Introduction
Gastric cancer (GC) is the fourth most prevalent
malignancy, and is the second most common cause of
cancer-associated mortality worldwide (1,2). In
addition, GC is one of the most common malignancies in East Asian
countries (3). The leading cause
of GC-associated mortality is the late detection of advanced stage
GC (IIIA-IV), due to the absence of early diagnostic biomarkers
(4). A previous study revealed
that the 5-year survival rate of patients with stage IV GC is only
7–10.1%; however, the 5-year survival rate of patients with stage
IA is 78–93.3% (5,6). Early diagnosis of GC is essential for
effective therapy; therefore, the detection of sensitive and
specific biomarkers for GC diagnosis may significantly improve
treatment and decrease mortality rates (7).
Autoimmunity refers to the production of antibodies
to autologous cellular antigens and is increasingly being
associated with malignancy, as autoantibodies against
tumor-associated antigens (TAA) have been discovered in the sera of
patients with various cancers and may be used as novel biomarkers
(8). Due to the general absence of
particular autoantibodies in normal conditions or non-cancer
individuals, it is feasible to use autoantibodies as serum
biomarkers for cancer diagnosis. In addition, autoantibodies
exhibit various properties that make them attractive early cancer
biomarkers (9–11). Firstly, autoantibodies may be
identified in the asymptomatic stage of cancer, and may be measured
as early as 5 years prior to the onset of malignancy (12). Secondly, autoantibodies against
TAAs have been detected in the sera of patients with cancer. In
addition, autoantibodies may be inherently persistent and stable in
the sera for relatively long periods of time. Serum biomarkers may
therefore be used to recognize tumorigenesis (13).
Generally, proteomics-based methods are available
for recognizing protein biomarkers in the sera of patients with
cancer (14). Using this approach,
we previously identified novel serological biomarkers, including
the anti-heat shock protein (HSP) 60 autoantibody for
hepatocellular carcinoma (15),
the anti-HSP70 autoantibody for esophageal squamous cell cancer
(16) and the anti-α-enolase
autoantibody for liver fibrosis (17). Measurement of serum autoantibodies
against TAAs may not only facilitate diagnosis of GC, but also aid
the advancement of molecular targeted therapy. The present study
aimed to verify novel TAAs in the AGS GC cell line and identify
associated autoantibodies in patient sera with GC using a
proteomics method.
Materials and methods
Clinical materials and sample
preparations
All clinical samples (85 sera samples from patients
with GC and 85 sera samples from healthy control individuals) were
obtained from the sera bank at the Cancer Autoimmunity Research
Laboratory at the University of Texas (UTEP; El Paso, TX, USA). The
patients with GC were histologically diagnosed and confirmed in
accordance with the American Joint Committee on Cancer (18). Due to regulations regarding studies
on human subjects, the names of the patients were not revealed to
investigators, and some clinical information concerning sera was
not available. The present study was approved by the Institutional
Review Board of UTEP.
Cell culture and cell extracts
The AGS GC cell line was purchased from American
Type Culture Collection (Manassas, VA, USA) and was cultured in
1640-RPMI medium (Gibco; Thermo Fisher Scientific, Inc., Waltham,
MA, USA) supplemented with 10% fetal bovine serum (Gibco; Thermo
Fisher Scientific, Inc.), 100 U/ml penicillin and 100 U/ml
streptomycin. AGS cells were allowed to reach 90% confluence in
75-cm2 Falcon tissue culture flasks. Cells were rinsed
once with PBS, incubated with 1640-RPMI medium containing 25%
trypsin-EDTA (Gibco; Thermo Fisher Scientific, Inc.), and finally
placed into a 15 ml centrifuge tube.
Two-dimensional gel electrophoresis
(2-DE) analysis
AGS cells were lysed in rehydration buffer (50 nM
dithiothreitil, 8 M urea, 0.2% bio-lyte 3/10 ampholyte, 4%
3-[(3-cholamidopropyl) dimethylammonio]-1-propanesulfonate and
0.001% bromophenol blue) purchased from Bio-Rad Laboratories, Inc.
(Hercules, CA, USA), and agitated using a vortex at room
temperature for 90 min. Insoluble substances were discarded by
centrifugation at 2,922 × g at 4°C for 30 min. The resulting
supernatants were harvested, and the protein concentration was
determined using the Bradford assay (Bio-Rad Laboratories, Inc.).
For the first dimensional gel electrophoresis assay, 150 µg protein
was mixed in rehydration buffer containing bromophenol blue
reconstituted in proteomics-grade water, and electrophoresis was
performed on a pH 3–10, 7-cm isoelectric focusing (IEF) strip
(Bio-Rad Laboratories, Inc., Hercules, CA, USA). IEF was conducted
at 50 mA per gel, 250 V for 30 min, followed by 4,000 V for 1.5 h,
and 4,000 V for 5 h. Strips were instantly stored at −80°C until
required. In the second dimensional gel electrophoresis assay, 12%
SDS-PAGE gels for strips were used. Proteins from AGS cell lysates
were isolated with 2-DE and visualized by Coomassie blue (Bio-Rad
Laboratories, Inc.). To determine autoantibodies against antigens
from AGS, proteins were isolated by 2-DE, transferred onto NC
membranes for western blotting and then probed with sera from 10
patients with GC or 10 healthy controls. The protein spots were
visualized using PDQuest 2-DE analysis software version 8.0.1
(Bio-Rad Laboratories, Inc.) (19).
One- and two-dimensional western
blotting
To screen the autoantibody-positive sera, AGS cells
were lysed in rehydration buffer directly and then boiled for 10
min. After the removing of the insoluble fraction by centrifuge,
samples were loaded onto 12% SDS-PAGE gel, which is subsequently
transferred onto nitrocellulose membrane (Bio-Rad Laboratories,
Inc.) for western blotting. Following blocking with 5% non-fat milk
prepared in Tris-buffered saline (TBS), containing 0.05% Tween-20
(TBST), for 1 h at room temperature, the membrane was incubated
with sera at a solution of 1:200. Horseradish peroxidase-conjugated
goat antihuman IgG (cat. no. 31410; Invitrogen; Thermo Fisher
Scientific, Inc.) was used as secondary antibody with a dilution of
1:5,000 for 1 h at room temperature. The positive bands were
detected with an ECL kit (Thermo Fisher Scientific, Inc.). For
2D-Western blotting, the proteins on 2D gel were directly
transferred onto nitrocellulose membrane and following the same
protocol as described above.
In-gel digestion
Excised gel fragments were destained with 40 mM
NH4HCO3 in 50% acetonitrile. Reduction was
performed with 5 mM tris-2-carboxyethylphosphine hydrochloride
(Sigma-Aldrich; Merck KGaA, Darmstadt, Germany) at room temperature
for 1 h, followed by alkylation with 50 mM iodoacetamide
(Sigma-Aldrich; Merck KGaA) for 1 h at room temperature in the
dark. The dehydrated gel slices were digested with trypsin in 10 mM
NH4HCO3 for 18 h and peptide digests were
extracted using extraction buffer, which was performed in a linear
gradient from 5 to 40% solvent A to B (Solvent A: 5%
acetonitrile/0.1% formic acid, Solvent B: 80% acetonitrile/0.1%
formic acid) over 60 min at a flow rate of 30 nl/min.
Nano-liquid
chromatography-electrospray ionization-tandem mass spectrometry
(LC-ESI-MS/MS) analysis
The digests were analyzed using an Eksigent
nanoLC™-1D-plus (SCIEX, Framingham, MA, USA) coupled to a LTQ XL™
Linear Ion Trap mass spectrometer (Thermo Fisher Scientific, Inc.)
as follows: The digests were loaded onto an online dual trap set up
(Eksigent Chrom XP nanoLC trap-column C18-CL-3 µm 120 Å, 350 µm
×0.5 mm) at a flow rate of 1.5 µl/min using channel 1A solution
[98% water, 2% acetonitrile (ACN), 0.5% formic acid (FA)].
Separation was achieved on an Eksigent Chrom XP nano-LC C18-reverse
phase column (3C18-CL-3 µm 120 Å, 0.075×150 mm) using channel 2
mobile phases (solvent 2A: 5% ACN/0.1% FA; solvent 2B: 80% ACN/0.1%
FA, on a linear gradient of 5–45% 2B over 60 min at a flow rate of
300 nl/min). The MS system was set to perform one full scan
(400–1,700 m/z range) followed by MS/MS scans of the 10 most
abundant parent-ions (ESI voltage, 3 kV; isolation width, 3.0 m/z;
35 normalized collision energy). The dynamic exclusion was set to
collect each parent-ion twice and then excluded for 120 sec.
Data analysis
The resulting MS/MS spectra (350–5,000 Da,
monoisotopic) were searched against a Uniprot protein database
(http://www.uniprot.org/) downloaded on April 4,
2013 comprising Homo sapiens, Bos Taurus and porcine trypsin
using a SEQUEST® algorithm in Proteome Discoverer 1.4
software (Thermo Fisher Scientific, Inc.). The parameters for
database search were: i) 2.0 and 1.0 Da for peptide and fragment
mass tolerance, respectively; ii) full digest using trypsin after
K/R (cleaving C-terminal of K and R amino acid residues) with up to
two missed cleavages allowed; and iii) methionine oxidation as a
fixed modification, and cysteine carbamidomethylation and
deamidation of asparagine and glutamine as variable modifications.
At least 2 peptides were used for assignment of proteins and search
results were filtered for a false discovery rate of 1%, employing a
decoy search strategy utilizing a reverse database.
Recombinant proteins and
antibodies
The recombinant 14–3-3ζ protein were provided by our
laboratory (Department of Biology Sciences, UTEP; El Paso, TX, USA)
(20). Polyclonal anti-14-3-3ζ
rabbit antibody (cat. no. ab51129) was purchased from Abcam, Inc.
(Cambridge, MA, USA). Horseradish peroxidase (HRP)-conjugated goat
anti-rabbit IgG (cat. no. sc-2004) was from Santa Cruz
Biotechnology, Inc. (Dallas, TX, USA), and HRP-conjugated goat
anti-human IgG (cat. no. 31410) from Invitrogen (Thermo Fisher
Scientific, Inc.). The recombinant proteins were for ELISA and
antibodies for western blotting analysis.
ELISA
After diluting the 14–3-3ζ protein in PBS to a final
concentration of 0.5 µg/ml to coat polystyrene 96-well microtiter
plates (Thermo Fisher Scientific, Inc.), the plates were blocked
with gelatin post-coating solution at room temperature for 2 h. The
antigen-coated wells were incubated with human sera diluted at
1:100 with serum diluent (875 ml ddH2O, 100 ml gelatin
at 10 mg/ml, 20 ml 0.5 M phosphate buffer, 8.2 g NaCl, 0.1 g
Thimerosal, 5 g bovine gamma globulin, 1 g bovine serum albumin and
5 ml 10%-Tween-20) at room temperature for 2 h. The final
reactivity was detected using goat anti-human IgG-HRP and the
substrate 2,2′-azino-bis-(3-ethylbenzo-thiazoline-6-sulfonic acid)
(Invitrogen; Thermo Fisher Scientific, Inc.) (17). Data were analyzed by measuring the
average optical density (OD) value at a wavelength of 405 nm. The
cut-off value, which indicated a positive reaction, was the mean OD
of 85 normal human sera (NHS) + 3 standard deviations.
Statistical analysis
Statistical analysis was conducted using SPSS
software version 21.0 (IBM Corp., Armonk, NY, USA). Data were
assessed by χ2 test and ELISA data are presented as the
mean ± 3 standard deviations. P<0.01 was considered to indicate
a statistically significant difference.
Results
Identification of immunoreactive
proteins in GC cells by LC-MS/MS
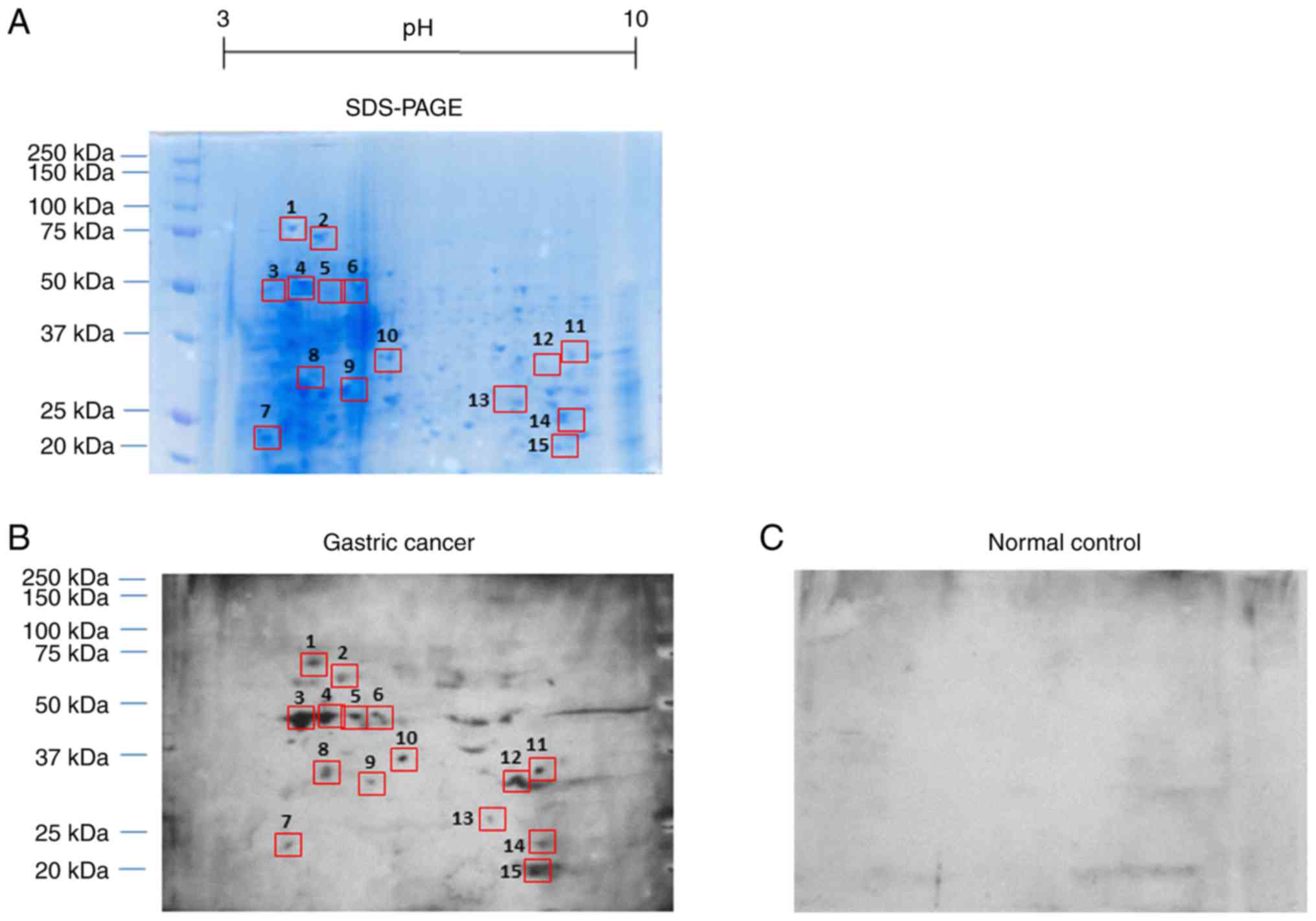
Proteins from AGS cell lysates were isolated with
2-DE and visualized by Coomassie blue staining (Fig. 1A). To determine autoantibodies
against antigens from AGS, proteins were isolated by 2-DE,
transferred onto NC membranes and then probed with sera from 10
patients with GC or 10 healthy controls. These sera were randomly
chosen in both groups. Each NC membrane was incubated with mixed
sera samples as the primary antibody, followed by an HRP-conjugated
goat anti-human IgG as a secondary antibody. The reactivity of
patients' sera with GC resulted in 15 spots (Fig. 1B), whereas no reactive protein
spots were observed in the normal control samples (Fig. 1C). Therefore, the sera were
considered to have non-specific reactivity. In the subsequent
study, 15 immunoreactive protein spots were excised from the
SDS-PAGE gels, digested with trypsin and further analyzed by
LC-MS/MS. The resulting MS/MS spectra were searched with a Uniprot
protein database, which is a comprehensive database for human
protein sequences. As demonstrated in Table I, 14 of the 15 protein spots were
identified by LC-MS/MS, with the exception of one uncharacteristic
protein.
 | Table I.Summary of identified protein spots
by mass spectrometry. |
Table I.
Summary of identified protein spots
by mass spectrometry.
| Spot no. | Accession no. | Identified
protein | Molecular mass
(kDa) | Protein
abundance | Protein
functions |
|---|
| 1 | P11021 | GRP78 | 78 | 56 | Interacts with many
endoplasmic reticulum protein and monitors transport through the
cell |
| 2 | B1AHM1 | DEAD
(Asp-Glu-Ala-Asp) box polypeptide 17 | 72.5 | 35 | Implicated in a
number of cellular processes involving alteration of RNA secondary
structure |
| 3 | Q53G71 | Calreticulin
variant | 46.9 | 30 | Acts as a major
Ca2+-binding protein in the lumen of the endoplasmic
reticulum |
| 4 | Q53G71 | Calreticulin
variant | 46.9 | 17 | Acts as a major
Ca2+-binding protein in the lumen of the endoplasmic
reticulum |
| 5 | Q53G71 | Calreticulin
variant | 46.9 | 21 | Acts as a major
Ca2+-binding protein in the lumen of the endoplasmic
reticulum |
| 6 | Q53G71 | Calreticulin
variant | 46.9 | 42 | Acts as a major
Ca2+-binding protein in the lumen of the endoplasmic
reticulum |
| 7 | P62820 | Ras-related protein
Rab-1A | 22.7 | 61 | Controls vesicle
traffic from the endoplasmic reticulum to the Golgi apparatus |
| 8 | B4E3C4 | Uncharacterized
protein | 33.8 | 5 | – |
| 9 | E7EUT4 |
Glyceraldehyde-3-phosphate
dehydrogenase | 31.5 | 59 | Serves a role in
glycolysis and nuclear functions |
| 10 | B4DVQ0 | Actin | 37.3 | 14 | Involved in various
types of cell motility |
| 11 | P22626 | hnRNP A2/B1 | 37.4 | 17 | Serves an important
role in proliferation |
| 12 | Q1WWK5 | SEPT9 protein | 36.5 | 9 | Is overexpressed in
diverse human tumors |
| 13 | P63104 | 14-3-3 protein
zeta | 27.7 | 45 | Mediates signal
transduction by binding to phosphoserine-containing proteins |
| 14 | Q06830 |
Peroxiredoxin-1 | 23 | 55 | Serves a role in
cancer development or progression |
| 15 | P30086 | PEBP | 21 | 2 | Interacts with
MAP2K1, c-Raf and MAPK1 |
Prevalence and autoantibody titers
against 14–3-3ζ in GC
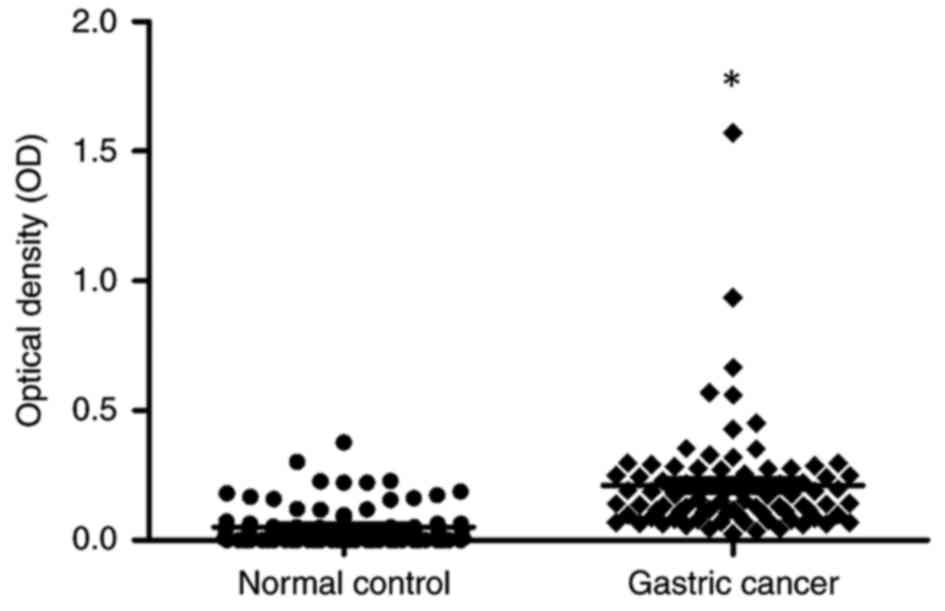
Sera from patients with GC and normal controls were
tested for the response of autoantibodies to 14-3-3ζ. The sera that
were detected included 85 from patients with GC, and 85 from normal
human individuals. Table II
revealed that autoantibody frequency to 14-3-3ζ was 17.6% (15/85)
in GC sera, which was significantly higher than that in NHS (2.4%;
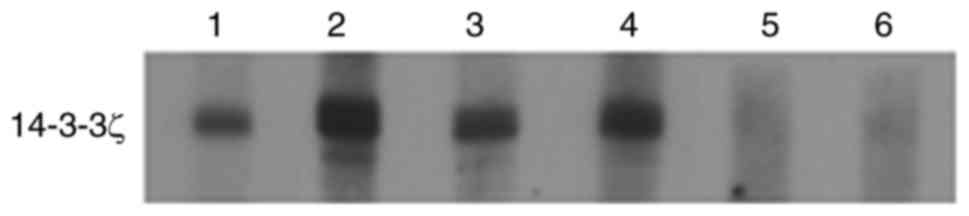
2/85; P<0.01). In addition, as presented in Fig. 2, autoantibody titers against
14-3-3ζ in GC sera were higher than in NHS (P<0.01). These ELISA
results were further confirmed by western blot analysis (Fig. 3), where a positive reaction to
14-3-3ζ was observed in representative GC sera compared with normal
sera.
 | Table II.Frequency of autoantibodies against
14-3-3ζ in human sera, as determined by ELISA. |
Table II.
Frequency of autoantibodies against
14-3-3ζ in human sera, as determined by ELISA.
| Type of sera | No. tested | Autoantibody to
14-3-3ζ (%) |
|---|
| GC | 85 | 15
(17.6)a |
| NHS | 85 | 2 (2.4) |
Discussion
The recognition of TAAs that evoke an antibody
response may be utilized for the early diagnosis of cancer, in
monitoring prognosis and as immunotherapy targets (21,22).
With advancement in protein isolation and identification methods,
proteomics-based technologies have acquired increased popularity
for the detection and recognition of TAAs and associated
autoantibodies. Thus, 2-D/MS remains a key technique in proteomics
for global protein profiling and serves a complementary role to
LC-MS-based analysis (23). In
addition, it enables experiments to be performed with
autoantibodies, and therefore improves screening of antigenicity
associated with abnormal post-translational alterations of cancer
cell proteins.
Proteomics techniques have been adopted to explore
protein expression in various human cancers. The most widely used
technique for large-scale protein expression detection is 2-DE
combined with MS, which may be an optimal method in the pursuit of
reliable immunodiagnostic biomarkers. With this proteomic
technique, autoantibodies against annexin-II (24), annexin-I, protein gene product 9.5
(25), peroxiredoxin-I (26), calreticulin (27), peroxiredoxin-VI (28) and RS/DJ-1 (29), have been identified in the sera of
patients with pancreatic, lung, esophageal squamous cell and breast
cancers.
In the present study, an immunoproteomics-based
approach was used to identify biomarkers associated with the
humoral immune responses in patients with GC. This approach
incorporated SDS-PAGE, 2-DE and western blotting to detect
autoantibodies in sera from patients with GC, which reacted to
proteins separated by 2-DE and were confirmed by MS. In total, 11
available proteins were identified. One of them, glucose-regulated
protein 78 (GRP78), has been regarded as a diagnostic biomarker for
GC (30). Two other proteins,
actin and GAPDH, are housekeeping proteins. Therefore, the 8
remaining tumor-associated proteins may be considered candidate
antigens.
The molecular functions of the identified proteins
have been documented in the literature, and the majority of these
proteins are associated with various cellular functions, including
cell differentiation, proliferation, apoptosis and signaling
transduction. To further investigate the association of these
identified proteins with cancer, literature searches were conducted
using PubMed (http://www.ncbi.nlm.nih.gov/pubmed/). GRP78 is a
molecular chaperone in the endoplasmic reticulum (ER), which may be
a candidate biomarker in GC (30).
DEAD-box helicase 3 X-linked (DDX3X) is a hepatitis C virus core
protein-associated cellular factor that belongs to the DEAD box RNA
helicase family (31–33). Whole-exome analyses have revealed
that mutated DDX3X serves an essential role in oncogenesis
(34). Calreticulin is also an ER
chaperone, which serves a role as a stress protein. Overexpression
of calreticulin occurs in numerous malignancies, including in
cancers of the prostate, breast, bladder, liver and lung (35–38).
Rab-1A, which is a Ras-associated protein, may be of pathological
significance in dealing with glucocorticoid-induced osteoporosis
(39). GAPDH and actin have
various functions in cells, in particular, they serve a vital role
in the control of gene expression. Heterogeneous nuclear
ribonucleoprotein A2/B1 (hnRNP A2/B1) is a member of the hnRNP A/B
family that may be considered a prognostic marker of hepatocellular
carcinoma (40). Septin 9, which
is a cytoskeletal component, has been recognized as a promising
oncogene in breast tumorigenesis (41). 14-3-3ζ is a member of a family of
seven highly conserved proteins that is considered a novel
predictive biomarker of tamoxifen therapeutic resistance in breast
cancer (42,43). Peroxiredoxin-1 is a member of the
peroxiredoxin family of antioxidant enzymes and may be a potential
biomarker for screening patients with hepatocellular carcinoma
(44).
Phosphatidylethanolamine-binding protein is regarded as a signal
transduction mediator and a suppression of metastasis in cancer,
and is often downregulated in various human malignancies (45), primarily in highly metastatic
cancers (46–50). However, the present study focused
on the 14-3-3ζ protein to identify whether this antigen may be
considered a tumor biomarker in the immunodiagnosis of GC. As these
identified proteins are associated with cancer, future work to
evaluate which of these may be attractive TAAs in GC is
required.
The 14-3-3 proteins are highly conserved regulatory
molecules that are universally expressed in all eukaryotic
organisms (51). In humans, seven
isoforms of 14-3-3 (β, ε, η, γ, τ, ζ and σ) have been verified
(52). Although 14-3-3 proteins
are short of endogenous enzymatic activity, they function by
forming homo- or hetero-dimers and binding to
phosphorylated-serine/threonine motifs on their target proteins
(53). By modulation of their
binding cooperators, 14-3-3 proteins have been implicated to
regulate a mass of cellular processes, including mitogenesis,
apoptosis, cell cycle progression, stress signaling, metabolism,
cytoskeletal integrity and transcription (54,55).
Numerous studies have reported that members of the 14-3-3 family,
particularly 14-3-3ζ, serve a pro-oncogenic role in various tumor
types, and overexpression of 14-3-3ζ is primarily associated with
poor survival of patients with cancer (56,57).
14-3-3ζ has been recognized as a clinically relevant prognostic
marker for lung cancer, breast cancer, and head and neck cancer
(58–60). The present study identified 14-3-3ζ
as a candidate biomarker for GC and determined autoantibodies
against 14-3-3ζ by ELISA and western blot analysis. It was
demonstrated that serum autoantibody prevalence to 14-3-3ζ was
significantly stronger in patients with GC (17.6%) than in normal
individuals (2.4%). Intensive studies are required to assess the
sensitivity and specificity of autoantibodies against 14-3-3ζ in a
greater number of samples, and to explore the underlying molecular
mechanism of autoantibody response to 14-3-3ζ in the progression of
GC.
14-3-3 proteins are generally cytosolic but also
bind to several nuclear proteins; therefore, it is hypothesized
that they may serve as a cytoplasmic anchor and block nuclear
import of target proteins (61).
Several proteins whose nuclear trafficking is regulated by 14-3-3
include a bipartite nuclear localization signal (NLS). 14-3-3
binding masks the NLS and displaces the import complex, which leads
to the cytoplasmic localization of target proteins (61). 14-3-3 proteins do not have any
catalytic activity; however, they exert their effect by modulating
subcellular localization or catalytic activity of target proteins
and by regulating formation of protein complexes (62). 14-3-3 proteins interact with
several proteins that potentially mediate various cellular
processes (63,64). Therefore, 14-3-3ζ may bind several
proteins and potentially mediate the protein complex involved in
numerous biological functions and tumor progression.
In conclusion, the present study detected
autoantibodies against 14-3-3ζ in sera from patients with GC.
14-3-3ζ may be attractive not only as a serological tumor
biomarker, but also to guide efficient immunological surveillance.
With regards to the detection of novel autoantibodies, including
14-3-3ζ, the proteomics approach employed in the present study may
be considered a promising method to identify potential proteins
that have clinical utility in malignancy.
Acknowledgements
The present study was supported by grants from the
Project for Tackling Key Problems in Science and Technology of
Henan province (grant no. 162102410044), the Major project of
Science and Technology in Henan province (grant no. 161100311400),
the Zhongyuan Scholar Program of Henan Province (grant no.
162101510006) and the Key Scientific Research Project of Henan
Province (grant no. 16A330007).
References
|
1
|
Bertuccio P, Chatenoud L, Levi F, Praud D,
Ferlay J, Negri E, Malvezzi M and La Vecchia C: Recent patterns in
gastric cancer: A global overview. Int J Cancer. 125:666–673. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Peleteiro B, Bastos A, Ferro A and Lunet
N: Prevalence of helicobacter pylori infection worldwide: A
systematic review of studies with national coverage. Dig Dis Sci.
59:1698–1709. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kamangar F, Dores GM and Anderson WF:
Patterns of cancer incidence, mortality, and prevalence across five
continents: Defining priorities to reduce cancer disparities in
different geographic regions of the world. J Clin Oncol.
24:2137–2150. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hiripi E, Jansen L, Gondos A, Emrich K,
Holleczek B, Katalinic A, Luttmann S, Nennecke A and Brenner H:
Gekid Cancer Survival Working Group: Survival of stomach and
esophagus cancer patients in Germany in the early 21st century.
Acta Oncol. 51:906–914. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hundahl SA, Phillips JL and Menck HR: The
National Cancer Data Base Report on poor survival of U.S. gastric
carcinoma patients treated with gastrectomy: Fifth Edition American
Joint Committee on Cancer staging, proximal disease, and the
‘different disease’ hypothesis. Cancer. 88:921–932. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ushijima T and Sasako M: Focus on gastric
cancer. Cancer Cell. 5:121–125. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Srinivas PR, Kramer BS and Srivastava S:
Trends in biomarker research for cancer detection. Lancet Oncol.
2:698–704. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Tan HT, Low J, Lim SG and Chung MC: Serum
autoantibodies as biomarkers for early cancer detection. FEBS J.
276:6880–6904. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Anderson KS and LaBaer J: The sentinel
within: Exploiting the immune system for cancer biomarkers. J
Proteome Res. 4:1123–1133. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Caron M, Choquet-Kastylevsky G and
Joubert-Caron R: Cancer immunomics using autoantibody signatures
for biomarker discovery. Mol Cell Proteomics. 6:1115–1122. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Casiano CA, Mediavilla-Varela M and Tan
EM: Tumor-associated antigen arrays for the serological diagnosis
of cancer. Mol Cell Proteomics. 5:1745–1759. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Fernandez Madrid F: Autoantibodies in
breast cancer sera: Candidate biomarkers and reporters of
tumorigenesis. Cancer Lett. 230:187–198. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Tan EM: Autoantibodies as reporters
identifying aberrant cellular mechanisms in tumorigenesis. J Clin
Invest. 108:1411–1415. 2001. View
Article : Google Scholar : PubMed/NCBI
|
|
14
|
Davis MA and Hanash S: High-throughput
genomic technology in research and clinical management of breast
cancer. Plasma-based proteomics in early detection and therapy.
Breast Cancer Res. 8:2172006. View
Article : Google Scholar : PubMed/NCBI
|
|
15
|
Looi KS, Nakayasu ES, Diaz RA, Tan EM,
Almeida IC and Zhang JY: Using proteomic approach to identify
tumor-associated antigens as markers in hepatocellular carcinoma. J
Proteome Res. 7:4004–4012. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhang J, Wang K, Zhang J, Liu SS, Dai L
and Zhang JY: Using proteomic approach to identify tumor-associated
proteins as biomarkers in human esophageal squamous cell carcinoma.
J Proteome Res. 10:2863–2872. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Peng B, Huang X, Nakayasu ES, Petersen JR,
Qiu S, Almeida IC and Zhang JY: Using immunoproteomics to identify
alpha-enolase as an autoantigen in liver fibrosis. J Proteome Res.
12:1789–1796. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yegin EG and Duman DG: Staging of
esophageal and gastric cancer in 2014. Minerva Med. 105:391–411.
2014.PubMed/NCBI
|
|
19
|
Jung E, Heller M, Sanchez JC and
Hochstrasser DF: Proteomics meets cell biology: The establishment
of subcellular proteomes. Electrophoresis. 21:3369–3377. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Dai L, Tsay JC, Li J, Yie TA, Munger JS,
Pass H, Rom WN, Zhang Y, Tan EM and Zhang JY: Autoantibodies
against tumor-associated antigens in the early detection of lung
cancer. Lung Cancer. 99:172–179. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Fernandez-Madrid F, Tang N, Alansari H,
Granda JL, Tait L, Amirikia KC, Moroianu M, Wang X and Karvonen RL:
Autoantibodies to Annexin XI-A and other autoantigens in the
diagnosis of breast cancer. Cancer Res. 64:5089–5096. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kim JH, Herlyn D, Wong KK, Park DC,
Schorge JO, Lu KH, Skates SJ, Cramer DW, Berkowitz RS and Mok SC:
Identification of epithelial cell adhesion molecule autoantibody in
patients with ovarian cancer. Clin Cancer Res. 9:4782–4791.
2003.PubMed/NCBI
|
|
23
|
Timms JF and Cramer R: Difference gel
electrophoresis. Proteomics. 8:4886–4897. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Brichory FM, Misek DE, Yim AM, Krause MC,
Giordano TJ, Beer DG and Hanash SM: An immune response manifested
by the common occurrence of annexins I and II autoantibodies and
high circulating levels of IL-6 in lung cancer. Proc Natl Acad Sci
USA. 98:9824–9829. 2001; View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Brichory F, Beer D, Le Naour F, Giordano T
and Hanash S: Proteomics-based identification of protein gene
product 9.5 as a tumor antigen that induces a humoral immune
response in lung cancer. Cancer Res. 61:7908–7912. 2001.PubMed/NCBI
|
|
26
|
Chang JW, Lee SH, Jeong JY, Chae HZ, Kim
YC, Park ZY and Yoo YJ: Peroxiredoxin-I is an autoimmunogenic tumor
antigen in non-small cell lung cancer. FEBS Lett. 579:2873–2877.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Hong SH, Misek DE, Wang H, Puravs E,
Giordano TJ, Greenson JK, Brenner DE, Simeone DM, Logsdon CD and
Hanash SM: An autoantibody-mediated immune response to calreticulin
isoforms in pancreatic cancer. Cancer Res. 64:5504–5510. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Fujita Y, Nakanishi T, Hiramatsu M,
Mabuchi H, Miyamoto Y, Miyamoto A, Shimizu A and Tanigawa N:
Proteomics-based approach identifying autoantibody against
peroxiredoxin VI as a novel serum marker in esophageal squamous
cell carcinoma. Clin Cancer Res. 12:6415–6420. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Le Naour F, Misek DE, Krause MC, Deneux L,
Giordano TJ, Scholl S and Hanash SM: Proteomics-based
identification of RS/DJ-1 as a novel circulating tumor antigen in
breast cancer. Clin Cancer Res. 7:3328–3335. 2001.PubMed/NCBI
|
|
30
|
Wu JY, Cheng CC, Wang JY, Wu DC, Hsieh JS,
Lee SC and Wang WM: Discovery of tumor markers for gastric cancer
by proteomics. PLoS One. 9:e841582014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
You LR, Chen CM, Yeh TS, Tsai TY, Mai RT,
Lin CH and Lee YH: Hepatitis C virus core protein interacts with
cellular putative RNA helicase. J Virol. 73:2841–2853.
1999.PubMed/NCBI
|
|
32
|
Owsianka AM and Patel AH: Hepatitis C
virus core protein interacts with a human DEAD box protein DDX3.
Virology. 257:330–340. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Mamiya N and Worman HJ: Hepatitis C virus
core protein binds to a DEAD box RNA helicase. J Biol Chem.
274:15751–15756. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Pugh TJ, Weeraratne SD, Archer TC, Krummel
DA Pomeranz, Auclair D, Bochicchio J, Carneiro MO, Carter SL,
Cibulskis K, Erlich RL, et al: Medulloblastoma exome sequencing
uncovers subtype-specific somatic mutations. Nature. 488:106–110.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Alur M, Nguyen MM, Eggener SE, Jiang F,
Dadras SS, Stern J, Kimm S, Roehl K, Kozlowski J, Pins M, et al:
Suppressive roles of calreticulin in prostate cancer growth and
metastasis. Am J Pathol. 175:882–890. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Chignard N, Shang S, Wang H, Marrero J,
Bréchot C, Hanash S and Beretta L: Cleavage of endoplasmic
reticulum proteins in hepatocellular carcinoma: Detection of
generated fragments in patient sera. Gastroenterology.
130:2010–2022. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Gromov P, Gromova I, Bunkenborg J, Cabezon
T, Moreira JM, Timmermans-Wielenga V, Roepstorff P, Rank F and
Celis JE: Up-regulated proteins in the fluid bathing the tumour
cell microenvironment as potential serological markers for early
detection of cancer of the breast. Mol Oncol. 4:65–89. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Iwaki H, Kageyama S, Isono T, Wakabayashi
Y, Okada Y, Yoshimura K, Terai A, Arai Y, Iwamura H, Kawakita M and
Yoshiki T: Diagnostic potential in bladder cancer of a panel of
tumor markers (calreticulin, gamma-synuclein, and
catechol-o-methyltransferase) identified by proteomic analysis.
Cancer Sci. 95:955–961. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Hong D, Chen HX, Yu HQ, Wang C, Deng HT,
Lian QQ and Ge RS: Quantitative proteomic analysis of
dexamethasone-induced effects on osteoblast differentiation,
proliferation, and apoptosis in MC3T3-E1 cells using SILAC.
Osteoporos Int. 22:2175–2186. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Mizuno H, Honda M, Shirasaki T, Yamashita
T, Yamashita T, Mizukoshi E and Kaneko S: Heterogeneous nuclear
ribonucleoprotein A2/B1 in association with hTERT is a potential
biomarker for hepatocellular carcinoma. Liver Int. 32:1146–1155.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Montagna C, Lyu MS, Hunter K, Lukes L,
Lowther W, Reppert T, Hissong B, Weaver Z and Ried T: The Septin 9
(MSF) gene is amplified and overexpressed in mouse mammary gland
adenocarcinomas and human breast cancer cell lines. Cancer Res.
63:2179–2187. 2003.PubMed/NCBI
|
|
42
|
Bergamaschi A, Christensen BL and
Katzenellenbogen BS: Reversal of endocrine resistance in breast
cancer: Interrelationships among 14-3-3ζ, FOXM1, and a gene
signature associated with mitosis. Breast Cancer Res. 13:R702011.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Frasor J, Chang EC, Komm B, Lin CY, Vega
VB, Liu ET, Miller LD, Smeds J, Bergh J and Katzenellenbogen BS:
Gene expression preferentially regulated by tamoxifen in breast
cancer cells and correlations with clinical outcome. Cancer Res.
66:7334–7340. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Sun QK, Zhu JY, Wang W, Lv Y, Zhou HC, Yu
JH, Xu GL, Ma JL, Zhong W and Jia WD: Diagnostic and prognostic
significance of peroxiredoxin 1 expression in human hepatocellular
carcinoma. Med Oncol. 31:7862014. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Granovsky AE and Rosner MR: Raf kinase
inhibitory protein: A signal transduction modulator and metastasis
suppressor. Cell Res. 18:452–457. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Akaishi J, Onda M, Asaka S, Okamoto J,
Miyamoto S, Nagahama M, Ito K, Kawanami O and Shimizu K:
Growth-suppressive function of phosphatidylethanolamine-binding
protein in anaplastic thyroid cancer. Anticancer Res. 26:4437–4442.
2006.PubMed/NCBI
|
|
47
|
Houben R, Michel B, Vetter-Kauczok CS,
Pföhler C, Laetsch B, Wolter MD, Leonard JH, Trefzer U, Ugurel S,
Schrama D and Becker JC: Absence of classical MAP kinase pathway
signalling in Merkel cell carcinoma. J Invest Dermatol.
126:1135–1142. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Chen Y, Ouyang GL, Yi H, Li MY, Zhang PF,
Li C, Li JL, Liu YF, Chen ZC and Xiao ZQ: Identification of RKIP as
an invasion suppressor protein in nasopharyngeal carcinoma by
proteomic analysis. J Proteome Res. 7:5254–5262. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Fu Z, Smith PC, Zhang L, Rubin MA, Dunn
RL, Yao Z and Keller ET: Effects of raf kinase inhibitor protein
expression on suppression of prostate cancer metastasis. J Natl
Cancer Inst. 95:878–889. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Chatterjee D, Bai Y, Wang Z, Beach S, Mott
S, Roy R, Braastad C, Sun Y, Mukhopadhyay A, Aggarwal BB, et al:
RKIP sensitizes prostate and breast cancer cells to drug-induced
apoptosis. J Biol Chem. 279:17515–17523. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Aitken A: 14-3-3 proteins on the MAP.
Trends Biochem Sci. 20:95–97. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Aitken A: 14-3-3 proteins: A historic
overview. Semin Cancer Biol. 16:162–172. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Muslin AJ, Tanner JW, Allen PM and Shaw
AS: Interaction of 14-3-3 with signaling proteins is mediated by
the recognition of phosphoserine. Cell. 84:889–897. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
54
|
van Hemert MJ, Steensma HY and van Heusden
GP: 14-3-3 proteins: key regulators of cell division, signalling
and apoptosis. Bioessays. 23:936–946. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Tzivion G, Gupta VS, Kaplun L and Balan V:
14-3-3 proteins as potential oncogenes. Semin Cancer Biol.
16:203–213. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Zhao J, Meyerkord CL, Du Y, Khuri FR and
Fu H: 14-3-3 proteins as potential therapeutic targets. Semin Cell
Dev Biol. 22:705–712. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Neal CL and Yu D: 14-3-3ζ as a prognostic
marker and therapeutic target for cancer. Expert Opin Ther Targets.
14:1343–1354. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Lu J, Guo H, Treekitkarnmongkol W, Li P,
Zhang J, Shi B, Ling C, Zhou X, Chen T, Chiao PJ, et al: 14-3-3zeta
Cooperates with ErbB2 to promote ductal carcinoma in situ
progression to invasive breast cancer by inducing
epithelial-mesenchymal transition. Cancer cell. 16:195–207. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Matta A, DeSouza LV, Shukla NK, Gupta SD,
Ralhan R and Siu KW: Prognostic significance of head-and-neck
cancer biomarkers previously discovered and identified using
iTRAQ-labeling and multidimensional liquid chromatography-tandem
mass spectrometry. J Proteome Res. 7:2078–2087. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Fan T, Li R, Todd NW, Qiu Q, Fang HB, Wang
H, Shen J, Zhao RY, Caraway NP, Katz RL, et al: Up-regulation of
14-3-3zeta in lung cancer and its implication as prognostic and
therapeutic target. Cancer Res. 67:7901–7906. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Muslin AJ and Xing H: 14-3-3 proteins:
Regulation of subcellular localization by molecular interference.
Cell Signal. 12:703–709. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Tzivion G and Avruch J: 14-3-3 proteins:
Active cofactors in cellular regulation by serine/threonine
phosphorylation. J Biol Chem. 277:3061–3064. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Benzinger A, Muster N, Koch HB, Yates JR
III and Hermeking H: Targeted proteomic analysis of 14-3-3 sigma, a
p53 effector commonly silenced in cancer. Mol Cell Proteomics.
4:785–795. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Jin J, Smith FD, Stark C, Wells CD,
Fawcett JP, Kulkarni S, Metalnikov P, O'Donnell P, Taylor P, Taylor
L, et al: Proteomic, functional, and domain-based analysis of in
vivo 14-3-3 binding proteins involved in cytoskeletal regulation
and cellular organization. Curr Biol. 14:1436–1450. 2004.
View Article : Google Scholar : PubMed/NCBI
|