
involvement: A single-center retrospective observational study.
Intern Med. 63:359–364. 2024.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Ikeda H, Nakamura S, Nishimaki H, Masuda
K, Takeo T, Kasai K, Ohashi T, Sakamoto N, Wakida Y and Itoh G:
Primary lymphoma of the heart: Case report and literature review.
Pathol Int. 54:187–195. 2004.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Gordon MJ, Danilova O, Spurgeon S and
Danilov AV: Cardiac non-Hodgkin's lymphoma: Clinical
characteristics and trends in survival. Eur J Haematol. 97:445–452.
2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Futela P, Shabtaie SA, Woelber TJ, Poddar
A, Deshmukh AJ and Kowlgi GN: Mantle cell lymphoma with cardiac
involvement presenting as complete heart block. JACC Case Rep.
29(102416)2024.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Kudo H, Shiroshita K, Shiozawa Y, Fujita
S, Sakamoto M, Nakamura N, Nakanishi K and Toyama T: Autopsy case
of cardiac mantle cell lymphoma presenting with recurrent pulmonary
tumor embolism after chemotherapy. J Clin Exp Hematop. 64:242–251.
2024.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Wilson MR, Barrett A, Cheah CY and Eyre
TA: How I manage mantle cell lymphoma: Indolent versus aggressive
disease. Br J Haematol. 201:185–198. 2023.PubMed/NCBI View Article : Google Scholar
|