Introduction
Non-small cell lung cancer (NSCLC) is the most
common histological type of lung cancer, accounting for about
80–85% of total lung cancer. In recent years, the incidence of
NSCLC continues to increase and has become the highest lethal rate
of cancer all over the world (1).
The application of epidermal growth factor receptor tyrosine kinase
inhibitors (EGFR-TKIs), such as gefitinib, has improved the
treatment of NSCLC (2). Detection
of sensitive mutations to EGFR-TKIs has stimulated the interest in
studying multiple oncogenic drivers. Previous results suggested
that somatic mutations in EGFR, KRAS, BRAF, NRAS, PIK3CA,
Her-2 and TP53 have been associated with efficacy of
EGFR-TKIs, metastasis or overall survival (3–6).
Therefore, molecular assays of EGFR, KRAS, BRAF, NRAS,
PIK3CA and Her-2 are widely used to guide individualized
treatment in NSCLC patients.
Commonly used technologies for oncogenic driver
detection include direct sequencing, next-generation sequencing
(NGS), amplification refractory mutation system (ARMS) and droplet
digital PCR (ddPCR). Sanger sequencing is used as standard for
detecting EGFR mutations because of accurate results and low
throughput. However, it is limited by high cost, time consuming and
low sensitivity, for detecting low frequency mutant alleles in a
specimen mixed with normal alleles. ddPCR is a new generation of
absolute quantification PCR technique, realizing the independent
amplification and fluorescence reading of thousands of individual
droplets in one well. It has an extremely high sensitivity
(0.04%-0.1%) and each well can only detect one site, limiting its
use in multiple assays (7). Next
Generation Sequencing (NGS) is a method that can detect multiple
genetic variations simultaneously and can detect tumor mutations
efficiently and economically. The scientists had a blinded
comparison of NGS and quantitative real-time PCR (qPCR) assays to
detect mutations in EGFR, KRAS, PIK3CA and BRAF in Chinese patients
with NSCLC. Sanger sequencing was used to verify the inconsistent
results of qPCR and NGS assays. The high consistency between NGS
and qPCR has shown clinical application prospects of NGS (8).
In the present study, we detect somatic mutations in
NSCLC by a small panel including 7 genes using the Iontorrent
personal genome machine (PGM), to evaluate the efficacy of NGS by
comparison to ddPCR assay and Sanger sequencing.
Patients and methods
Patient characteristics
Non-small lung tumor tissues were obtained from 112
Chinese patients in Jiangsu Cancer Hospital (Nanjing, China)
between June 2015 and June 2016. Clinical characteristics of all
patients were recorded with detailed information summarized in
Table I. The histological
diagnosis of all samples was confirmed by the pathologists. TNM
classification of malignant tumors was used to determine tumor
stage. All patients participated in the study signed informed
consent. The ethics approval was awarded by the Cancer Institute of
Jiangsu Province Ethics Committee.
 | Table I.Patient characteristics (n=112). |
Table I.
Patient characteristics (n=112).
| Variables | Number of
patients |
|---|
| Sex |
|
|
Male | 67 |
|
Female | 45 |
| Age |
|
| <60
years | 35 |
| ≥60
years | 77 |
| Histological
type |
|
|
Adenocarcinoma | 82 |
|
Squamous cell carcinoma | 24 |
|
Adenosquamous carcinoma | 1 |
|
Others | 5 |
| Histopathological
grading |
|
|
High-median | 33 |
|
Low | 79 |
| TNM staging |
|
|
I–II | 34 |
|
III–IV | 78 |
DNA extraction from formalin-fixed
paraffin-embedded (FFPE) tissue
Tumor-rich samples were obtained when the patient
underwent surgery. DNA was extracted with DNA FFPE tissue kit
(Omega, Norcross, GA, USA) according to the guidebook and the
concentrations were detected by Qubit® 2.0 fluorometer
dsDNA HS assay kit (Thermo Fisher Scientific, Inc., Waltham, MA,
USA).
Mutation analysis by NGS
The Lung panel (including BRAF, EGFR, KRAS, NRAS,
PIK3CA, Her-2 and TP53) on Iontorrent system was
generally provided by Thermo Fisher Scientific, Inc. DNA was
extracted and purified after microdissection using
Agencourt® AMPure™ XP beads (Beckman Coulter,
Brea, CA, USA). After DNA concentration detection, 15 ng of DNA was
then amplified, fragmented, ligated to adapters, barcoded, and
clonally amplified onto beads to create DNA libraries, using
Iontorrent ampliSeq kit 2.0 and IonXpress barcode adapters kit
(Thermo Fisher Scientific, Inc.) by user guidebook. After
quantification, library mixtures were amplified with Iontorrent
Onetouch template kit (Thermo Fisher Scientific, Inc.) and enriched
on Iontorrent Onetouch system according to the protocol. Finally,
the library pool was sequenced with Iontorrent PGM sequencing
supplies 200 v2 kit (Thermo Fisher Scientific, Inc.) using
Iontorrent PGM system. The mutation site was analyzed by the
Iontorrent variant caller plugin v4.0 according to the reference
genome hg19. The threshold of mutation frequency for mutation was
1%. The overall median coverage of depth was >1000X. The
sequencing coverage of amplicons is >1,000 and the uniformity
was >90%.
Sanger sequencing
Firstly, PCR was performed in a PCR Amplifier
(Biometra, GmbH, Göttingen, Germany) for Sanger sequencing. Primers
used for exon 18–21 of EGFR were listed in Table II. Secondly, PCR products were
purified by Axyprep™ PCR cleanup kit (Axygen, Hangzhou,
China). Thirdly, sequencing reaction was performed with big dye
terminator v3.1 (Thermo Fisher Scientific, Inc.). Finally, the
products were denatured and analysed by a DNA sequencer (Applied
Biosystems 3500; Thermo Fisher Scientific, Inc.). Sequencing
analysis v5.4 software was used to analyze the results.
 | Table II.Primers for direct sequencing. |
Table II.
Primers for direct sequencing.
| Exon | Primer name | Sequence |
|---|
| 18 | EGFR 18S F |
5′-AGCATGGTGAGGGCTGAGGTGAC-3′ |
|
| EGFR 18S R |
5′-ATATACAGCTTGCAAGGACTCTGG-3′ |
| 19 | EGFR 19S F |
5′-CCAGATCACTGGGCAGCATGTGGCACC-3′ |
|
| EGFR 19S R |
5′-AGCAGGGTCTAGAGCAGAGCAGCTGCC-3 |
| 20 | EGFR 20S F |
5′-GATCGCATTCATGCGTCTTCACC-3′ |
|
| EGFR 20S R |
5′-TTGCTATCCCAGGAGCGCAGACC-3′ |
| 21 | EGFR 21S F |
5′-TCAGAGCCTGGCATGAACATGACCCTG-3′ |
|
| EGFR 21S R |
5′-GGTCCCTGGTGTCAGGAAAATGCTGG-3′ |
Droplet digtal PCR
Genotypes with L858R, exon 19 deletion, T790M or
G719S were conducted by ddPCR. 20 µl of PCR reaction mixtures were
prepared. After droplets generation, the products were shifted to a
96-well plate for amplification. The amplified products were
analyzed on QX200™ Droplet Digital™ PCR (BioRad
Laboratories, Inc., Hercules, CA, USA). The samples which contained
at least 2 droplets in the FAM positive area were called
positive.
Statistical analysis
The ability of NGS and ddPCR platforms to detect
EGFR mutations was analyzed using χ2 test with IBM SPSS
Statistics for Windows (v19.0. IBM Corp., Armonk, NY, USA).
P<0.05 represents statistically significant differences. All
figures were produced with GraphPad Prism (v6.0; GraphPad Software,
Inc., La Jolla, CA, USA).
Results
The patient mutation profile
There were 86 FFPE specimens, 26 fresh resection
specimens, 13 fine needle aspiration specimens and 4 pleural
effusion specimens. Finally, 17 specimens failed to pass quality
control. The remaining 112 specimens were successful submitted to
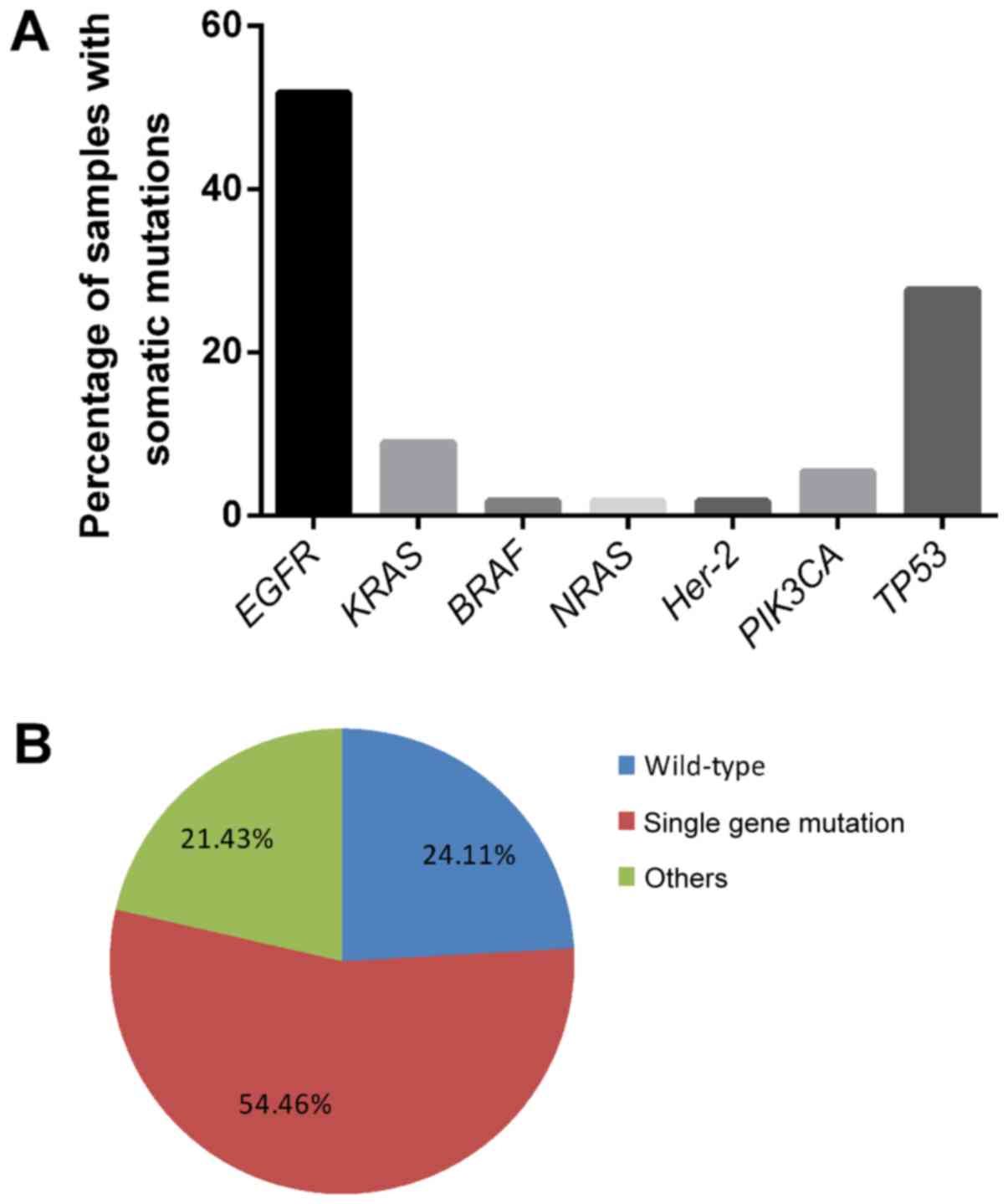
NGS. As shown in Fig. 1A,
mutations were detected in EGFR (58/112, 51.79% of tumors),
KRAS (10/112, 8.93%), BRAF (2/112, 1.79%),
NRAS (2/112, 1.79%), Her-2 (2/112, 1.79%),
PIK3CA (6/112, 5.36%) and TP53 (31/112, 27.69%).
Fig. 1B showed that there were 27
samples without any somatic mutations in all genes while 24 samples
harboured mutations in two or more genes. 61 samples had mutations
in single gene. Concomitant EGFR and TP53 mutations
accounted for 54.17% (13/24) of samples with multiply gene
mutations including two specimens with triple gene alterations
(EGFR, KRAS, TP53/EGFR, PIK3CA, TP53). There were 3
samples occupied KRAS and TP53 mutations. Concomitant
TP53 and PIK3CA mutations occurred in 2 NSCLC
patients. Doublet mutations of EGFR and PIK3CA, EGFR
and KRAS, EGFR and NRAS, EGFR and Her-2, BRAF
and TP53, BRAF and PIK3CA occurred in 1 NSCLC
each.
Genetic alterations of 7 genes
EGFR mutations. All genetic alterations of
EGFR gene were illustrated in Table III. Mutations were found in 6
samples in exon 18, 29 in exon 19 including 21 samples of 19
deletions, 2 in exon 20 and 34 in exon 21. There are 56 cases with
EGFR mutations in adenocarcinoma and two in squamous cell
carcinoma. Ten samples have doublet mutations in EGFR gene.
The distribution of doublet EGFR mutations was one with
L858R and E746_S752del, one with L858R and E746_A750del, one with
C781S and E746_T751delinsE, one with L858R and V834L, one with
L747_P753delinsS and T790M, one with E746_R748del and A750P, one
with E746_R748del and K754E, one with E749Q and A750P and two with
G719S and E709K. One sample harboured quadruple mutations with
L861Q, L858R, E745_A750del and G729A.
 | Table III.EGFR mutations detected by NGS. |
Table III.
EGFR mutations detected by NGS.
| Exon | EGFR mutation
site | Protein
position | Number of
mutations |
|---|
| Exon 18 | c.2155G>A | p.G719S | 3 |
|
| c.2125G>A | p.E709K | 2 |
|
| c.2127_2129del |
p.E709_T710delinsD | 1 |
| Exon 19 | c.2245G>C | p.E749Q | 1 |
|
| c.2248G>C | p.A750P | 5 |
|
| c.2260A>G | p.K754E | 1 |
|
| c.2186G>C | p.G729A | 1 |
|
| c.2238_2252del |
p.E746_T751delinsE | 3 |
|
| c.2236_2244del | p.E746_R748del | 2 |
|
| c.2239_2256del | p.L747_S752del | 1 |
|
| c.2236_2250del | p.E746_A750del | 3 |
|
| c.2236_2256del | p.E746_S752del | 1 |
|
| c.2235_2249del | p.E746_A750del | 5 |
|
| c.2236_2249del | p.E746_A750del | 1 |
|
| c.2237_2251del | p.E746fs | 1 |
|
| c.2240_2257del |
p.L747_P753delinsS | 4 |
| Exon 20 | c.2369C>T | p.T790M | 1 |
|
| c.2341T>A | p.C781S | 1 |
| Exon 21 | c.2573T>G | p.L858R | 30 |
|
| c.2471G>C | p.G824A | 1 |
|
| c.2582T>A | p.L861Q | 1 |
|
| c.2588G>A | p.G863D | 1 |
|
| c.2500G>T | p.V834L | 1 |
KRAS mutations. KRAS, BRAF, Her-2,
NRAS and PIK3CA mutations were shown in Table IV. Representative types of genetic
alterations in KRAS were six, with all of these located in
exon 2. One sample harboured doublet KRAS mutations with
G12C and G12A.
 | Table IV.KRAS, BRAF, Her-2, NRAS and PIK3CA
mutations detected by NGS sequencing. |
Table IV.
KRAS, BRAF, Her-2, NRAS and PIK3CA
mutations detected by NGS sequencing.
| Gene | Mutation site | Protein
position | Number of
mutations |
|---|
| KRAS | c.34G>T | p.G12C | 2 |
|
| c.37G>T | p.G13C | 1 |
|
| c.35G>A | p.G12D | 4 |
|
| c.34G>A | p.G12C | 1 |
|
| c.35G>T | p.G12V | 2 |
|
| c.35G>C | p.G12A | 1 |
| BRAF | c.1799T>A | p.V600E | 1 |
|
| c.1854G>T | p.L618F | 1 |
| Her-2 | c.2282C>A | p.P761H | 2 |
| NRAS | c.99T>G | p.D33E | 1 |
|
| c.35G>A | p.G12D | 1 |
| PIK3CA | c.1624G>A | p.E542K | 2 |
|
| c.1633G>A | p.E545K | 3 |
|
| c.3140A>T | p.H1047L | 2 |
| TP53 | c.338G>T | p.G113V | 2 |
|
| c.128G>A | p.R43H | 2 |
|
| c.422G>T | p.R141L | 1 |
|
| c.337G>T | p.G113C | 1 |
|
| c.431C>G | p.A144G | 2 |
|
| c.105delG | p.Q35fs | 1 |
|
| c.437C>A | p.P146H | 1 |
|
| c.443G>C | p.R148T | 1 |
|
| c.329G>A | p.C110Y | 1 |
|
| c.335G>A | p.G112D | 2 |
|
| c.422G>A | p.R141H | 1 |
|
| c.98C>G | p.P33R | 5 |
|
| c.415G>T | p.E139X | 1 |
|
| c.326C>T | p.S109F | 1 |
|
| c.448C>T | p.R150W | 1 |
|
| c.320delA | p.N107fs | 1 |
|
| c.422G>C | p.R141P | 1 |
|
| c.401G>T | p.G134V | 2 |
|
| c.353 C>T | p.P118L | 1 |
|
| c.419_439 del | p.140_147 del | 1 |
|
| c.436 C>T | p.P146S | 1 |
|
| c.326 C>A | p.S109Y | 1 |
|
| c.305 A>C | p.Y102S | 1 |
|
| c.428 G>T | p.C143F | 1 |
|
| c.424 G>T | p.V142F | 1 |
BRAF mutations. Two samples carried
BRAF mutations were p.V600E and p.L618F.
NRAS mutations. One patient carried
NRAS D33E mutations plus EGFR 19 deletion while another
patient carried NRAS G12D alteration.
Her-2 mutations. Both of the patients with
Her-2 mutations were P761H mutation.
PIK3CA mutations. There were 6 cases of
PIK3CA mutations, with 4 located in exon 9 and 2 in exon 20.
One sample carried doublet PIK3CA mutations with E545K and
E542K. The remaining patients with PIK3CA mutations all have
other gene mutations such as BRAF, EGFR or TP53.
TP53 mutations. The tumour suppressor gene
TP53 mutations are diverse. 25 classes of mutations occurred
in Tp53.
Comparison of NGS, Sanger sequencing
and ddPCR for detecting EGFR mutations
Sanger sequencing, as golden standard, were
performed all 112 specimens. The overall detection rate of NGS and
Sanger sequencing was 51.79% (58/112) and 37.50% (42/112),
respectively (χ2=5.88, P=0.015). There were 18 samples
owning low frequency of mutations according to NGS results. In 58
positive samples, 40 samples were identified both by NGS and Sanger
sequencing. 16 mutation-positive samples in NGS results became
negative by Sanger sequencing and two negative samples were
identified as positive by Sanger sequencing (Table V). Compared to Sanger sequencing,
the total sensitivity and specificity of NGS assays was 95.24%
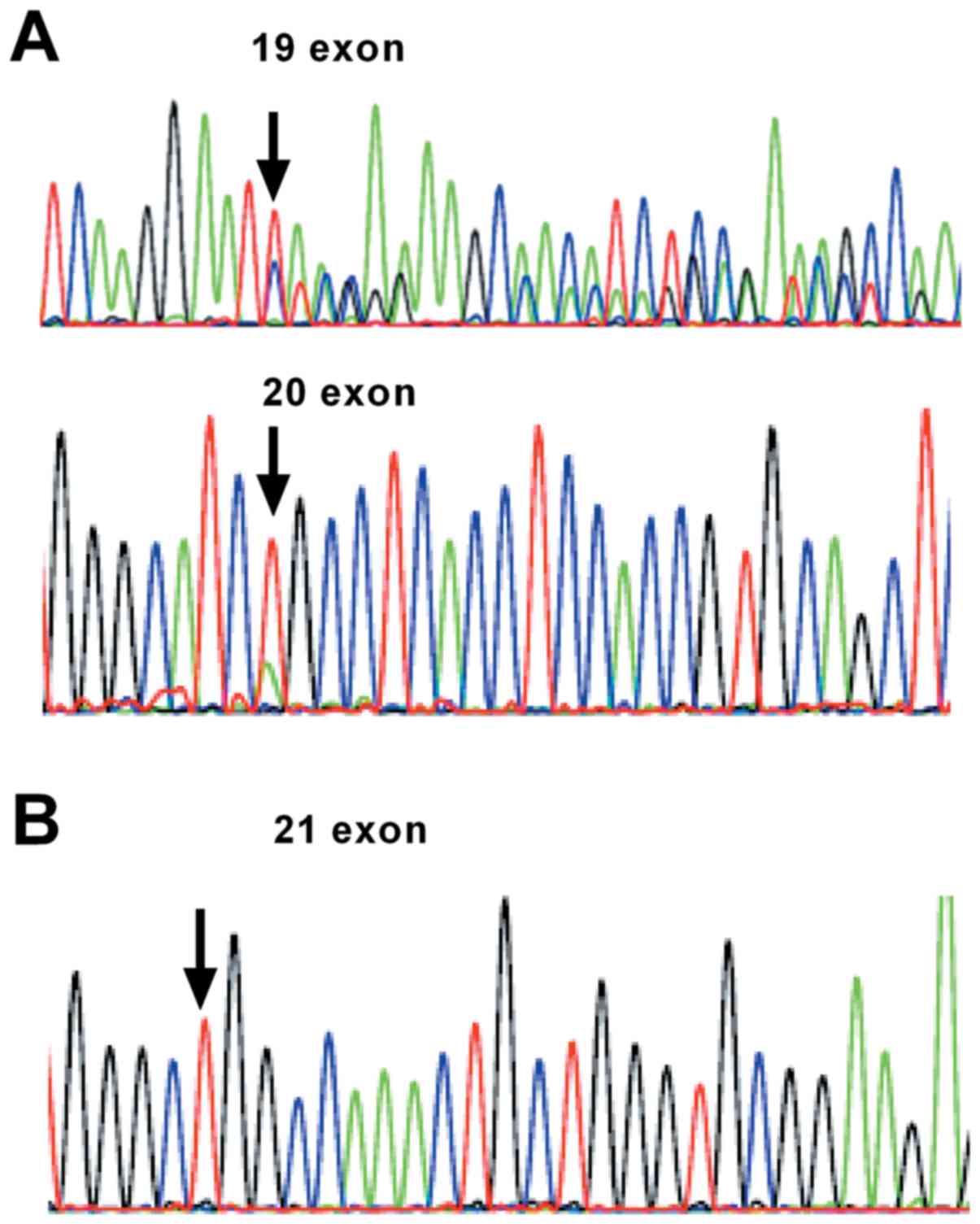
(40/42) and 77.14% (54/70), respectively. Fig. 2 showed that rare mutations with 19
deletion and E-20 c.2341T>A mutation were also found in Sanger
sequencing. Apart from uncommon mutations of EGFR, ddPCR was
conducted in 101 NSCLC specimens. As shown in Table VI, the overall positive rate of
NGS and ddPCR was 45.54% (46/101) and 47.52% (48/101), respectively
(χ2=0.000598, P=0.98). Compared to ddPCR, the overall
sensitivity and specificity of NGS assays was 95.83% (46/48) and
98.11% (52/53), respectively. The advantages and disadvantages of
the NGS, Sanger and ddPCR were presented in Table VII.
 | Table V.Performance of NGS and Sanger
sequencing platforms for detection of epidermal growth factor
receptor mutation. |
Table V.
Performance of NGS and Sanger
sequencing platforms for detection of epidermal growth factor
receptor mutation.
|
| Sanger sequencing
(+) | Sanger sequencing
(−) |
|---|
| NGS (+) | 40 | 16 |
| NGS (−) | 2 | 54 |
 | Table VI.Performance of NGS and ddPCR
platforms for detection of EGFR mutation. |
Table VI.
Performance of NGS and ddPCR
platforms for detection of EGFR mutation.
| Variable | ddPCR (+) | ddPCR (−) |
|---|
| NGS (+) | 46 | 1 |
| NGS (−) | 2 | 52 |
 | Table VII.Characteristics of the NGS, Sanger
sequencing and ddPCR. |
Table VII.
Characteristics of the NGS, Sanger
sequencing and ddPCR.
| Features | Sanger
sequencing | ddPCR | NGS |
|---|
| Frequency
quantity | No | Yes | Yes |
| Sensitivity | 10% | 0.04–0.1% | 0.1% |
| Coverage area | Common/uncommon
mutations | Common
mutations | Common/uncommon
mutations |
| Time for
results | 2-3 days | 1 day | 2-3 days |
| Technical
characteristics | High accuracy, only
suitable for tissues | Very high
sensitivity but questioned by false-positive error | High output |
Discussion
In lung cancer, the mutational status of oncogenic
driver can implicate the efficacy of EGFR-TKIs and future survival
for patients. It has been reported that EGFR mutation status
resulted in the structural changes in the tyrosine kinase domain of
EGFR. The main types of EGFR mutations were in exon19
deletions and exon21 (L858R) (9).
Consistent with previous research (10), more EGFR mutations were detected in
adenocarcinomas compared with squamous cell carcinoma. The positive
rate of EGFR was 68.29% (56/82) in adenocarcinoma vs. 8.33%
(2/24) in squamous cell carcinoma. The patients with KRAS
mutations may not respond to EGFR antibodies and EGFR kinase
inhibitors (11). A study in 5125
samples from NSCLC patients revealed that 8.0% of KRAS
mutations were located in exon 2 and exon 3 (12). In this investigation, all genetic
alterations in KRAS were found in exon 2. The quantity of
samples attributed to the different results. Moreover, additional
targeted drugs for NSCLC patients include BRAF inhibitors.
Melanomas with BRAF mutations have been reported to be
highly sensitive to BRAF inhibitors (13). Dabrafenib, a BRAF inhibitor
is currently undergoing phase 2 trial for treatment of V600E
BRAF-mutant lung adenocarcinomas, which may become another
new drug in individualized therapy for lung cancer patients.
BRAF V600E mutated lung cancer is a genetically distinct
subtype that occurs in 1.7% of non-small cell lung carcinomas and
2.3% among 646 adenocarcinomas (14). However, we found only 1 sample
(1/112) with p.V600E and 1 with p.L618F. One of the BRAF-positive
samples was also PIK3CA-mutated, and one had a TP53
mutation. HER2, a member of the human EGFR (ErbB) family, is a
receptor tyrosine kinase is encoded by the Her-2 gene. It is
involved in PI3K-Akt and MEK/ERK signaling pathways, associated
with cell proliferation and migration (15). Her-2 mutations have been
found in 2–4% of lung adenocarcinomas (16,17).
The frequency of Her-2 mutation was 1.8% in our present
studies, all in exon 19 mutations not exon 20. The results are
different from the previous reports, probably due to geographical
area and sample size.
Our investigation found 2 patients with three types
of gene mutations and 22 patients with two types. It is rare that
mutations in NRAS and KRAS occur along with other
driver-driven genetic alterations. Although concomitant mutations
of some double genes seem paradox theoretically, we found
TKI-sensitive and TKI-resistant variants co-existed. Overlap
mutations in driver genes may puzzle clinical doctors in making
individualized treatment for lung cancer. The sensitivity analysis
of these patients to EGFR-TKIs requires follow-up. Advanced lung
cancer patients with EGFR mutations or KRAS mutations
and PIK3CA mutations have a poor prognosis. Patients with
concurrent PIK3CA and EGFR mutations can not benefit
from EGFR-TKIs (18). One study
reported the mutation characteristics of patients with stage 1b
lung adenocarcinoma in China. The results showed that only one
patient had EGFR T790M mutation and KRAS mutation. No
other EGFR mutation coexisting with KRAS was found
(19). We believe there will be
more reports of concurrent mutations in driver genes in the future,
and the clinical detection of multiple oncogene mutations can help
determine the optimal treatment regimen.
High throughput sequencing has not only provided us
with rich genetic information, but also greatly reduced the cost
and time of sequencing, with high output and high resolution. This
technology has been applied wildly in cancer research. Previous
reports have shown that though the frequency of single gene
mutations in lung cancer may be low, the mutation rate of multiple
oncogenic driver genes was really high. Individuals with oncogenic
driver gene mutations receiving targeted therapy lived longer
(20). In this study, we carried
out NGS in NSCLC patients to evaluate the efficacy of NGS by
comparison to ddPCR assay and Sanger sequencing. Our results showed
NGS-based methods have demonstrated performance sensitivity but low
specificity of NGS due to 18 low frequency mutant specimens
compared to Sanger sequencing. Among them, 16 specimens were
EGFR wildtype by Sanger sequencing. In addition, the results
of NGS and ddPCR test were highly consistent. The high clinical
sensitivity and specificity support the routine use of NGS
detection in clinical trials to promote the treatment of patients
with lung cancer. The detection rate of NGS for EGFR was
significantly higher than that of Sanger sequencing. However, there
was no significant statistical difference between ddPCR and NGS
results. Besides, NGS can detect both hotspot and non-hotspot
mutations. In general, ddPCR diagnostic kits are commonly used to
detect common mutations or hotspots. However, rare mutations in
EGFR are also important for predicting the efficacy of EGFR-TKI
drugs, so the identification of non-hotspot mutations is essential
for clinical research and treatment (2,21).
In EMSO 2017, AURA17 studies initiated by Zhou et al
(22) demonstrated the objective
response rates (ORR) of ochitinib in patients with T790M mutations
detected by the three detection methods were 56% (Cobas; Roche
Diagnostics, Basel, Switzerland), 64% (SuperARMS) and 56% ddPCR,
respectively. Furthermore, ORR of ochitinib in patients without
T790M mutations detected by Cobas and ddPCR was higher than that in
positive patients. Whether there is false-negative and
false-positive error made by ddPCR is also needed for further
study. However, NGS has its limitation. In the process of
high-throughput sequencing, there are many problems that need to be
solved: the role of data in clinical diagnosis, storage and
analysis of sequencing data, data security and information
privacy.
In conclusion, our results show that NGS has the
advantages of high sensitivity and multiplexed testing. More data
should be required to evaluate sensitivity, stability and clinical
applicability. Each detection method has its advantages and
disadvantages. Practice is the sole criterion for testing truth,
and the benefit of cancer patients after treatment is the only
criterion for judging methods. Detection methods should complement
each other to achieve balance and coexistence, maximizing benefit
of patients. In daily work, Sanger sequencing and ddPCR, as
supplement of NGS results, are suggested to confirm uncommon
mutations and low frequency mutations, respectively.
Acknowledgements
Not applicable.
Funding
The present study was supported by the program from
the Health Department of Jiangsu Province (grant no. Z201602) and
from the Science Foundation of Jiangsu Province (grant no.
BE2016795).
Availability of data and materials
The datasets used and analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
CJ, XM and ZW wrote the manuscript and designed the
study. KS performed the ddCPR experiments. RM performed NGS and
Sanger sequencing. JW and HC contributed to the design of the
study. All authors read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
The research using human tissue was approved by the
Cancer Institute of Jiangsu Province Ethics Committee. All patients
participated in the study signed informed consent.
Patient consent for publication
All patients participated in the study signed
informed consent.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Chen W, Zheng R, Baade PD, Zhang S, Zeng
H, Bray F, Jemal A, Yu XQ and He J: Cancer statistics in China,
2015. CA Cancer J Clin. 66:115–132. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Baek JH, Sun JM, Min YJ, Cho EK, Cho BC,
Kim JH, Ahn MJ and Park K: Efficacy of EGFR tyrosine kinase
inhibitors in patients with EGFR-mutated non-small cell lung cancer
except both exon 19 deletion and exon 21 L858R: A retrospective
analysis in Korea. Lung Cancer. 87:148–154. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Tomasini P, Serdjebi C, Khobta N, Metellus
P, Ouafik L, Nanni I, Greillier L, Loundou A, Fina F, Mascaux C and
Barlesi F: EGFR and KRAS Mutations Predict the incidence and
outcome of brain metastases in non-small cell lung cancer. Int J
Mol Sci. 17:pii: E2132. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Smit E: BRAF mutations in non-small-cell
lung cancer. J Thorac Oncol. 9:1594–1595. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Scheffler M, Bos M, Gardizi M, König K,
Michels S, Fassunke J, Heydt C, Künstlinger H, Ihle M, Ueckeroth F,
et al: PIK3CA mutations in non-small cell lung cancer (NSCLC):
Genetic heterogeneity, prognostic impact and incidence of prior
malignancies. Oncotarget. 6:1315–1326. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lee SY, Jeon HS, Hwangbo Y, Jeong JY, Park
JY, Lee EJ, Jin G, Shin KM, Yoo SS, Lee J, et al: The influence of
TP53 mutations on the prognosis of patients with early stage
non-small cell lung cancer may depend on the intratumor
heterogeneity of the mutations. Mol Carcinog. 54:93–101. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhu G, Ye X, Dong Z, Lu YC, Sun Y, Liu Y,
McCormack R, Gu Y and Liu X: Highly sensitive droplet digital PCR
method for detection of EGFR-activating mutations in plasma
cell-free DNA from patients with advanced non-small cell lung
cancer. J Mol Diagn. 17:265–272. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Xu X, Yang Y, Li H, Chen Z, Jiang G and
Fei K: Assessment of the clinical application of detecting EGFR,
KRAS, PIK3CA and BRAF mutations in patients with non-small cell
lung cancer using next-generation sequencing. Scand J Clin Lab
Invest. 76:386–392. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Maemondo M, Inoue A, Kobayashi K, Sugawara
S, Oizumi S, Isobe H, Gemma A, Harada M, Yoshizawa H, Kinoshita I,
et al: Gefitinib or chemotherapy for non-small-cell lung cancer
with mutated EGFR. Engl J Med. 362:2380–2388. 2010. View Article : Google Scholar
|
|
10
|
Maheswaran S, Sequist LV, Nagrath S, Ulkus
L, Brannigan B, Collura CV, Inserra E, Diederichs S, Iafrate AJ,
Bell DW, et al: Detection of mutations in EGFR in circulating
lung-cancer cells. Engl J Med. 359:366–377. 2008. View Article : Google Scholar
|
|
11
|
Jackman DM, Miller VA, Cioffredi LA, Yeap
BY, Jänne PA, Riely GJ, Ruiz MG, Giaccone G, Sequist LV and Johnson
BE: Impact of epidermal growth factor receptor and KRAS mutations
on clinical outcomes in previously untreated non-small cell lung
cancer patients: Results of an online tumor registry of clinical
trials. Clin Cancer Res. 15:5267–5273. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Li S, Li L, Zhu Y, Huang C, Qin Y, Liu H,
Ren-Heidenreich L, Shi B, Ren H, Chu X, et al: Coexistence of EGFR
with KRAS, or BRAF, or PIK3CA somatic mutations in lung cancer: A
comprehensive mutation profiling from 5125 Chinese cohorts. Br J
Cancer. 110:2812–2820. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Flaherty KT, Puzanov I, Kim KB, Ribas A,
McArthur GA, Sosman JA, O'Dwyer PJ, Lee RJ, Grippo JF, Nolop K and
Chapman PB: Inhibition of mutated, activated BRAF in metastatic
melanoma. N Engl J Med. 363:809–819. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Brustugun OT, Khattak AM, Trømborg AK,
Beigi M, Beiske K, Lund-Iversen M and Helland Å: BRAF-mutations in
non-small cell lung cancer. Lung Cancer. 84:36–38. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yarden Y and Sliwkowski MX: Untangling the
ErbB signalling network. Nat Rev Mol Cell Biol. 2:127–137. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Cancer Genome Atlas Research Network:
Comprehensive molecular profiling of lung adenocarcinoma. Nature.
511:543–550. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Mazières J, Peters S, Lepage B, Cortot AB,
Barlesi F, Beau-Faller M, Besse B, Blons H, Mansuet-Lupo A, Urban
T, et al: Lung cancer that harbors an HER2 mutation: Epidemiologic
characteristics and therapeutic perspectives. J Clin Oncol.
31:1997–2003. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Eng J, Woo KM, Sima CS, Plodkowski A,
Hellmann MD, Chaft JE, Kris MG, Arcila ME, Ladanyi M and Drilon A:
Impact of concurrent PIK3CA mutations on response to EGFR tyrosine
kinase inhibition in EGFR-mutant lung cancers and on prognosis in
oncogene-driven lung adenocarcinomas. J Thorac Oncol. 10:1713–1719.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Wen YS, Cai L, Zhang XW, Zhu JF, Zhang ZC,
Shao JY and Zhang LJ: Concurrent oncogene mutation profile in
Chinese patients with stage Ib lung adenocarcinoma. Medicine
(Baltimore). 93:e2962014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kris MG, Johnson BE, Berry LD, Kwiatkowski
DJ, Iafrate AJ, Wistuba II, Varella-Garcia M, Franklin WA, Aronson
SL, Su PF, et al: Using multiplexed assays of oncogenic drivers in
lung cancers to select targeted drugs. JAMA. 311:1998–2006. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Keam B, Kim DW, Park JH, Lee JO, Kim TM,
Lee SH, Chung DH and Heo DS: Rare and complex mutations of
epidermal growth factor receptor, and efficacy of tyrosine kinase
inhibitor in patients with non-small cell lung cancer. Int J Clin
Oncol. 19:594–600. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zhou C, et al: Phase II Single Arm Study
of AZD9291 to Treat NSCLC Patients in Asia Pacific (AURA17).
https://clinicaltrials.gov/ct2/show/study/NCT02442349April
25–2017
|