Introduction
During pregnancy and the peripartum period, there
are changes in the coagulation system, which may lead to a
physiological hypercoagulable state (1). Hemodynamic factors and venous stasis
are certain factors that increase the risk of suffering an ischemic
stroke in pregnant women (2). These
changes predispose the pregnant patient to higher rates of
prothrombotic events, such as deep vein thrombosis, superficial
vein thrombosis, pulmonary thromboembolism or ischemic stroke
(3). Although pregnancy generally
increases the risk of developing thrombosis, the highest risk is
during peripartum period, which is ≤12 weeks following delivery
(4). Statistically, the majority of
stroke cases occur following delivery (50%) and in the peripartum
period (40%), with the lowest probability (10%) in the antepartum
period (5).
Imaging in pregnant patients is a diagnostic dilemma
due to radiation exposure (6).
Certain factors that influence the potentially harmful effects of
radiation from CT scans for pregnant patients are as follows:
Gestational age, the total dose of radiation that the patient is
exposed to, fetal exposure to radiation, and the need for the
administration of contrast agents. Whilst fetal exposure to
radiation from head CT scans is extremely low, the radiation dose
is markedly higher during head CT scans with intravenous contrast
due to multiple additional scans (7). Therefore, magnetic resonance imaging
(MRI) is the recommended imaging method, using
non-contrast-enhanced time-of-flight magnetic resonance angiography
(6).
Previous studies recommend that thrombolysis should
be considered when the expected benefits of treating
life-threatening or debilitating stroke outweigh the risk of
uterine bleeding (8,9). However, at present, to the best of our
knowledge, there are no randomized controlled trials that have
evaluated pregnant patients with thromboembolism. A recent review
highlighted that the risk associated with thrombolytic agents in
pregnant patients appears reasonable when balanced with the risk
associated with a disease that places the life of the patient in
danger (1). In addition, it has been
reported that the complications rate of thrombolysis in pregnant
patients is not higher than that of non-pregnant patients (1,3). In a
previous review article, of the 30 pregnant patients suffering a
thrombolysed stroke included in the review, the main complications
described were the following: Major bleeding (n=1), maternal
mortality due to arterial dissection (n=1), and spontaneous
abortions (n=3) (1). However,
pregnancy is still considered a relative contraindication for
thrombolysis (1).
Certain case studies have suggested that mechanical
thrombectomy can be performed safely during pregnancy, particularly
for pregnant patients who present with severe stroke [demonstrated
by high National Institutes of Health Stroke Scale (NIHSS) scores]
(6,9). The patients in these cases experienced
excellent recovery and there was no impact on the infants (6). Moreover, it is widely accepted that
mechanical thrombectomy in pregnant patients is technically
feasible with acceptable rates of recanalization and maternal
outcomes and fetal outcomes (8).
Mechanical thrombectomy using the Penumbra system appears to be a
safe and effective treatment option for acute ischemic stroke
during pregnancy when thrombolysis is unsuitable (10). Therefore, mechanical thrombectomy
should be considered for pregnant patients as would be indicated in
non-pregnant patients (8).
Case report
A 29-year-old female patient, who was 38 weeks
pregnant, presented at the Emergency Room of University Emergency
Hospital of Bucharest, Romania, on a Sunday, in June 19, 2023. This
was the patient s first pregnancy, with no previous
spontaneous abortions. A cesarean section was scheduled for the
following day as the patient had two placentas. The patient was a
smoker (10 pack years), with no history of gestational diabetes,
preeclampsia, eclampsia or hypertension.
The patient was admitted to the hospital for sudden
onset symptomatology characterized by a motor deficit and numbness
of the right upper limb associated with pronunciation disorder. The
neurological clinical examination upon admission revealed the
following: Mild-moderate dysarthria (slurred speech, but
understandable); minor paralysis (flat nasolabial fold, smile
asymmetry); right brachial mono paresis 3/5 on the Medical Research
Council (MRC) scale; mild-moderate sensory loss on the right upper
arm; and ataxia in right upper arm. The patient had an a NIHSS
score of 7 points, and the score was disabling, in that the patient
was a 29-year-old with motor deficits in the dominant hand and who
was due to have a newborn the following day. Moreover, the patient
presented in the revascularization window at ~30 min from
symptomatology onset, as a thrombolysis code.
In terms of the diagnostic approach, in numerous
developing countries, including Romania, a routine cerebral MRI is
not commonly performed in emergency settings due to a combination
of factors, such as limited healthcare resources and infrastructure
challenges. Furthermore, Romania is still struggling to meet the
European standards of quality in healthcare (11). The patient in the present case report
was admitted during the night on a weekend; therefore, MRI was not
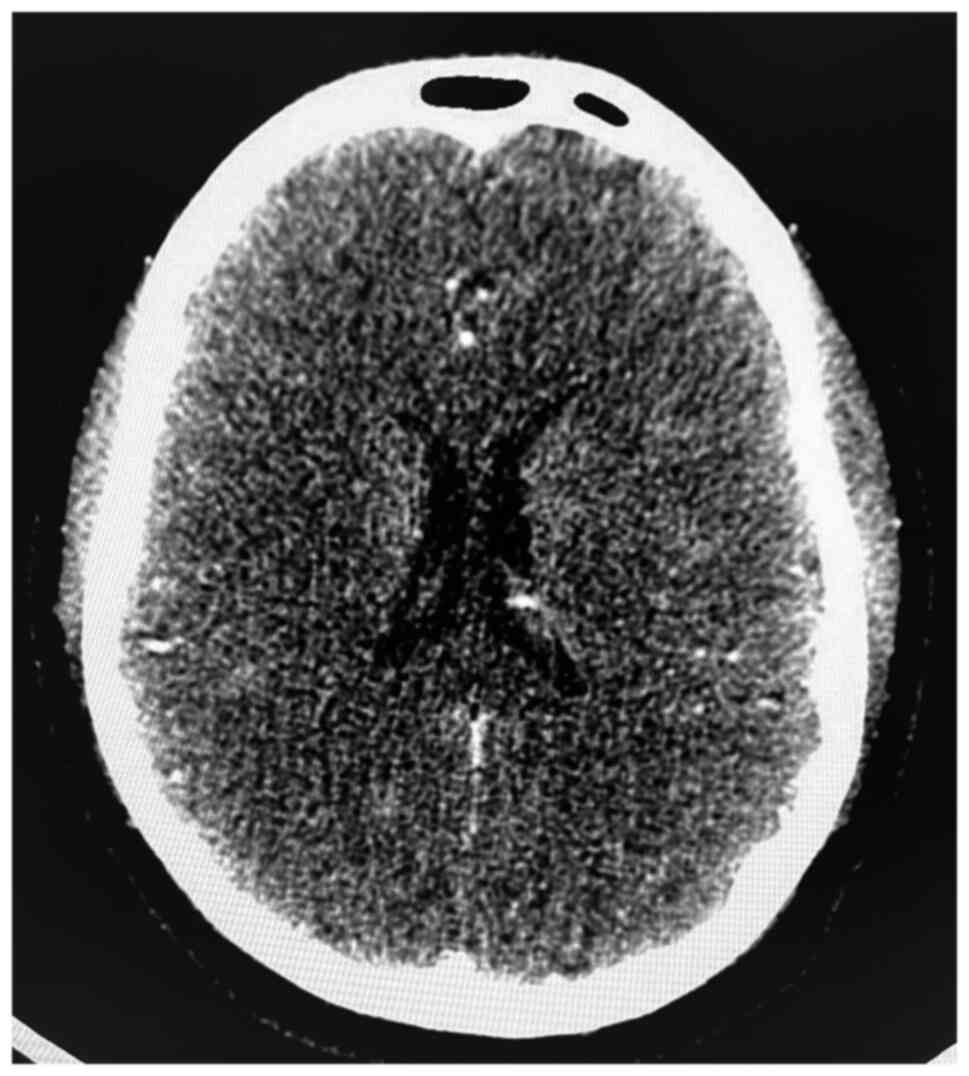
available. As a result, the first radiological investigation was a
native brain CT scan (intravascular contrast being avoided in
pregnancy), which did not reveal any cranial lesions. The native
cerebral CT scan in presented in Fig.
1. The clear native cerebral CT scan excluded other pathologies
that would explain a sudden neurological deficit (such as a
cerebral tumor) or that could contraindicate revascularization
therapy (such as hemorrhagic stroke). Given the pregnancy, medical
revascularization therapy with tissue plasminogen activator (tPA)
was excluded. Moreover, as a CT scan with contrast or a CT
angiography of the cerebral arteries were contraindicated in
pregnancy, and as the patient was at 38 weeks of gestation with a
viable fetus ready for delivery, a multidisciplinary team
comprising a neurologist and an obstetrician recommended an
emergency cesarean section. Although the procedure was planned for
the following day, the urgency of the case and the consent of the
family supported proceeding without delay. Following the delivery,
the neurological deficits persisted, with a NIHSS score of 7
points. Furthermore, even though the patient was still in the
thrombolysis window of 4.5 h following delivery, the major surgery
contraindicated revascularization with tPA due to the massive
hemorrhagic risk. However, the patient was still eligible for
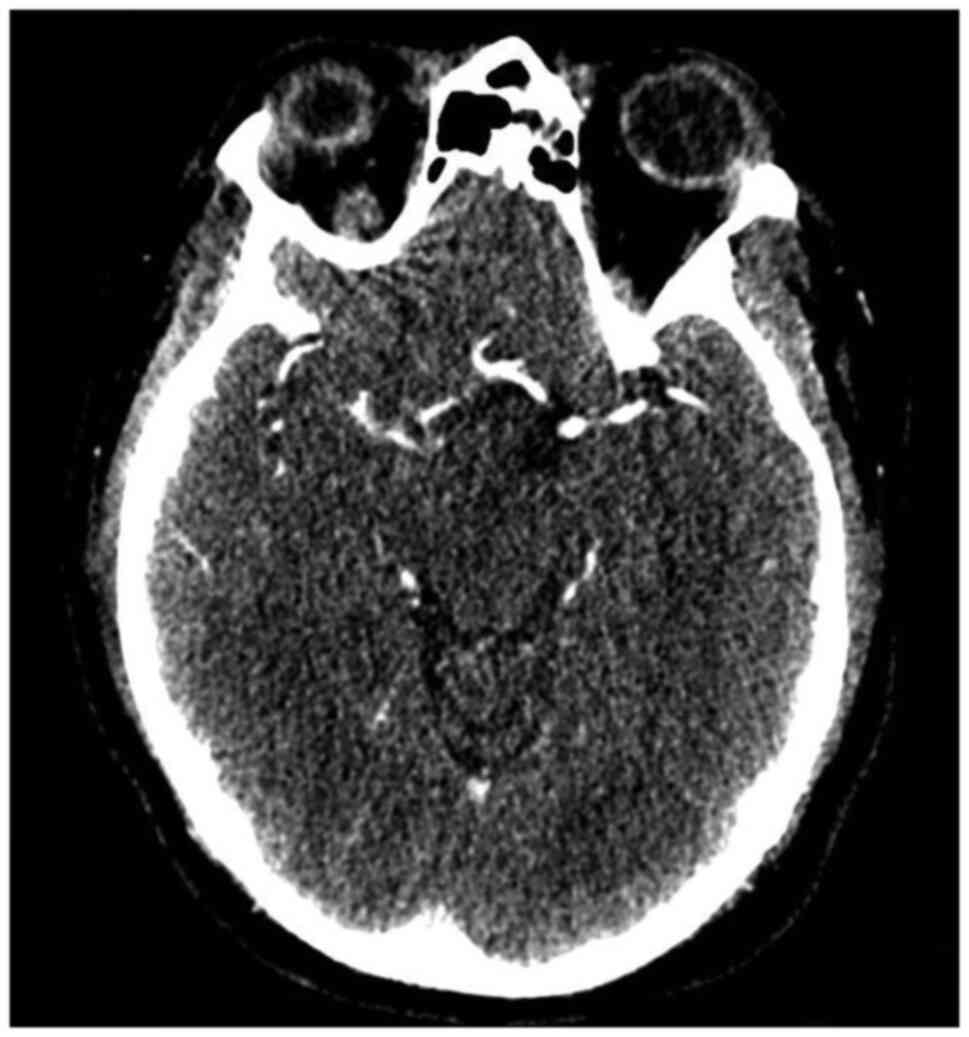
mechanical revascularization. Therefore, the patient underwent CT
angiography of the cerebral arteries, which did not detect large
vessel occlusion, and finally, mechanical thrombectomy was excluded
and drug treatment for secondary prevention with aspirin was
decided. The CT angiography of the cerebral arteries in presented
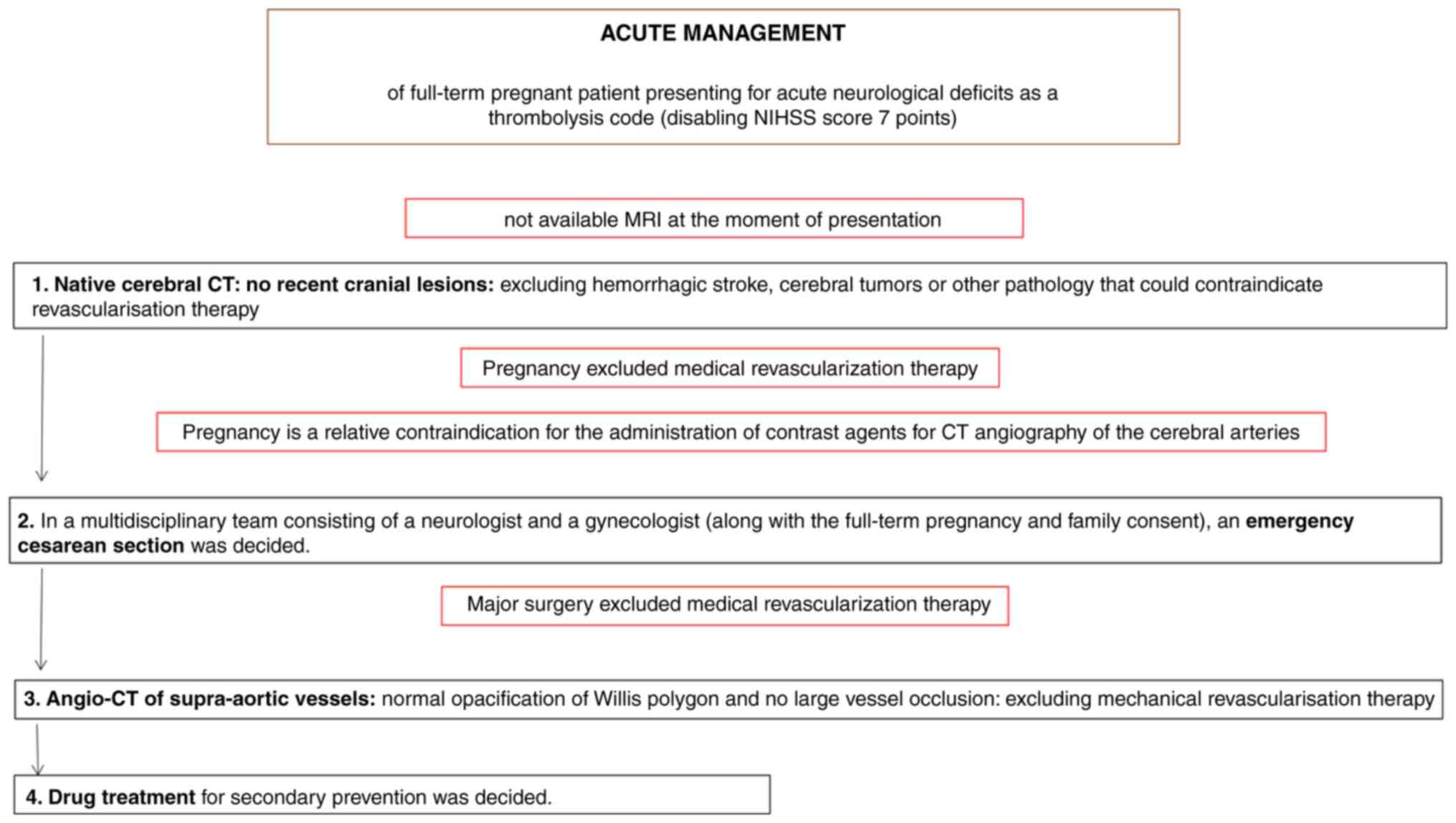
in Fig. 2. The acute management of
the patient is presented in Fig.
3.
The neonatal outcomes were favorable, with a
birthweight of 2.840 g, an Apgar score of 9, with favorable
neonatal adaptation and an increasing weight-growth curve. The
mother demonstrated an excellent post-operative recovery: On
post-operative day 1, the patient was mobilized, able to sit up and
ambulate without assistance. The motor deficit was limited to the
right upper limb (3/5 MRC). The patient reported no notable
abdominal pain and vital signs remained stable throughout. Wound
healing proceeded without complications, and the overall functional
status of the patient improved, allowing the performance of routine
maternal duties. By the end of the hospitalization period (from
June 19 until June 30, 2023), the patient was able to feed the
newborn with a bottle, even with a motor deficit in the right hand,
demonstrating marked adaptability and resilience.
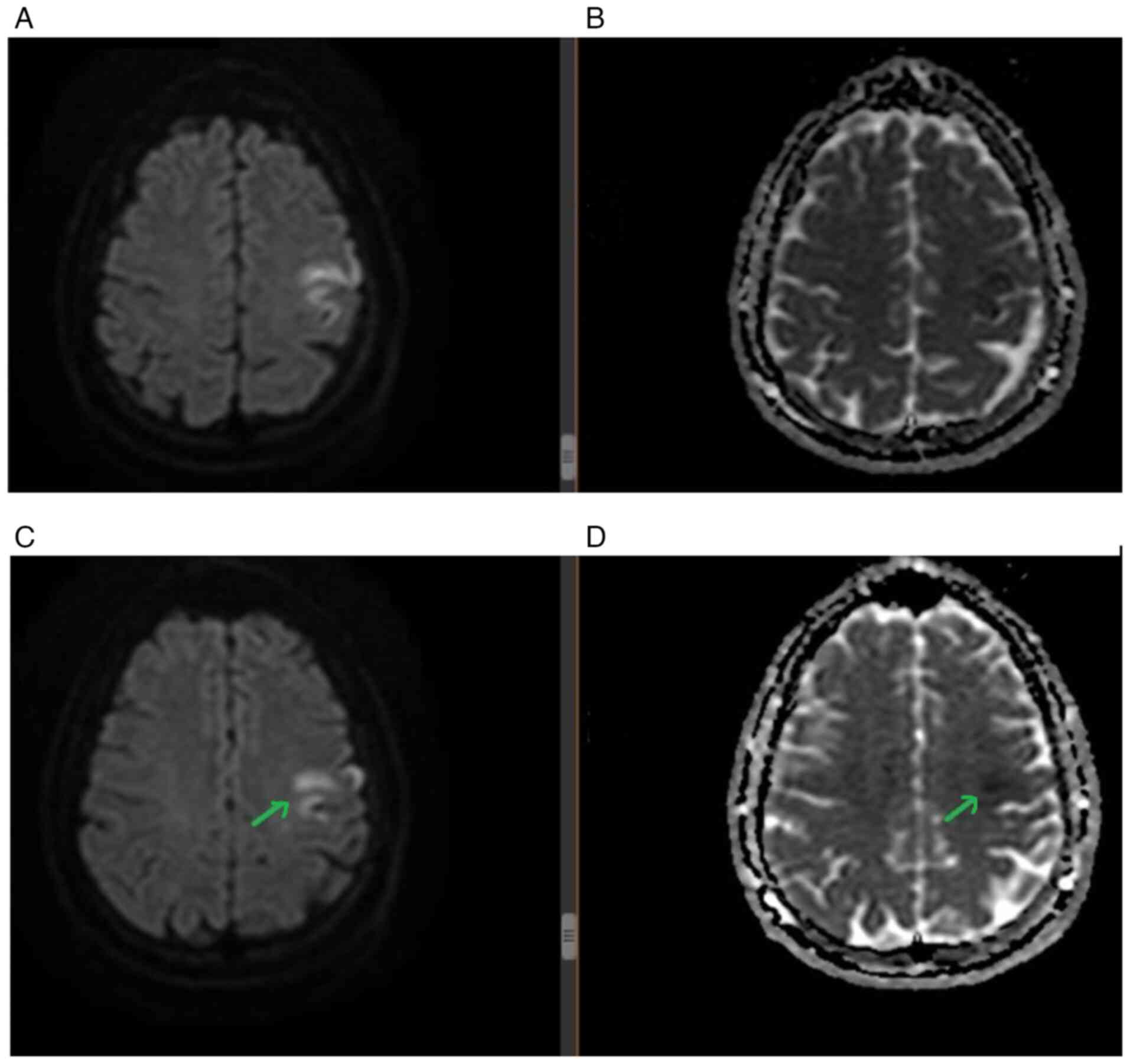
During admission, several paraclinical
investigations were performed. A brain MRI revealed a hyperintense
lesion in diffusion sequence with low apparent diffusion
coefficient correspondence at the frontal level of the left side,
affecting middle gyrus and precentral gyrus (Fig. 4). A Doppler ultrasound of
cervico-cerebral vessels did not detect atheroma plaques. A 24-h
electrocardiogram did not reveal atrial fibrillation episodes;
however, an outpatient extended cardiac rhythm monitoring was
recommended for 3-7 days. Microemboli detection revealed the
passage of 8-10 microemboli, suggestive of an interatrial
communication. A subsequent transesophageal ultrasound revealed a
small patent foramen ovale (PFO), and an 8-point Risk of
Paradoxical Embolism (RoPE) score of PFO was determined (no history
of hypertension, no history of diabetes, stroke or cortical
infarct, and an age of 29 years). This indicated an 84% chance that
the cause of the stroke of the patient was due to PFO. However, the
small anatomical proportions of the PFO did not indicate the need
for interventional closure (12).
Due to the PFO, a compression ultrasound of the lower limbs was
performed, and no deep vein thrombosis was identified. Furthermore,
vitamin B12 deficiency and mild anemia were detected.
However, laboratory tests for the usual hereditary
thrombophilic risk factors for arterial embolism, such as factor V
Leiden (G1691A), prothrombin G20210A, antithrombin deficiency,
protein C and S deficiencies and antiphosolipid syndrome, were
negative. The genotyping of the Factor V Leiden mutation was
performed using a quantitative PCR assay (LightCycler®
Factor V Leiden Mutation Detection kit; cat. no. BM05, Roche
Diagnostics) on the LightCycler® 2.0 instrument,
following the manufacturer s instructions. The prothrombin
G20210A variant was analyzed by quantitative PCR using the
LightCycler® Prothrombin G20210A Mutation Detection kit
(cat. no. BM06, Roche Diagnostics). Antithrombin functional
activity was measured using a chromogenic assay (STA®
Antithrombin; cat. no. HE34, Diagnostica Stago, Inc.), performed on
the STA-R Evolution analyzer. Protein C activity was assessed using
a chromogenic method (Protein C Chromogenic assay; cat. no. HE35,
Siemens Healthineers). Free Protein S antigen was quantified by
immunoturbidimetry (Liatest® Free Protein S; cat. no.
HE36, Diagnostica Stago, Inc.). Testing for lupus anticoagulant
followed the current International Society on Thrombosis and
Haemostasis (ISTH) guidelines and included both screening and
confirmatory assays: dRVVT screen and confirm reagents (LA1/LA2
dRVVT; cat. no. HE32, Werfen/Instrumentation Laboratory) and
aPTT-based lupus-sensitive assay (SynthASil®; cat. no.
HE32, Werfen). IgG and IgM anticardiolipin antibodies were measured
using ELISA kits (QUANTA Lite® ACA IgG/IgM; cat. nos.
IM328, Inova Diagnostics, Inc.). IgG and IgM anti-β2GPI antibodies
were determined using ELISA (QUANTA Lite® β2-GPI
IgG/IgM; cat. no. IM225, Inova Diagnostics, Inc.).
Building upon laboratory investigations suggesting a
potential thrombophilic status, genetic testing revealed a
homozygous mutation in the methylenetetrahydrofolate reductase
(MTHFR) gene and heterozygous mutation in the plasminogen activator
inhibitor-1 gene. The genotyping of MTHFR C677T and A1298C
polymorphisms was performed using
LightCycler®-compatible quantitative PCR assays with
hybridization probes (LightMix® kit MTHFR C677T/A1298C;
cat. no. BM33, TIB MOLBIOL Syntheselabor GmbH). Reactions were run
on the LightCycler® 2.0 instrument following the
manufacturer s protocol. The PAI-1 promoter 4G/5G polymorphism
was detected using a LightCycler®-based quantitative PCR
assay (LightMix® kit PAI-1 4G/5G; cat. no. BM35, TIB
MOLBIOL Syntheselabor GmbH), with allele discrimination performed
by melting-curve analysis on the LightCycler® 2.0
system. The results of thrombophilia screening and genetic
thrombofilia testing are presented in Table I.
 | Table IThrombophilia status results. |
Table I
Thrombophilia status results.
| Laboratory test | Result | Reference
interval |
|---|
| Thrombophilia
screening | | |
|
Factor V
Leiden with activated protein C | 91.1 | 38-144/sec |
|
Factor V
Leiden without activated protein C | 32.2 | 24-184/sec |
|
Activated
protein C ratio | 2.83 | ≥2.3 |
|
Antithrombin
deficiency | 142 | 83-128% |
|
Protein C
deficiency | 135 | 70-140% |
|
Protein S
deficiency | 60.4 | 54.7-123.7% |
|
Lupus
anticoagulant screen | 38.5 | 29-39.76 |
|
Lupus
anticoagulant confirm | 28.9 | 27.6-36 |
|
Homocisteinemia | 7.65 | 4.3-11.1/µmol/l |
| Genetic thrombophilia
testing | | |
|
MTHFR gene:
A1298C mutation | Homozygous
genotype | Negative |
|
MTHFR gene:
C677T mutation | Negative | Negative |
|
PAI-1 gene
(polimorfism 675 4G/5G) | Heterozygote
genotype | Negative |
|
Factor V
Leiden mutation | Negative | Negative |
|
Factor II
(prothrombin) mutation | Negative | Negative |
Due to the existing PFO with a high RoPE score and
positive thrombophilic status, anticoagulation medication was
decided for stroke secondary prevention, during hospitalization and
in the first month after delivery with low molecular weight
heparin, enoxaparin (80 mg, corresponding to 0.8 ml twice daily for
a patient with a weight of 80-kg). Following this period, the
patient received bridging therapy with both enoxaparin and
acenocoumarol for 5 days. After these 5 days, oral anticoagulation
with acenoumarol was dose-adjusted to maintain an international
normalized ratio (INR) of 2.0-3.0. Finally, following adjustments,
the patient remained on a dose of 2 mg of acenocoumarol daily.
Discussion
The first particularity of the present case report
is derived from the therapeutic management: The series of medical
interventions when admitting the 38-week pregnant patient with
acute ischemic stroke in the revascularization window. A native
brain CT was initially performed to rule out another cause of acute
neurological deficit, and after excluding cerebral tumors or
hemorrhagic stroke, an emergency cesarean section was performed
under general anesthesia. Subsequently, a CT angiography of the
cerebral arteries was performed. Finally, a mechanical
revascularization procedure would have followed if a large vessel
occlusion was identified.
The first factor that should highlight potential
thrombolysis in pregnant patients is stroke severity: NIHSS score,
stroke position, consciousness, motor and sensitive deficits,
language disorder and speech disorder (1). The second factor that should be taken
into account is the risk of bleeding, considering previous
pathologies of the patient, such as the bleeding history,
hypertension and other known coagulopathies (1). Personal factors should also be taken
into account, such as age, medical history and body weight
(1). Lastly, from an obstetrical
point of view, the decision to thrombolyze a pregnant patient
should consider gestational age and obstetrical conditions
(1). Other previous personal
pathologies may increase the risk of stroke in pregnancy, such as:
Hematologic diseases (sickle cell anemia, thrombocytopenia and
thrombophilia), cardiac disease (hypertension and heart disease),
diabetes and migraine-type headaches (6). Other risk factors include smoking and
alcohol consumption (5,13).
The second particularity of the present case
originates from the diagnosis of acute ischemic stroke in a
full-term pregnant patient, and the evaluation the possible
etiologies of cryptogenic stroke. Therefore, the present case
report emphasizes the importance of evaluating thrombophilic status
and PFO in patients with ischemic stroke at a young age. The most
probable etiology of the stroke was the procoagulant status of the
patient based on the pregnancy itself, the peripartum period of the
patient and the positive genetic thrombophilic status. Notably, the
patient had no personal history pointing towards this diagnosis,
such as history of spontaneous abortions, superficial or deep
venous thrombosis, or pulmonary thromboembolism.
It has been suggested that PFO is an independent
risk factor for ischemic stroke, particularly in young patients
with cryptogenic stroke; however, the causality between PFO and
ischemic stroke is not yet confirmed (14,15).
Moreover, when patient suffering a stroke is diagnosed with PFO,
this is not an indication that PFO was the cause of the stroke;
therefore, secondary prevention for these patients is still
debatable (14). However, in the
event that a patient suffering a stroke is discovered with both PFO
and prothrombotic coagulopathies, oral anticoagulants should be
considered for secondary prevention, rather than platelet
inhibitors (14). Other studies have
suggested that warfarin is superior to platelet inhibitors as a
secondary prevention for PFO-related stroke cases (16,17).
Moreover, the placement of infarct localization of a
PFO-related stroke is due to the physiopathological mechanism of a
PFO: As they are an interatrial shunt, they will allow smaller
emboli to pass through the PFO (left-right) and then reach multiple
scattered places within the brain on both hemispheres (18). Thus, in terms of imaging
characteristics, PFO-related stroke is usually revealed as a single
cortical ischemic lesion or multiple small scattered ischemic
lesions (18).
For PFO-related strokes, thrombogenic conditions are
usually present, as they lead to a predisposition of venous
thrombus formation and further lead to a paradoxical embolism
(18). Pezzini et al
(14) reported that the G20210A
variant of the prothrombin gene and the G1691A mutation of factor V
gene had a higher rate of prevalence in patients with stroke and
PFO, suggesting a possible pathophysiological role of these minor
thrombophilias. By contrast, their study also reported that the
homozygous deficient TT MTHFR genotype was not a genetic minor
thrombophilia found in patients with PFO-related stroke (14). Furthermore, a recent study reported
that usual risk factors for stroke (such as smoking, dyslipidemia
or diabetes) are not associated with risk for PFO-related stroke
(19). Moreover, that study
highlighted that thrombophilias or intracardiac shunt size are not
associated with stroke occurrence in patients with PFO (19).
Lastly, the third particularity of the present case
comes from the medication treatment. From a neurological
perspective, secondary prevention following cryptogenic stroke is
generally achieved with aspirin or a direct oral anticoagulant. A
total of two large randomized trials, NAVIGATE ESUS and RE-SPECT
ESUS, evaluated the efficiency of rivaroxaban and dabigatran,
respectively, compared with aspirin; however, the results
demonstrated no definitive superiority of direct oral
anticoagulants over aspirin, and the evidence remains under
evaluation (19-21).
However, for the patient in the present case report, with both PFO
and positive thrombophilic status, anticoagulation was decided as
secondary prevention: Considering the postpartum status of the
patient, low molecular weight heparin was administered for the
first month following delivery, and acenocoumarole was then
administered for the ensuing 3 months.
Furthermore, from a psychological perspective,
following ischemic stroke, young adults are more predisposed to
fatigue, depression and anxiety (23,24).
Other feelings may include anger, denial, frustration, negative
body image and impaired self-esteem (24). Additionally, certain common practical
problems that young stroke survivors experience are family
conflicts, loss of home, loss of employment and loss of spouse
(25), with psychological
adjustments including reduced quality of life (associated with
dependence, being single and unemployment), financial stress,
conflicts with spouses, children, childcare difficulties, sexual
problems, separation, reduced social and leisure activities,
disruption of self and identity and reduced life satisfaction
(24). It has been suggested that
depot injectable medication may increase quality of life in
patients with psychotic symptoms (26). Furthermore, pregnancy and the
peripartum period is considered a critical period for marriage, and
pregnant women are at risk for developing marital burnout (27). Burnout syndrome is characterized by
psychiatric, psychosomatic, somatic and social symptoms; whilst
chronic fatigue, continuous exhaustion and mental stressors may
arise during pregnancy and peripartum; therefore, this is a period
where women are predisposed to burnout syndrome (28). Medical treatment for psychiatric
symptoms in pregnant patients or patients during the peripartum
period should be carefully considered and given only if the
benefits exceed the risks for the infant.
In conclusion, the particularity of the case
described herein originates from the series of medical
interventions in a full-term pregnant patient who presented with
acute ischemic stroke in the revascularization window: Clinical
examination, native head CT scan, emergency cesarean section, CT
angiography of the cerebral arteries, and, eventually, mechanical
thrombectomy, were performed. The present case report also
emphasizes the importance of evaluating inherited genetic
thrombophilia and PFO in young patients suffering a stroke, and
highlights the need for psychological and psychiatric evaluation
for possible reactive depression, anxiety and burnout in young
patients suffering a stroke, particularly in the peripartum
period.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors contributions
All authors (AIV, ADT, CN and ST) were involved in
the conceptualization of the study, as well as in the writing of
the initial draft of the manuscript, and in the writing, revising
and editing of the manuscript. AIV and CN were involved in the
curation of the patient s data. AIV and ADT were involved in
the analysis of the patient s data. AIV was involved in the
analysis of the patient s data. AIV, ADT, CN and ST were
involved in the description of the medical procedure performed for
the patient in the present case report, the series of interventions
and the series of etiological investigations performed. CN and ST
were the physicians that handled the case. AIV participated in the
therapeutic management of the patient as a resident and ADT was
involved in the writing of the manuscript as a medical student. CN
was the primary neurologist who was on the case and obtained the
consent, the medical images and was responsible for the main
medical decisions. CN and ST supervised the study and were involved
in data validation and in the critical review of the manuscript.
AIV and CN confirm the authenticity of all the raw data. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
Complete written informed consent was obtained from
the patient for her participation in the present case report.
Patient consent for publication
Complete written informed consent was obtained from
the patient for the publication of the present case report and the
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
Use of artificial intelligence tools
During the preparation of this work, artificial
intelligence tools were used to improve the readability and
language of the manuscript or to generate images, and subsequently,
the authors revised and edited the content produced by the
artificial intelligence tools as necessary, taking full
responsibility for the ultimate content of the present
manuscript.
References
|
1
|
Sousa Gomes M, Guimarães M and Montenegro
N: Thrombolysis in pregnancy: A literature review. J Matern Fetal
Neonatal Med. 32:2418–2428. 2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Dicpinigaitis AJ, Sursal T, Morse CA,
Briskin C, Dakay K, Kurian C, Kaur G, Sahni R, Bowers C, Gandhi CD,
et al: Endovascular thrombectomy for treatment of acute ischemic
stroke during pregnancy and the early postpartum period. Stroke.
52:3796–3804. 2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Leonhardt G, Gaul C, Nietsch HH, Buerke M
and Schleussner E: Thrombolytic therapy in pregnancy. J Thromb
Thrombolysis. 21:271–276. 2006.PubMed/NCBI View Article : Google Scholar
|
|
4
|
del Zoppo GJ, Levy DE, Wasiewski WW,
Pancioli AM, Demchuk AM, Trammel J, Demaerschalk BM, Kaste M,
Albers GW and Ringelstein EB: Hyperfibrinogenemia and functional
outcome from acute ischemic stroke. Stroke. 40:1687–1691.
2009.PubMed/NCBI View Article : Google Scholar
|
|
5
|
James AH, Bushnell CD, Jamison MG and
Myers ER: Incidence and risk factors for stroke in pregnancy and
the puerperium. Obstet Gynecol. 106:509–516. 2005.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Bhogal P, Aguilar M, AlMatter M, Karck U,
Bäzner H and Henkes H: Mechanical thrombectomy in pregnancy: Report
of 2 cases and review of the literature. Interv Neurol. 6:49–56.
2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Hoang JK, Wang C, Frush DP, Enterline DS,
Samei E, Toncheva G, Lowry C and Yoshizumi TT: Estimation of
radiation exposure for brain perfusion CT: Standard protocol
compared with deviations in protocol. AJR Am J Roentgenol.
201:W730–W734. 2013.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Al-Mufti F, Schirmer CM, Starke RM,
Chaudhary N, De Leacy R, Tjoumakaris SI, Haranhalli N, Abecassis
IJ, Amuluru K, Bulsara KR, et al: Thrombectomy in special
populations: Report of the society of neuroInterventional surgery
standards and guidelines committee. J Neurointerv Surg.
14:1033–1041. 2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Demchuk AM: Yes, intravenous thrombolysis
should be administered in pregnancy when other clinical and imaging
factors are favorable. Stroke. 44:864–865. 2013.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Aaron S, Shyamkumar NK, Alexander S, Babu
PS, Prabhakar AT, Moses V, Murthy TV and Alexander M: Mechanical
thrombectomy for acute ischemic stroke in pregnancy using the
penumbra system. Ann Indian Acad Neurol. 19:261–263.
2016.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Tereanu C, Minca D, Costea R, Janta D,
Grego S, Ravera L, Pezzano D and Viganò P: ExpIR-RO: A
collaborative International project for experimenting voluntary
incident reporting in the public healthcare sector in Romania. Iran
J Public Health. 40:22–31. 2011.PubMed/NCBI
|
|
12
|
Egred M, Andron M, Albouaini K, Alahmar A,
Grainger R and Morrison WL: Percutaneous closure of patent foramen
ovale and atrial septal defect: Procedure outcome and medium-term
follow-up. J Interv Cardiol. 20:395–401. 2007.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Furtunescu F, Minca DG, Vasile A and
Domnariu C: Alcohol consumption impact on premature mortality in
Romania. Rom J Leg Med. 17:296–302. 2009.
|
|
14
|
Pezzini A, Del Zotto E, Magoni M, Costa A,
Archetti S, Grassi M, Akkawi NM, Albertini A, Assanelli D, Vignolo
LA and Padovani A: Inherited thrombophilic disorders in young
adults with ischemic stroke and patent foramen ovale. Stroke.
34:28–33. 2003.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Safouris A, Kargiotis O, Psychogios K,
Kalyvas P, Ikonomidis I, Drakopoulou M, Toutouzas K and Tsivgoulis
G: A narrative and critical review of randomized-controlled
clinical trials on patent foramen ovale closure for reducing the
risk of stroke recurrence. Front Neurol. 11(434)2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Orgera MA, O Malley PG and Taylor AJ:
Secondary prevention of cerebral ischemia in patent foramen ovale:
Systematic review and meta-analysis. South Med J. 94:699–703.
2001.PubMed/NCBI
|
|
17
|
Kheiri B, Simpson TF, Osman M, Golwala H,
Radaideh Q, Dalouk K, Stecker EC, Zahr F, Nazer B and Rahmouni H:
Meta-analysis of secondary prevention of cryptogenic stroke.
Cardiovasc Revasc Med. 21:1285–1290. 2020.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Kim BJ, Sohn H, Sun BJ, Song JK, Kang DW,
Kim JS and Kwon SU: Imaging characteristics of ischemic strokes
related to patent foramen ovale. Stroke. 44:3350–3356.
2013.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Badea RŞ, Ribigan AC, Grecu N, Terecoasǎ
E, Antochi FA, Bâldea Mihǎilǎ S, Tiu C and Popescu BO: Differences
in clinical and biological factors between patients with
PFO-related stroke and patients with PFO and no cerebral vascular
events. Front Neurol. 14(1104674)2023.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Diener HC, Sacco RL, Easton JD, Granger
CB, Bar M, Bernstein RA, Brainin M, Brueckmann M, Cronin L, Donnan
G, et al: Antithrombotic treatment of embolic stroke of
undetermined source: RE-SPECT ESUS elderly and renally impaired
subgroups. Stroke. 51:1758–1765. 2020.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Diener HC, Sacco RL, Easton JD, Granger
CB, Bernstein RA, Uchiyama S, Kreuzer J, Cronin L, Cotton D, Grauer
C, et al: Dabigatran for prevention of stroke after embolic stroke
of undetermined source. N Engl J Med. 380:1906–1917.
2019.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Diener HC, Easton JD, Granger CB, Cronin
L, Duffy C, Cotton D, Brueckmann M and Sacco RL: RE-SPECT ESUS
Investigators. Design of Randomized, double-blind, evaluation in
secondary stroke prevention comparing the efficacy and safety of
the oral thrombin inhibitor dabigatran etexilate vs.
acetylsalicylic acid in patients with embolic stroke of
undetermined source (RE-SPECT ESUS). Int J Stroke. 10:1309–1312.
2015.PubMed/NCBI View Article : Google Scholar
|
|
23
|
de Bruijn MA, Synhaeve NE, van Rijsbergen
MW, de Leeuw FE, Mark RE, Jansen BP and de*Kort PL: Quality of life
after young ischemic stroke of mild severity is mainly influenced
by psychological factors. J Stroke Cerebrovasc Dis. 24:2183–2188.
2015.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Morris R: The Psychology of Stroke in
Young Adults: The roles of service provision and return to work.
Stroke Res Treat. 2011(534812)2011.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Teasell RW, McRae MP and Finestone HM:
Social issues in the rehabilitation of younger stroke patients.
Arch Phys Med Rehabil. 81:205–209. 2000.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Trifu S and Trifu AD: Receptor profiles of
atypical antipsychotic molecules. Chem Mater Sci. 82:113–128.
2020.
|
|
27
|
Moravejjifar M, Hassannia R, Esmaeili H,
Tehrani H and Vahedian*Shahroodi M: Predictors of marital burnout
in pregnant women based on social cognitive theory components. J
Midwifery Reprod Health. 9:2834–2843. 2021.
|
|
28
|
Trifu S: Neuroendocrine insights into
burnout syndrome. Acta Endocrinol (Buchar). 15:404–405.
2019.PubMed/NCBI View Article : Google Scholar
|