Introduction
Carcinoma of the lung is responsible for the highest
rate of cancer-related mortality. The majority of these fatalities
(84%) are caused by non-small cell lung cancer (NSCLC) (1). Over half of the cases of NSCLC have
detectable distant metastasis at the time of diagnosis, including
16% with pleural metastasis. They are thus classified as stage IIIB
or IV (2,3). Platinum-based chemotherapy is the
treatment of choice for advanced and metastatic NSCLC. Although
novel chemotherapeutic agents continue to emerge, the development
of chemoresistance remains a significant problem (4). A number of mechanisms lead to
chemoresistance; it has been shown that altered expression of even
a single gene can result in cancer cell resistance to particular
drugs (5). Recent studies have
highlighted four genes involved in drug-resistance in NSCLC:
Excision repair cross-complementing gene 1 (ERCC1); thymidylate
synthase (TYMS); ribonucleotide reductase M1 (RRM1); and
βIII-tubulin (TUBB3) (6). These
molecules are important in DNA repair, and cell replication and
division.
ERCC1 is a key member of the nucleotide repair
exonuclease family. The ERCC1 protein forms a heterodimer with XPF
(ERCC4) and acts as a 5′-endonuclease to excise the lesion as well
as nucleotides surrounding the damaged site, a process termed
nucleotide excision repair (NER). ERCC1 is the rate-limiting enzyme
in NER (7). A recent study in
NSCLC cell lines showed that elevated DNA repair capacity, as a
result of enhanced ERCC1 expression, induced drug resistance
(8). Immunohistochemical studies
have shown that in patients with NSCLC, only those individuals with
ERCC1-negative tumors benefit from cisplatin-based chemotherapy
(9,10). TYMS is a rate-limiting enzyme in
thymidylate synthesis and dTMP is a required precursor for nucleic
acid synthesis (11). Pemetrexed
is an antifolate agent that predominantly targets TYMS. Treatment
with pemetrexed leads to thymidine and purine deficiency, thereby
inhibiting DNA synthesis, cell replication and tumor growth. A
number of studies have demonstrated that overexpression of TYMS
correlates with resistance to pemetrexed (12,13).
RR is comprised of two regulatory subunits of RRM1 and two
catalytic subunits of RRM2. RR is a rate-limiting enzyme for DNA
synthesis and is the only enzyme that reduces ribonucleotides into
deoxyribonucleotides. It is thus required for DNA synthesis and
repair (14). Vilmar et al
(15) showed that patients with
RRM1-negative advanced NSCLC who were treated with cisplatin and
vinorelbine, exhibited an improvement in disease control, longer
progression-free survival (PFS) and longer overall survival (OS).
Tubulin is a key constituent of the cytoskeleton, which
participates in cell movement, intracellular transportation and
cell mitosis. β-tubulin is the target of tubulin-binding agents.
These therapies inhibit mitosis by interfering with mitotic spindle
formation and are effective in treating a number of types of tumor.
The most commonly used anti-microtubule drugs are paclitaxel,
docetaxel and vincristine. Taxol promotes microtubule
polymerization and increases the stability of polymerized
microtubules. The persistent presence of microtubules during cell
division induces apoptosis. TUBB3 is primarily expressed in the
central and peripheral nervous system and is strongly expressed
during embryonic development (16). Expression of TUBB3 in NSCLC has
been associated with drug resistance to tubulin-binding agents
(17).
Myosin II is multifunctional, it has been identified
in muscle and non-muscle cells. Within muscle cells, myosin II
provides the driving force for muscle contraction, whereas in
non-muscle cells, it is an integral component of the cytoskeleton,
participating in cell movement, cytoplasmic flow, organelle
movement and mitosis. A recent study demonstrated that myosin II is
involved in lysophosphatidic acid (LAP)-mediated breast cancer cell
migration and invasion (18).
Myoglobin is an oxygen-carrying globin, which is primarily
distributed in skeletal muscle cells and cardiomyocytes. Myoglobin
reversibly binds to and releases oxygen, thereby promoting oxygen
diffusion from cytoplasm to mitochondria (19). Flonta et al (20) identified myoglobin expression in a
variety of epithelial tumors, including lung carcinoma. However, no
expression was detected in corresponding healthy tissues. Myoglobin
has been proposed to be important for tumor survival in hypoxia,
tumor cell metabolism and tumor growth. MyoDl is a transcription
factor, which is a member of the myogenic determination family,
MyoD. In breast cancer cells, MyoD binds to the E-box on the BRCA1
promoter and activates its transcription by inducing histone
acetylation (21). During
embryonic development, MyoD1 binds to the DNA E-box of stem cells,
to induce myogenic differentiation (22). In routine pathological practice,
MyoDl is primarily used as a marker for rhabdomyosarcoma.
In the current study, the expression of ERCC1, TYMS,
RRM1, TUBB3, myosin II, myoglobin and MyoD1 in pleural effusions
from patients with lung adenocarcinoma was evaluated and the
correlation between expression of these factors was analyzed.
Clinical follow-up was conducted in a subset of patients following
platinum-based chemotherapy and the association between survival
and protein expression was also investigated. The study aimed to
provide novel insights into the molecular pathology of lung
adenocarcinoma.
Materials and methods
Patient recruitment and cytological
sample collection
Pleural fluid from 116 patients with untreated
metastatic lung adenocarcinoma was collected between January 2011
and July 2012 at the China Medical University First Affiliated
Hospital (Shenyang, China). Diagnoses were made cytologically. This
procedure included the preliminary diagnosis of suspicious tumor
cells by microscopy, and the subsequent hematoxylin and eosin
staining and immunocytochemical staining of epithelial tumor
markers, in order to make a comprehensive assessment. Cytological
samples from 20 patients with inflammation-induced pleural
effusions were collected as the control group. The 116 patients
with malignant pleural effusions were comprised of 47 males and 69
females, with a mean age of 57 years (range, 26–87 years). Clinical
follow-up data were available in 48 patients with metastatic lung
adenocarcinoma, treated with platinum-based chemotherapy. The
follow-up periods varied between 15 and 28 months (until patients
succumbed to disease or 30th April, 2013).
This study was approved by the ethics committee of
China Medical University (Shenyang, China).
ThinPrep® cytology test (TCT)
and cell block preparation
Freshly collected pleural effusions (25 ml) were
centrifuged at 670 × g, at room temperature for 5 min. Supernatants
were discarded, and pellets were washed and centrifuged again at
670 × g for 5 min. Pellets were mixed with preservation solution
(Hologic, Inc., Bedford, Massachusetts, USA). ThinPrep slides were
made automatically by Thinprep 5000 (Product Insight Inc., Acton,
MA, USA).
For cell block preparation, 200 ml freshly collected
pleural effusion was centrifuged at 670 × g at room temperature for
5 min. Pellets were fixed in 95% ethanol for 12 h, embedded in
paraffin, sectioned (5 μm) and stained with hematoxylin and eosin
(HE). The slides were visualized under a microscope (Nikon 80i;
Nikon Corporation, Tokyo, Japan) and further observed by
transmission electron microscopy (JEM-1400; JEOL Ltd., Tokyo,
Japan).
Immunocytochemical stains
Immunocytochemical analysis was performed according
to the manufacturer’s instructions for EnVision (Maixin Biotech
Co., Ltd., Fuzhou, China). Table I
shows the details of the primary antibodies used. Paraffinized
slides were placed into an oven at 60°C for 120 min. Slides were
then placed into xylene solution in order to remove paraffin and
then into a graded ethanol series in order to remove the xylene.
Slides were then rinsed in distilled water. Following
deparaffinization and rehydration, the antigens were retrieved for
30 min at 100°C using Tris/Borate/EDTA cell-conditioning solution
(Maixin Biotech Co., Ltd.). Primary antibodies were incubated
separately for 60 min at room temperature, followed by incubation
with either mouse or rabbit polymers (ZSGB-BIO Co., Ltd., Beijing,
China) for 30 min. Visualization was facilitated with enhanced
diaminobenzidine chromagen (Maixin Biotech Co., Ltd.). Slides were
counterstained with hematoxylin. Appropriate positive and negative
controls were used to evaluate the human tissue samples, according
to the manufacturer’s instructions. Phosphate-buffered saline was
used as the negative control.
 | Table IPrimary antibodies used for
immunohistochemistry and western blot analysis. |
Table I
Primary antibodies used for
immunohistochemistry and western blot analysis.
| | Dilution | | |
|---|
| |
| | |
|---|
| Antibody | Host | ICC | Western blot | Source | Catalog no. |
|---|
| Cytokeratin 7 | Mouse
monoclonal | 1:100 | - | Santa Cruz | sc-23876 |
| TTF-1 | Rabbit
polyclonal | 1:100 | - | Santa Cruz | sc-13040 |
| Vimentin | Mouse
monoclonal | 1:100 | - | Santa Cruz | sc-53464 |
| ERCC1 | Mouse
monoclonal | 1:50 | 1:500 | Abcam | ab113941 |
| TYMS | Rabbit
polyclonal | 1:50 | 1:500 | Abcam | ab155795 |
| TUBB3 | Rabbit
monoclonal | 1:50 | 1:500 | Abcam | ab52901 |
| RRM1 | Mouse
monoclonal | 1:50 | 1:500 | Abcam | ab157250 |
| Nonmuscle Myosin
IIA | Rabbit
polyclonal | 1:50 | 1:500 | Abcam | ab24762 |
| Myoglobin | Mouse
monoclonal | 1:50 | 1:500 | Abcam | ab47702 |
| MyoD1 | Mouse
monoclonal | 1:50 | 1:500 | Abcam | ab16148 |
Dark brown staining observed in either the cytoplasm
or nuclei of cells was counted as a positive result. The average
percentage of positive cells in five randomly-selected high power
fields (x200) was calculated using a microscope (Nikon 80i, Nikon
Corporation, Tokyo, Japan). Samples with >5% positive cells were
regarded as positive for that stain. The immunocytochemical stains
were evaluated by three attending cytopathologists, and the results
shown are an average of the scores obtained by these
individuals.
Western blot analysis
Pleural effusions were collected and stored at −70°C
in a freezer. Total protein was extracted from cells in the
effusion and the protein concentration was measured using a
Bradford Protein Assay kit (Beyotime Institute of Biotechnology,
Haimen, China) which is based on the absorbance of Coomassie
Brilliant Blue G-250. The colorimetric absorbance of the samples
was measured at 465–595 nm on an Enzyme Standard instrument (MK3;
Thermo Fisher Scientific, Bedford, MA, USA). Following separation
by electrophoresis on SDS-PAGE gels, protein was transferred to
polyvinylidine fluoride membranes (Beyotime Institute of
Biotechnology). Membranes were blocked with 5% non-fat milk for 2 h
at room temperature and incubated with primary antibody (Table I) separately at 4°C overnight.
Following washing in Tris-buffered saline with Tween-20 (Beyotime
Institute of Biotechnology), membranes were incubated with goat
anti-mouse polyclonal horseradish peroxidase-conjugated secondary
antibodies (ZSGB-BIO. Co., Ltd.), at room temperature for 2 h.
Membranes were developed using Thermo chemiluminescent substrate
kits (Thermo Fisher Scientific). β-actin was used as an internal
control. Protein expression was quantified using a gel imaging
analysis system (Systems BioImaging Lab, Santa Barbara, CA,
USA).
Statistical analysis
Statistical data analysis was performed using
SPSS17.0 statistical software (SPSS Inc., Chicago, IL, USA). The
association between gene expression and clinical characteristics
was analyzed using χ2 test or Fisher’s exact test. The
correlation between different chemoresistance factors was analyzed
using Spearman’s correlation coefficients. The Kaplan-Meier method
and the Log-rank test were performed to analyze the relationship
between patient survival and expression of the proteins
investigated. Multivariate Cox regression analysis was used to
analyze the correlation between age, gender and survival. P<0.05
was considered to indicate a statistically significant
difference.
Results
Pleural effusion cytology and
immunocytochemistry
Diagnosis of metastatic lung adenocarcinoma was made
cytologically from pleural fluid samples and confirmed by positive
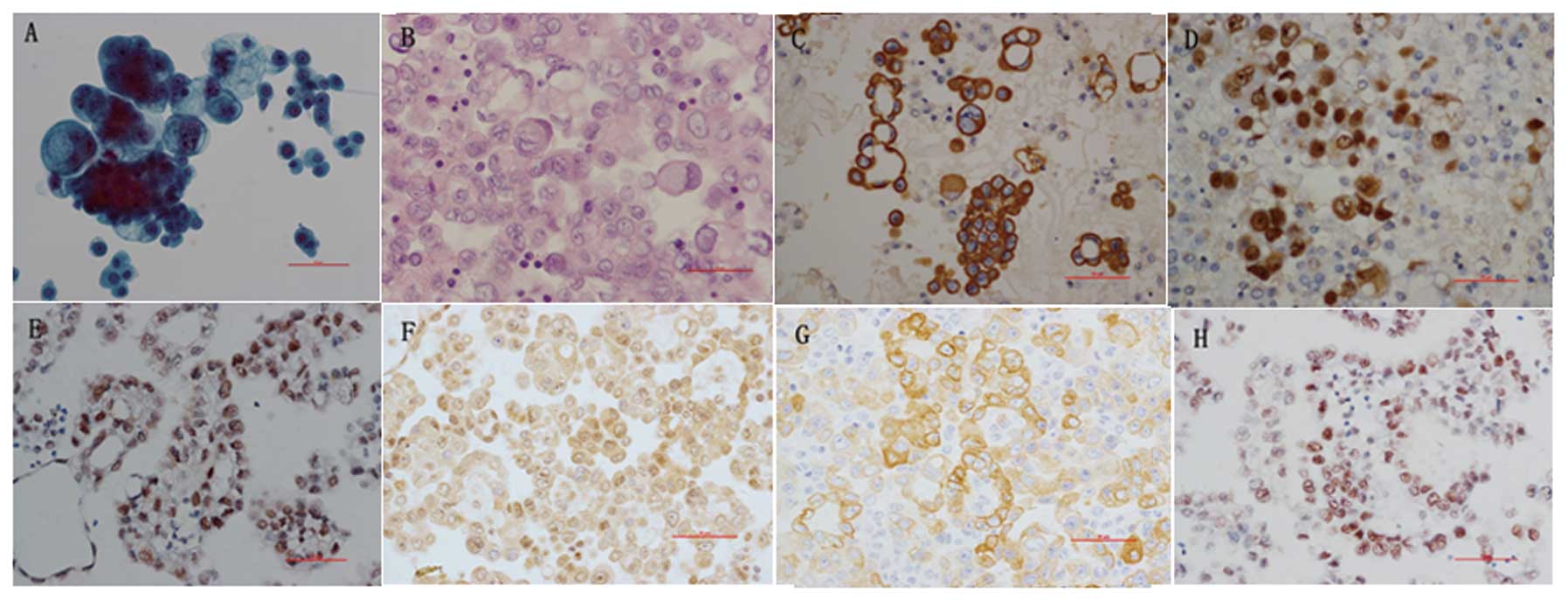
TTF-1 and CK7 staining in cell blocks (Fig. 1).
Protein expression of drug
resistance-related factors
The expression of ERCC1, TYMS, RRM1, TUBB3 and
vimentin was evaluated in the 116 samples from patients with
metastatic lung adenocarcinoma (Fig.
1). The positive rate for ERCC1 was 37%, with positive staining
observed in the nuclei. The positive rate for TYMS was 36.2%, with
positive staining observed in the nuclei and cytoplasm. Positive
rates for RRM1 and TUBB3 were 82.7 and 69.8%, respectively, and
positive staining was observed in the cytoplasm. The positive rate
for vimentin was 83.6%, with positive staining observed in the
cytoplasm. In the subset of 50 patients with clinical follow-up who
were treated with platinum-based chemotherapy, the expression of
myosin II, myoglobin, and MyoD1 were also found to be upregulated
(Fig. 1). The positive rate for
myosin II was 48%, with cytoplasmic staining observed. The positive
rate for myoglobin was 40%, with cytoplasmic staining observed. The
positive rate for MyoD1 was 38%, with nuclear staining
observed.
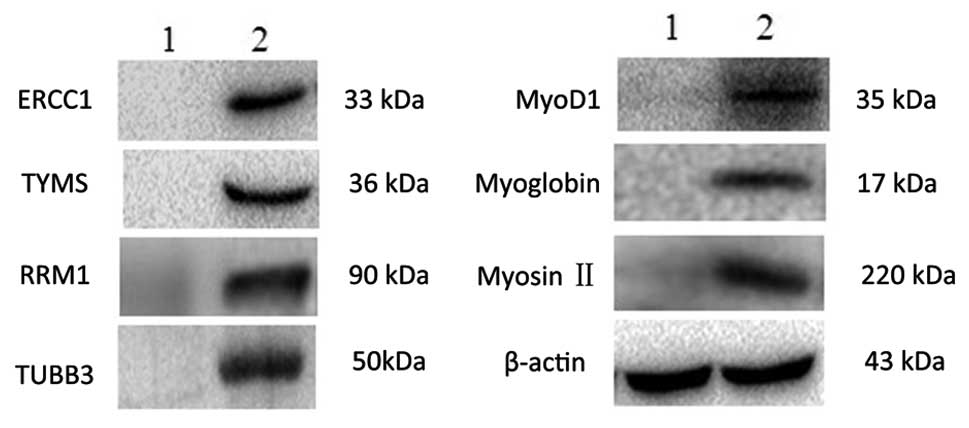
The protein expression levels of ERCC1, TYMS, TUBB3,
non-muscle myosin II, myoglobin and MyoD1 were also measured by
western blot analysis. These proteins were not measurable in the
inflammation-induced pleural fluids from the control group.
However, they were all detectable in the pleural effusions from
patients with metastatic lung adenocarcinoma (Fig. 2).
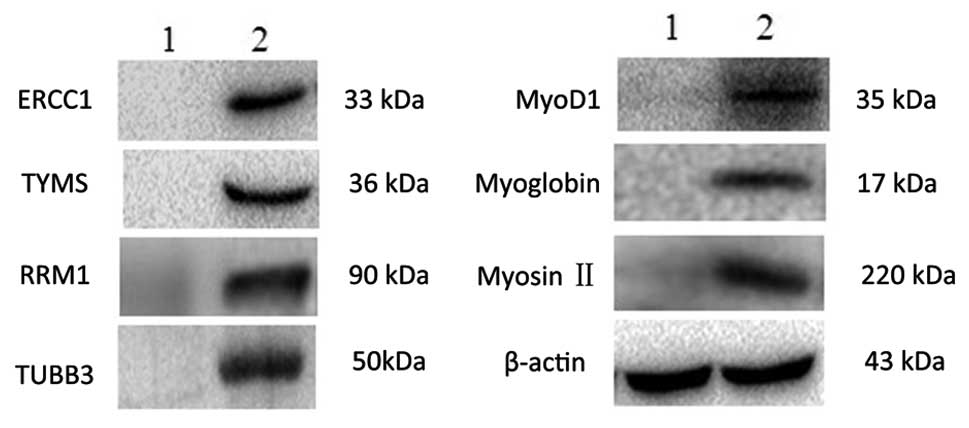 | Figure 2Expression of ERCC1, TYMS, RRM1,
TUBB3, vimentin, myosin II, myoglobin and MyoD1 in cells from
pleural fluid was analyzed by western blotting. Sample 1 contained
cells from reactive inflammatory cell pleural effusions. Sample 2
contained cells from malignant pleural effusions in patients with a
diagnosis of lung adenocarcinoma. β-actin was used as a control.
ERCC1, excision repair cross-complementing gene 1; TYMS,
thymidylate synthase; RRM1, ribonucleotide reductase M1; TUBB3,
βIII-tubulin. |
Correlation between drug
resistance-related factor expression
In the 116 samples of pleural fluid from patients
with metastatic lung adenocarcinomas there was a significant
positive correlation between the expression of ERCC and TYMS
(r=0.54, P=0.000), between RRM1 and TUBB3 (r=0.45, P=0.000),
between ERCC1 and TUBB3 (r=0.35, P=0.000), between ERCC1 and RRM1
(r=0.26, P=0.006), and between TYMS and TUBB3 (r=0.22, P=0.017).
The correlation between the expression of TYMS and RRM1 was not
statistically significant, (r=0.06, P=0.530; Table II).
 | Table IICorrelation between expression of
ERCC1, TYMS, RRM1 and TUBB3. |
Table II
Correlation between expression of
ERCC1, TYMS, RRM1 and TUBB3.
| A, Presence of
ERCC1 in relation to that of TYMS, TUBB3 and RRM1. |
|---|
|
|---|
| ERCC1 + | ERCC1 − | Total | r | P-value |
|---|
| TYMS |
| + | 30 | 12 | 42 | 0.54 | 0.000 |
| − | 13 | 61 | 74 | | |
| Total | 43 | 73 | 116 | | |
| TUBB3 |
| + | 39 | 42 | 81 | 0.35 | 0.000 |
| − | 4 | 31 | 35 | | |
| Total | 43 | 73 | 116 | | |
| RRM1 |
| + | 41 | 55 | 96 | 0.25 | 0.006 |
| − | 2 | 18 | 20 | | |
| Total | 43 | 73 | 116 | | |
|
| B, Presence of RRM1
in relation to that of TUBB3. |
|
| RRM1 + | RRM1 − | Total | r | P |
|
| TUBB3 |
| + | 76 | 5 | 81 | 0.45 | 0.000 |
| − | 20 | 15 | 35 | | |
| Total | 96 | 20 | 116 | | |
|
| C, Presence of TYMS
in relation to that of TUBB3 and RRM1. |
|
| TYMS + | TYMS − | Total | r | P |
| TUBB3 |
|
| + | 35 | 46 | 81 | 0.22 | 0.017 |
| − | 7 | 28 | 35 | | |
| Total | 42 | 74 | 116 | | |
| RRM1 |
| + | 36 | 60 | 96 | 0.06 | 0.530 |
| − | 6 | 14 | 20 | | |
| Total | 42 | 74 | 116 | | |
In the subset of 50 cases treated with
platinum-based chemotherapy who received clinical follow-up,
significantly positive correlations were identified between the
expression of myoglobin and MyoD1 (r=0.96, P=0.000), between myosin
II and MyoD1 (r=0.81, P=0.000), and between myosin II and myoglobin
(r=0.77, P=0.000; Table III).
Expression of these three factors was also positively correlated
with the expression of ERCC1, TYMS, RRM1 and TUBB3 (Table IV).
 | Table IIICorrelation between expression of
myosin II, myoglobin and MyoD1 (50 samples). |
Table III
Correlation between expression of
myosin II, myoglobin and MyoD1 (50 samples).
| A, Presence of
myosin II in relation to that of myoglobin anf MyoD1. |
|---|
|
|---|
| Myosin II + | Myosin II − | Total | r | P-value |
|---|
| Myoglobin |
| + | 19 | 1 | 20 | 0.77 | 0.000 |
| − | 5 | 25 | 30 | | |
| Total | 24 | 26 | 50 | | |
| MyoD1 |
| + | 19 | 0 | 19 | 0.81 | 0.000 |
| − | 5 | 26 | 31 | | |
| Total | 24 | 26 | 50 | | |
|
| B, Presence of
myoglobin in relation to that of MyoD1. |
|
| Myoglobin + | Myoglobin − | Total | r | P-value |
|
| MyoD1 |
| + | 19 | 0 | 19 | 0.96 | 0.000 |
| − | 1 | 30 | 31 | | |
| Total | 20 | 30 | 50 | | |
 | Table IVCorrelation between expression of
seven proteins (50 Samples). |
Table IV
Correlation between expression of
seven proteins (50 Samples).
| A, Presence of
myosin in relation to that of ERCC1, TYMS, TUBB3 and RRM1. |
|---|
|
|---|
| Myosin + | Myosin − | r | P-value |
|---|
| ERCC1 |
| + | 20 | 1 | 0.8 | 0.000 |
| − | 4 | 25 | | |
| TYMS |
| + | 18 | 4 | 0.6 | 0.000 |
| − | 6 | 22 | | |
| TUBB3 |
| + | 21 | 13 | 0.4 | 0.004 |
| − | 3 | 13 | | |
| RRM1 |
| + | 24 | 17 | 0.45 | 0.001 |
| − | 0 | 9 | | |
|
| B, Presence of
myoglobin in relation to that of ERCC1, TYMS, TUBB3 and RRM1. |
|
| Myglobin + | Myoglobin − | r | P-value |
|
| ERCC1 |
| + | 18 | 3 | 0.79 | 0.000 |
| − | 2 | 27 | | |
| TYMS |
| + | 18 | 4 | 0.76 | 0.000 |
| − | 2 | 26 | | |
| TUBB3 |
| + | 20 | 14 | 0.56 | 0.000 |
| − | 0 | 16 | | |
| RRM1 |
| + | 20 | 21 | 0.38 | 0.006 |
| − | 0 | 9 | | |
|
| C, Presence of
MyoD1 in relation to that of ERCC1, TYMS, TUBB3 and RRM1. |
|
| MyoD1 + | MyoD1 − | r | P-value |
|
| ERCC1 |
| + | 17 | 4 | 0.75 | 0.000 |
| − | 2 | 27 | | |
| TYMS |
| + | 18 | 4 | 0.80 | 0.000 |
| − | 1 | 27 | | |
| TUBB3 |
| + | 19 | 15 | 0.54 | 0.000 |
| − | 0 | 16 | | |
| RRM1 |
| + | 19 | 22 | 0.37 | 0.009 |
| − | 0 | 9 | | |
Association between protein expression
and survival
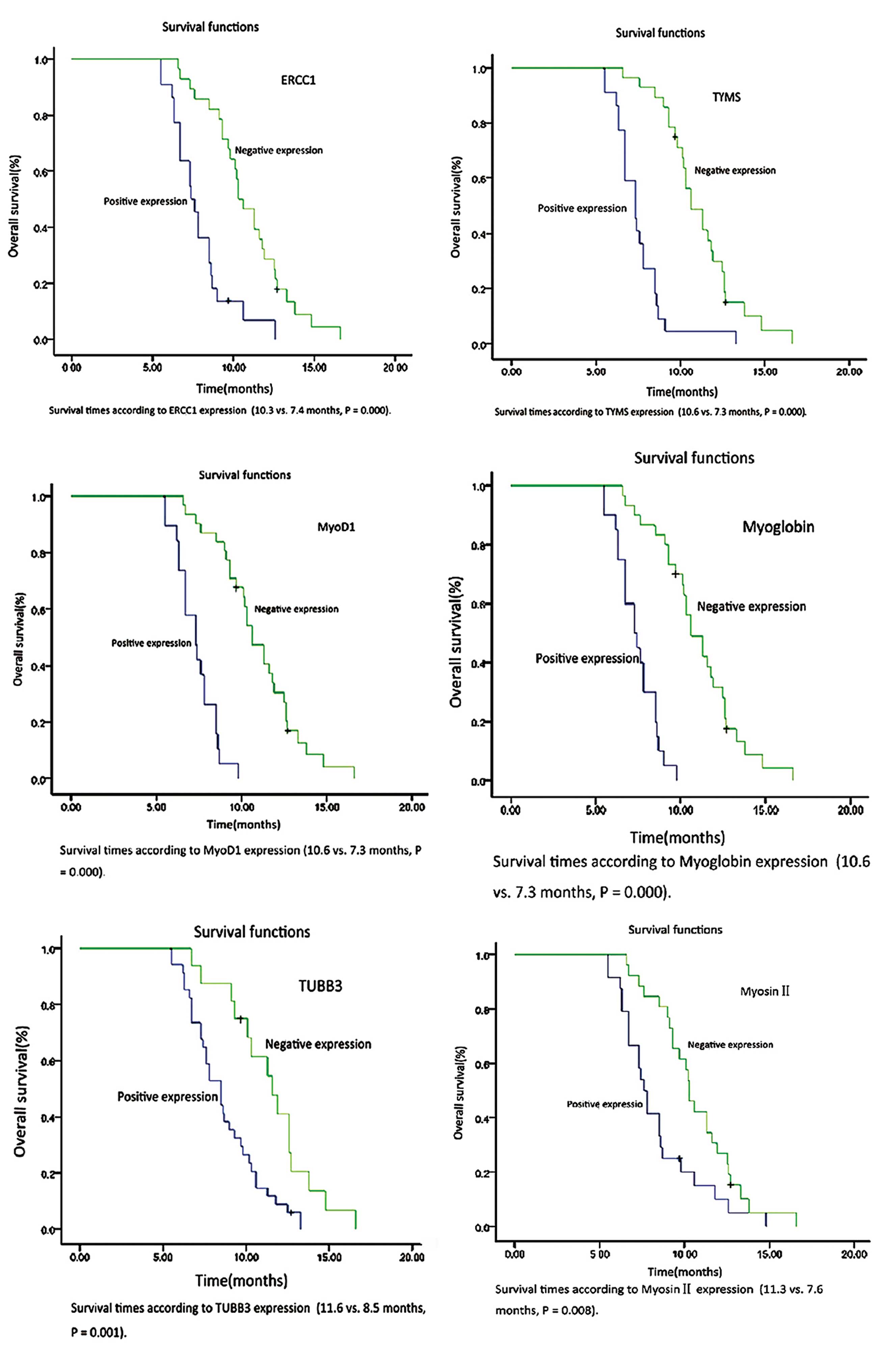
Two out of 50 patients were lost to clinical
follow-up. Kaplan-Meier survival analysis was performed in the
remaining 48 cases. Patients with an undetectable expression of
ERCC1, TYMS, and TUBB3 had a longer survival time compared with
patients with a positive expression of these proteins (10.3 months
and 7.4 months, P=0.000; 10.6 months and 7.3 months, P=0.000; and
11.6 months and 8.5 months, P=0.001, respectively). Negative
correlations were also observed between the expression of myosin
II, myoglobin, and MyoD1 and survival. Positive expression was
related to a worse prognosis (10.3 months compared with 7.6 months,
P=0.008; 10.6 months compared with 7.3 months, P=0.000; and 10.6
months compared with 7.3 months, P=0.000, respectively; Fig. 3). The expression of RRM1 showed no
correlation with survival time (P=0.158). Survival was not
associated with age or gender (P=0.517 and P=0.592,
respectively).
Discussion
Chemotherapy is the treatment of choice for advanced
or metastatic NSCLC. According to the recent non-small cell lung
cancer treatment guideline from the National Comprehensive Cancer
Network website (NCCN, Fort Washington, PA, USA, 2011), cisplatin
or carboplatin-based chemotherapy remains the first-line treatment
for standard chemotherapy. The combination of a platinum-based drug
with another drug, constitutes an effective treatment protocol
(23). However, the development of
drug resistance has become a significant problem. A change in the
expression of a resistance protein may induce resistance towards
one or more drugs. Platinum interacts with DNA to form Pt-DNA
adducts, resulting in DNA cross-linking or chain cross-linking and
the formation of an abnormal DNA double helix, thereby resulting in
apoptosis (24). ERCC1 clears
cisplatin-induced DNA complexes and repairs the damaged DNA,
leading to resistance to platinum-based therapies (25). Amongst patients with NSCLC treated
with platinum-based chemotherapy, ERCC1-negative individuals
exhibit a longer PFS than ERCC1-positive individuals (26,27).
The present study confirmed these observations, demonstrating a
poor prognosis in patients with lung adenocarcinoma who expressed
ERCC1 in tumor cells from pleural effusions. TYMS is a key enzyme
in DNA synthesis, affecting the efficacy of drugs that target this
process. Shimizu et al (28) showed that the level of expression
of TYMS mRNA affected pemetrexed treatment efficacy. For patients
with NSCLC receiving pemetrexed treatment, TYMS is a molecular
marker, which predicts treatment effect. RRM1, like ERCC1 and TYMS,
is important in DNA synthesis and repair. An association between
its overexpression and gemcitabine resistance has previously been
reported (29). In a
meta-analysis, Gonga et al (30) showed that amongst patients with
late-stage NSCLC receiving a gemcitabine chemotherapy regimen, a
low or negative level of expression of RRM1 was associated with a
higher rate of drug response, longer survival and time to
progression. In healthy adult tissues, TUBB3 distribution is
primarily limited to nervous system tissues. However, a number of
studies have demonstrated TUBB3 expression in non-neurogenic solid
tumors, such as breast cancer, ovarian cancer and colon cancer
(31–35). The expression of TUBB3 in tumor
cells may represent a ‘dedifferentiation’, indicating a greater
malignant and metastatic capacity (36). High expression levels of TUBB3 in
NSCLC, breast cancer, ovarian cancer and metastatic carcinoma have
been reported to be associated with a lower sensitivity to
vinblastine and paclitaxel, as well as lower survival rates
(31–34,37).
The present results indicate increased expression of ERCC1, RRM1,
TYMS and TUBB3 in pleural effusions from a subpopulation of
patients with metastatic lung adenocarcinoma. The expression of
these factors appears to be correlated. The median survival of
patients with detectable ERCC1, TYMS and TUBB3 expression was
shorter than that of patients with negative expression of these
proteins. The impact of RRM1 expression on survival was not found
to be statistically significant.
Previous studies have shown that
epithelial-mesenchymal transition (EMT) is important in tumor
invasion, metastasis, the acquisition of stem cell-like
characteristics and the development of drug resistance (38). Studies have demonstrated that
gemcitabine-resistant pancreatic cancer cells undergo EMT via
activation of the Notch signaling pathway. The transitioned cells
exhibited decreased expression of E-cadherin and β-catentin, and
increased expression of ZEB1, Snail and vimentin. They also
displayed morphological alterations (39). An oxaliplatin-resistant colorectal
cancer cell line developed a phenotype akin to that of mesenchymal
cells, with long spindle-shaped cells, loss of polarity, loss of
cell cohesiveness, increased metastasis and invasion, and changes
in molecular markers (40).
Similar changes have also been reported in paclitaxel-resistant
ovarian cancer cell lines (41).
Snail has been reported to enhance ERCC1 expression. It thus
contributes to cisplatin resistance (42). The association between other
drug-resistance genes and EMT is largely unknown. The present study
measured myoglobin, myosin II and MyoD1 protein expression in 50
randomly-selected patients. Kocaefe et al (43) found that following MyoD1
transfection into umbilical cord blood mesenchymal stem cells, the
stem cells displayed certain functional proteins characteristic of
muscle cells, such as desmin, myosin and myoglobin. The results
from the present study demonstrated the expression of myoglobin,
myosin II and MyoD1 in lung adenocarcinoma cells obtained from
pleural effusions. The expression of each of these markers was
positively correlated. To the best of our knowledge, MyoD1
expression in lung cancer has not been previously reported in the
literature. Giarnieri et al (44) found that when lung adenocarcinoma
in pleural effusions underwent EMT, the tumor cells lost expression
of E-cadherin and exhibited enhanced expression of N-cadherin. In
the current study, cancer cells expressed not only the epithelial
marker, CK7, but also the mesenchymal marker, vimentin, in 83.6% of
cases. One explanation for the increased expression of myglobin,
myosin II and MyoD1, is that these proteins are by-products of
adenocarcinoma cells undergoing the EMT process. Tumor cells may
acquire certain mesenchymal characteristics and upregulate the
expression of MyoD1, followed by the expression of myoglobin and
myosin II. Furthermore, increased expression of myosin II may also
be a response to an increase in cytoskeletal activity. The
cytoskeleton is important in maintaining cell morphology,
intracellular transportation and cellular motility. The present
results showed increased cytoskeletal components, TUBB3 and myosin
II, in pleural fluid samples from certain patients with metastatic
lung adenocarcinoma. These are key components of microtubules and
actin filaments, respectively. Such changes may enhance the
metastatic capability of late-stage tumor cells. In the present
study TCT and HE slides were produced, and visualized under an
electron microscope. Increased myosin II protein expression levels
were shown to be associated with fibrous components in the
cytoplasm, with a reticular pattern. The fibrous net may form a
mechanical barrier against chemotherapy drugs, thereby facilitating
the development of drug resistance.
The present study also showed that expression of the
myoglobin, myosin II and MyoD1 proteins was positively correlated
with the expression of four known drug-resistance genes. Snail, a
key regulator of the EMT process, is known to increase ERCC1
expression. The current results further suggest the importance of
EMT in the malignant transformation of tumor cells. Oleksiewicz
et al (45) observed
myoglobin expression in primary lung adenocarcinoma. Individuals
with a higher expression level had a shorter average survival time,
which may have been associated with the increased anti-hypoxia
capacity of the tumors. Xiong et al (46) found that in patients with
early-stage bladder cancer, high myosin II expression was
associated with a lower five-year survival rate, as well as an
increase in lymph node metastasis. The results from the present
study also illustrated that the average survival time of myoglobin,
myosin II and MyoD1-positive patients was shorter than that of
negative patients. The exact mechanisms underlying this reduction
in survival time are unknown. We hypothesize that this expression
pattern is a common phenotype in all highly-malignant tumor cells
and increases tumor cell resistance to hypoxia, nutritional
deficiencies and chemotherapy treatment. This phenotype also
enhances the invasion and metastasis of tumor cells, which gain
certain cancer stem cell-like properties.
The enhanced protein expression of drug resistance
genes increases DNA synthesis in tumor cells, accelerates tumor
proliferation, promotes tumor cell invasion and metastasis, and
induces resistance to drugs targeting these molecules. Sensitivity
to standard chemotherapy varies significantly among individuals,
even those with the same pathological type and stage of tumors. In
recent years the concept of individualized medicine has been
proposed. The current data showed drug resistance protein
expression in samples of pleural fluid from subsets of patients
with metastatic lung adenocarcinoma. The expression of these
proteins was correlated with one another and the overall survival
in patients expressing drug resistance factors was lower than that
in patients in whom these factors were undetectable. The collection
of pleural fluid is a technically simple method for obtaining tumor
cells. Immunocytochemical analysis of drug resistance gene protein
expression is a rapid and convenient approach to analyze the
expression of these drug resistance genes. The results of
immunocytochemical analyses may provide a reliable basis for the
choice of individualized chemotherapy protocols, thus improving
prognosis and potentially reducing treatment costs.
References
|
1
|
Siegel R, Naishadham D and Jemal A: Cancer
statistics, 2013. CA Cancer J Clin. 63:11–30. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Marshall HM, Leong SC, Bowman RV, et al:
The science behind the 7th edition Tumour, Node, Metastasis staging
system for lung cancer. Respirology. 17:247–260. 2012. View Article : Google Scholar
|
|
3
|
Morgensztern D, Waqar S, Subramanian J, et
al: Prognostic impact of malignant pleural effusion at presentation
in patients with metastatic non-small-cell lung cancer. J Thorac
Oncol. 7:1485–1489. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zahreddine H and Borden LB: Mechanisms and
insights into drug resistance in cancer. Front Pharmacol. 4:282013.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Suh DH, Kim MK, Kim HS, Chung HH and Song
YS: Epigenetic therapies as a promising strategy for overcoming
chemoresistance in epithelial ovarian cancer. J Cancer Prev.
18:227–234. 2013. View Article : Google Scholar
|
|
6
|
Zhang L, Yang H and Xu J: Gene expression
significance in personalized medicine of non-small-cell lung cancer
and gene expression analyzing platforms. Curr Drug Metab.
12:455–459. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sancar A and Reardon JT: Nucleotide
excision repair in E. coli and man. Adv Protein Chem. 69:43–71.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Van Den Broeck A, Nissou D, Brambilla E,
et al: Activation of a Tip60/E2F1/ERCC1 network in human lung
adenocarcinoma cells exposed to cisplatin. Carcinogenesis.
33:320–325. 2012. View Article : Google Scholar
|
|
9
|
Olaussen KA, Dunant A, Fouret P, et al:
DNA repair by ERCC1 in non-small-cell lung cancer and
cisplatin-based adjuvant chemotherapy. N Engl J Med. 355:983–991.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Xianjun F, Xiu-guang Q, Li Z, et al: ERCC1
and BRCA1 mRNA expression predicts the clinical outcome of
non-small cell lung cancer receiving platinum-based chemotherapy.
Pak J Med Sci. 30:488–492. 2014.
|
|
11
|
Gangjee A, Yu J, McGuire JJ, et al:
Design, synthesis, and X-ray crystal structure of a potent dual
inhibitor of thymidylate synthase and dihydrofolate reductase as an
antitumor agent. J Med Chem. 43:3837–3851. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sigmond J, Backus HH, Wouters D, et al:
Induction of resistance to the multitargeted antifolate Pemetrexed
(ALIMTA) in WiDr human colon cancer cells is associated with
thymidylate synthase overexpression. Biochem Pharmacol. 66:431–438.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wang T, Chuan Pan C, Rui Yu J, et al:
Association between TYMS expression and efficacy of
pemetrexed-based chemotherapy in advanced non-small cell lung
cancer: a meta-analysis. PLoS one. 8:e742842013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Rosell R, Cobo M, Isla D, et al:
Pharmacogenomics and gemcitabine. Ann Oncol. 17(Suppl 5): 13–16.
2006. View Article : Google Scholar
|
|
15
|
Vilmar AC, Santoni-Rugiu E and Sorensen
JB: Predictive impact of RRM1 protein expression on vinorelbine
efficacy in NSCLC patients randomly assigned in a chemotherapy
phase III trial. Ann Oncol. 24:309–314. 2013. View Article : Google Scholar
|
|
16
|
Katsetos CD, Herman MM and Mörk SJ: Class
III beta-tubulin in human development and cancer. Cell Motil
Cytoskeleton. 55:77–96. 2003. View
Article : Google Scholar : PubMed/NCBI
|
|
17
|
McCarroll JA, Gan PP, Liu M and Kavallaris
M: betaIII-tubulin is a multifunctional protein involved in drug
sensitivity and tumorigenesis in non-small cell lung cancer. Cancer
Res. 70:4995–5003. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kim JH and Adelstein RS: LPA(1)-induced
migration requires nonmuscle myosin II light chain phosphorylation
in breast cancer cells. J Cell Physiol. 226:2881–2893. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Merx MW, Flögel U, Stumpe T, et al:
Myoglobin facilitates oxygen diffusion. FASEB J. 15:1077–1079.
2001.PubMed/NCBI
|
|
20
|
Flonta SM, Arena S, Pisacane A, et al:
Expression and functional regulation of myoglobin in epithelial
cancers. Am J Pathol. 175:201–206. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Jin W, Liu Y, Chen L, et al: Involvement
of MyoD and c-myb in regulation of basal and estrogen-induced
transcription activity of the BRCA1 gene. Breast Cancer Res Treat.
125:699–713. 2011. View Article : Google Scholar
|
|
22
|
Soleimani VD, Yin H, Jahani-Asl A, et al:
Snail regulates MyoD binding-site occupancy to direct enhancer
switching and differentiation-specific transcription in myogenesis.
Mol Cell. 47:457–468. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Polo V and Besse B: Maintenance strategies
in stage IV non-small-cell lung cancer (NSCLC): in which patients,
with which drugs? Ann Oncol. 25:1283–1293. 2014. View Article : Google Scholar
|
|
24
|
Hildebrandt MA, Gu J and Wu X:
Pharmacogenomics of platinum-based chemotherapy in NSCLC. Expert
Opin Drug Metab Toxicol. 5:745–755. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ota S, Ishii G, Goto K, et al:
Immunohistochemical expression of BCRP and ERCC1 in biopsy specimen
predicts survival in advanced non-small-cell lung cancer treated
with cisplatin-based chemotherapy. Lung Cancer. 64:98–104. 2009.
View Article : Google Scholar
|
|
26
|
Das M, Riess JW, Frankel P, et al: ERCC1
expression in circulating tumor cells (CTCs) using a novel
detection platform correlates with progression-free survival (PFS)
in patients with metastatic non-small-cell lung cancer (NSCLC)
receiving platinum chemotherapy. Lung Cancer. 77:421–426. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Gao Z, Han B, Shen J, et al: ERCC1 protein
as a guide for individualized therapy of late-stage advanced
non-small cell lung cancer. Exp Ther Med. 2:811–815. 2011.
|
|
28
|
Shimizu T, Nakanishi Y, Nakagawa Y, et al:
Association between expression of thymidylate synthase,
dihydrofolate reductase, and glycinamide ribonucleotide
formyltransferase and efficacy of pemetrexed in advanced non-small
cell lung cancer. Anticancer Res. 32:4589–4596. 2012.PubMed/NCBI
|
|
29
|
Dong X, Hao Y, Wei Y, et al: Response to
first-line chemotherapy in patients with non-small cell lung cancer
according to RRM1 expression. PLoS One. 9:e923202014. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Gong W, Zhang X, Wu J, et al: RRM1
expression and clinical outcome of gemcitabine-containing
chemotherapy for advanced non-small-cell lung cancer: a
meta-analysis. Lung Cancer. 75:374–380. 2012. View Article : Google Scholar
|
|
31
|
Dumontet C, Isaac S, Souquet PJ, et al:
Expression of class III beta tubulin in non-small cell lung cancer
is correlated with resistance to taxane chemotherapy. Bull Cancer.
92:E25–E30. 2005.PubMed/NCBI
|
|
32
|
Sève P, Isaac S, Trédan O, et al:
Expression of class III β-tubulin is predictive of patient outcome
in patients with non-small cell lung cancer receiving
vinorelbine-based chemotherapy. Clin Cancer Res. 11:5481–5486.
2005. View Article : Google Scholar
|
|
33
|
Ferrandina G, Zannoni GF, Martinelli E, et
al: Class III beta-tubulin overexpression is a marker of poor
clinical outcome in advanced ovarian cancer patients. Clin Cancer
Res. 12:2774–2779. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Tommasi S, Mangia A, Lacalamita R, et al:
Cytoskeleton and paclitaxel sensitivity in breast cancer: the role
of beta-tubulins. Int J Cancer. 120:2078–2085. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Portyanko A, Kovalev P, Gorgun J and
Cherstvoy E: beta(III)-tubulin at the invasive margin of colorectal
cancer: possible link to invasion. Virchows Arch. 454:541–548.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Katsetos CD and Dráber P: Tubulins as
therapeutic targets in cancer: from bench to bedside. Curr Pharm
Des. 18:2778–2792. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Maus MK, Mack PC, Astrow SH, et al:
Histology-related associations of ERCC1, RRM1, and TS biomarkers in
patients with non small-cell lung cancer: implications for therapy.
J Thoracic Oncol. 8:582–586. 2013.
|
|
38
|
Polyak K and Weinberg RA: Transitions
between epithelial and mesenchymal states: acquisition of malignant
and stem cell traits. Nat Rev Cancer. 9:265–273. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Wang Z, Li Y, Kong D, et al: Acquisition
of epithelial-mesenchymal transition phenotype of
gemcitabine-resistant pancreatic cancer cells is linked with
activation of the notch signaling pathway. Cancer Res.
69:2400–2407. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Yang AD, Fan F, Camp ER, et al: Chronic
oxaliplatin resistance induces epithelial-to-mesenchymal transition
in colorectal cancer cell lines. Clin Cancer Res. 12:4147–4153.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Kajiyama H, Shibata K, Terauchi M, et al:
Chemoresistance to paclitaxel induces epithelial-mesenchymal
transition and enhances metastatic potential for epithelial ovarian
carcinoma cells. Int J Oncol. 31:277–283. 2007.PubMed/NCBI
|
|
42
|
Hsu DS, Lan HY, Huang CH, et al:
Regulation of excision repair cross-complementation group 1 by
Snail contributes to cisplatin resistance in head and neck cancer.
Clin Cancer Res. 16:4561–4571. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Kocaefe C, Balci D, Hayta BB and Can A:
Reprogramming of human umbilical cord stromal mesenchymal stem
cells for myogenic differentiation and muscle repair. Stem Cell
Rev. 6:512–522. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Giarnieri E, De Vitis C, Noto A, et al:
EMT markers in lung adenocarcinoma pleural effusion spheroid cells.
J Cell Physiol. 228:1720–1726. 2013. View Article : Google Scholar
|
|
45
|
Oleksiewicz U, Daskoulidou N, Liloglou T,
et al: Neuroglobin and myoglobin in non-small cell lung cancer:
expression, regulation and prognosis. Lung Cancer. 74:411–418.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Xiong D, Ye YL, Chen MK, et al: Non-muscle
myosin II is an independent predictor of overall survival for
cystectomy candidates with early-stage bladder cancer. Oncol Rep.
28:1625–1632. 2012.PubMed/NCBI
|