Introduction
Melkersson-Rosenthal syndrome (MRS) is a rare
neuro-mucocutaneous disorder characterized by a clinical triad
consisting of recurrent orofacial edema, peripheral facial
paralysis and a fissured tongue (1).
However, the complete triad is observed in only 8 to 25% of cases,
with monosymptomatic presentations being more common. Among these,
orofacial edema is the predominant manifestation, occurring in ~80%
of patients (2). The estimated
prevalence of MRS is <0.1% in the general population. It is most
frequently diagnosed in the second and third decades of life, and
its occurrence during childhood or in older adults is exceptional
(3). Pathophysiology remains poorly
understood, although proposed mechanisms include an autosomal
dominant inheritance with variable penetrance, along with possible
contributions from immunologic, infectious, or allergic factors
(4).
Diagnosis is primarily clinical and relies on
identifying the characteristic signs, while excluding other causes
of recurrent facial edema and facial palsy. In cases with atypical
or incomplete presentations, the biopsy of affected tissues may be
useful, often revealing a non-caseating granulomatous inflammatory
infiltrate consistent with granulomatous cheilitis. However, these
findings are not pathognomonic, and their absence does not rule out
the diagnosis (5).
The management of MRS focuses on symptom control.
Systemic or intralesional corticosteroids are the mainstay for
treating acute episodes, providing favorable outcomes in reducing
edema and facial palsy. In chronic or refractory cases,
immunosuppressive agents such as methotrexate, azathioprine, or
even biological therapies targeting tumor necrosis factor
(anti-TNF) have been proposed. Surgical intervention may also be
considered for patients with persistent lip edema or severe facial
dysfunction unresponsive to medical therapy (6).
Given the broad clinical spectrum of MRS and the
fact that the majority of patients do not present with the complete
triad of symptoms, reporting atypical or incomplete cases is
crucial to improving clinical recognition. These cases highlight
the diagnostic challenges posed by overlapping symptoms with
infectious, allergic, or autoimmune conditions and underscore the
importance of a thorough differential diagnosis.
In this context, the present study reports the case
of a 22-year-old male patient with facial swelling and palsy, whose
diagnosis of MRS was particularly challenging due to the presence
of systemic symptoms, such as fever and the absence of the classic
fissured tongue. The present case report aimed to emphasize the
atypical nature of the presentation, discuss the diagnostic
difficulties, and provide educational value for clinicians who may
encounter similar scenarios.
Case report
The present study describes the case of a
22-year-old male patient from Tuxtla Gutiérrez, Chiapas, Mexico.
The patient was a university student with no relevant medical
history, who experienced a first episode of left-sided facial
paralysis in June, 2022. He was treated at 'Dr. Belisario
Domínguez’ General Hospital ISSSTE, Tuxtla Gutiérrez, Chiapas,
Mexico with prednisone (5 mg) and antihistamines, exhibiting a
favorable response. In November, 2022, he developed dermatosis
characterized by edema of the right cheek, which progressively
extended to the remainder of his face (Fig. 1). This was accompanied by
intermittent fever reaching up to 38˚C, predominantly in the late
afternoon and evening, which was resolved with antipyretics. The
patient also reported unintentional weight loss and alopecia.
The diagnostic evaluation began in March, 2023.
Laboratory tests revealed decreased C1q complement levels (54.3
mg/dl) and positive antinuclear antibody (ANA) with a titer of 1:80
and a cytoplasmic reticular immunofluorescence pattern.
Anti-double-stranded DNA, anti-Ro, anti-La and ANCA antibodies were
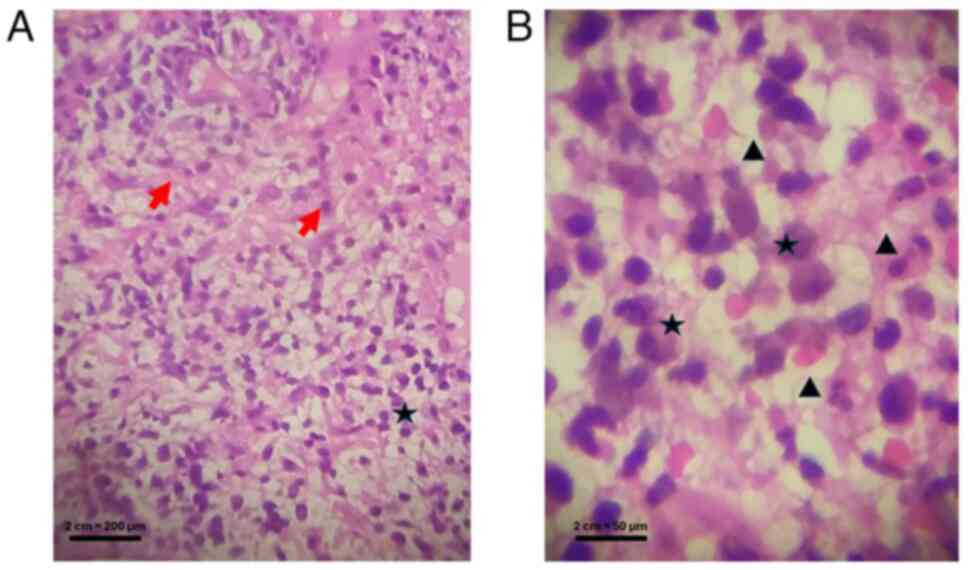
negative. In December, 2023, a biopsy of the lower lip mucosa was
performed. A histological evaluation was performed on
formalin-fixed, paraffin-embedded tissue sections of the lip
mucosa. The samples were sectioned at a thickness of 4 µm, mounted
on positively charged glass slides (Superfrost™ Plus, Thermo Fisher
Scientific, Inc.) and dried overnight at 37˚C. The sections were
then deparaffinized in xylene (cat. no. 534056, MilliporeSigma) and
rehydrated through a graded ethanol series (100, 95 and 70%) to
distilled water. Routine hematoxylin and eosin (H&E) staining
was performed using Mayer's hematoxylin (cat. no. 1.09249.0500,
Merck KGaA) and eosin Y alcoholic solution (cat. no. E4382,
MilliporeSigma). The slides were subsequently dehydrated in
ascending ethanol concentrations, cleared in xylene and mounted
with synthetic resin (cat. no. 1.07961.0100, Entellan™ New, Merck
KGaA).
No immunohistochemical staining was applied to this
specimen. Histopathological analysis revealed moderate irregular
acanthosis, focal hydropic degeneration of the basal layer, and a
dense mixed inflammatory infiltrate composed of lymphocytes,
histiocytes, neutrophils and plasma cells, along with dilated and
congested blood vessels (Fig.
2).
Based on the clinical presentation and
histopathological findings, a diagnosis of MRS was established.
Treatment was initiated in January, 2024 with deflazacort at 12
mg/day, epinastine at 20 mg/day and methotrexate at 10 mg/week for
6 months, resulting in a marked clinical improvement of the
dermatosis without any side-effects (Fig. 1B).
Discussion
The present study describes the case of a young male
patient with a history of unilateral facial paralysis who
subsequently developed persistent facial edema; the
histopathological findings consistent with granulomatous cheilitis,
and favorable clinical improvement following treatment with
corticosteroids and immunomodulators. These elements led to the
diagnosis of MRS, a rare condition whose incomplete presentation
may hinder timely recognition.
MRS is an uncommon neuro-mucocutaneous disorder
characterized by the classic triad of recurrent orofacial edema,
peripheral facial palsy and fissured tongue. Although it can occur
at any age, it is most prevalent between the second and fourth
decades of life, with a 2:1 female predominance (X-5). Pediatric
cases are rare, but have been reported in children between 7 and 12
years of age. The overall incidence in the general population is
estimated to be approximately 0.08% (7).
The etiology of MRS remains unclear, although
several predisposing factors have been proposed. Infectious agents,
such as Epstein-Barr virus, cytomegalovirus and SARS-CoV-2 have
been implicated, along with bacteria such as Mycobacterium
tuberculosis. Associations have also been described with atopy,
food allergies, exposure to environmental antigens and
hypersensitivity reactions to monosodium glutamate; however,
conclusive evidence of causality is lacking (8,9).
Dysregulated immune responses are also considered relevant
(10,11).
Clinically, MRS may present in complete or partial
forms. The classic triad of symptoms is present in only 8 to 18% of
cases. The most common manifestation is recurrent orofacial edema,
typically painless, unilateral, and most frequently affecting the
upper lip. Edema may extend to the cheeks, palate, tongue, gums,
periorbital region, pharynx, or larynx (12). Facial palsy occurs in 50 to 90% of
cases and is generally unilateral and transient, while a fissured
tongue is observed in up to 40% of patients (13-15).
The diagnosis of MRS poses a clinical challenge due
to the absence of standardized diagnostic criteria or specific
biomarkers. Diagnosis is primarily clinical, based on the
recognition of characteristic signs and exclusion of other
conditions with similar symptoms. Biopsy may be useful in atypical
or incomplete cases. In the early stages, histological findings are
often non-specific, featuring edema and a mixed inflammatory
infiltrate. In advanced stages, non-caseating granulomas may be
observed, such as those observed in sarcoidosis or Crohn's disease
(16).
In the patient described herein, the presence of
fever and the absence of fissured tongue complicated the diagnostic
process, as systemic symptoms such as fever are rarely reported in
MRS. This required a careful differential diagnosis, including
infectious etiologies, such as bacterial abscesses, viral
reactivations and Hansen's disease, as well as non-infectious
causes such as sarcoidosis, angioedema, Crohn's disease and
lymphoproliferative disorders. Ultimately, the combination of
persistent orofacial edema, recurrent facial palsy and
histopathological features consistent with granulomatous cheilitis
supported the diagnosis of MRS.
The differential diagnosis is broad and should
include hereditary or acquired angioedema, Hansen's disease,
sarcoidosis, dental absences, lymphomas, trauma and other
granulomatous disorders, such as Wegener's granulomatosis,
amyloidosis, specific infections, or foreign body reactions
(17). There is no standardized
treatment for MRS; management focuses on symptom control. Systemic
or intralesional corticosteroids remain the cornerstone of therapy,
with recommended courses lasting 3 to 6 weeks using prednisone or
triamcinolone in combination with antihistamines (18). Antibiotics may be indicated in cases
with bacterial superinfection. Immunomodulatory agents such as
azathioprine, methotrexate, thalidomide, tacrolimus and
antimalarials such as chloroquine have exhibited efficacy in
refractory cases (19). Biological
therapies such as infliximab or adalimumab (anti-TNF-α) have also
demonstrated benefit. Physical therapy may help preserve muscular
function in patients with facial paralysis. In most cases, facial
palsy is resolved spontaneously within approximately three weeks.
Reconstructive surgery is reserved for cases with persistent or
refractory edema, while surgical decompression of the facial nerve
may be considered in selected cases when compression is presumed to
be the underlying mechanism (12).
In the patient in the present study, corticosteroid
therapy led to clinical improvement; however, methotrexate was
introduced as a steroid-sparing agent to minimize the risks of
long-term corticosteroid exposure. Although methotrexate is not
universally required in MRS, its use has been supported in
recurrent or persistent cases, and previous reports describe its
efficacy as part of immunomodulatory therapy (20-22).
This rationale guided the therapeutic decision for the present
case.
Compared with previous case reports, the novelty of
the present case report lies in the atypical presentation,
particularly the association with systemic symptoms (fever), an
incomplete clinical triad and inconclusive early histopathology. By
highlighting these features, the present case report adds
educational value for clinicians and underscores the need to
consider MRS even in patients who do not fully meet the classic
diagnostic triad (23).
The present case report has several limitations
which should be mentioned. First, the absence of long-term
follow-up data precludes evaluation of recurrence patterns,
sustained treatment response, and potential late complications.
Second, as with all single-patient case reports, the findings
cannot be generalized, and causality between clinical
manifestations and therapeutic outcomes cannot be firmly
established. Finally, histopathological findings in this case were
not pathognomonic, which reflects the inherent diagnostic
uncertainty in atypical forms of MRS. Despite these limitations,
the present case report underscores the importance of documenting
incomplete or unusual presentations of MRS, particularly those
associated with systemic symptoms such as fever, which are rarely
described in the literature. From a clinical perspective, the
present case report highlights the need for heightened awareness of
diagnostic challenges and for careful differential diagnosis in
patients presenting with orofacial edema and facial palsy (24,25).
Future research is required to focus on larger case series or
prospective registries to better characterize the full clinical
spectrum of MRS, identify reliable diagnostic biomarkers, and
evaluate the long-term efficacy and safety of different therapeutic
strategies, including corticosteroid-sparing immunomodulators such
as methotrexate.
In conclusion, the present case report highlights
the importance of including MRS in the differential diagnosis of
recurrent facial paralysis and persistent orofacial edema, even in
the absence of the complete triad of symptoms. A histopathological
evaluation and a comprehensive clinical approach are essential for
timely diagnosis and appropriate management. Documenting atypical
cases such as the one presented herein contributes to a broader
understanding of this rare condition and may facilitate its
recognition in unconventional clinical scenarios.
Acknowledgements
The authors would like to sincerely thank Dr María
José Calvo Domínguez, from ‘'Dr. Belisario Domínguez’ General
Hospital ISSSTE, Tuxtla Gutiérrez, Chiapas, Mexico, for her
invaluable support and guidance during the preparation of this
manuscript. Her generosity in sharing her expertise and insights
was instrumental to the development of this work.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
ATSV was the main contributor to the conception of
the study as well as to the literature search for related studies.
APT, MJCD, MPPA and VIMP were involved in the literature review, in
the writing of the manuscript, and in the analysis and
interpretation of the patient´s data. All authors confirm the
authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent for
participation
The present study was performed in accordance with
the ethical standards of the Declaration of Helsinki 1964. The
patient provided written informed consent for his participation in
the present case report.
Patient consent for publication
The patient provided written informed consent for
the publication of the present case report and all accompanying
images, including those that contain potentially identifiable
features.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Lin TY, Chiang CH and Cheng PS:
Melkersson-Rosenthal syndrome. J Formos Med Assoc. 115:583–584.
2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Cancian M, Giovannini S, Angelini A,
Fedrigo M, Bendo R, Senter R and Sivolella S: Melkersson-Rosenthal
syndrome: A case report of a rare disease with overlapping
features. Allergy Asthma Clin Immunol. 15(1)2019.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Dhawan SR, Saini AG and Singhi PD:
Management strategies of Melkersson-Rosenthal syndrome: A review.
Int J Gen Med. 13:61–65. 2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Carolino F, Fernandes M and Plácido JL:
Melkersson-Rosenthal syndrome-delay in the diagnosis of an
early-onset oligosymptomatic variant. Porto Biomed J. 1:43–45.
2016.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Wehl G and Rauchenzauner M: A systematic
review of the literature of the three related disease entities
cheilitis granulomatosa, orofacial granulomatosis and
Melkersson-Rosenthal syndrome. Curr Pediatr Rev. 14:196–203.
2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Zewde YZ: Melkersson-Rosenthal syndrome
misdiagnosed as recurrent Bell's palsy: A case report and review of
literature. Allergy Asthma Clin Immunol. 17(8)2021.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Mansour M, Mahmoud MB, A Kacem, Zaouali J
and Mrissa R: Melkersson-Rosenthal syndrome: About a Tunisian
family and review of the literature. Clin Neurol Neurosurg.
185(105457)2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Apaydin R, Bilen N, Bayramgürler D, Efendi
H and Vahaboğlu H: Detection of Mycobacterium tuberculosis
DNA in a patient with Melkersson-Rosenthal syndrome using
polymerase chain reaction. Br J Dermatol. 142:1251–1252.
2000.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Taşlıdere B, Mehmetaj L, Özcan AB, Gülen B
and Taşlıdere N: Melkersson-Rosenthal syndrome induced by COVID-19.
Am J Emerg Med. 41:262.e5–262.e7. 2021.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Ibrahim A, Ibrahim M, Al Adawi M, Oweis L
and Bahou Y: Think Melkersson-Rosenthal syndrome: A fissured tongue
with facial paralysis. Cureus. 12(e9480)2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Pei Y, Beaman GM, Mansfield D,
Clayton-Smith J, Stewart M and Newman WG: Clinical and genetic
heterogeneity in Melkersson-Rosenthal syndrome. Eur J Med Genet.
62(103536)2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Alencar TN, Botelho MM, Carasek N and
Bahmad F: Surgical treatment outcome for familial
Melkersson-Rosenthal syndrome. Am J Case Rep.
24(e938670)2023.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Sharma DR, Resident S, Mohan C, Minnas RS,
Mohindroo NK and Sharma ML: Melkersson-Rosenthal syndrome. Indian J
Otolaryngol Head Neck Surg. 51:30–31. 1999.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Giudici N, Bianchetti MG, Ramelli GP and
Milani GP: Recurrent episodes of peripheral facial nerve palsy and
fissured tongue. J Paediatr Child Health. 53(609)2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Jasinska D and Boczon J:
Melkersson-Rosenthal syndrome as an early manifestation of mixed
connective tissue disease. Eur J Med Res. 20(100)2015.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Luo X, Wang J, Zeng X and Kuang W:
Research progress on Melkersson-Rosenthal syndrome. Zhejiang Da Xue
Xue Bao Yi Xue Ban. 50:148–154. 2021.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Gavioli CFB, Cidade Y da SA, Florezi GP,
Lourenço SV and Nico MMS: Melkersson-Rosenthal syndrome in children
and adolescents: A series of seven cases. An Bras Dermatol.
97:676–681. 2022.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Wu A, Zhang Y, Cao W, Wang X, Song Z,
Jaspers RT, Chen L, Pathak JL and Zhang Q: A case of
Melkersson-Rosenthal syndrome with temporomandibular joint
osteoarthritis: Multidisciplinary treatment and autoimmune
etiological hypothesis. BMC Oral Health. 24(935)2024.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Pathania YS: Current treatment modalities
in granulomatous cheilitis. Int J Dermatol. 61:755–759.
2022.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Chan J: Methotrexate for the treatment of
Corticosteroid-dependent asthma. Can J Hosp Pharmacy. 42:39–40.
1989.
|
|
21
|
Coffey MJ, Sanders G, Eschenbacher WL,
Tsien A, Ramesh S, Weber RW, Toews GB and McCune WJ: The role of
methotrexate in the management of steroid-dependent asthma. Chest.
105:117–121. 1994.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Davies H, Olson L and Gibson PG:
Methotrexate as a steroid sparing agent for asthma in adults.
Cochrane Database Syst Rev. 1998(CD000391)2000.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Dixit A: Melkersson-Rosenthal syndrome
associated with anti-RNP positive undifferentiated connective
tissue disease in a young female: Case report and review of
literature. Egypt J Intern Med. 37(109)2025.
|
|
24
|
Elendu C, Osamuyi EI, Afolayan IA, Opara
NC, Chinedu-Anunaso NA, Okoro CB, Nwankwo AU, Ezidiegwu DO, Anunaso
CA, Ogbu CC, et al: Clinical presentation and symptomatology of
Guillain-Barré syndrome: A literature review. Medicine (Baltimore).
103(e38890)2024.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Mohammadi K, Faramarzi S, Yaribash S,
Valizadeh Z, Rajabi E, Ghavam M, Samiee R, Karim B, Salehi M, Seifi
A and Shafaati M: Human metapneumovirus (hMPV) in 2025: Emerging
trends and insights from community and hospital-based respiratory
panel analyses-a comprehensive review. Virol J.
22(150)2025.PubMed/NCBI View Article : Google Scholar
|