1. Introduction
Blood gas analysis has evolved significantly beyond
traditional arterial sampling paradigms, with emerging technologies
and evidence-based practices reshaping clinical decision-making in
critical care and emergency medicine. While fundamental
physiological principles remain constant, recent advances in
artificial intelligence (AI), non-invasive monitoring and
systematic evidence synthesis have challenged conventional
approaches and established new standards for clinical practice
(1-5).
The present review aimed to critically evaluate
emerging technologies and methodologies in blood gas analysis,
synthesizing evidence from recent systematic reviews, meta-analyses
and consensus guidelines to provide evidence-based recommendations
for contemporary clinical practice. Unlike traditional reviews that
focus on basic physiological principles, the present review
addresses current controversies, technological innovations and
quality improvement strategies that directly impact patient care
outcomes.
Recent systematic reviews have questioned the
absolute necessity of arterial sampling in all clinical scenarios,
with level 1 evidence supporting venous blood gas analysis in
specific clinical contexts. Simultaneously, artificial intelligence
applications have achieved diagnostic accuracy comparable to expert
clinicians, with some algorithms demonstrating superior performance
in detecting subtle acid-base abnormalities (3,6).
The integration of closed-loop monitoring systems,
automated interpretation algorithms and predictive analytics
represents a fundamental shift toward precision medicine in
critical care, providing the potential for improved patient
outcomes, while reducing healthcare costs and the workload of
clinicians (3,6).
Through this comprehensive evidence-based approach,
the present review aimed to provide clinicians with practical,
contemporary guidance for implementing modern blood gas analysis
strategies that optimize patient care, while addressing real-world
clinical challenges and resource constraints.
2. Physiological basis of blood gas
analysis
Blood gas analysis provides key insight into the
homeostatic regulation of the body through the evaluation of pH,
partial pressure of oxygen (PaO2), partial pressure of
carbon dioxide (PaCO2) and bicarbonate
(HCO3-) levels. These parameters reflect the
delicate balance maintained between the respiratory and renal
systems, which function synergistically to ensure stable internal
conditions.
The pH, regulated tightly between 7.35 and 7.45,
depends on the ratio between HCO3- and
CO2, not their absolute concentrations. This association
is represented by the Henderson-Hasselbalch equation.
CO2, a volatile acid, is regulated by the respiratory
system and is in equilibrium with carbonic acid, which dissociates
into HCO3- and hydrogen ions. This
equilibrium is accelerated by carbonic anhydrase within red blood
cells, supporting rapid buffering (7).
PaO2 reflects the oxygenation capacity of
blood, with normal arterial values ranging from 75 to 100 mmHg.
Moreover, PaCO2 levels, typically between 35 and 45
mmHg, provide insight into ventilatory function. Base excess helps
determine the metabolic component of acid-base disorders,
indicating whether there is a surplus or deficit of bases in the
blood (8).
Buffer systems are essential for pH regulation. The
main one is the HCO3-/carbonic acid buffer,
an open system enhanced by CO2 excretion and
HCO3- reabsorption. The phosphate buffer,
although less active in plasma, plays a key intracellular role.
Proteins, particularly hemoglobin, also contribute significantly to
buffering due to their amphoteric nature and concentration in blood
(8).
Respiratory regulation modulates CO2
elimination via changes in ventilation rate, while the renal system
contributes by excreting hydrogen ions and reabsorbing
HCO3-. Type A and B intercalated cells in the
collecting duct adapt secretion or reabsorption processes depending
on the pH status of the body (8,9).
Together, this complex physiological interplay
ensures acid-base homeostasis, enabling the body to respond
effectively to internal and external stressors, and forms the
foundational basis for interpreting arterial blood gas (ABG)
results in clinical practice.
3. Clinical applications of blood gas
analysis
ABG analysis remains the gold standard for assessing
oxygenation, ventilation and acid-base status in clinical practice.
Although less invasive techniques are increasingly available, ABG
continues to play a central role, particularly in critical settings
(10).
In critically ill patients, such as those in
intensive care units (ICUs) or emergency departments, ABG helps
detect and monitor conditions such as sepsis, acute respiratory
distress syndrome (ARDS) and shock. It allows early identification
of hypoxia, hypercapnia, and lactic acidosis, guiding oxygen
therapy, ventilatory support, and prognosis (10).
In respiratory diseases, such as chronic obstructive
pulmonary disease (COPD) and asthma, ABG provides essential
information to assess disease severity and guide treatment. In
COPD, it detects chronic hypoxemia and CO2 retention,
indicating the need for home oxygen therapy or non-invasive
ventilation. In acute exacerbations, ABG assists in distinguishing
between hypoxemia and hypercapnic respiratory failure. In asthma,
particularly during severe attacks, ABG allows for the early
recognition of impending respiratory failure, aiding in timely
intervention (11,12).
The diagnosis and management of metabolic disorders,
such as diabetic ketoacidosis, renal failure, or lactic acidosis
also rely on ABG. By analyzing pH, PaCO2,
HCO3-, base excess and anion gap (AG),
clinicians can classify disorders, assess compensations and
identify mixed disturbances (10,13).
ABG is also vital in adjusting mechanical
ventilation. It enables the evaluation of oxygenation efficiency
(PaCO2), ventilatory status (PaCO2) and
acid-base balance (pH and HCO3-), supporting
decisions on fraction of inspired oxygen (FiO2), tidal
volume, respiratory rate and positive end-expiratory pressure
(PEEP). The PaCO2/FiO2 ratio, for instance,
is used to assess the severity of ARDS and tailor ventilation
strategies accordingly (14).
Ultimately, blood gas analysis is not only a
diagnostic tool, but a dynamic method that can be used for
continuous monitoring and therapeutic adjustment in a wide range of
acute and chronic conditions. Its value lies in its immediacy,
precision and ability to reflect the physiological state of a
patient in real-time, rendering it indispensable in modern medical
practice.
4. Pathological alterations and their
interpretation
The accurate interpretation of ABG results is
essential for identifying acid-base disorders. The process begins
by evaluating the pH: Values <7.35 indicate acidemia, while
those >7.45 indicate alkalemia. A normal pH does not exclude a
disorder, as it may be compensated (10).
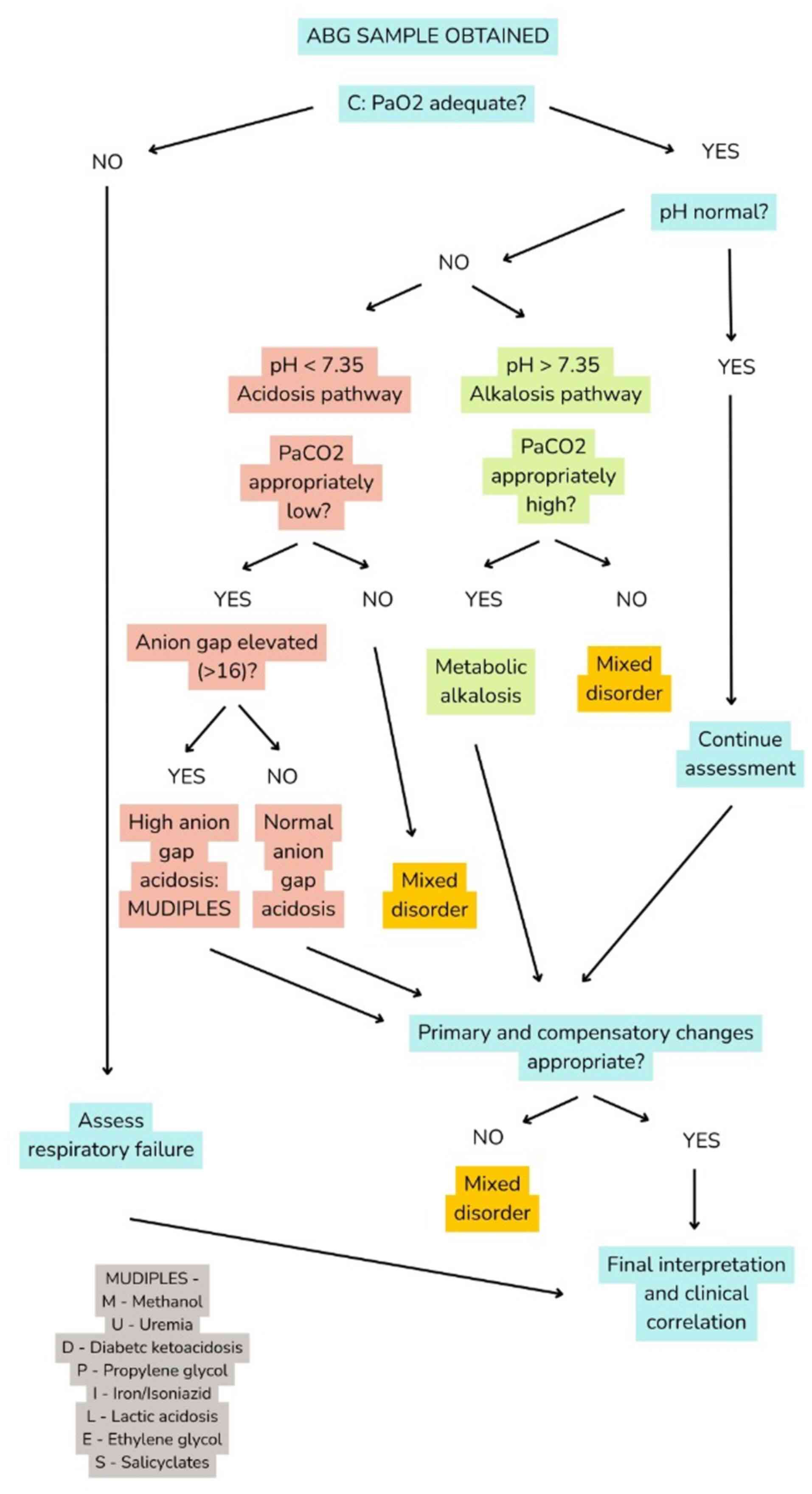
Interpreting ABG results requires a systematic
approach to minimize errors and ensure the comprehensive assessment
of acid-base disorders and respiratory status. A flowchart of
systematic ABG interpretation using the Check oxygenation, look at
pH, evaluate compensation, assess AG, and Review for mixed
disorders (CLEAR) algorithm is presented in Fig. 1. The CLEAR algorithm guides
clinicians through sequential decision points. Color coding
differentiates normal, acidotic, alkalotic, and mixed disorder
pathways, while the integrated MUDPILES mnemonic supports rapid
identification of high AG causes.
The primary disorder is then identified by examining
PaCO2 and HCO3-. In the event that
changes in PaCO2 follow the same direction as pH, the
origin is respiratory; however, in the event that
HCO3- follows the pH, the origin is
metabolic. Compensation mechanisms, respiratory or renal, aim to
restore pH, but are rarely complete. Empirical formulas, such as
Winter's help determine whether compensation is appropriate
(9,10,15).
In metabolic acidosis, the AG [AG=Na+-
(CI- + HCO3-)] helps differentiate
between HCO3- and acid accumulation. A high
AG suggests conditions such as diabetic ketoacidosis, lactic
acidosis, or renal failure, while a normal AG indicates
gastrointestinal or renal HCO3- loss
(15).
The four main disorders are the following: i)
Metabolic acidosis: A low pH and HCO3-, often
with compensatory hyperventilation. Symptoms include fatigue,
hypotension, and in severe cases, coma. Causes vary from
ketoacidosis to renal failure (15).
ii) Metabolic alkalosis: Elevated pH and
HCO3-, usually from vomiting or diuretics.
Hypoventilation is the compensatory response, limited by hypoxia.
Presents with muscle cramps, paresthesia and arrhythmias. iii)
Respiratory acidosis: Low pH with elevated PaCO2, often
due to COPD or respiratory depression. Renal compensation increases
HCO3- over time. Symptoms include dyspnea,
confusion, and, in severe cases, coma. iv) Respiratory alkalosis:
High pH with decreased PaCO2, usually caused by anxiety,
sepsis, or hypoxia. Compensation involves renal
HCO3- excretion. Symptoms include dizziness,
paresthesia and palpitations (11,12).
The accurate classification of primary acid-base
disturbances and their compensatory responses is critical for
tailored therapy. A brief reference guide to five key disorders,
metabolic acidosis/alkalosis, respiratory acidosis/alkalosis and
mixed disturbances, with expected PaCO2 compensation
formulas, typical etiologies, and anion gap considerations is
provided in Table I. This concise
format facilitates rapid bedside interpretation and assists in
distinguishing simple from mixed disorders.
 | Table IAcid-base disorders guide. |
Table I
Acid-base disorders guide.
| Disorder | pH | Primary change | Compensation | Expected
PaCO2 | Common causes | Anion gap |
|---|
| Metabolic
acidosis | <7.35 | ↓
HCO3- (<22 mEq/l) | ↓ PaCO2
(hyperventilation) | 1.5 x
[HCO3-] + 8±2 | DKA, lactic
acidosis, uremia, diarrhea, poisoning | Check: Normal
(8-16) vs. high (>16) |
| Metabolic
alkalosis | >7.45 | ↑
HCO3- (>26 mEq/l) | ↑ PaCO2
(hypoventilation) | 0.7 x
Δ[HCO3-] + 40±5 | Vomiting,
diuretics, hyperaldosteronism | Usually normal
(8-16) |
| Respiratory
acidosis | <7.35 | ↑ PaCO2
(> 45 mmHg) | ↑
HCO3- (renal retention) | ‘Acute: 0.1 x
ΔPCO2 chronic: 0.4 x ΔPCO2’ | COPD, pneumonia,
opioids, CNS depression | Usually normal
(8-16) |
| Respiratory
alkalosis | >7.45 | ↓ PaCO2
(<35 mmHg) | ↓ HCO3-
(renal excretion) | ‘Acute: 0.2 x
ΔPCO2 chronic: 0.5 x ΔPCO2’ | Anxiety, pain,
hypoxia, sepsis, pregnancy | Usually normal
(8-16) |
| Mixed acidosis | <7.35 | ↓
HCO3- + ↑ PaCO2 |
Variable/inadequate | No predictable
formula | Cardiopulmonary
arrest, severe sepsis | Often elevated
(>16) |
| Mixed
alkalosis | >7.45 | ↑
HCO3- + ↓ PaCO2 |
Variable/inadequate | No predictable
formula | Diuretics +
hyperventilation | Variable
(8-20) |
Mixed disorders occur when two imbalances coexist,
complicating the clinical picture. Proper identification requires
the full interpretation of all parameters and compensation patterns
(15).
Understanding these patterns enables an accurate
diagnosis and the effective treatment of patients with complex
acid-base disturbances.
5. Methods and techniques
The accuracy of blood gas analysis depends on proper
sample collection, handling and measurement. There are three main
types of blood samples: Arterial, venous and capillary. Arterial
blood, usually drawn from the radial artery, is preferred due to
its reliability in reflecting oxygenation and acid-base status.
Venous samples are less invasive, but less precise, while capillary
samples are used mainly in neonates and are influenced by
peripheral perfusion (10).
Measurement relies on specific electrodes: pH is
determined by a glass electrode sensitive to H+ ions;
PaO2 is measured using the Clark electrode, based on an
electrochemical reaction with oxygen; and PaCO2 is
assessed using the Severinghaus electrode, which detects pH changes
caused by CO2 diffusion. These methods provide rapid and
precise results but are sensitive to temperature and contamination
(13).
Certain parameters, such as HCO3-, base
excess, or oxygen saturation, are not measured directly, but are
calculated using formulas such as the Henderson-Hasselbalch
equation. The alveolar-arterial gradient is also derived and helps
assess gas exchange efficiency (16).
Modern analyzers often include electrolyte
measurements (Na+, K+, CI- and
Ca2+) and markers such as lactate, which reflect tissue
perfusion. Co-oximetry further allows the detection of abnormal
hemoglobin species, such as carboxyhemoglobin or methemoglobin
(17).
Accurate analysis requires strict pre-analytical and
analytical protocols to avoid errors. When properly conducted,
blood gas analysis provides immediate, vital data that guides
clinical decisions and supports patient monitoring in both acute
and chronic settings (18).
In an aim to guide clinicians in selecting the most
appropriate sampling approach for blood gas analysis, the present
review provides a comparative overview of arterial, venous and
capillary sampling methods. A summary of key performance metrics,
including analytical accuracy, correlation with arterial blood gas
values, procedural risks, patient comfort and diagnostic utility,
alongside sensitivity and specificity data for respiratory failure,
is presented in Table II. This
evidence-based comparison highlights scenarios in which alternative
sampling techniques [e.g., venous with venous-to-arterial
conversion (v-TAC)] can safely replace arterial puncture without
compromising diagnostic integrity.
 | Table IIComparison of arterial, venous, and
capillary blood gas sampling. |
Table II
Comparison of arterial, venous, and
capillary blood gas sampling.
| Parameter | Arterial | Venous | Capillary |
|---|
| Sample site | Radial/femoral
artery | Peripheral/central
vein |
Fingertip/earlobe |
| pH accuracy | Gold standard | Good (r=0.92) | Good (r=0.88) |
| PaCO2
accuracy | Gold standard | Good (r=0.85) | Fair (r=0.75) |
| PaO2
accuracy | Gold standard | Poor (not
reliable) | Fair (r=0.70) |
|
HCO3- accuracy | Gold standard | Excellent
(r=0.95) | Good (r=0.90) |
| Patient
discomfort | High (painful) | Low | Minimal |
| Procedural
risk | Moderate (bleeding,
thrombosis) | Low | Minimal |
| Cost | High | Moderate | Low |
| Time to result | 3-5 min | 2-3 min | 1-2 mi |
| Clinical
applications | All clinical
scenarios | Metabolic
disorders, DKA monitoring | Pediatric, routine
monitoring |
|
Contraindications | Coagulopathy,
severe PVD | Acute respiratory
failure | Poor circulation,
shock |
| Correlation with
ABG | 100% | 85-95% | 70-85% |
| Sensitivity
(RF) | 100% | 97.6% | 89.2% |
| Specificity
(RF) | 100% | 36.9% | 78.4% |
6. Challenges and limitations
Despite its clinical value, blood gas analysis is
subject to several limitations and potential errors that can affect
result accuracy and interpretation. These are classified as
pre-analytical, analytical and post-analytical (18).
Pre-analytical errors are the most frequent and can
compromise up to 70% of results. They include incorrect sample
type, improper anticoagulant use (excess or poorly mixed heparin),
air bubbles in the syringe, or delayed analysis. These factors
alter gas tensions and pH, leading to false readings. To minimize
these errors, samples need to be collected with care, using
pre-heparinized syringes, removing air immediately, and analyzing
promptly or refrigerating if delayed (10).
Analytical errors stem from equipment-related
issues, such as improper calibration, electrode contamination, or
failure to account for temperature. These affect pH,
PaO2 and PaCO2 measurements. Regular
maintenance and quality control are essential to ensure reliable
operation (12).
Post-analytical errors arise during the
interpretation, transcription, or communication of results.
Misreading values, applying incorrect reference ranges
(particularly in pediatrics or chronic conditions), or failing to
correlate data with the clinical context can lead to erroneous
decisions. Interpretation should always be integrated with the
patient's condition and previous measurements (10).
While blood gas analysis provides immediate and
valuable information, its reliability depends on rigorous
technique, proper equipment handling and informed interpretation.
Recognizing its limitations is crucial to avoid misdiagnosis and
ensure it remains a powerful tool in clinical practice.
7. Quality improvement and standardization
initiatives
Recent quality improvement initiatives have
demonstrated significant reductions in diagnostic errors through
standardized protocols. The implementation of evidence-based blood
gas indication algorithms reduces inappropriate testing by 34%,
while maintaining diagnostic sensitivity (3,19,20).
In pre-analytical standardization, automated heparin
dosing systems reduce sample dilution errors by 67%; pneumatic tube
system optimization maintains sample integrity over extended
transport and temperature-controlled storage protocols for delayed
analysis scenarios (https://acutecaretesting.org/en/articles/standards-provide-a-quality-approach-to-blood-gas-analysis;
https://www.siemens-healthineers.com/si/blood-gas/blood-gas-systems/rapid-lab-348-ex).
In analytical quality control, real-time quality
control monitoring with automated recalibration protocols provides
proficiency testing programs achieving 98.2% interlaboratory
agreement and the integration of internal quality control with
external quality assurance programs (21).
An outline of a phased roadmap for technology
integration, describing how point-of-care systems, smart analyzers
and closed-loop automation are reshaping accuracy, efficiency and
clinical decision-making (3,22) is provided below:
i) Phase 1-basic automation (currently available):
Point-of-care analyzers equipped with integrated quality control
mechanisms have streamlined workflow efficiency and minimized
analytical errors. Electronic result verification and transmission
systems ensure rapid communication between laboratory and clinical
teams, while basic decision-support algorithms assist clinicians in
interpreting acid-base disturbances with greater consistency and
accuracy.
ii) Phase 2-AI integration (emerging): Machine
learning models are increasingly applied to recognize complex
acid-base patterns and provide early warnings for clinical
deterioration. Natural language processing enables automated
correlation between blood gas results and electronic health
records, facilitating real-time clinical context generation.
Predictive analytics are being developed to optimize ventilator
weaning protocols and guide therapeutic interventions based on
continuous data analysis (23).
iii) Phase 3-closed-loop systems (in development):
Next-generation closed-loop systems integrate automated sampling,
analysis and therapeutic adjustment within a single framework.
These platforms can communicate with wearable monitoring devices to
provide continuous assessment of oxygenation and ventilation
status. Personalized diagnostic algorithms are also being designed
to adapt interpretation and intervention strategies according to
each patient's physiological profile (22,24).
Cost-effectiveness studies have demonstrated a 28%
reduction in overall diagnostic costs through optimized testing
strategies, a decreased length of stay (average of 1.3 days)
through improved diagnostic accuracy and a reduced procedural
complication saving $3,200 per patient annually (3,22,24).
8. Venous vs. arterial sampling:
Evidence-based practice guidelines
The controversy surrounding venous vs. ABG sampling
has been extensively addressed in recent systematic reviews and
meta-analyses. While arterial sampling remains the gold standard,
emerging evidence supports the selective use of venous blood gas
analysis in specific clinical scenarios (https://www.cochrane.org/evidence/CD010841_how-accurate-blood-test-using-blood-collected-vein-rather-artery-diagnosing-abnormalities-oxygen).
Recent Cochrane systematic reviews have demonstrated
that peripheral venous blood gas analysis achieves a sensitivity of
97.6% and specificity of 36.9% for diagnosing respiratory failure.
The introduction of v-TAC technology has significantly improved
diagnostic accuracy, allowing the calculation of arterial values
from venous samples with correlation coefficients exceeding 0.85
for pH and PaCO2 (25).
Venous blood gas analysis provides adequate
diagnostic information for the following disorders: Metabolic
acid-base disorder assessment when oxygenation is not the primary
concern, in diabetic ketoacidosis monitoring where pH and
bicarbonate trends are most relevant, in chronic kidney disease
patients requiring frequent acid-base monitoring and in pediatric
populations where arterial sampling poses increased procedural
risks (https://www.cochrane.org/evidence/CD010841_how-accurate-blood-test-using-blood-collected-vein-rather-artery-diagnosing-abnormalities-oxygen).
However, venous sampling should be avoided in
patients with acute respiratory failure requiring precise
oxygenation assessment, in mechanical ventilation adjustments based
on PaO2/FiO2 ratios and in suspected carbon
monoxide or methemoglobin poisoning `requiring co-oximetry
(2,4).
The integration of v-TAC algorithms in modern
analyzers has reduced the diagnostic gap between venous and
arterial sampling, rendering venous analysis a viable option in
selected clinical scenarios, while improving patient comfort and
reducing procedural complications.
9. Closed-loop blood gas management in
critical care
Modern critical care increasingly utilizes
closed-loop systems that integrate blood gas analysis with
automated therapeutic interventions, representing a paradigm shift
toward precision medicine (22).
Closed-loop blood gas management systems consist of
real-time monitoring components (continuous blood gas analyzers
with automated sampling systems, AI-powered interpretation
algorithms providing immediate clinical alerts and integration with
electronic health records for trending analysis) and automated
response protocols (FiO2 adjustment based on
PaO2 targets (maintaining peripheral oxygen saturation
at 88-92% in patients with COPD), ventilator parameter
modifications triggered by pH and PaCO2 changes and
automated alerts for metabolic derangements requiring immediate
intervention) (3,22). Clinical implementation examples are
provided below:
Case 1-ARDS management: Automated FiO2
titration based on PaO2/FiO2 ratios, with
real-time PEEP adjustments to maintain optimal oxygenation, while
minimizing ventilator-induced lung injury.
Case 2-Diabetic ketoacidosis protocol: Automated
insulin infusion adjustments based on pH trends and anion gap
calculations, with integrated electrolyte replacement
protocols.
Case 3-post-operative monitoring: Continuous
monitoring with automated alerts for respiratory depression,
enabling immediate intervention in opioid-treated patients.
The implementation of closed-loop systems
demonstrates a 23% reduction in time to therapeutic targets, a 31%
decrease in blood gas sampling frequency, while maintaining
diagnostic accuracy, and an improved ICU staff workflow efficiency
with 18% reduction in manual interventions (3,22,24).
Modern AI algorithms provide pattern recognition for
early clinical deterioration (sensitivity, 94.2%), predictive
modeling for ventilator weaning protocols and automated
interpretation with 97% concordance with expert clinicians
(26,27).
10. Future perspectives
The future of blood gas analysis is closely tied to
technological advances aimed at improving precision, accessibility
and real-time clinical applicability. One of the most promising
developments is the miniaturization of devices, which will allow
for rapid, bedside measurements in pre-hospital and home-care
settings. This will be particularly relevant in chronic patient
monitoring and emergency interventions (5).
At the same time, the integration of AI and
predictive algorithms into analyzers will facilitate
interpretation, reduce human error and enhance clinical
decision-making. These systems will be capable of recognizing
deterioration patterns in real-time, contributing to early
diagnosis and timely interventions (23).
Modern intensive care leverages closed-loop systems
that automatically adjust therapeutic interventions based on blood
gas parameters. In Table III,
eight clinical scenarios are presented, ranging from ARDS
management to diabetic ketoacidosis, detailing specific ABG
triggers, automated responses, monitoring frequencies, safety
thresholds, alert conditions and success metrics. These protocols
demonstrate how integrated blood gas analysis can optimize care
delivery while maintaining stringent safety oversight.
 | Table IIIClosed-loop protocols for abg-guided
therapeutic interventions. |
Table III
Closed-loop protocols for abg-guided
therapeutic interventions.
| Clinical
scenario | ABG trigger | Automated
response | Monitoring
frequency | Safety
parameters | Alert
conditions | Success
metrics |
|---|
| ARDS
management |
PaO2/FiO2
<300 | ↑ PEEP + 2 cm
H2O ↑ FiO2 +10% | q30 min x 2 h, then
q1 h | PEEP ≤ 18 cm
H2O, FiO2 ≤ 80% | No improvement in 2
h |
PaO2/FiO2
>300 |
| COPD
exacerbation | PaO2
>50 mmHg, pH <7.30 | NIV initiation,
bronchodilators | q15 min x 1 h, then
q30 min | Max NIV pressure 25
cm H2O | PaCO2
>80 mmHg | PaCO2
<50, pH >7.35 |
| Diabetic
ketoacidosis | pH <7.30,
HCO3- <15 | Insulin infusion ↑
20% | q1 h until pH
>7.30 | Max insulin 20
units/h | pH <7.10 or
glucose <70 | pH >7.30, anion
gap <12 |
| Post-operative
monitoring | PaCO2
>50 mmHg | Naloxone 0.1mg IV,
↑ RR | q15 min x 2 h | Total naloxone ≤2
mg | Apnea >30
sec | Stable
ventilation |
| Septic shock | pH <7.20,
lactate > 4 | ↑ Norepinephrine,
fluid bolus | q30 min until
stable | MAP ≥65 mmHg | Refractory
hypotension | pH >7.30,
lactate <2 |
| Cardiac surgery
recovery | pH <7.35 or
>7.50 | Ventilator
adjustment | q30 min x 4 h | Tidal volume 6-8
ml/kg | Arrhythmias | Normal acid-base
status |
| Pediatric critical
care | pH <7.30 or
>7.50 | Age-appropriate
protocol | q30 min | Age-specific
limits | Sustained abnormal
values | Age-appropriate
norms |
| Weaning
protocol | pH 7.35-7.45,
PaCO2 35-45 | Pressure support ↓
2 cm H2O | q2 h during
weaning | Spontaneous
breathing | Failed weaning
trial | Successful
extubation |
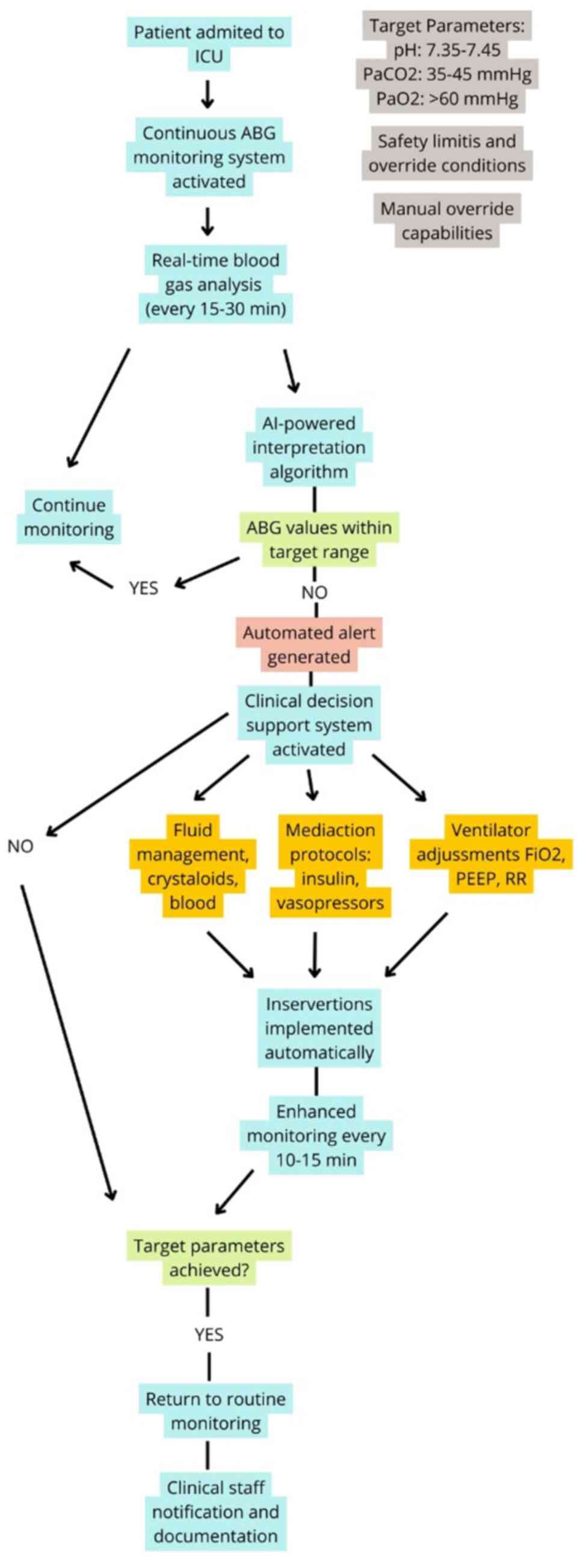
To visualize the integration of continuous blood gas
monitoring with automated therapeutic adjustments, Fig. 2 depicts the closed-loop management
algorithm in critical care. Beginning with real-time ABG sampling
and AI-powered interpretation, the flowchart in Fig. 2 illustrates decision points that
trigger ventilator changes, medication protocols, or fluid
management. Safety limits and manual override capabilities ensure
clinician control within an otherwise automated system.
Efforts are also being made toward non-invasive
blood gas monitoring, which could eliminate the need for repeated
arterial punctures. Sensors capable of estimating PaO2
and PaCO2 continuously would improve patient comfort and
allow uninterrupted monitoring, particularly in intensive care
units (23).
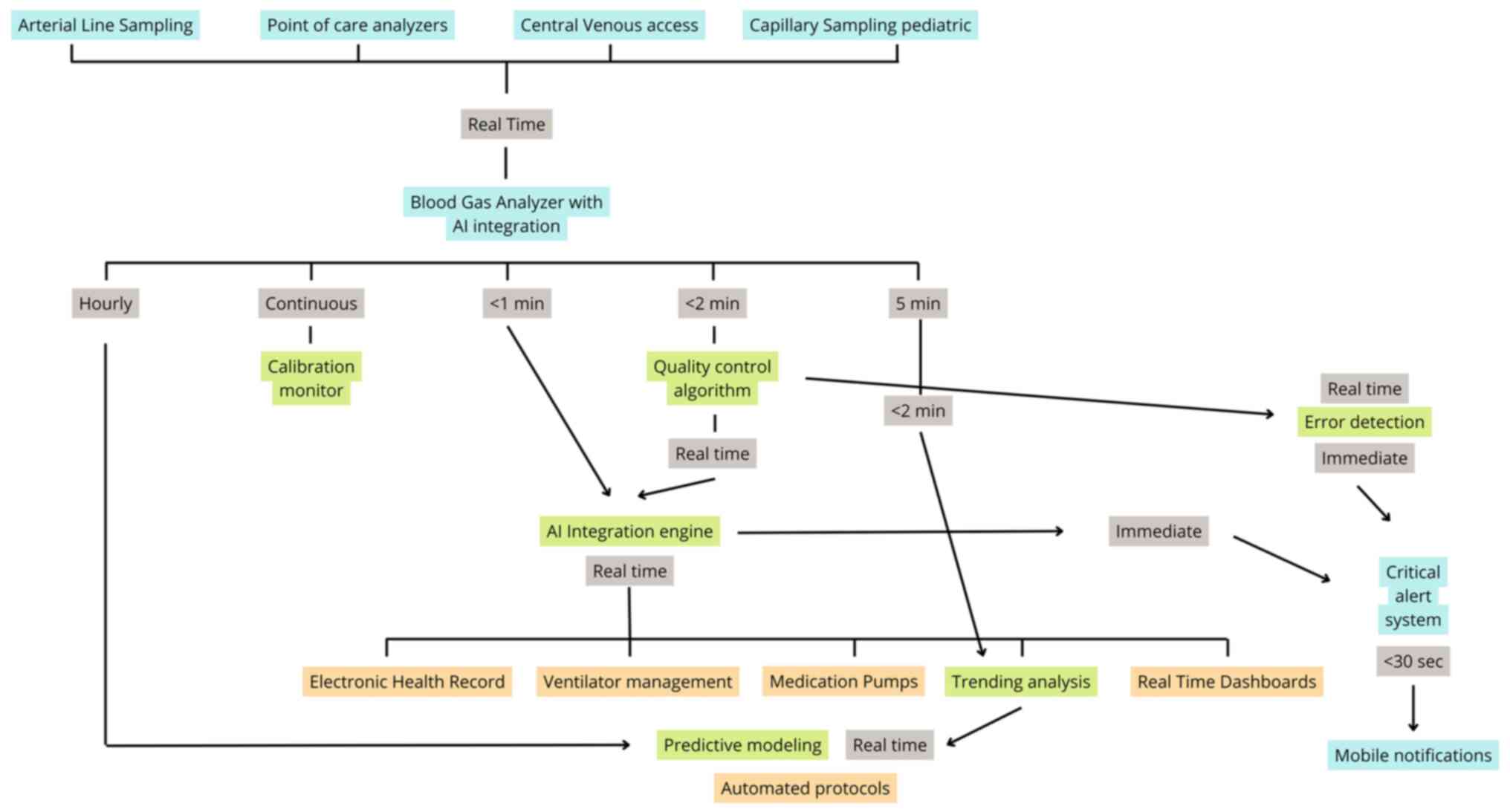
A comprehensive view of modern blood gas monitoring
infrastructure is provided in Fig.
3, which maps the data and process flows among sampling
devices, AI interpretation engines, quality control modules,
clinical decision support systems, and therapeutic platforms. This
diagram underscores how bidirectional integration with electronic
health records, ventilator systems, infusion pumps, and mobile
alerts enables real-time decision-making and enhances diagnostic
accuracy across diverse clinical settings.
Telemedicine will play a central role in the remote
management of chronic patients. Through wireless data transmission,
clinicians will be able to follow-up on gasometry values without
the need for in-person visits, improving healthcare access and
reducing unnecessary hospitalizations (28).
In summary, the future of blood gas analysis lies in
automation, real-time monitoring and personalized medicine,
reinforcing its role as a key diagnostic and management tool in
21st-century healthcare.
11. Conclusions
Blood gas analysis is a very useful diagnostic tool
for evaluating respiratory and metabolic function, particularly in
critical care and emergency settings. It allows for the rapid
assessment of key parameters, such as pH, PaO2,
PaCO2 and HCO3-, and base excess,
enabling timely therapeutic decisions.
The present review has summarized its physiological
foundations, clinical applications and interpretation methodology,
highlighting its relevance in diagnosing acid-base disorders and
guiding ventilation strategies. Additionally, it has emphasized the
importance of correct sampling techniques and the need to minimize
errors throughout the analytical process.
Despite its precision, the technique is not exempt
from limitations, and its effectiveness depends on proper use and
interpretation. Technological advances, such as miniaturized
devices, AI integration and non-invasive monitoring, point toward a
future of greater accessibility, automation, and personalized
care.
Ultimately, blood gas analysis remains a cornerstone
in clinical practice, and its continued development will further
enhance patient monitoring and treatment in modern medicine.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
Not applicable.
Author's contributions
JO was involved in the conceptualization and design
of the review. MNS was involved in the literature review, and in
the drafting of the manuscript. JO was involved in the final
supervision of the manuscript. Both authors have read and approved
the final manuscript. Data authentication is not applicable.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Use of artificial intelligence tools
During the preparation of this work, AI tools were
used to improve the readability and language of the manuscript or
to generate images, and subsequently, the authors revised and
edited the content produced by the AI tools as necessary, taking
full responsibility for the ultimate content of the present
manuscript'.
References
|
1
|
Shastri L, Thomsen LP, Toftegaard M,
Tygesen GB, Weinreich UM, Rychwicka-Kielek BA, Davies MG, Ekström
M, Rittger H, Kelly AM, et al: The use of venous blood gas in
assessing arterial Acid-base and oxygenation status-an analysis of
aggregated data from multiple studies evaluating the venous to
arterial conversion (v-TAC) method. Expert Rev Respir Med.
18:553–559. 2024.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Byrne AL, Pace NL, Thomas PS, Symons RL,
Chatterji R and Bennett M: Peripheral venous blood gas analysis for
the diagnosis of respiratory failure, hypercarbia and metabolic
disturbance in adults. Cochrane Database Syst Rev.
6(CD010841)2025.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Musa Hussain EY, Sidahmed Abdullah AM,
Mahgoub Idris RM, Hashim Gabir ZT, Mohammed Diab RA, Mustafa Ahmed
RN, Ahmed Elbalal KA, Ibrahim Elhaj OY, Mohammed Abdelmagid MH,
Mahmoud Ahmed RA, et al: Evaluation and improving the quality of
arterial blood gas interpretation among junior doctors in Aswan
university hospital: A clinical audit. Cureus.
16(e74906)2024.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Habib T, Nair A, Murphy S, Saeed H and
Ishaya N: Mastering blood gas interpretation: A practical guide for
primary care providers. S Afr Fam Pract (2004). 67:e1–e7.
2025.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Zaboli A, Biasi C, Magnarelli G, Miori B,
Massar M, Pfeifer N, Brigo F and Turcato G: Arterial blood gas
analysis and clinical decision-making in emergency and Intensive
Care Unit nurses: A performance evaluation. Healthcare (Basel).
13(261)2025.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Giani D, Santoro MC, Gabrielli M, Di Luca
R, Malaspina M, Lumare M, Scatà LA, Pala M, Manno A, Candelli M, et
al: The role of venous blood gas analysis in critical care: A
narrative review. Medicina (Kaunas). 61(1337)2025.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Occhipinti R and Boron WF: Role of
carbonic anhydrases and inhibitors in Acid-base physiology:
Insights from mathematical modeling. Int J Mol Sci.
20(3841)2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Hopkins E, Sanvictores T and Sharma S:
Physiology, acid base balance. En: StatPearls. Treasure Island
(FL), StatPearls Publishing, 2025.
|
|
9
|
MDCalc: Winters' Formula for metabolic
acidosis compensation. Available from: https://www.mdcalc.com/calc/117/winters-formulametabolic-acidosis-compensation.
Accessed April 9, 2025.
|
|
10
|
Castro D, Patil SM, Zubair M and Keenaghan
M: Arterial blood gas. En: StatPearls. Treasure Island (FL),
StatPearls Publishing, 2025.
|
|
11
|
Adrogué HJ and Madias NE: Management of
life-threatening acid-base disorders. First of two parts. N Engl J
Med. 338:26–34. 1998.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Adrogué HJ, Gennari FJ, Galla JH and
Madias NE: Assessing Acid-base disorders. Kidney Int. 76:1239–1247.
2009.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Wagner PD: The physiological basis of
pulmonary gas exchange: Implications for clinical interpretation of
arterial blood gases. Eur Respir J. 45:227–243. 2015.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Gattinoni L, Marini JJ, Collino F, Maiolo
G, Rapetti F, Tonetti T, Vasques F and Quintel M: The future of
mechanical ventilation: Lessons from the present and the past. Crit
Care. 21(183)2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Kraut JA and Madias NE: Metabolic
acidosis: Pathophysiology, diagnosis and management. Nat Rev
Nephrol. 6:274–285. 2010.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Cecconi M, De Backer D, Antonelli M, Beale
R, Bakker J, Hofer C, Jaeschke R, Mebazaa A, Pinsky MR, Teboul JL,
et al: Consensus on circulatory shock and hemodynamic monitoring.
Task force of the European Society of Intensive Care Medicine.
Intensive Care Med. 40:1795–1815. 2014.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Severinghaus JW, Astrup P and Murray JF:
Blood gas analysis and critical care medicine. Am J Respir Crit
Care Med. 157 (Suppl):S114–S122. 1998.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Baird G: Preanalytical considerations in
blood gas analysis. Biochem Med (Zagreb). 23:19–27. 2013.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Muhammed A, Abdalgadir Hamdnaalla M,
Fakher Aldeen Noman F, et al: Assessing and Enhancing the
Interpretation Quality of Arterial Blood Gas Among Junior Doctors.
Cureus. 17(e87241)2025.PubMed/NCBI View Article : Google Scholar :
doi:10.7759/cureus.87241.
|
|
20
|
Saberian L, Sharif M, Aarabi M, Broumand B
and Shafiee MA: Arterial versus venous blood gas analysis
comparisons, appropriateness, and alternatives in different
acid/base clinical settings: a systematic review. Cureus.
15(e41707)2023.doi: 10.7759/cureus.41707.
|
|
21
|
D'Orazio P, Toffaletti JG, Ehrmeyer SS,
Wandrup DrMed C, Scient J and Facb EJP: Blood Gas and pH Analysis
and Related Measurements. 2nd Edition. Clinical and Laboratory
Standards Institute, Wayne, PA, 2009.
|
|
22
|
Goossen RL, Schultz MJ, Tschernko E, Chew
MS, Robba C, Paulus F, van der Heiden PLJ and Buiteman-Kruizinga
LA: Effects of closed loop ventilation on ventilator settings,
patient outcomes and ICU staff workloads-a systematic review. Eur J
Anaesthesiol. 41:438–446. 2024.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Mahapatra C: Recent advances in medical
gas sensing with artificial intelligence-enabled technology. Med
Gas Res. 15:318–326. 2025.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Pooja M, Karun KM and Madathil RK:
Comparison of average Blood Gas parameters between arterial blood
& capillary blood in neonates: A protocol for systematic review
and meta-analysis. Int J Health Sci Res. 14:170–174. 2024.
|
|
25
|
Lumholdt M, Andreasen JB, Damgaard K,
Christensen EF, Leutscher PDC and Rasmussen BS: Comparison of
venous and calculated blood gas values to arterial values in
critically ill patients. Acta Anaesthesiol Scand.
69(e14555)2025.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Park JE, Kim DY, Park JW, Jung YJ, Lee KS,
Park JH, Sheen SS, Park KJ, Sunwoo MH and Chung WY: Development of
a machine learning model for predicting ventilator weaning outcomes
based solely on continuous ventilator parameters during spontaneous
breathing trials. Bioengineering. 10(1163)2023.PubMed/NCBI View Article : Google Scholar : https://doi.org/10.3390/bioengineering10101163.
|
|
27
|
Turan Eİ, Baydemir AE, Balıtatlı AB and
Şahin AS: Assessing the accuracy of ChatGPT in interpreting blood
gas analysis results ChatGPT-4 in blood gas analysis. J Clin
Anesth. 102(111787)2025.PubMed/NCBI View Article : Google Scholar : doi:
10.1016/j.jclinane.2025.111787.
|
|
28
|
Vitazkova D, Foltan E, Kosnacova H, Micjan
M, Donoval M, Kuzma A, Kopani M and Vavrinsky E: Advances in
respiratory monitoring: A comprehensive review of wearable and
remote technologies. Biosensors (Basel). 14(90)2024.PubMed/NCBI View Article : Google Scholar
|