Introduction
Parathyroid adenomas (PAs) are the most common cause
of primary hyperparathyroidism (HPT), an endocrine disorder that
frequently leads to hypercalcemia of varying severity based on the
progression of the condition (1).
Complications affecting the heart, kidneys, and bones, as well as a
tendency for peptic ulcer disease, are frequently linked to primary
HPT. In rare instances, hypercalcemia can escalate into a
hypercalcemic crisis, a critical emergency requiring immediate
medical attention (2).
Ectopic parathyroid glands occur from abnormal
migration during early development, with an incidence of ~2 to 43%.
Ectopic inferior parathyroid glands are most commonly located in
the anterior mediastinum, often associated with the thymus or
thyroid gland. By contrast, ectopic superior parathyroid glands are
typically found in the tracheoesophageal groove or the
retroesophageal region (3). The PAs
can be located posterior to the thyroid lobes or in ectopic
locations. Intrathyroidal PAs are relatively rare, accounting for 1
to 6% of all PA cases. Despite their rare occurrence, they can
present diagnostic challenges that complicate management (4).
In patients with thyroid nodules and abnormal
parathyroid-related laboratory findings, the suspicion of an
intrathyroidal parathyroid may arise (5). Parathyroid imaging techniques have
advanced, providing for more precise localization for surgery. In
the case of intrathyroidal PAs, ultrasound (US) is the preferred
imaging modality (6).
The standard treatment for primary HPT is the
surgical removal of the PA (7). In
recent years, advancements in thermal ablation technology have led
to the use of microwave ablation (MWA) and other techniques, such
as radiofrequency ablation (RFA) and laser ablation, in treating
HPT. These methods have proven to be safe and effective for
managing primary HPT in patients who are either ineligible for
surgery or who do not opt to undergo surgical intervention
(8).
The present study describes a case of intrathyroidal
PA successfully treated with US-guided MWA. The eligibility of all
references has been evaluated, and the report is structured
following the CaReL guidelines (9,10).
Case report
Patient information
A 29-year-old woman presented to Smart Health Tower
(Sulaymaniyah, Iraq), in September, 2024 with recurrent HPT and
bilateral loin pain. An analysis of her medical history revealed a
prior diagnosis of HPT, while her surgical history included a right
upper and lower parathyroidectomy, tonsillectomy, cesarean section
and two anterior vaginal wall repairs.
Clinical findings
The vital signs of the patient were stable, and a
neck examination did not reveal any notable findings. Physical
examinations of the chest, abdomen, skin and extremities did not
reveal any abnormalities.
Diagnostic approach
The parathyroid hormone (PTH) level of the patient
was elevated at 183 pg/ml (reference range, 15-65 pg/ml), with a
serum calcium concentration of 11.06 mg/dl (reference range,
8.5-10.5 mg/dl) and the thyroglobulin level measured at 2.62 ng/ml
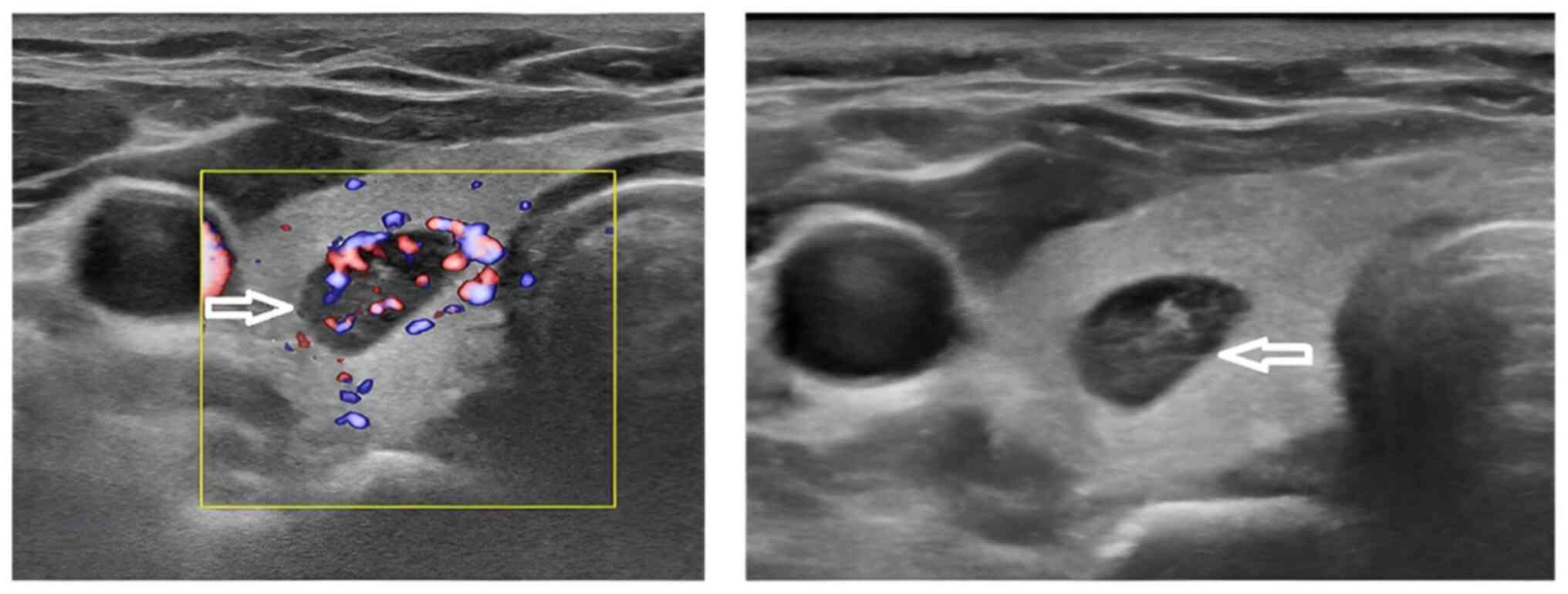
(reference range, 3.5-77 ng/ml). A neck US revealed that both
thyroid lobes were of normal size with a homogeneous echotexture,
along with a single well-defined solid hypoechoic nodule in the
right mid-third of the thyroid, measuring 10x7.7x4.8 mm. The
nodule, which was hypervascular on color Doppler, was suspected to
be an intrathyroidal parathyroid nodule (TR4) (Fig. 1). This nodule had previously been
diagnosed as a benign follicular nodule with thyroiditis on fine
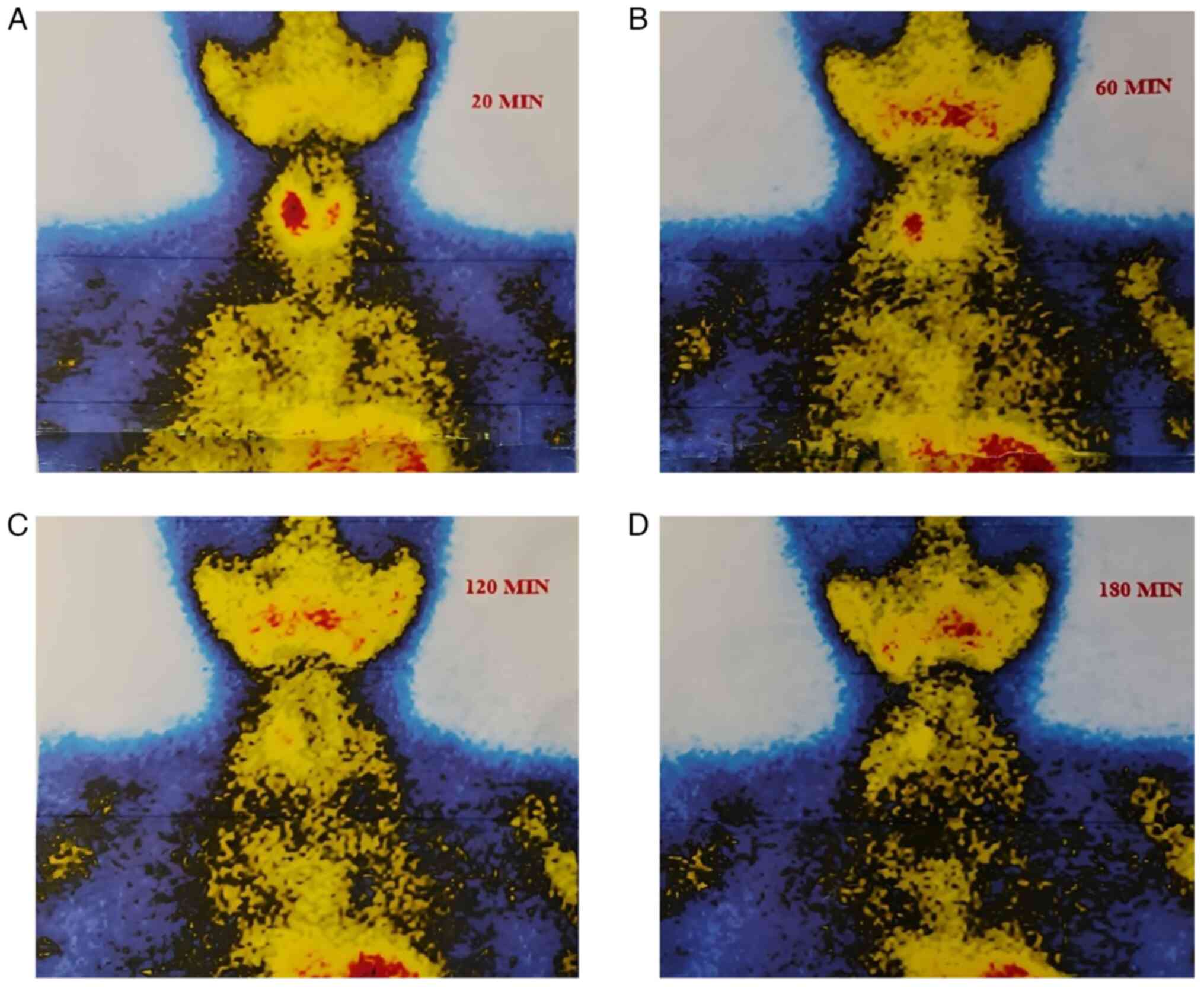
needle aspiration (FNA). A sestamibi scan demonstrated increased
radiotracer accumulation in the right thyroid lobe on the initial
image, with washout observed from the thyroid gland, apart from the
right lobe, on the delayed image (Fig.
2).
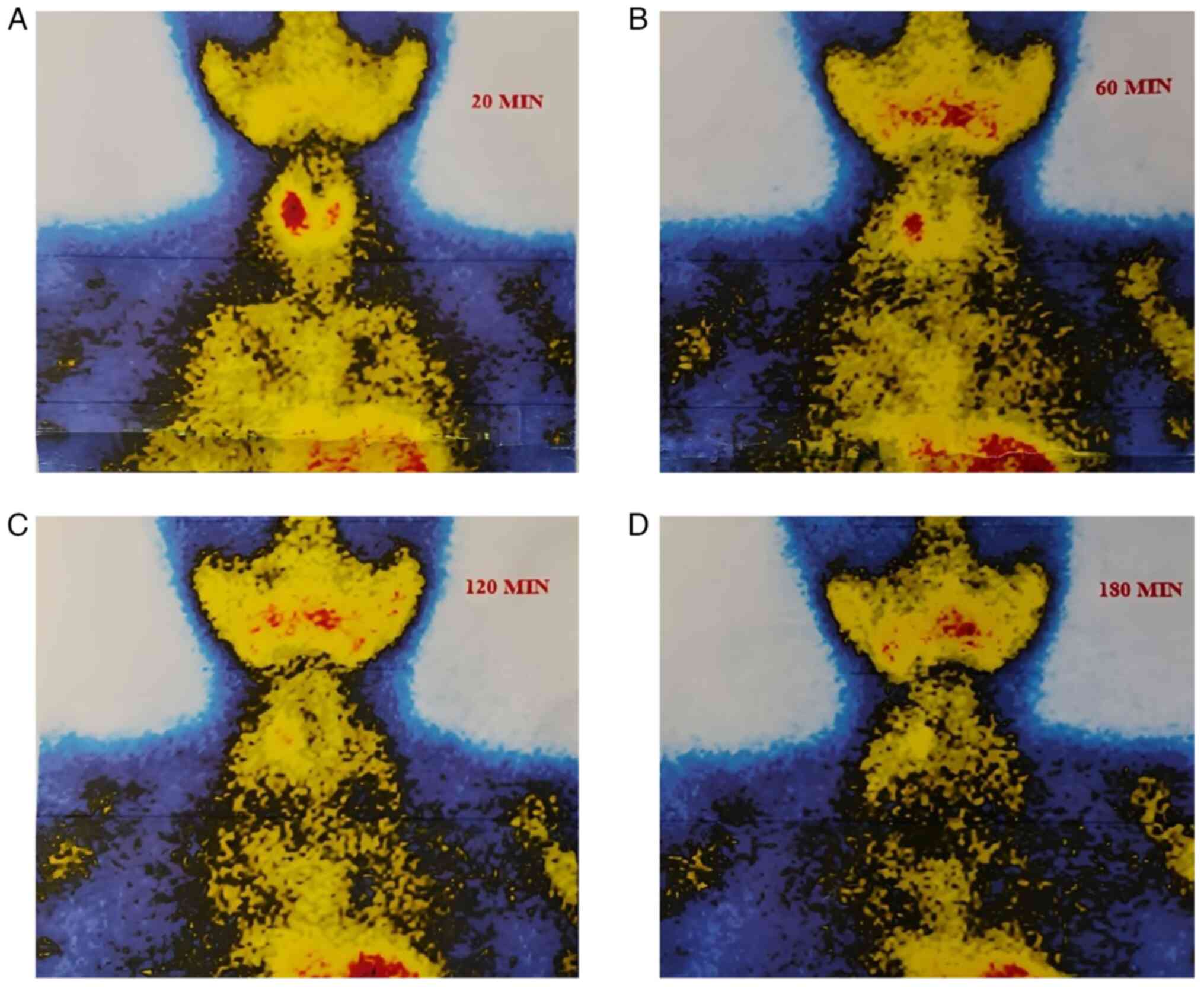 | Figure 2Sequential 99mTc-sestamibi
scintigraphy images obtained at different time intervals
demonstrating radiotracer uptake and washout patterns in the
thyroid region. (A) At 20 min (early phase), there is intense
radiotracer uptake in both thyroid lobes, with a focally increased
accumulation in the right thyroid lobe, suggesting a
hyperfunctioning lesion. (B) At 60 min, partial washout of tracer
activity is observed from most of the thyroid tissue, while the
right thyroid lobe shows persistent uptake. (C) At 120 min, further
washout from normal thyroid tissue occurs, with sustained focal
uptake in the right lobe. (D) At 180 min, complete washout from the
thyroid gland is seen, except for persistent radiotracer retention
in the mid-portion of the right lobe, confirming the presence of an
intrathyroidal parathyroid adenoma. |
Therapeutic interventions
Due to the previous parathyroidectomy, repeat
surgery was considered technically challenging and associated with
a higher risk of complications, including recurrent laryngeal nerve
injury, post-operative hypocalcemia, scarring-related difficulties
and potential cosmetic concerns. The patient, therefore, preferred
a minimally invasive approach under local anesthesia to avoid
another neck surgery.
Using US guidance and local anesthesia, a Microwave
Therapeutic System ECO-200G (ECO Medical Instruments Co., Ltd.)
equipped with an 18-gauge internally cooled needle antenna was
employed to ablate the solid hypoechoic intrathyroidal nodule on
the right side. The antenna was advanced through a trans-isthmic
puncture path to ensure stability and maintain a safe distance from
critical structures, including the recurrent laryngeal nerve and
trachea.
The microwave energy output was set at 25 W, with a
total ablation time of 10 sec. The ablation endpoint was determined
by real-time US visualization of a hyperechoic zone (‘cloud sign’)
surrounding the antenna tip, indicating adequate coagulation of the
target tissue. Continuous US monitoring was maintained throughout
the procedure to confirm complete ablation and to prevent excessive
thermal spread.
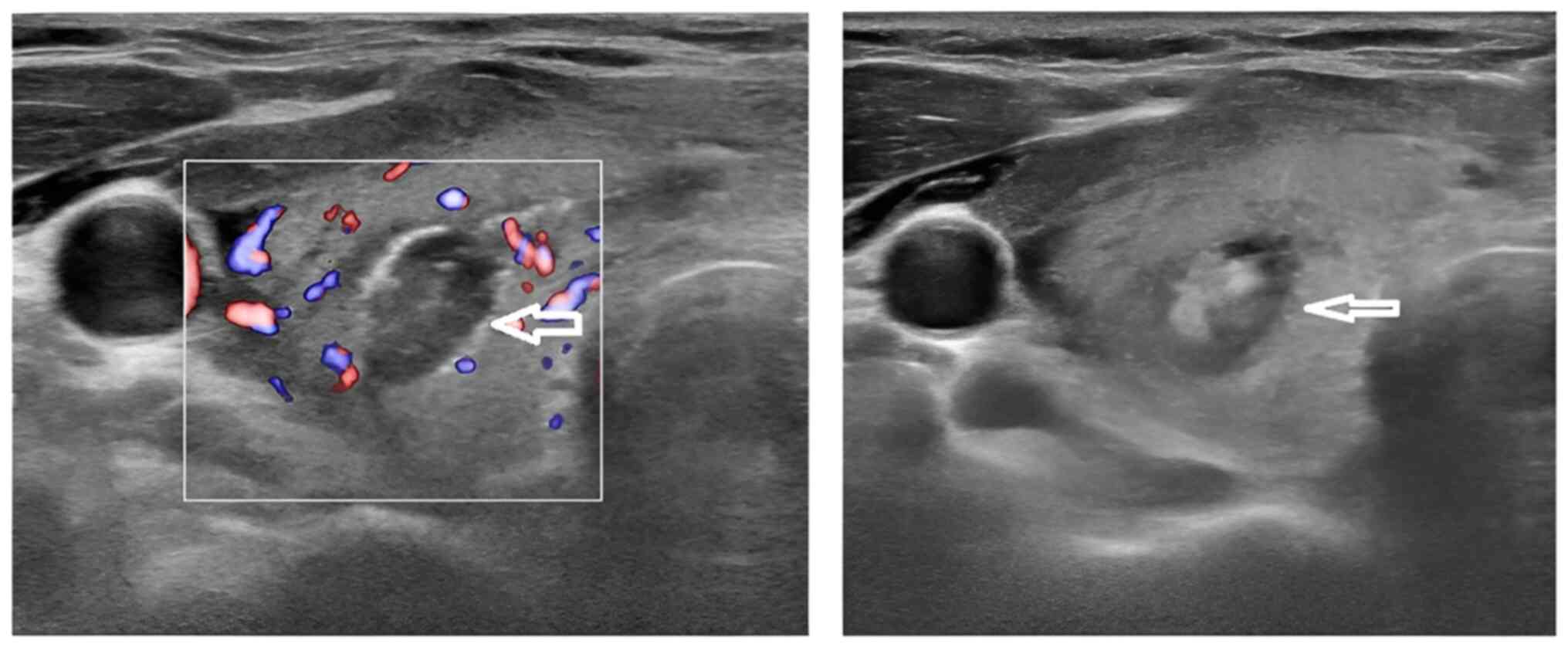
Immediate post-ablation US demonstrated
inhomogeneous echotexture and reduced vascularity, confirming
successful ablation (Fig. 3). As a
result, the serum PTH level of the patient decreased to normal
levels (4 pg/ml) within a few hours, and the serum calcium level
normalized (9.88 mg/dl) during follow-up.
Follow-up and outcome
Following MWA, the patient recovered uneventfully
with no reported complications. At 3 weeks following the procedure,
both the serum calcium (9.35 mg/dl) and PTH levels (30.5 pg/ml)
remained within normal ranges. The patient is currently under
active follow-up. Serial measurements of serum PTH and calcium
levels were scheduled at 3-, 6- and 12-month post-ablation to
monitor for biochemical recurrence.
Discussion
Primary HPT predominantly affects women and older
adults, with a prevalence of ~1% in individuals aged ≥69 years
(11). The case presented herein was
a 29-year-old female patient with a history of HPT and prior right
upper and lower parathyroidectomy.
The complications associated with HPT include the
formation of renal stones, reduced bone density leading to
osteoporosis and persistent bone pain. Additionally, this condition
may contribute to the development of hypertension, increasing the
risk of cardiovascular issues. These complications arise due to
prolonged elevated calcium levels and excessive secretion of PTH,
which can significantly affect both the renal and skeletal systems,
as well as overall cardiovascular health (12).
Biochemical testing is a cornerstone in the
diagnosis of primary HPT and assessing the functionality of PAs.
Serum calcium is the most direct indicator of parathyroid
dysfunction, with elevated levels suggesting HPT. In cases of
suspected PAs, high serum calcium levels serve as a prompt for
further diagnostic investigation. Elevated calcium levels,
particularly when persistent, indicate an imbalance due to
autonomous PTH secretion. The excess calcium in the blood can lead
to severe symptoms and complications affecting the renal, skeletal
and cardiovascular systems (4). The
patient in the present case report exhibited elevated PTH and serum
calcium levels without any complications affecting the renal,
skeletal or cardiovascular systems.
Several imaging techniques are essential for
improving pre-operative localization, including US, sestamibi
scanning and contrast-enhanced computed tomography scan. However,
due to overlapping imaging characteristics with thyroid lesions,
intrathyroidal PAs may still evade accurate detection, posing a
diagnostic challenge (11). In the
US, intrathyroidal PAs can resemble other abnormalities, such as
benign thyroid nodules, which are often found concurrently with
intrathyroidal PAs. Indicators suggestive of an intrathyroidal PA
include a solid lesion lacking cystic components, hypoechogenicity,
and the identification of a single polar feeding artery on Doppler
imaging (13). In the present case
report, a neck US revealed a homogeneous echotexture and a single,
well-defined solid hypoechoic nodule in the right mid-third of the
thyroid, measuring 10x7.7x4.8 mm. The nodule appeared hypervascular
on color Doppler. However, the sestamibi scan revealed increased
radiotracer uptake in the right thyroid lobe on the initial scan,
with a washout from the thyroid gland observed on the delayed
image, apart from the right lobe.
FNA of the lesion can provide insight into the cell
type, potentially supporting the diagnosis. However, distinguishing
between parathyroid and thyroid tissue is challenging due to marked
overlap in cytological and architectural features. Characteristics
once considered indicative of thyroid tissue, such as colloid,
follicles and perivacuolar granulation, are frequently observed in
parathyroid samples. Additionally, a number of PAs exhibit
similarities to follicular, papillary and medullary thyroid
carcinomas (13). In the present
case report, FNA had previously diagnosed the nodule as a benign
follicular nodule with thyroiditis.
The standard treatment for primary HPT is the
surgical removal of one or more PAs. It is estimated that skilled
surgeons successfully identify the affected gland in 95% of cases.
However, the morbidity and mortality rates associated with
parathyroid surgery are higher in elderly patients (14). In recent years, local anesthesia and
minimally invasive nonsurgical therapies have been increasingly
utilized to treat primary HPT. However, the effectiveness of these
minimally invasive non-surgical approaches remains a subject of
debate (14). The patient in the
present case report had a recurrent intrathyroidal PA following a
previous parathyroidectomy, rendering repeat surgery technically
challenging and associated with an increased risk of complications,
such as recurrent laryngeal nerve injury, hypocalcemia and
scarring-related difficulties.
US-guided laser ablation can temporarily lower serum
PTH and calcium levels; however, it does not provide a permanent
resolution of HPT. Consequently, laser ablation cannot be
considered a definitive treatment for primary HPT (14). Other non-surgical treatments,
including RFA and high-intensity focused US, have been previously
introduced. However, clinical experience with these methods remains
limited, as only a small number of patients have undergone these
treatments (14).
MWA has emerged as a promising, minimally invasive
alternative for cases where traditional surgery has not succeeded.
Unlike RFA, which has been explored more extensively in endocrine
pathology, MWA enables greater tissue penetration and more rapid
heating times, reducing the duration of treatment and the risk of
damage to adjacent structures (6,15). The
therapeutic effect of MWA on PAs is principally mechanical and
thermal. MWA produces dielectric heating via the oscillation of
water molecules, which raises intralesional temperatures rapidly
and leads to coagulative necrosis and protein denaturation in the
central treatment zone. This direct thermal injury destroys
parathyroid chief cells and thereby abolishes autonomous PTH
secretion (16).
In comparing MWA with traditional surgery and other
ablation modalities for intrathyroidal PA, several recent studies
have provided helpful insight. A large retrospective cohort study
on 212 patients with primary HPT compared MWA with
parathyroidectomy, with a median follow-up of 28.5 months (17). Following propensity-score matching,
there was no statistically significant difference in clinical cure
rates between the two groups; persistent or recurrent disease rates
were also comparable (17). This
suggests that MWA may provide long-term efficacy similar to
surgery, at least in well-selected patients.
In another prospective multicenter study including
132 patients with primary HPT, the efficacy and safety of MWA and
RFA were compared over follow-up periods ranging from 6 to 36
months (median, ~12 months). The overall cure rate was ~80%, with
no significant differences observed between the MWA and RFA groups
in terms of cure or complication rates. Notably, the pre-ablation
PTH level was identified as the primary prognostic factor (18).
In their study, Liu et al (7) treated 15 patients with benign
parathyroid nodules, concluding that MWA is a safe and effective
technique for managing primary HPT associated with parathyroid
nodules. The procedure was shown to reduce adenoma size, lower
serum PTH and calcium levels, and alleviate symptoms related to the
nodules (7). However, in another
study, Yu et al reported that MWA may be a safe and
effective option for managing recurrent and persistent nodules
associated with secondary HPT (14).
In the present case report, MWA was used to treat intrathyroidal
PA, leading to a reduction and normalization of both PTH and serum
calcium levels. Furthermore, a review of the literature revealed no
reported cases of intrathyroidal PAs treated with MWA. However, 6
reported cases of intrathyroidal PAs were included in the
literature review (Table I)
(2,4-6,19).
 | Table ISummary of 6 cases of intrathyroidal
parathyroid adenoma reported in the literature. |
Table I
Summary of 6 cases of intrathyroidal
parathyroid adenoma reported in the literature.
| First author/year of
publication | Country | Age, years | Sex | Clinical
presentation | S. Ca (reference
range) | PTH (reference
range) | Neck U/S | Management | Outcome | (Refs.) |
|---|
| Papanikos, 2024 | Greece | 67 | Male | Palpable right neck
mass | 14.4 mg/dl (8.5-10.5
mg/dl) | 451 pg/ml (15-65
pg/ml) | Multilobulated cystic
mass 6.9x3.0x2.6 cm, lower right thyroid lobe | Partial
parathy-roidectomy + total thyroidectomy | Normal Ca and PTH
after surgery | (2) |
| Papanikolaou,
2020 | Greece | 43 | Female | Right thyroid-lobe
mass | 12.97 mg/dl (8.5-10.5
mg/dl) | 457.2 pg/ml (15-65
pg/ml) | Predominantly cystic
nodule 3.7x2.5x4 cm with increased peripheral vascularity | Thyroidectomy +
central neck dissection | Normal Ca and PTH
after surgery | (4) |
| Kim, 2024 | Korea | 60 | Male | A thyroid nodule | 10.4 mg/dl (8.5-10.5
mg/dl) | 1,172 pg/ml (15-65
pg/ml) | Right mid-lower-pole
2.6 cm + left upper-pole 1.4 cm nodules | Right hemithy
roidectomy + multi-gland resection | Normal Ca and PTH
after surgery | (5) |
| Eldeiry, 2024 | USA | 64 | Female | Long-standing primary
HPT | N/A | 85 pg/ml (15-65
pg/ml) | 6-mm vascular nodule,
left thyroid lobe | RFA | Normal Ca and PTH
after RFA | (6) |
| Shi, 2016 | China | 59 | Female | Incidental right
thyroid nodule | Not detected | Not detected | Hypoechoic nodule
1.4x0.9 cm, right lobe | Surgical
excision | N/A | (19) |
| Shi, 2016 | China | 45 | Female | Twitching, palpable
left neck mass | 10.68 mg/dl (8.5-10.5
mg/dl) | 182.8 pg/ml (15-65
pg/ml) | Hypervascular mass
1.8x1.1 cm, left lobe | Surgical
excision | Normal Ca and PTH
after surgery | (19) |
MWA for PAs and HPT generally demonstrates a
favorable safety profile; however, evidence indicates that certain
risks require careful management. In a previous systematic review
of US-guided MWA for secondary HPT involving 26 studies and 932
patients, hypocalcemia occurred in 35.2% of cases and transient
hoarseness in ~9.2% of cases, with no major complications or
mortality reported (20). Similarly,
a previous retrospective study including 264 patients with primary
and secondary HPT reported an overall complication rate of 12.1%,
with major complications comprising aphonia or hoarseness in some
patients and severe hypocalcemia in 18.2%; one instance of
permanent recurrent laryngeal nerve injury was documented (21). In the present case report, no
complications such as hoarseness or clinically significant
hypocalcemia were observed.
The present case report has several limitations.
First, the short follow-up duration restricted the assessment of
long-term biochemical and structural outcomes following MWA.
Second, as a single-patient observation, the present case report
lacks statistical validity and cannot yield generalizable
conclusions regarding the efficacy or safety of MWA in treating
intrathyroidal PA. Furthermore, imaging interpretation was based
primarily on US and sestamibi scan findings, which, while standard,
may have inherent limitations in sensitivity and specificity for
intrathyroidal lesions. Additionally, the lack of standardized
anterior-posterior and oblique views in the presented sestamibi
scan, as well as the absence of a uniform color scale to indicate
the intensity of radioactive distribution, may limit the visual
standardization and comparability of the imaging data.
In conclusion, MWA may be a safe and effective
alternative for the treatment of intrathyroidal PAs, particularly
when traditional surgery is not a viable option.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
AJQ and AMS were major contributors to the
conception of the study, as well as to the literature search for
related studies. HAN, AAQ and FHK contributed to the literature
review, in the writing of the manuscript, and in the analysis and
interpretation of the patient's data. SFA, RMA, ANQ and IJH were
involved in the literature review, in the design of the study, in
the critical revision of the manuscript, and in the processing of
the table. AJQ was the radiologist who performed the assessment of
the case. AMA was the pathologist who performed the diagnosis of
the case. FHK and AJQ confirm the authenticity of all the raw data.
All authors have read and approved the final manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from the
patient for her participation in the present study.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the present case report and any
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Pallan S, Rahman MO and Khan AA: Diagnosis
and management of primary hyperparathyroidism. BMJ.
344(e1013)2012.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Papanikos V, Papadodima E, Bantouna D,
Paparodis RD, Livadas S, Angelopoulos I and Karvounis E:
Hypercalcemic crisis due to a giant intrathyroidal parathyroid
adenoma, with postsurgical severe hypocalcemia and hungry bone
syndrome: A case report. Clin Pract. 14:179–187. 2024.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Noussios G, Anagnostis P and Natsis K:
Ectopic parathyroid glands and their anatomical, clinical and
surgical implications. Exp Clin Endocrinol Diabetes. 120:604–610.
2012.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Papanikolaou A, Katsamakas M, Boudina M,
Pamporaki C, Intzidis I, Kiziridou A, Kleidaradaki E, Rakitzi P,
Venetsanaki V and Chrisoulidou A: Intrathyroidal parathyroid
adenoma mimicking thyroid cancer. Endocr J. 67:639–643.
2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Kim JK, Kim GJ, Cha J, Kang SW, Jeong JJ,
Nam KH and Chung WY: Intrathyroidal parathyroid hyperplasia
misdiagnosed as hurthle cell neoplasm. J Endocr Surg. 24:19–24.
2024.
|
|
6
|
Eldeiry LS, Faintuch S and Sacks BA:
Successful radiofrequency ablation of an intrathyroidal parathyroid
adenoma after failed parathyroidectomy. AACE Clin Case Rep.
10:253–256. 2024.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Liu C, Wu B, Huang P, Ding Q, Xiao L,
Zhang M and Zhou J: US-guided percutaneous microwave ablation for
primary hyperparathyroidism with parathyroid nodules: Feasibility
and safety study. J Vasc Interv Radiol. 27:867–875. 2016.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Liu F, Yu X, Liu Z, Qiao Z, Dou J, Cheng
Z, Han Z, Yu J and Liang P: Comparison of ultrasound-guided
percutaneous microwave ablation and parathyroidectomy for primary
hyperparathyroidism. Int J Hyperthermia. 36:834–839.
2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Abdullah HO, Abdalla BA, Kakamad FH, Ahmed
JO, Baba HO, Hassan MN, Bapir R, Rahim HM, Omar DA, Kakamad SH, et
al: Predatory publishing lists: A review on the ongoing battle
against fraudulent actions. Barw Med J. 2:26–30. 2024.
|
|
10
|
Prasad S, Nassar M, Azzam AY,
García-Muro-San José F, Jamee M, Sliman RKI, Evola G, Mustafa AM,
Abdullah HO, Abdalla MA, et al: CaReL guidelines: A consensus-based
guideline on case reports and literature review (CaReL). Barw Med
J. 2:13–19. 2024.
|
|
11
|
Siilin H, Lundgren E, Mallmin H, Mellström
D, Ohlsson C, Karlsson M, Orwoll E and Ljunggren O: Prevalence of
primary hyperparathyroidism and impact on bone mineral density in
elderly men: MrOs Sweden. World J Surg. 35:1266–1272.
2011.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Sattarinezhad A, Rasekhi A and Soveid M:
Management of a parathyroid adenoma with radiofrequency ablation: A
case report. Iran Red Crescent Med J. 19:1–4. 2017.
|
|
13
|
Gowrishankar SV, Bidaye R, Das T, Majcher
V, Fish B, Casey R and Masterson L: Intrathyroidal parathyroid
adenomas: Scoping review on clinical presentation, preoperative
localization, and surgical treatment. Head Neck. 45:706–720.
2023.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Yu MA, Yao L, Zhang L, Peng L, Zhuo L,
Zhang Y, Li W and Lv MD: Safety and efficiency of microwave
ablation for recurrent and persistent secondary hyperparathyroidism
after parathyroidectomy: A retrospective pilot study. Int J
Hyperthermia. 32:180–186. 2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Abdalla BA, Abdullah HO, Nasralla HA, Ali
RM, Omar SS, Ghafour AK, Asaad SK, Raoof SS, Tahir SH, Rashid RJ,
et al: The efficacy and safety of microwave ablation in managing
osteoid osteoma: A systematic review. Case Reports Plast Surg Hand
Surg. 12(2503195)2025.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Hernández JI, Cepeda MF, Valdés F and
Guerrero GD: Microwave ablation: State-of-the-art review. Onco
Targets Ther. 8:1627–1632. 2015.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Wei Y, Zhao ZL, Cao XJ, Peng LL, Li Y, Wu
J and Yu MA: Microwave ablation versus parathyroidectomy for the
treatment of primary hyperparathyroidism: A cohort study. Eur
Radiol. 32:5821–5830. 2022.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Liu F, Liu Y, Peng C, Yu M, Wu S, Qian L,
Han Z, Yu J, Chai H and Liang P: Ultrasound-guided microwave and
radiofrequency ablation for primary hyperparathyroidism: A
prospective, multicenter study. Eur Radiol. 32:7743–7754.
2022.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Shi C, Guan H, Qi W, Ji J, Wu J, Yan F and
Wang H: Intrathyroidal parathyroid adenoma: Diagnostic pitfalls on
fine-needle aspiration: Two case reports and literature review.
Diagn Cytopathol. 44:921–925. 2016.PubMed/NCBI View
Article : Google Scholar
|
|
20
|
Zhou X, Shen Y, Zhu Y, Lv Q, Pu W, Gao L,
Gu M and Li C: Ultrasound-guided microwave ablation for secondary
hyperparathyroidism: A systematic review and meta-analysis. Int J
Hyperthermia. 38:1285–1294. 2021.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Wei Y, Peng LL, Zhao ZL, Li Y and Yu MA:
Complications encountered in the treatment of primary and secondary
hyperparathyroidism with microwave ablation-a retrospective study.
Int J Hyperthermia. 36:1263–1270. 2019.PubMed/NCBI View Article : Google Scholar
|