Introduction
Hypercholesterolemia is one of the major risk
factors for the induction and progression of ischemic heart
disease. Findings of previous studies have demonstrated that
hypercholesterolemia or hyperlipidemia accelerated the progression
of myocardial ischemic reperfusion injury, delayed the myocardial
recovery on reperfusion and deteriorated the cardioprotective
effects of preconditioning and postconditioning (1,2).
Although a number of drugs have been shown to be effective in
preventing myocardial ischemic reperfusion injury, few are capable
of preserving cardioprotection in the presence of
hypercholesterolemia (3).
Rho-kinase activity is involved in diverse
cardiovascular diseases and regulation of Rho-kinase signaling is
important for cellular function, including contraction, death,
proliferation and apoptosis (4,5). A
previous study showed that Rho-kinase is activated in ischemic
myocardium and the inhibition of Rho-kinase activity is a novel
target for preventing myocardial ischemia reperfusion injury
(6). Fasudil, a Rho-kinase
inhibitor, not only has beneficial effects in ischemic heart
disease (7), but induces
preconditioning and postconditioning against myocardial ischemia
reperfusion injury in normal rat (8,9).
However, whether fasudil is capable of inducing preconditioning and
postconditioning in the hypercholesterolemic rat remains unknown.
Therefore, this issue was examined in the initial phase of the
study using an isolated rat model.
Inhibiting Rho-kinase may lead to activation of the
phosphoinositol 3-kinase (PI3K)/Akt/endothelial nitric oxide
synthase (eNOS) signal transduction pathway (10). Rho-kinase acts as a negative
regulator of PI3K activation and modulates the protective effect
via the PI3K/Akt/eNOS pathway on myocardial preconditioning and
postconditioning (11). In
addition, fasudil-induced preconditioning and postconditioning is
mediated by mitochondrial KATP (m-KATP) channels in the normal rat
(9,12). Therefore, in the second phase of
the study, fasudil was tested to determine whether it is capable of
inducing preconditioning and postconditioning in the
hypercholesterolemic rat and if it is involved in upregulating the
PI3K/Akt/eNOS pathway and inducing the opening of the m-KATP
channel.
Therefore, the present study was performed to
clarify whether fasudil induces preconditioning and
postconditioning in the hypercholesterolemic rat and if so, whether
the cardioprotective effects are mediated by regulation of the
PI3K/Akt/eNOS pathway and m-KATP channel.
Materials and methods
Animals
A total of 90 male Wistar rats purchased from the
Center of Experimental Animals (China Medical University), weighing
200±10 g were used in this study. The animals used were treated in
accordance with the Guide for the Care and Use of Laboratory
Animals, published by the National Institutes of Health (NIH). The
study instructions were approved by the Institutional Ethics
Committee.
Drugs
Fasudil was purchased from Chase Sun Pharmaceutical
Co., Ltd. (Tianjin, China). 5-Hydroxydecanoic acid (5HD), an m-KATP
channel blocker and 2,3,5-triphenyltetrazolium chloride (TTC) were
purchased from Sigma-Aldrich (St. Louis, MO, USA).
Induction of experimental
hypercholesterolemia
Prior to beginning an 8-week feeding period, blood
samples were collected from the rat's caudal vein for determination
of plasma levels of total cholesterol (TC), high-density
lipoprotein (HDL) and low-density lipoprotein (LDL) using
commercial kits [Total Cholesterol Assay kit-Fluoro Cholesterol
(Cell Technology Inc., Mountain View, CA, USA), Cholesterol LDL
direct and Cholesterol HDL direct (both Biosystems S.A., Costa
Brava, Barcelona, Spain)]. Animals were fed with diet enriched with
1.5% cholesterol, 5% egg yolk powder, 10% lard, 0.5% sodium
cholate, 3% sugar and 80% normal feedstuff for 8 weeks and this
formula was modified as previously reported (13). Following the 8-week feeding period,
blood samples were collected from the rat's caudal vein again for
determination of serum lipid to determine the success of
hypercholesterolemic models.
Heart preparation
Rats were anesthetized with an intraperitoneal
injection of pentobarbital sodium (100 mg/kg). Heparin (1,500
IU/kg) was administered intravenously to prevent intracoronary clot
formation. The heart was rapidly excised and immediately immersed
in ice-cold heparinized modified Krebs-Henseleit (K-H) buffer
containing:127 mM NaCl, 17.7 mM NaHCO3, 5.1 mM KCl, 1.5
mM CaCl2, 1.26 mM MgCl2 and 11 mM D-glucose
(pH 7.4). The heart was mounted on a Langendorff perfusion
apparatus and retrogradely perfused through the aorta with
recirculating buffer saturated with 95% O2 and 5%
CO2 at 37°C. The heart was maintained in a thermostatic
chamber at 37°C. Perfusion was maintained at a constant pressure of
75 mmHg. A fluid-filled latex balloon was inserted in the left
ventricle (LV) via the left atrium for pressure measurement. The
balloon was connected to a pressure transducer and inflated to an
initial LV end-diastolic pressure between 8 and 10 mmHg.
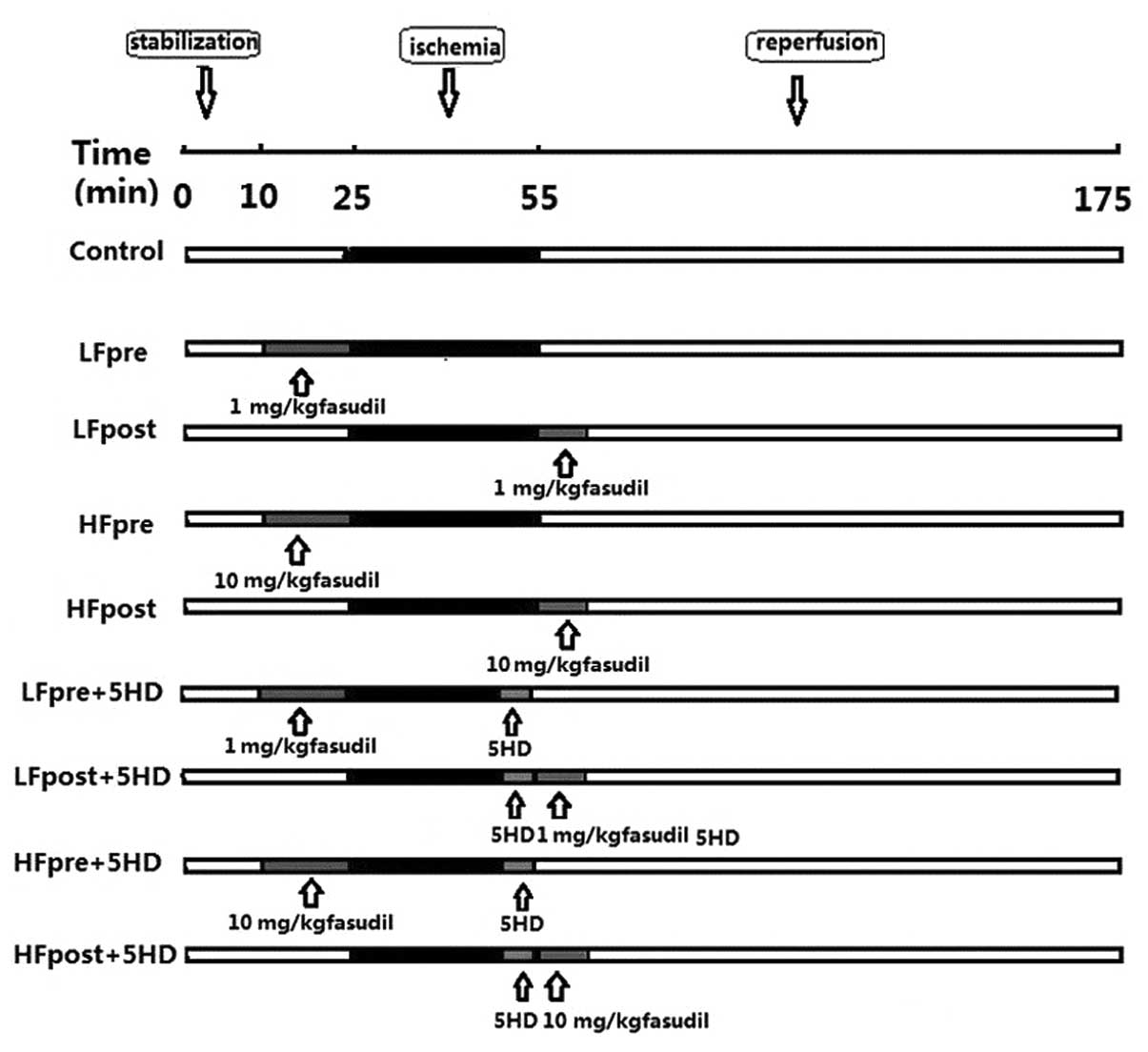
Experimental instructions
Rats were divided into 9 groups with 10
animals/group (Fig. 1). In all the
groups, the isolated rat hearts were perfused with K-H solution
(127 mM NaCl, 17.7 mM NaHCO3, 5.1 mM KCl, 1.5 mM
CaCl2, 1.26 mM MgCl2 and 11 mM D-glucose,
pH=7.4) and allowed 10 min stabilization. Isolated rat hearts were
then subjected to 30 min global ischemia and 120 min
reperfusion.
Isolated rat hearts for the control group were
subjected to 30 min global ischemia and 120 min reperfusion. In the
low-dose fasudil preconditioning group (LFpre), the isolated rat
hearts were perfused with K-H solution containing 1 mg/kg dose
fasudil 15 min prior to ischemia. In the LF postconditioning group
(LFpost), the isolated rat hearts were perfused with K-H solution
containing 1 mg/kg dose fasudil at the onset of reperfusion. In the
high-dose fasudil preconditioning group (HFpre), the isolated rat
hearts were perfused with K-H solution containing 10 mg/kg dose
fasudil 15 min prior to ischemia. In the HF postconditioning group
(HFpost), the isolated rat hearts were perfused with K-H solution
containing 10 mg/kg dose fasudil at the onset of reperfusion. In
the LFpre + 5HD group (LFpre + 5HD), the isolated rat hearts
received fasudil as described above and were administered K-H
solution containing 10 mg/kg dose 5HD at 5 min prior to
reperfusion. In the LFpost + 5HD group (LFpost + 5HD), the isolated
rat hearts received fasudil and 5HD as described above. In the
HFpre + 5HD group (HFpre + 5HD), the isolated rat hearts received
fasudil and 5HD as described above. In the HFpost + 5HD group
(HFpost + 5HD), the isolated rat hearts received fasudil and 5HD as
described above.
Hemodynamic monitoring
The hemodynamic assessment included heart rate (HR),
left ventricular developed pressure (LVDP), positive first order
derivative of ventricular pressure (+dp/dt) and negative first
order derivative of ventricular pressure (−dp/dt). These parameters
were continuously monitored throughout the experiment. The HR,
LVDP, +dp/dt and −dp/dt were sampled and digitally processed via a
hemodynamic system (MP150; Biopac Systems, Inc., Goleta, CA,
USA).
Assessment of myocardial injury
To determine the extent of myocardial injury, the
release of creatine kinase-MB (CK-MB) and lactate dehydrogenase
(LDH) in coronary effluents were measured using commercially
available kits [Rat Creatine Kinase MB Isoenzyme (CK-MB) ELISA kit
and rat LDH ELISA kit (both Bioss, Woburn, MA, USA)]. Values are
expressed in international units (IU) per liter.
Measurement of infarct size
Infarct size was determined as previously described
(14). Briefly, after 2 h
reperfusion, the hearts were harvested and the left ventricles were
sectioned from apex to base into 2–3-mm sections, following
incubation for 20 min at 37°C in 1% TTC and unstained tissue was
carefully separated from stained tissue by an independent observer.
The unstained tissue represented the dead cells and the stained
tissue represented the viable cells. The unstained mass was
expressed as a percentage of total left ventricular mass. The total
left ventricle mass also corresponds to the risk area since global
ischemia was induced.
Western blotting
Following 30 min reperfusion, left ventricles were
homogenized in a lysis buffer: 10 mM Tris-HCl, 20 mM
orthophosphate, 1 mM EGTA, 1 mM EDTA, 2 mM
Na3VO4 and 1 mM phenylmethylsulfonyl fluoride
(pH 7.4). Following sonication, the lysates were centrifuged,
proteins were separated by electrophoresis on SDS-PAGE and
transferred onto polyvinylidene difluoride-plus membrane. The
membranes were blocked with 5% milk, followed by incubation
overnight at 4°C with the following antibodies: Akt (1:500);
phospho-Akt (at Ser473, 1:500) eNOS (1:500) and phospho-eNOS (at
Ser1177, 1:500; all Santa Cruz Biotechnology, Inc., Santa Cruz, CA,
USA). Following incubation, the membranes were washed three times
with 0.1% Tween-20 for 15 min and incubated with horseradish
peroxidase (Boster, Wuhan, China) for 2 h. Levels of phosphorylated
proteins were normalized to their total protein levels. Relative
densitometry was performed using a computerized software package
(NIH Image 1.63 software; National Institutes of Health, Bethesda,
MD, USA).
Statistical analysis
The data are expressed as mean ± SD. Statistical
analysis was performed using SigmaStat software, version 3.5
(Systat Software, Inc., Chicago, IL, USA). Differences between
groups were evaluated using one-way analysis of variance (ANOVA),
followed by Student-Newman-Keuls post-hoc test. P<0.05 was
considered to indicate a statistically significant difference.
Results
Plasma lipid levels
Table I shows the
average values for TC, HDL and LDL in the plasma of animals prior
to and following an 8-week cholesterol-enriched diet. A significant
increase (P<0.05) in the average TC and LDL values was observed
in the animals fed with the cholesterol-enriched diet as compared
with the control group. There was no significant difference in the
value of HDL between the two groups (P>0.05).
 | Table IBiochemical analysis (mean ± SD, n=40
for each group). |
Table I
Biochemical analysis (mean ± SD, n=40
for each group).
| Parameters | Total cholesterol
(mg/dl) | HDL-C (mg/dl) | LDL-C (mg/dl) |
|---|
| Prior to
cholesterol-enriched diet feed | 53.7±6.1 | 44.3±4.6 | 14.7±4.3 |
| Following
cholesterol-enriched diet feed | 307.1±7.6a | 45.4±5.1 | 42.5±5.3a |
Hemodynamic changes
Table II shows the
values of HR, LVDP, +dp/dt and −dp/dt at baseline and during
specific times of reperfusion. No significant differences were
identified within or among the groups in HR, LVDP, +dp/dt and
−dp/dt at any measurement point.
 | Table IIHR, +dp/dt, −dp/dt and LVDP prior to
and during reperfusion. |
Table II
HR, +dp/dt, −dp/dt and LVDP prior to
and during reperfusion.
| Time | Baseline | R-10 | R-20 | R-60 |
|---|
| HR |
| Control | 226±23 | 150±18 | 174±19 | 160±24 |
| LFpre | 217±20 | 145±26 | 165±23 | 158±15 |
| LFpost | 225±17 | 158±22 | 178±27 | 166±22 |
| HFpre | 220±18 | 146±17 | 176±12 | 164±16 |
| HFpost | 215±16 | 143±21 | 168±15 | 165±12 |
| LFpre + 5HD | 227±21 | 141±26 | 159±23 | 149±25 |
| LFpost + 5HD | 221±22 | 139±22 | 172±22 | 166±17 |
| HFpre + 5HD | 230±18 | 136±27 | 164±22 | 148±26 |
| HFpost + 5HD | 212±26 | 140±18 | 170±15 | 155±24 |
| LVDP (mmHg) |
| Control | 86±6.4 | 34±5.4 | 38±5.1 | 34±3.2 |
| LFpre | 84±6.5 | 32±7.3 | 38±4.5 | 33±4.3 |
| LFpost | 83±6.6 | 36±7.9 | 37±6.0 | 32±3.4 |
| HFpre | 88±7.5 | 33±8.4 | 34±7.7 | 30±4.9 |
| HFpost | 84±6.9 | 34±6.7 | 39±4.2 | 34±3.4 |
| LFpre + 5HD | 86±4.4 | 34±5.4 | 35±5.1 | 32±3.8 |
| LFpost + 5HD | 85±7.3 | 32±7.7 | 37±6.5 | 31±6.3 |
| HFpre + 5HD | 89±5.6 | 35±7.2 | 36±6.6 | 40±7.4 |
| HFpost + 5HD | 87±8.5 | 31±9.4 | 34±5.4 | 36±4.9 |
| +dp/dt |
| Control | 2,322±233 | 1,589±103 | 1,622±208 | 1,362±198 |
| LFpre | 2,318±187 | 1,466±259 | 1,589±217 | 1,284±134 |
| LFpost | 2,472±274 | 1,546±202 | 1,666±244 | 1,354±143 |
| HFpre | 2,312±233 | 1,589±103 | 1,602±221 | 1,362±198 |
| HFpost | 2,298±177 | 1,466±259 | 1,589±217 | 1,284±114 |
| LFpre + 5HD | 2,402±244 | 1,536±207 | 1,566±287 | 1,454±203 |
| LFpost + 5HD | 2,231±262 | 1,489±301 | 1,684±212 | 1,335±158 |
| HFpre + 5HD | 2,331±251 | 1,519±301 | 1,584±231 | 1,315±138 |
| HFpost + 5HD | 2,330±198 | 1,476±225 | 1,601±201 | 1,378±167 |
| −dp/dt |
| Control | 1,476±222 | 1,178±178 | 1,422±117 | 1,238±156 |
| LFpre | 1,378±207 | 1,109±167 | 1,271±189 | 1,079±134 |
| LFpost | 1,408±190 | 1,189±312 | 1,308±202 | 1,136±234 |
| HFpre | 1,400±156 | 1,146±242 | 1,298±345 | 1,178±198 |
| HFpost | 1,476±222 | 1,158±168 | 1,406±177 | 1,202±176 |
| LFpre + 5HD | 1,395±137 | 1,129±187 | 1,271±189 | 1,169±144 |
| LFpost + 5HD | 1,428±180 | 1,109±232 | 1,408±206 | 1,106±153 |
| HFpre + 5HD | 1,410±176 | 1,176±232 | 1,278±275 | 1,078±208 |
| HFpost + 5HD | 1,401±165 | 1,098±198 | 1,274±237 | 1,156±159 |
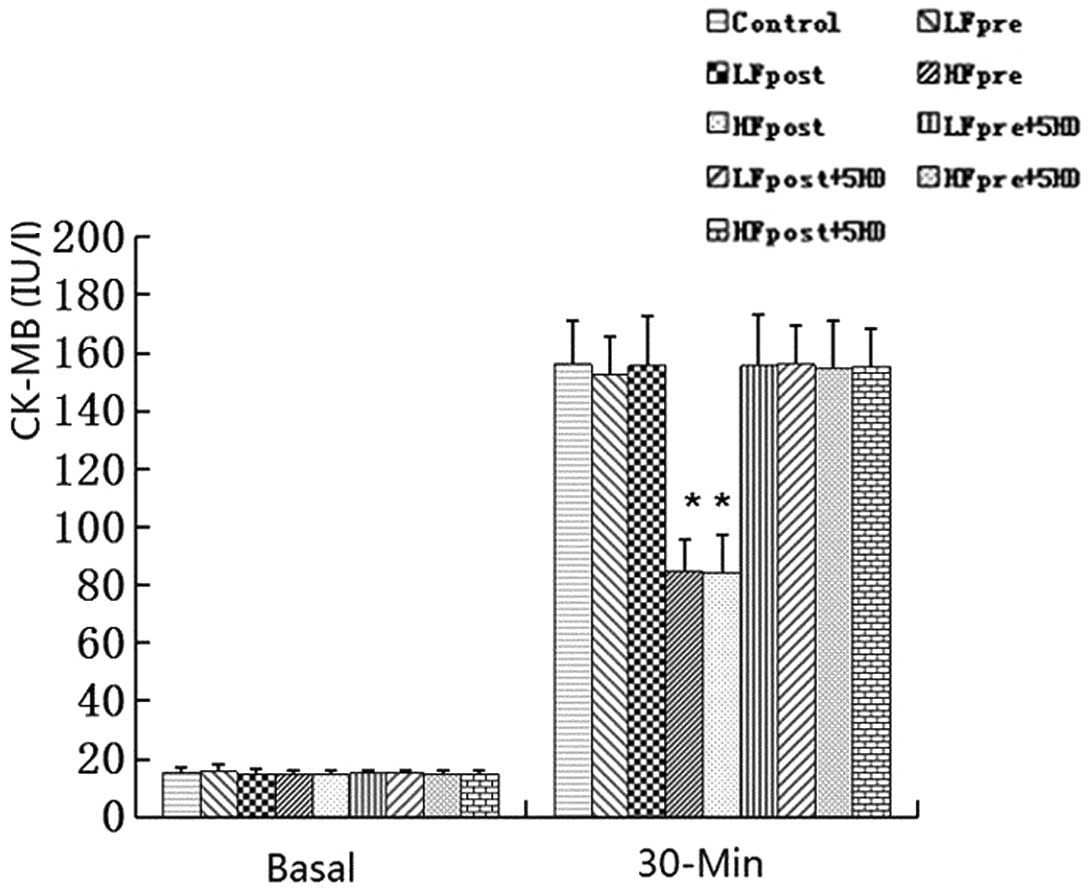
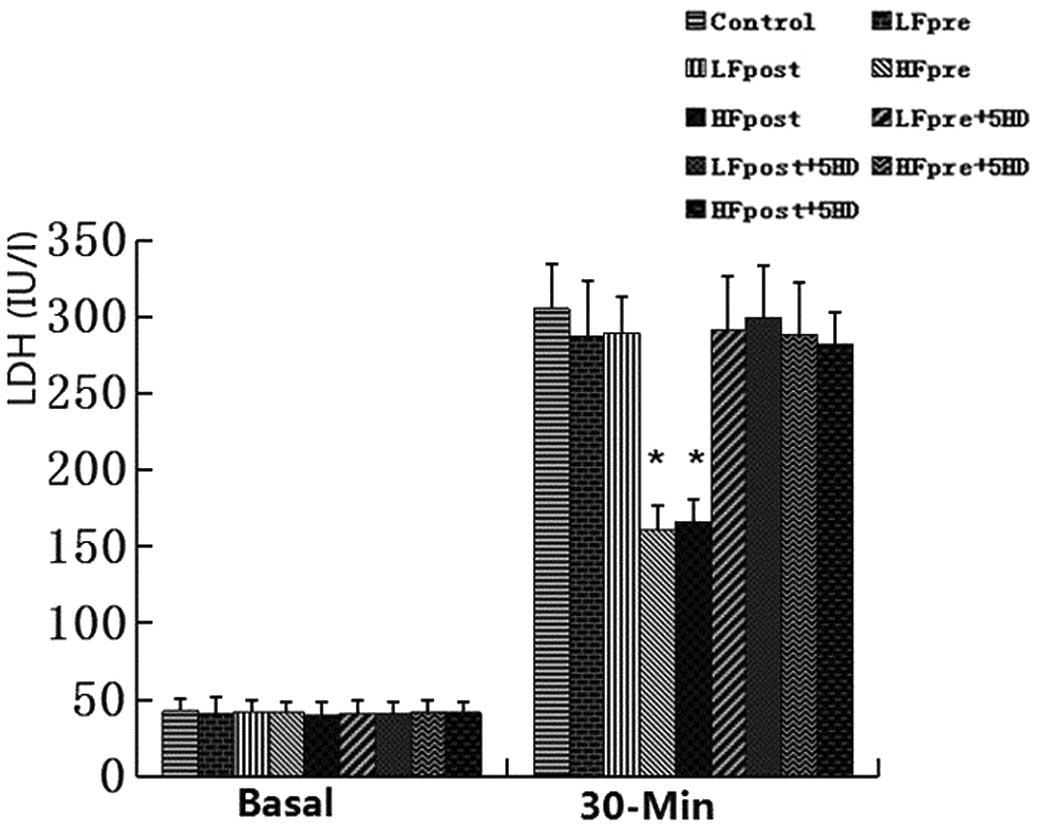
Release of CK-MB and LDH measurement
Figs. 2 and
3 show the release of CK-MB and
LDH of isolated hearts following 30 min global no-flow ischemia and
120 min reperfusion. There was no difference in the baseline values
of CK-MB and LDH among all the groups (P>0.05). HFpre and HFpost
significantly reduced the release of CK-MB and LDH in
hypercholesterolemic rat hearts as compared with the control group
(P<0.05). However, LFpre and LFpost did not decrease the release
of CK-MB and LDH in hypercholesterolemic rat hearts (P>0.05). In
addition, 5HD treatment failed to significantly attenuate the
release of CK-MB and LDH by high-dose fasudil-induced
preconditioning and postconditioning in hypercholesterolemic rat
hearts as compared with the control group (P>0.05).
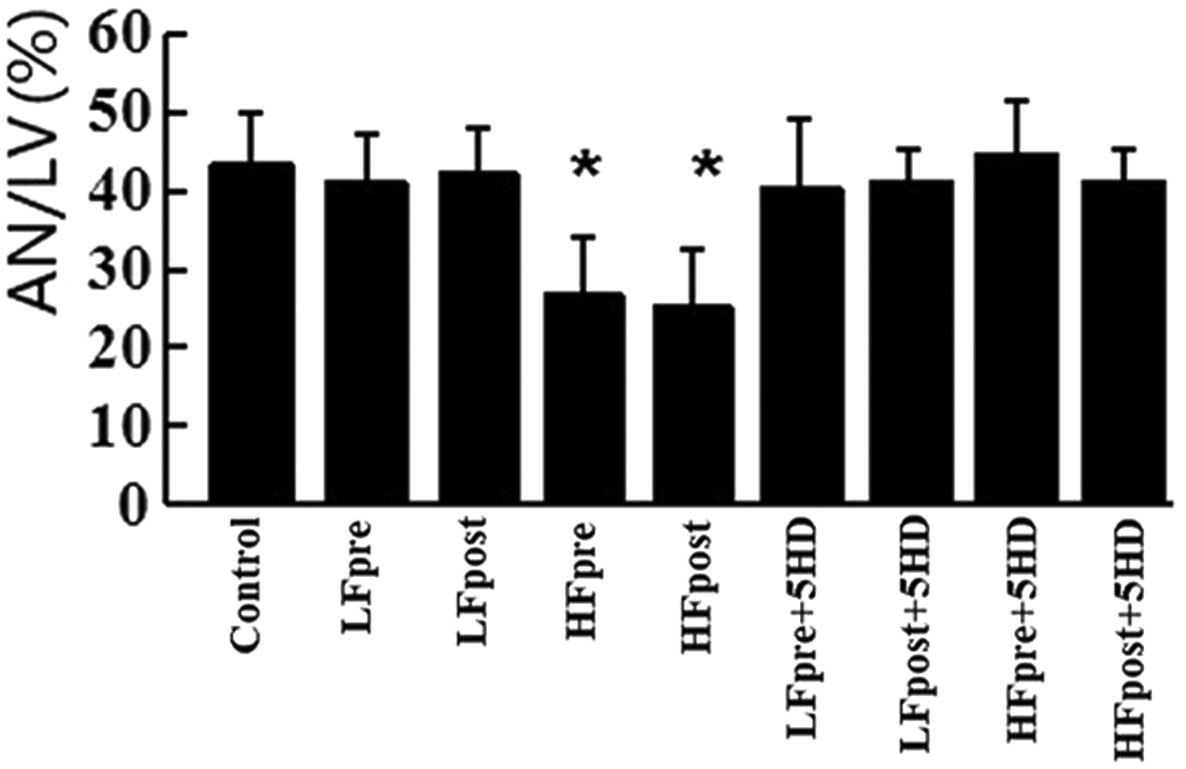
Infarct size measurement
As shown in Fig. 4,
infarct size was measured as an area of necrosis expressed as a
percentage of the left ventricular area. Infarct size was
significantly reduced by HFpre and HFpost as compared with the
control group (26.9±6.9, 25.3±7.3 vs. 43.6±6.2%; P<0.05).
However, LFpre and LFpost did not reduce infarct size as compared
with the control group (41.3±5.8, 42.3±5.6 vs. 43.6±6.2%;
P>0.05) and there was no significant difference between the
HFpre and HFpost groups (26.9±6.9 vs. 25.3±7.2%; P>0.05). In
addition, HFpre and HFpost failed to significantly reduce infarct
size when treated with 5HD as compared with the control group
(44.7±6.6, 41.1±4.3 vs. 43.6±6.2%; P>0.05).
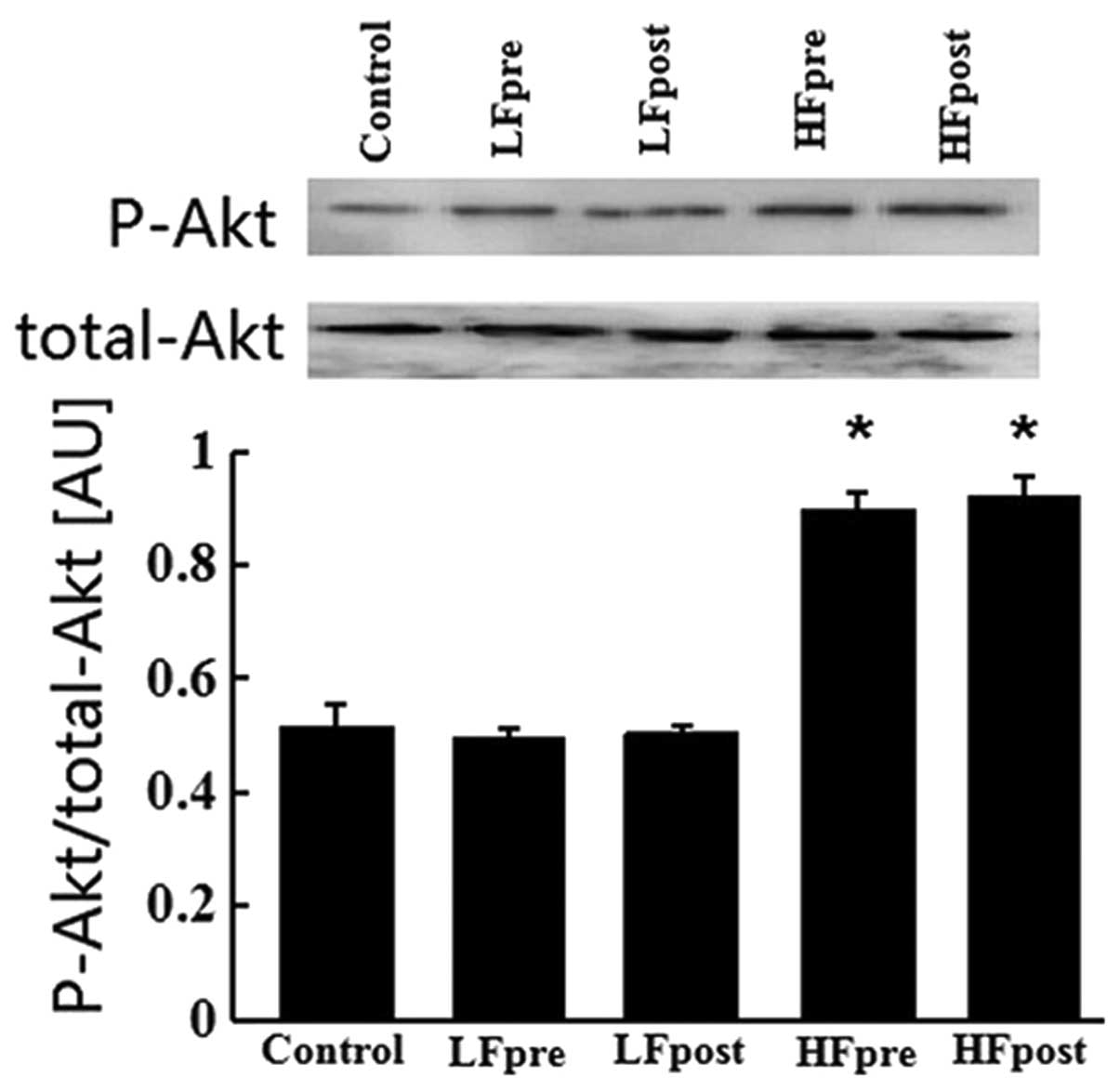
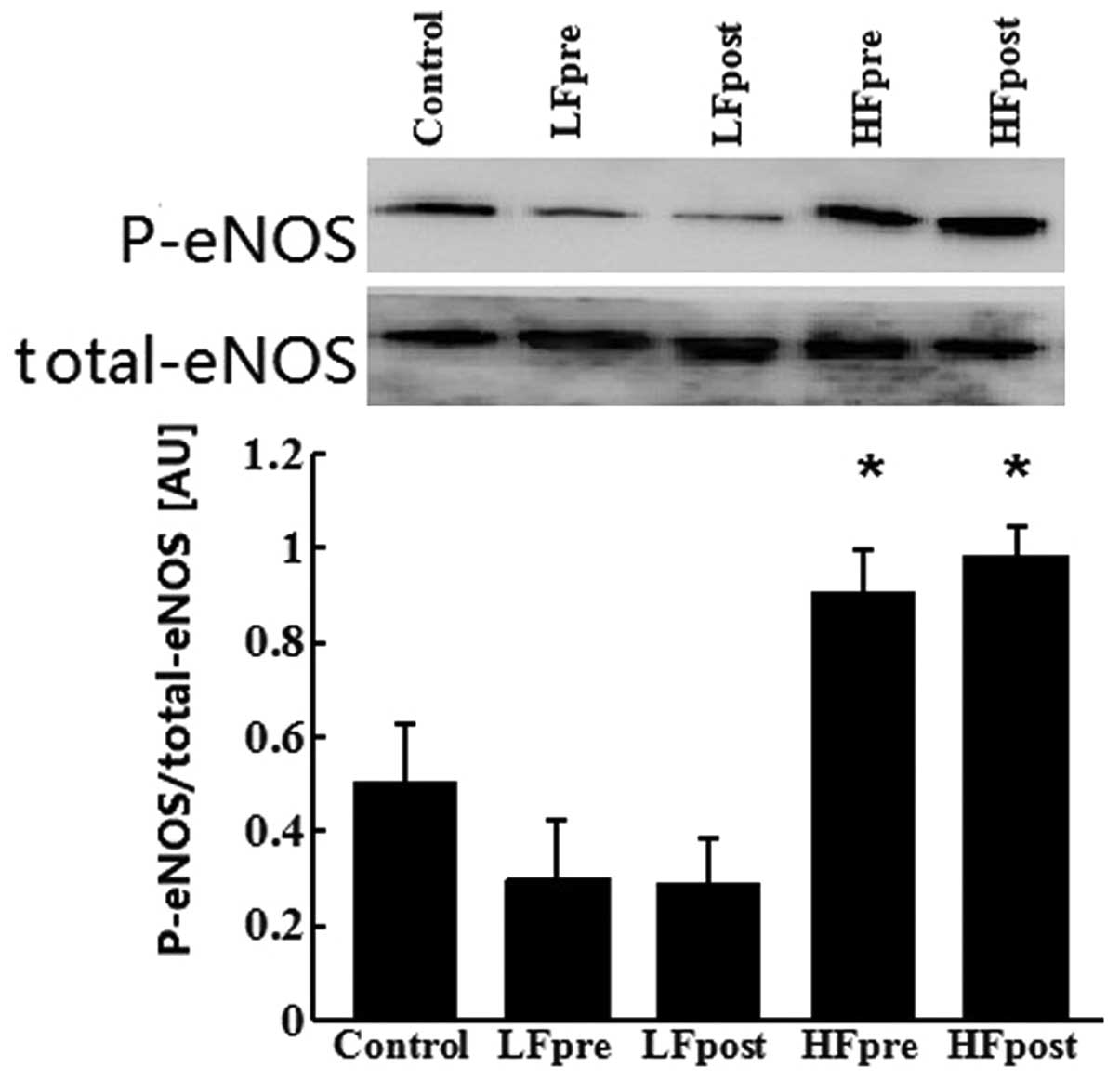
Expression of Akt and eNOS proteins
As shown in Figs. 5
and 6, Akt phosphorylation and
eNOS phosphorylation were enhanced in the HFpre and HFpost groups
as compared with the control group (0.899±0.030, 0.921±0.034 vs.
0.516±0.037; P<0.05), but no significant alteration in Akt and
eNOS phosphorylation was observed between these two groups
(0.899±0.030 vs. 0.921±0.034; P>0.05). In addition, there was no
significant change in Akt and eNOS phosphorylation in the LFpre and
LFpost groups as compared with the control group (0.497±0.013,
0.505±0.012 vs. 0.516±0.037; P>0.05).
Discussion
Previously, a number of studies have demonstrated
that fasudil induces the pharmacological preconditioning and
postconditioning in normal rat (8,9). The
present study shows that high-dose fasudil preserves
preconditioning and postconditioning against myocardial ischemia
reperfusion injury under hypercholesterolemia in rats and is
involved in upregulating the PI3K/Akt/eNOS pathway and inducing the
opening of the m-KATP channel.
Controversies remains in the literature with regard
to improvement in postischemic functional recovery of fasudil
preconditioning. Nishizawa et al (15) observed that fasudil preconditioning
did not improve recovery of the myocardium following ischemic
reperfusion and even prevented KATP channel-induced improvement in
postischemic functional recovery. By contrast, Demiryürek et
al (8) showed that fasudil, at
1 and 10 mg/kg doses, caused significant decreases in the mean
arterial blood pressure. However, no significant change in mean
arterial blood pressure was observed with fasudil at 0.3 mg/kg dose
(8). In the current study, fasudil
preconditioning at 1 or 10 mg/kg doses was observed to improve the
functional recovery of the myocardium following ischemic
reperfusion in hypercholesterolemic rats. In addition, fasudil
postconditioning at 1 and 10 mg/kg doses did not improve cardiac
function recovery in the presence of hypercholesterolemia. A
similar result was reported by Ichinomiya et al (9), which showed that 0.15 and 0.5 mg/kg
doses of fasudil postconditioning did not improve cardiac function
recovery under hyperglycemia, as well as normoglycemia.
Although fasudil induces the pharmacological
preconditioning and postconditioning in the normal rat, whether
fasudil is capable of inducing preconditioning and postconditioning
in hypercholesterolemic rat remains unknown. The present study
showed that high-dose fasudil preconditioning and postconditioning
markedly decreased myocardial infarct size and reduced the release
of CK-MB and LDH in hypercholesterolemic rat hearts as compared
with the control group. However, low-dose fasudil preconditioning
and postconditioning failed to decrease myocardial infarct size and
reduced the release of CK-MB and LDH as compared with the control
group. It is hypothesized that hypercholesterolemia blocked
low-dose fasudil-induced preconditioning, while postconditioning
and high-dose fasudil restores the cardioprotection. Ma et
al (16,17) reported that hypercholesterolemia
induced by a cholesterol-rich diet may increase the myocardial
Rho-kinase activity, thus, hypercholesterolemia was hypothesized to
increase the myocardial Rho-kinase activity during
ischemia-reperfusion and raise the threshold of fasudil-induced
preconditioning and postconditioning. In addition, Demiryürek et
al (8) firstly demonstrated
that cardioprotection of fasudil had a dose-dependent effect. Only
10 mg/kg dose fasudil was capable of mimicking the beneficial
effects of ischemic and pharmacological preconditioning in
anesthetized rats (8). Ichinomiya
et al (9) also showed that
only high-dose fasudil preserved postconditioning against
myocardial infarction under hyperglycemia in rats. The present
study also demonstrated that cardioprotection of fasudil
preconditioning and postconditiong tended to exhibit a
dose-dependent effect in the hypercholesterolemic rat.
Preconditioning and postconditioning have been shown
to involve the activation of the PI3K/Akt/eNOS pathway and
ultimately prevent the opening of the mitochondrial permeability
transition pore (18). Wolfrum
et al (10) showed that the
cardioprotective effect of Rho-kinase inhibition prior to ischemia
is involved in PI3K/Akt and nitric oxide synthase (NOS) activation.
Hamid et al (6) showed that
inhibition of Rho-kinase by Y27632, a structurally unrelated
inhibitor of fasudil, at reperfusion onset limited infarct size
through an Akt/eNOS-dependent mechanism. In addition, a number of
types of pharmacological preconditioning and postconditioning were
shown to depend on the PI3K/Akt/eNOS pathway (19,20).
The present western blot analysis revealed that high-dose fasudil
preconditioning and postconditioning markedly increased the
phosphorylation of Akt and eNOS as compared with the control group,
but low-dose fasudil preconditioning and postconditioning did not
increase the phosphorylation of Akt and eNOS as compared with the
control group. The results confirm a previous report that
hypercholesterolemia blocked phosphorylation of Akt and eNOS in
postconditioned myocardium (21).
It was also observed that high-dose fasudil preserved
preconditioning and postconditioning against myocardial
ischemia-reperfusion in hypercholesterolemic rats involved in
upregulating the PI3K/Akt/eNOS pathway.
The m-KATP channel is a target downstream of the
PI3K/Akt/eNOS pathway and an effector in cardioprotection by
ischemic preconditioning and postconditioning (22,23).
Fasudil-induced preconditioning and postconditioning is dependent
on activation of the m-KATP channel (9,12).
The current study reported that the preconditioning and
postconditioning stimulus of fasudil was eliminated by 5HD, an
m-KATP channel blocker and suggested that it is likely that fasudil
induced preconditioning and postconditioning in
hypercholesterolemic rats is mediated by m-KATP channels.
In conclusion, low-dose fasudil-induced
preconditioning postconditioning are abrogated by
hypercholesterolemia, but high-dose fasudil restores the
cardioprotection, which is involved in upregulating the
PI3K/Akt/eNOS pathway and inducing the opening of the m-KATP
channel.
Acknowledgements
This study was supported by a grant from the
Liaoning Provincial Science and Technology Projects, China (no.
2009225051-1).
References
|
1
|
Iliodromitis EK, Zoga A, Vrettou A, et al:
The effectiveness of postconditioning and preconditioning on
infarct size in hypercholesterolemic and normal anesthetized
rabbits. Atherosclerosis. 188:356–362. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ferdinandy P, Schulz R and Baxter GF:
Interaction of cardiovascular risk factors with myocardial
ischemia/reperfusion injury, preconditioning, and postconditioning.
Pharmacol Rev. 59:418–458. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Balakumar P and Babbar L: Preconditioning
the hyperlipidemic myocardium: fact or fantasy? Cell Signal.
24:589–595. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Nunes KP, Rigsby CS and Webb RC:
RhoA/Rho-kinase and vascular diseases: what is the link? Cell Mol
Life Sci. 67:3823–3836. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Satoh K, Fukumoto Y and Shimokawa H:
Rho-kinase: important new therapeutic target in cardiovascular
diseases. Am J Physiol Heart Circ Physiol. 301:H287–H296. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hamid SA, Bower HS and Baxter GF:
Rho-kinase activation plays a major role as a mediator of
irreversible injury in reperfused myocardium. Am J Physiol Heart
Circ Physiol. 292:H2598–H2606. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Fukumoto Y, Mohri M, Inokuchi K, et al:
Anti-ischemic effects of fasudil, a specific Rho-kinase inhibitor,
in patients with stable effort angina. J Cardiovasc Pharmacol.
49:117–121. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Demiryürek S, Kara AF, Celik A, Babül A,
Tarakçioglu M and Demiryürek AT: Effects of fasudil, a Rho-kinase
inhibitor, on myocardial preconditioning in anesthetized rats. Eur
J Pharmacol. 527:129–140. 2005.PubMed/NCBI
|
|
9
|
Ichinomiya T, Cho S, Higashijima U,
Matsumoto S, Maekawa T and Sumikawa K: High-dose fasudil preserves
postconditioning against myocardial infarction under hyperglycemia
in rats: role of mitochondrial KATP channels. Cardiovasc Diabetol.
11:282012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wolfrum S, Dendorfer A, Rikitake Y, et al:
Inhibition of Rho-kinase leads to rapid activation of
phosphatidylinositol 3-kinase/protein kinase Akt and cardiovascular
protection. Arterioscler Thromb Vasc Biol. 24:1842–1847. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Manintveld OC, Verdouw PD and Duncker DJ:
The RISK of ROCK. Am J Physiol Heart Circ Physiol. 292:H2563–H2565.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zhao JL, Yang YJ, Pei WD, Sun YH, You SJ
and Gao RL: Remote periconditioning reduces myocardial no-reflow by
the activation of K ATP channel via inhibition of Rho-kinase. Int J
Cardiol. 133:179–184. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhao H, Wang Y, Wu Y, et al:
Hyperlipidemia does not prevent the cardioprotection by
postconditioning against myocardial ischemia/reperfusion injury and
the involvement of hypoxia inducible factor-1alpha upregulation.
Acta Biochim Biophys Sin (Shanghai). 41:745–753. 2009. View Article : Google Scholar
|
|
14
|
Jia D: The protective effect of
mitochondrial ATP-sensitive K+ channel opener,
nicorandil, combined with Na+/Ca2+ exchange
blocker KB-R7943 on myocardial ischemia-reperfusion injury in rat.
Cell Biochem Biophys. 60:219–224. 2011.PubMed/NCBI
|
|
15
|
Nishizawa K, Wolkowicz PE, Yamagishi T,
Guo LL and Pike MM: Fasudil prevents KATP channel-induced
improvement in postischemic functional recovery. Am J Physiol Heart
Circ Physiol. 288:H3011–H3015. 2005. View Article : Google Scholar
|
|
16
|
Ma Z, Zhang J, Du R, Ji E and Chu L: Rho
kinase inhibition by fasudil has anti-inflammatory effects in
hypercholesterolemic rats. Biol Pharm Bull. 34:1684–1689. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ma Z, Zhang J, Ji E, Cao G, Li G and Chu
L: Rho kinase inhibition by fasudil exerts antioxidant effects in
hypercholesterolemic rats. Clin Exp Pharmacol Physiol. 38:688–694.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hausenloy DJ, Tsang A and Yellon DM: The
reperfusion injury salvage kinase pathway: a common target for both
ischemic preconditioning and postconditioning. Trends Cardiovasc
Med. 15:69–75. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Sumi S, Kobayashi H, Yasuda S, Iwasa M,
Yamaki T, Yamada Y, et al: Postconditioning effect of granulocyte
colony-stimulating factor is mediated through activation of risk
pathway and opening of the mitochondrial KATP channels. Am J
Physiol Heart Circ Physiol. 299:H1174–H1182. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Hönisch A, Theuring N, Ebner B, Wagner C,
Strasser RH and Weinbrenner C: Postconditioning with levosimendan
reduces the infarct size involving the PI3K pathway and
KATP-channel activation but is independent of PDE-III inhibition.
Basic Res Cardiol. 105:155–167. 2010.PubMed/NCBI
|
|
21
|
Andreadou I, Farmakis D, Prokovas E, et
al: Short-term statin administration in hypercholesterolaemic
rabbits resistant to postconditioning: effects on infarct size,
endothelial nitric oxide synthase, and nitro-oxidative stress.
Cardiovasc Res. 94:501–509. 2012. View Article : Google Scholar
|
|
22
|
Ghosh S, Standen NB and Galiñanes M:
Evidence for mitochondrial K ATP channels as effectors of human
myocardial preconditioning. Cardiovasc Res. 45:934–940. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Mykytenko J, Reeves JG, Kin H, et al:
Persistent beneficial effect of postconditioning against infarct
size: role of mitochondrial K(ATP) channels during reperfusion.
Basic Res Cardiol. 103:472–484. 2008. View Article : Google Scholar : PubMed/NCBI
|