Introduction
The National Institute on Drug Abuse (NIDA) reports
that inhalants continue to be one of the most commonly abused
substances in the USA (1). They are
used through methods such as sniffing, huffing, or bagging and
often involve easily accessible products such as compressed air
duster cans containing hydrofluorocarbons, including
tetrafluoroethane and difluoroethane. These chemicals induce rapid
psychoactive effects via gamma-aminobutyric acid enhancement and
N-methyl-D-aspartate receptor receptor suppression; however, their
overall toxic effects are not yet fully defined (2). Compressed air duster cans are widely
available inhalants composed of liquefied hydrofluorocarbon
propellants, most commonly difluoroethane. These products are
intended for cleaning electronic equipment, but can produce
significant toxicity when misused. Safety data for these agents
warn that concentrated inhalation may lead to respiratory
irritation, altered mental status, cardiac conduction
abnormalities, arrhythmias, impaired circulation, loss of
consciousness and even sudden death. High-level exposure has also
been shown to be associated with renal dysfunction and other
systemic complications (3,4). Although the majority of reported cases
involve individuals aged between 18 and 50 years, the 2019 National
Youth Risk Behavior Survey noted that ~6.5% of younger students had
engaged in the use of inhalants, highlighting early-age
vulnerability (5).
The present study describe the case of a young male
patient with severe multi-organ toxicity (cardiac, renal and
skeletal) following chronic compressed air duster use, who
exhibited significant improvement with supportive care and was
ultimately discharged. The present case report underscores the need
for clinicians to recognize the varied presentations of duster
abuse to ensure timely diagnosis and appropriate acute
management.
Case report
A 29-year-old Caucasian male with a history of
chronic alcohol use disorder, daily tetrahydrocannabinol use,
asthma, hypertension and psychiatric comorbidities presented to the
Emergency Department of Wellstar Spalding Regional Hospital
(Griffin, USA) May 12, 2025 following a syncopal episode. He
described several days of progressive weakness, dizziness and joint
pain requiring cane-assisted ambulation. On the day of admission,
he collapsed while descending stairs. This event was witnessed, and
there was no evidence of seizure activity or post-ictal confusion.
He admitted to the extensive daily use of compressed air duster
cans for several months, experiencing euphoria and increasing
nausea with each use. On the day of presentation, he had used 8
cans of dust inhalant, instead of 4 as per his routine use.
Upon arrival, he was hypotensive and symptomatic. An
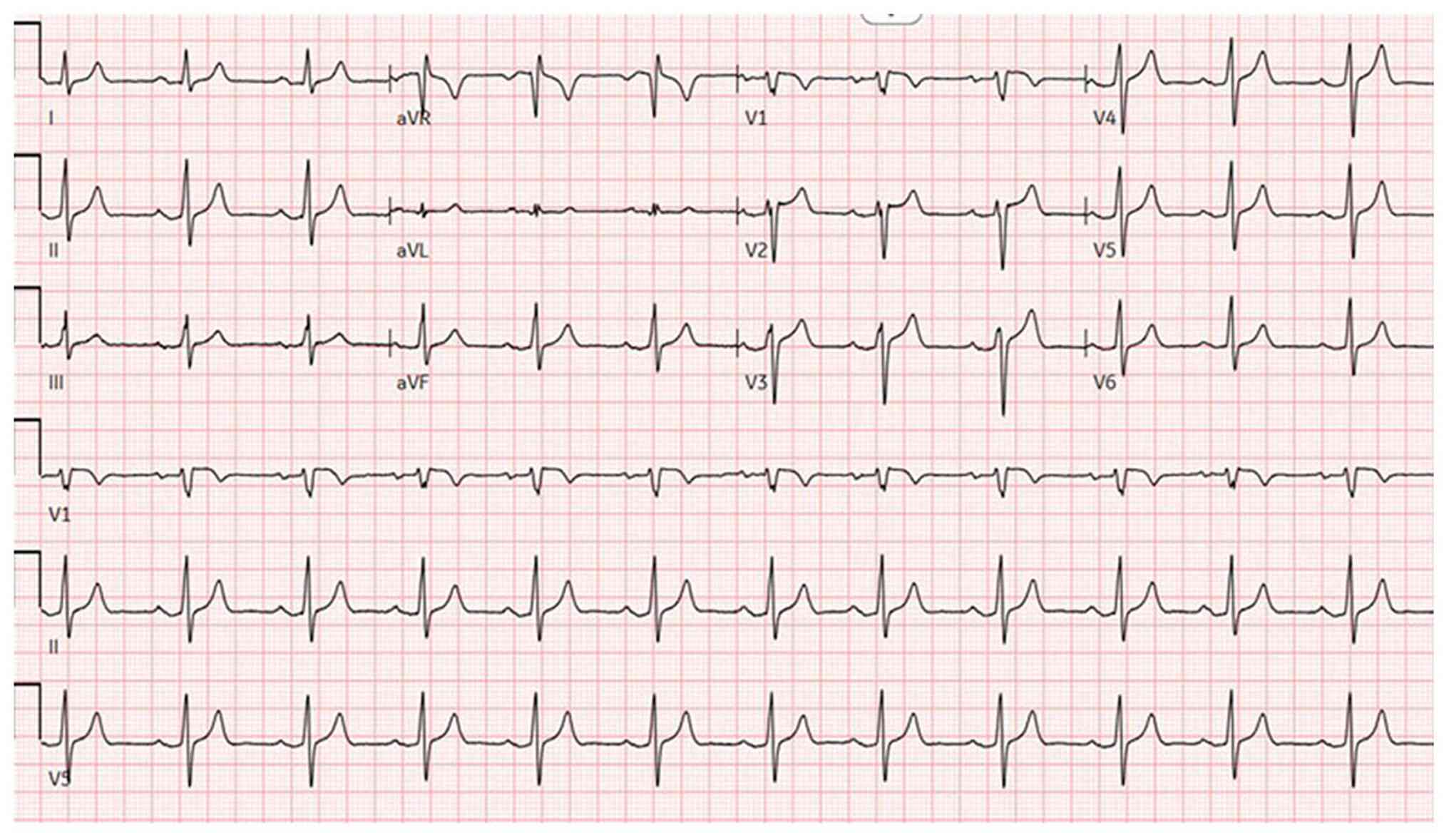
electrocardiogram (Fig. 1)
demonstrated sinus rhythm with peaked T waves. Laboratory results
revealed hyperkalemia, elevated levels of troponins (in thousands;
ng/l), acute kidney injury and high anion gap metabolic acidosis.
Urine drug screening yielded negative results, while salicylate and
acetaminophen levels were normal. Other laboratory results are
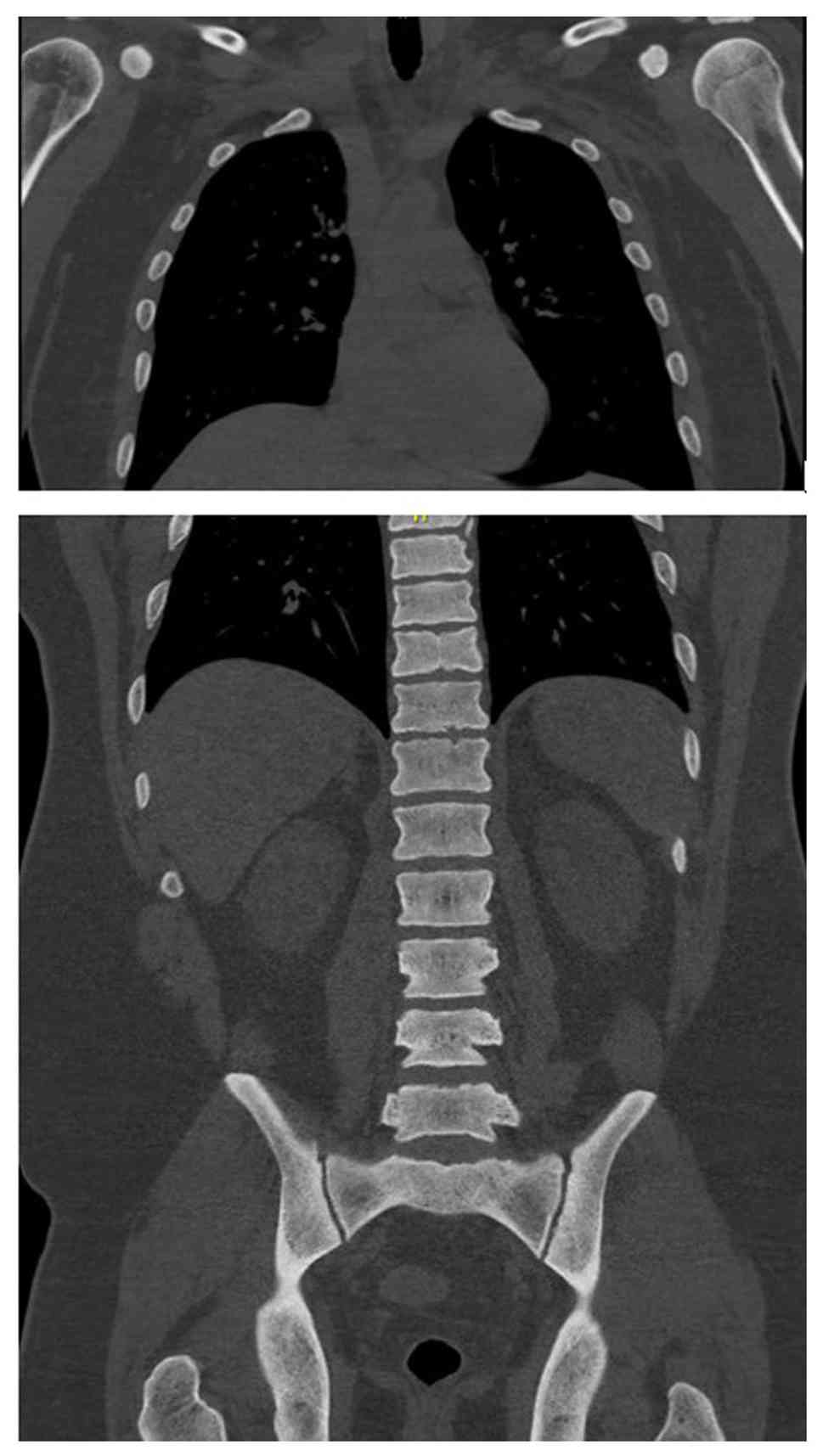
listed in Table I. Imaging analyses,
including a computed tomography scan of the cervical spine
(Fig. 2), and chest, abdomen and
pelvis (Fig. 3), revealed diffuse
bony sclerosis.
 | Table ILaboratory values of the patient upon
admission. |
Table I
Laboratory values of the patient upon
admission.
| Laboratory test | Patient value | SI unit | Reference range |
|---|
| Sodium (Na) | 129.0 | mmol/l | 135-145 mmol/l |
| Chloride (Cl) | 102.0 | mmol/l | 98-106 mmol/l |
| Potassium (K) | 7.3 | mmol/l | 3.5-5.1 mmol/l |
| Bicarbonate
(HCO3) | 14.0 | mmol/l | 22-28 mmol/l |
| Phosphorus
(PO4) | 1.1 | mg/dl | 2.5-4.5 mg/dl |
| Calcium | 10.1 | mg/dl | 8.4-10.2 mg/dl |
| BUN | 45.0 | mg/dl | 7-20 mg/dl |
| Creatinine | 2.49 | mg/dl | 0.6-1.3 mg/dl |
| Anion gap | 20.0 | mmol/l | 8-16 mmol/l |
| Creatine kinase
(CK) | 361.0 | U/l | 38-174 U/l |
| Troponin | 1062.0 | ng/l | <14 ng/l |
| Pro-BNP | 416.0 | pg/ml | <125 pg/ml |
| Alkaline phosphatase
(ALP | 292.0 | U/l | 44-147 U/l |
| ALP bone
fraction | 96.0 | U/l | 28-66 U/l |
| ALP intestinal
fraction | 0.0 | U/l | 1-24 U/l |
| ALP liver
fraction | 14.0 | U/l | 25-69 U/l |
| Haptoglobin | 770.0 | mg/dl | 30-200 mg/dl |
| Lactic acid | 1.0 | mmol/l | 0.5-2.2 mmol/l |
| Vitamin D | 39.0 | ng/ml | 30-100 ng/ml |
| Hemoglobin | 12 | g/dl | 13.5-17.5 g/dl |
| Ferritin | 1255.0 | ng/ml | 20-500 ng/ml |
| Iron | 66.0 | µg/dl | 60-170 µg/dl |
| MCV | 95.0 | fl | 80-100 fl |
| Folate | 7.3 | ng/ml | 3.1-17.5 ng/ml |
| Vitamin B12 | 655.0 | pg/ml | 200-900 pg/ml |
| Platelets | 550.0 |
x103/µl |
150-400x03/µl |
| ESR | 90.0 | mm/h | 0-20 mm/h |
| INR | 1.38 | | 0.8-1.2 |
| TSH | 1.01 | µIU/ml | 0.4-4.0 µIU/ml |
| Cardio CRP | 8.4 | mg/l | <3.0 mg/l |
| Complement C3 | 200.0 | mg/dl | 90-180 |
| Complement C4 | 37.0 | mg/dl | 10-40 |
| PSA | 0.2 | ng/ml | 0-4.0 |
| PTH | 25 | pg/ml | 10-65 |
| ANA | Negative | | Negative |
| ANCA | Negative | | Negative |
| Hepatitis panel | Negative | | Negative |
| HIV | Negative | | Negative |
| UPCR | 1,269 High | | 22-128 mg/g |
| UA microscopy | 1+ blood, 2+
protein | | None |
| SPEP/UPEP with
immunofixation | No paraprotein
detected | | No paraprotein
detected |
| Serum free light
chains | Not detected | | Not detected |
| Urine drug
screen | Not detected | | Not detected |
| Serum
salicylate/acetaminophen | Not detected | | Not detected |
He was managed with intravenous fluids, a heparin
drip 10 units/kg/h for 24 h; aspirin at 325 mg, one dose;
atorvastatin at 80 mg for 2 days; a hyperkalemia protocol including
10 ml of 10% calcium gluconate, 1 dose and 10 mg nebulized
albuterol, one dose; and sodium bicarbonate infusion at 100 ml/h
for 1 day. Cardiology attributed the troponin elevation to
non-thrombotic myocardial injury (type 2 MI) rather than acute
plaque rupture, given the clinical context and normal ventricular
function on an echocardiogram. Therefore, the heparin drip was
discontinued after 24 h. The patient was monitored on telemetry and
had no arrhythmias.
Nephrology and Hematology-Oncology were consulted to
investigate potential underlying etiologies for his acute kidney
injury and diffuse skeletal sclerosis. A comprehensive differential
diagnosis was considered and methodically ruled out. Multiple
myeloma was excluded with negative serum and urine
protein-to-creatinine ratio (UPCR) and immunofixation analyses.
Renal osteodystrophy was deemed unlikely due to preserved renal
function on follow-up and lack of secondary hyperparathyroidism.
Glomerulonephritis and vasculitis were excluded via negative
serologic and urinary studies. No evidence of paraneoplastic
syndrome or infiltrative bone marrow disorder was found, and
vitamin D deficiency and prostate-specific antigen levels were
within normal range. Imaging and laboratory trends supported a
toxic-metabolic etiology, most likely secondary to chronic inhalant
exposure. The patient improved with supportive therapy, with
laboratory values returning to levels within normal limits; he was
discharged after 3 days with referrals to nephrology,
hematology-oncology and addiction medicine.
Discussion
1,1-Difluoroethane, a hydrofluorocarbon propellant
found in a number of compressed-gas cleaning products, is
frequently misused for its rapid onset of central nervous system
depression and transient euphoria. Owing to its high lipid
solubility, the compound readily crosses the blood-brain barrier,
producing effects that last only a few minutes. Its easy
availability, low cost and short-lived intoxication render
difluoroethane-containing compressed air duster cans particularly
attractive for recurrent recreational use (6). The patient described herein reported
inhaling approximately four cans daily for several months and
doubled this amount to eight cans on the day of presentation,
highlighting both tolerance and escalating exposure patterns
typical of chronic inhalant misuse.
Reported neurologic manifestations of difluoroethane
and other inhalant exposure range from mild to severe and may
include drowsiness, headaches, gait instability, dizziness, visual
disturbances, generalized weakness, profound fatigue, lethargy,
altered consciousness, seizures and even coma. Hypoxia resulting
from oxygen displacement within the alveoli or aspiration-related
lung injury can further exacerbate central nervous system
depression. Chronic users may also experience lasting effects, such
as cognitive deficits, cerebellar dysfunction and peripheral
neuropathy (7). In the case
described herein, the inhalant use of the patient culminated in a
syncopal episode, consistent with the acute neurologic and systemic
instability described in the literature (4).
Marked cardiovascular complications from hydrocarbon
inhalation include myocardial dysfunction and life-threatening
arrhythmias. Halogenated hydrocarbons, in particular, have been
shown to be associated with fatal ventricular dysrhythmias and the
phenomenon of ‘sudden sniffing death’, an unpredictable event
reported even in first-time users. This is deemed to result from
increased myocardial sensitivity to catecholamines, compounded by
inhalant-induced hypoxia, which promotes delayed
after-depolarizations and malignant ventricular arrhythmias
(8-12).
In the patient in the present study, inhalant use was accompanied
by severe hyperkalemia with corresponding electrocardiogram
changes, syncope and markedly elevated troponin levels in the
thousands, although echocardiography demonstrated preserved
systolic function without structural abnormalities.
Cao et al (3)
reported the case of a 35-year-old chronic duster user who
developed ischemic-appearing electrocardiogram changes and elevated
troponin, ultimately found to have non-obstructive coronaries on
catheterization, consistent with inhalant-related cardiac injury.
Similarly, the patient in the present study exhibited
electrocardiogram abnormalities most notably peaked T waves along
with syncope and significant troponin elevation. Similarly, in the
patient described herein, the increase in troponin levels was
ultimately deemed type 2 MI (supply-demand mismatch) or toxic
myocardial injury, rather than a classic type 1 infarction. As the
clinical suspicion for true coronary disease was low and
echocardiography was normal, cardiac catheterization was deferred.
The Fourth Universal Definition of myocardial infarction (13) emphasizes that troponin elevation
without evidence of acute atherothrombosis should be classified as
myocardial injury or type 2 MI (due to this, his heparin was
terminated and angiography was deferred). Hydrocarbon toxicity can
also cause myocarditis; cardiac MRI in such cases presents as
inflammation; however, in the patient in the present study, the
echo was normal and he had no focal wall motion abnormalities. In
summary, the clinical picture favors a toxic myocardium from
inhalants (type 2 MI) over an acute plaque rupture infarct
(13). Long et al (14) previously described one of the
earliest reported cases of acute renal failure associated with
duster inhalation. Similar to that report, the patient described
herein also presented with acute kidney injury, which improved
significantly with intravenous fluid resuscitation. Although
dehydration likely contributed to his renal dysfunction, a direct
nephrotoxic effect of difluoroethane cannot be fully excluded.
Inhalant-related skeletal fluorosis can produce
diffuse osteosclerosis, trabecular coarsening, cortical thickening
and soft-tissue ossifications, with imaging serving as the most
sensitive diagnostic tool. As fluoride accumulates in bone with a
long half-life, radiographic changes may persist for years even
after exposure stops (15). In the
patient in the present study, extensive osteosclerosis was evident
despite his young age, consistent with chronic hydrofluorocarbon
exposure, although a DEXA scan was not obtained. However, in the
present study, serum or urine fluoride levels were not measured to
confirm fluorosis; thus, this is a limitation of the present study.
Without fluoride quantification, a definitive diagnosis of skeletal
fluorosis cannot be made. Instead, toxic-metabolic bone disease
from inhalant exposure was considered more likely. The differential
diagnosis for diffuse osteosclerosis is limited, but includes
osteoblastic metastases (e.g., prostate and breast), sclerotic
myeloma, myelofibrosis, mastocytosis, Paget's disease and rare
granulomatous disorders, such as sarcoidosis. In the case described
herein, malignancy and myeloma were investigated and excluded, and
there was no evidence of systemic diseases (such as sarcoidosis)
that may cause similar bone changes.
In conclusion, the present study describes the case
of a 29-year-old male patient who developed syncope after inhaling
multiple compressed air duster cans, presenting with acute cardiac
injury, renal dysfunction and diffuse skeletal sclerosis. His
findings parallel prior reports of multisystem toxicity from
hydrofluorocarbon inhalation (3,5,6,14,15).
Although the current evaluation was limited by the absence of
cardiac catheterization and DEXA imaging, the clinical picture
strongly supports inhalant-induced organ injury. Clinicians should
consider duster abuse in young patients with unexplained syncope,
electrocardiogram abnormalities, or multiorgan dysfunction. Ongoing
research is required in order to better define the pathophysiology
and long-term effects of these increasingly common exposures.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
PA identified and managed the case, collected
clinical data, performed the literature review, and drafted the
manuscript. SI and MA assisted with the literature review, were
involved in the conception of the study, and assisted in preparing
the figures/table. NN assisted with the literature review and was
involved in the design of the study. SM and MS critically revised
the manuscript for important intellectual content and were also
involved in the design of the study. All authors have read and
approved the final manuscript. PA and MS confirm the authenticity
of all the raw data.
Ethics approval and consent to
participate
Written informed consent for participation was
obtained from the patient.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the present case report and any
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
NIDA. Inhalants. National Institute on
Drug Abuse website. Available from: https://nida.nih.gov/research-topics/inhalants.
Accessed January 10, 2026.
|
|
2
|
Levari E, Stefani M, Ferrucci R, Negri A
and Corazza O: The dangerous use of inhalants among teens: A case
report. Emerg Trends Drugs Addict Health. 1(100006)2021.
|
|
3
|
Cao SA, Ray M and Klebanov N: Air duster
inhalant abuse causing non-ST elevation myocardial infarction.
Cureus. 12(e8402)2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Romero J, Abboud R, Elkattawy S, Romero A,
Elkattawy O, Samak AAA and Shamoon R: Troponemia secondary to air
duster inhalant abuse. Eur J Case Rep Intern Med.
9(003556)2022.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Centers for Disease Control and
Prevention. High School Youth Risk Behavior Surveillance - United
States 2019. Available from: https://www.cdc.gov/yrbs/index.html. Accessed October
8, 2026.
|
|
6
|
Mohideen H, Dahiya DS, Parsons D, Hussain
H and Ahmed RS: Skeletal fluorosis: A case of inhalant abuse
leading to a diagnosis of colon cancer. J Investig Med High Impact
Case Rep: Mar 28, 2022 (Epub ahead of print).
|
|
7
|
Hoody L, Cronin M and Balasanova AA: A
case of multisystem organ failure in a patient with inhalant use
disorder. Prim Care Companion CNS Disord.
25(22cr03349)2023.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tormoehlen LM, Tekulve KJ and Nañagas KA:
Hydrocarbon toxicity: A review. Clin Toxicol (Phila). 52:479–489.
2014.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Adgey AA, Johnston PW and McMechan S:
Sudden cardiac death and substance abuse. Resuscitation.
29:219–221. 1995.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Shepherd RT: Mechanism of sudden death
associated with volatile substance abuse. Hum Toxicol. 8:287–291.
1989.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Nelson LS: Toxicologic myocardial
sensitization. J Toxicol Clin Toxicol. 40:867–879. 2002.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Mullin LS, Azar A, Reinhardt CF, Smith PE
Jr and Fabryka EF: Halogenated hydrocarbon-induced cardiac
arrhythmias associated with release of endogenous epinephrine. Am
Ind Hyg Assoc J. 33:389–396. 1972.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Thygesen K, Alpert JS, Jaffe AS, Chaitman
BR, Bax JJ, Morrow DA and White HD: ESC Scientific Document Group.
Fourth universal definition of myocardial infarction (2018). Eur
Heart J. 40:237–269. 2019.
|
|
14
|
Long D, Zhu D and Arnouk S: A case of
Ultra Duster intoxication causing acute renal failure. Chest.
144(290A)2013.
|
|
15
|
Suwak P, Van Dyke JC, Robin KJ, Leonovicz
OG and Cable MG: Rare case of diffuse skeletal fluorosis due to
inhalant abuse of difluoroethane. J Am Acad Orthop Surg Glob Res
Rev: Oct 12, 2021 (Epub ahead of print).
|