Introduction
Head and neck squamous cell carcinoma (HNSCC) is
essentially a heterogeneous disease, usually resulting from the
mucosal lining of the upper respiratory tract, including oral
cavity, nasal cavity and throat. HNSCC is ranked sixth in the
leading cause of cancer-associated fatalities worldwide. It is
characterized by complex anatomy, regional diffusion, distant
metastasis and high recurrence. HNSCC can induce the production of
cytokines and growth factors that participate in the processes of
gene expression, cell growth, survival and chemosensitivity
(1,2). Over the past few decades, although
the diagnostic techniques and treatment methods have made great
progress, the morbidity and mortality rates of HNSCC patients
remain high (3). The development
of novel molecular biology investigation techniques contributes to
identify the molecules that serve an inhibitory role or
facilitating role in tumors. Targeting these molecules has become
an effective strategy for the treatment of cancer and may
ultimately improve the disease-free survival rates of cancer
patients.
Cancer-testis antigens (CTAs) are a class of
tumor-associated antigens that contains more than 200 members,
characterized by specific expression in placental tissue and in a
variety of tumor tissues and testes, but expressed at a low level
or not expressed in other normal tissues (4). Previously, certain CTAs have been
studied as target antigens in clinical trials and demonstrated
available therapeutic effect on the treatment of glioblastoma,
particularly for melanoma associated antigen (MAGEA)1 and NY-ESO1
(5). Additionally, frequent
expression of specific CTA genes in HNSCC has been studied. For
example, Atanackovic et al (6) have reported that the expression of
MAGEA3 and SSX1 in HNSCC was 72 and 45%, respectively. However, the
roles of CTA genes in HNSCC remain unknown. Actin-like protein 8
(ACTL8) is a member of the CTA family and contains 366 amino acids.
ACTL8 is also known as CT57, as it is the 57th member of the CTA
family (http://www.CTA.lncc.br). The ACTL8 gene
was reported to be highly expressed in glioblastoma, whereas it was
expressed at a low level in the bladder, pancreas, thymus and colon
tissues, and not expressed in normal brain tissues (7). Yao et al (8) have suggested that the expression of
ACTL8 gene in breast cancer was also upregulated. ACTL8 gene is
located on chromosome 1p36.13 and the aberrations of chromosome 1
occur frequently in head and neck cancer (9). However, to date, there is little
direct evidence of the role of ACTL8 in head and neck cancer.
In order to investigate the potential role of ACTL8,
the present study investigated the expression levels and clinical
significance of ACTL8 in HNSCC. Furthermore, the effects of ACTL8
on the proliferation, invasion and migration of HNSCC PCI-13 cells
were determined by knockdown of ACTL8. In addition, alterations in
the expression levels of proteins involved in the
phosphatidylinositol-4,5-bisphosphate 3-kinase (PI3K)/protein
kinase B (AKT) signaling pathway were detected upon transfection of
PCI-13 cells with ACTL8 small interfering RNA (siRNA). The results
indicated that ACTL8 may serve an important role in HNSCC
progression and could be considered a significant prognostic marker
and therapeutic target for HNSCC.
Materials and methods
Patients
A total of 110 patients of HNSCC, who had received
curative surgery at the Department of Otolaryngology-Head and Neck
Surgery in Jinan Central Hospital Affiliated to Shandong University
(Jinan, China) were selected by reviewing the medical records
between January 2002 and December 2014. Furthermore, 110 adjacent
normal tissues taken from the corresponding patients were selected.
Notably, no radiotherapy and chemotherapy were performed for all
samples prior to surgery. Half specimens were imbedded with
paraffin following fixation with 10% formalin at room temperature
for 48 h and protected from light at room temperature. The other
half number of specimens were used to detect mRNA expression
levels. The clinical features including age, gender,
pathological-stage and tumor status are presented in Table I. This study obtained the informed
consent of all patients and was approved by the Jinan Central
Hospital Affiliated to Shandong University Medical Ethics
Committee.
 | Table I.Correlation between
clinicopathological parameters and ACTL8 expression in head and
neck squamous cell carcinoma (n=110). |
Table I.
Correlation between
clinicopathological parameters and ACTL8 expression in head and
neck squamous cell carcinoma (n=110).
|
| Expression of
ACTL8 |
|
|---|
|
|
|
|
|---|
| Characteristics | Low | High | P-value |
|---|
| Age |
|
| 0.699 |
|
<60 | 22 | 24 |
|
| ≥60 | 33 | 31 |
|
| Sex |
|
| 0.152 |
|
Female | 21 | 14 |
|
| Male | 34 | 41 |
|
|
Pathological-stage |
|
| 0.251 |
| I+II | 28 | 22 |
|
|
III+IV | 27 | 33 |
|
| Tumor status |
|
| 0.702 |
|
T1+T2 | 30 | 28 |
|
|
T3+T4 | 25 | 27 |
|
| Node metastasis |
|
| 0.002a |
| N0 | 49 | 35 |
|
| N1 | 6 | 20 |
|
| Distant
metastasis |
|
| 1.000 |
| M0 | 54 | 53 |
|
| M1 | 1 | 2 |
|
| Grade |
|
| 0.021a |
|
G1+G2 | 48 | 38 |
|
|
G3+G4 | 7 | 17 |
|
In the present study, the gene expression profile
information for patients with HNSCC was obtained from TCGA data
portal (cancergenome.nih.gov). A total of 502
samples with HNSCC as disease group and 44 healthy samples as a
control group were selected.
Cell culture
Human HNSCC cell line PCI-13 was purchased from the
Chinese Academy of Medical Sciences cell bank (Shanghai, China).
Normal oral cells of primary gingival keratinocytes, which were
used as a control were obtained from the American Type Culture
Collection, (Manassas, VA, USA; PCS-200-014™). Cells
were cultured in RPMI1640 (Gibco; Thermo Fisher Scientific, Inc.,
Waltham, MA, USA) medium at a humidified chamber of 37°C containing
5% CO2. In addition, 10% heat-inactivated fetal bovine
serum (FBS, Thermo Fisher Scientific, Inc.), 100 µg/ml streptomycin
and 100 U/ml penicillin (Thermo Fisher Scientific, Inc.) were
supplemented in the medium.
RNA extraction and reverse
transcription-quantitative polymerase chain reaction (RT-qPCR)
detection
Total RNA was separated from PCI-13 cells using
TRIzol reagent (Invitrogen; Thermo Fisher Scientific, Inc.)
according to the manufacturer's protocol. Reverse transcription was
conducted on 3 µg of total RNA per sample to generate cDNA with a
RevertAid First Strand cDNA Synthesis kit (Fermentas, Thermo Fisher
Scientific, Inc.). The obtained cDNAs were used in amplification,
analysis and quantification of PCR. Probes were amplified by RT-PCR
with specific primers. The primer sequences of ACTL8 mRNA were
designed and synthesized as follows: 5′-GCCACGTGCTCACAGAGTAG-3′
(forward) and 5′-CTCAGCTGCACACTGCAAAC-3′ (reverse). GAPDH was used
as an internal control. The primer sequences of GAPDH were as
follows: Forward, 5′-GGAGCGAGATCCCTCCAAAAT-3′ and reverse,
5′-GGCTGTTGTCATACTTCTCATGG-3′ (Table
II). The PCR cycle condition was set as follows: 95°C for 5
min, followed by 40 cycles of 95°C for 30 sec, 60°C for 45 sec,
72°C for 30 min. For the RT-qPCR analysis, comparative
Cq method (DDCq) (10) was performed to compute the
expression levels. All experiments were independently repeated
three times.
 | Table II.Primers sequences used. |
Table II.
Primers sequences used.
| Gene | Primer
sequence | PCR cycle
condition |
|---|
| ACTL8 | Forward:
5′-GCCACGTGCTCACAGAGTAG-3′ | 95°C 5 sec |
|
| Reverse:
5′-CTCAGCTGCACACTGCAAAC-3′ | 95°C 30 sec |
| GAPDH | Forward:
5′-GGAGCGAGATCCCTCCAAAAT-3′ | 60°C 45 sec |
|
| Reverse:
5′-GGCTGTTGTCATACTTCTCATGG-3′ | 72°C 30 sec |
Western blot assay
The cancer samples and cell line were lysed in RIPA
lysis buffer (Beyotime Institute of Biotechnology, Nantong, China).
Lysates were collected by centrifugation 13,400 × g at 4°C for 20
min. The concentration of proteins was detected using bicinchoninic
acid Protein Assay kit (CWBiotech Co., Ltd., Beijing, China)
according to the manufacturer's protocol. Subsequently, equal
amounts (20 µg) of each sample were placed on a 10% polyacrylamide
gel, isolated using 12% SDS-PAGE and then the samples were
transferred onto a polyvinylidene fluoride membranes (EMD
Millipore, Billerica, MA, USA). Furthermore, the membrane was
blocked in TBS with 5% non-fat dry milk at room temperature for 1
h. Finally, western blot analysis was conducted by incubating the
membrane with rabbit anti-human ACTL8 antibody (anti-ACTL8;
1:1,000; cat. no. sc-377372; Santa Cruz Biotechnology, Inc.,
Dallas, TX, USA), PI3K (1:1,000; cat. no. 4255), AKT (1:1,000; cat.
no. 9272), P-70S6K (1:1,000; cat. no. 9202) and the phosphorylation
antibody p-PI3K (1:1,000; cat. no. 4228), p-AKT (1:1,000; cat. no.
9271), p-p70S6K (1:1,000; cat. no. 9204; CST Biological Reagents
Co., Ltd.) at 4°C overnight and incubated with secondary antibody
anti-rabbit HRP (1:5,000; cat. no. 7074; CST Biological Reagents
Co., Ltd.) at room temperature for 2 h. GAPDH (1:2,000; cat. no.
5174) was used as control. Consequently, all blot analysis was
conducted using a Pierce™ ECL Western Blotting Substrate kit
(Thermo Fisher Scientific, Inc.).
Cell transfection
PCI-13 cells were placed in 6-well plates
(1×105 cells/well) and cultured using serum-free medium
when the density reached to 80%. A total of 125 µl opti-MEM medium
(Thermo Fisher Scientific, Inc.) was used to mix the ACTL8 siRNA
(si-ACTL8: 5′-GAGTCTCTTTAAGGAAGATTGCGAT-3′) or negative control
siRNA (5′-TAGCGTTAGAAGGAATTTCTCTGAG-3′) at 50 nM. A total of 3.75
µl Lipofectamine-2000 (Thermo Fisher Scientific, Inc.) was
extracted to mix with another 125 µl opti-MEM medium and then was
incubated for 5 min. Subsequently, the mixture was re-seeded to a
6-well plate after reaching 60–80% confluency and cultured at 37°C
for 3–5 days. Finally, the transfected cells were extracted for
subsequent analysis.
Cell proliferation
PCI-13 cells were digested and counted following
transfection for 72 h to prepare cell suspensions. A total of 100
µl the cell suspension was extracted and seeded to a 96-well plate
at a density of 103 cell/well, then placing in a carbon
dioxide incubator for routine cultivation. Cell Counting Kit-8
(CCK-8; Beijing Solarbio Science & Technology Co., Ltd.,
Beijing, China) was employed to measure the proliferation of PCI-13
cells, the results were detected at 0, 24, 48, 72 and 96 h,
respectively. Microplate reader at 450 nm was conducted to detect
the absorbance of the wells in the plate.
Plate colony formation assay
Stably transfected PCI-13 cells were placed into a
6-well plate at a density of 500 cell/well in triplicate and
maintained in DMEM containing 10% FBS for cultivation. Following
incubation for 12 days at 37°C in a humid chamber, the cells were
washed with PBS and fixed using 4% paraformaldehyde for 30 min at
room temperature. Subsequently, the fixative was removed and cells
were stained with 0.1% crystal violet at room temperature for 30
min. Finally, after the residual staining solution was rinsed with
running water, the size and number of clones were counted under a
light microscope.
Cell invasion and migration
assays
For the cell invasion assay, 100 µl Matrigel
(serum-free medium diluted 1:6) dissolved overnight was added to
the upper chamber of transwell chamber with a 24-well plate, which
then was shaken and placed in carbon dioxide incubator for 4–6 h.
After the addition of gelatin, 500 µl of serum-free medium was
added to the lower chamber and maintained for 30 min to hydrate the
basement membrane. Cells following 24 h of transfection were used
to prepare cell suspensions with serum-free medium and extracting
100 µl cell suspension (1×105 cells) to add to the upper
chamber and 500 µl complete medium was added to the lower chamber.
After overnight incubation, residual cells in the upper chamber
were removed with a cotton-tipped swab. Cells penetrating the
bottom chamber from the membrane were fixed in 4% paraformaldehyde
at room temperature for 15 min and stained with 0.1% crystal violet
at room temperature for 30 min. A total of five fields of view were
randomly selected to count the number of cells using a light
microscope. The procedures in the migration assay is similar to the
invasion assays. The difference is that there is no matrigel
precoating in the transwell chamber for the migration assay.
Statistical analysis
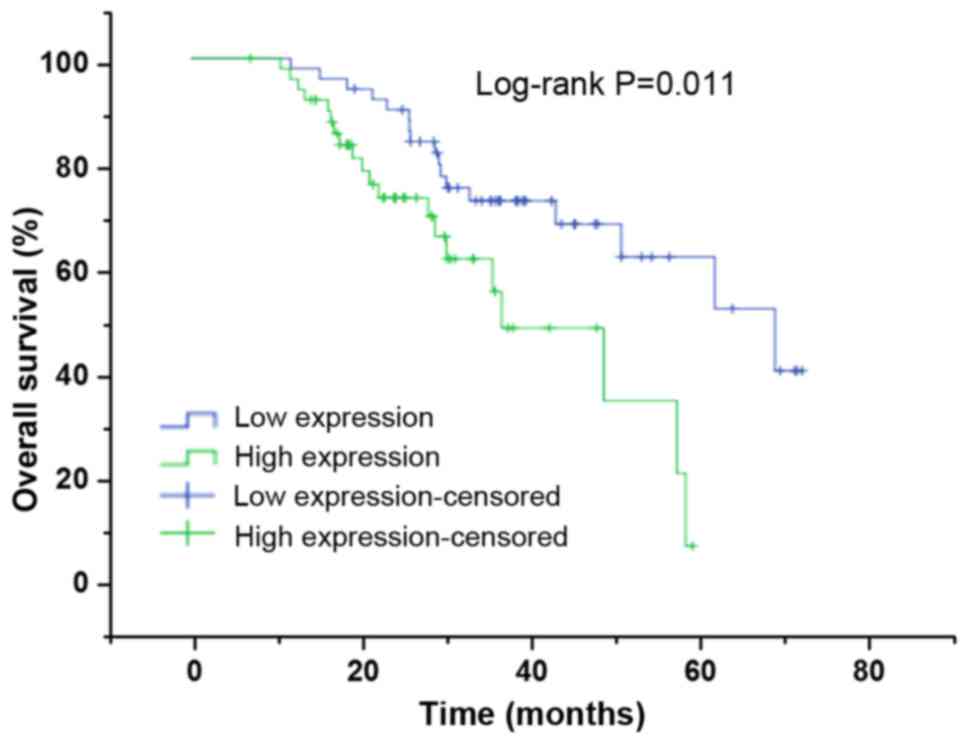
Kaplan-Meier method was used to analyze the survival
rate of patients with HNSCC. Furthermore, a log-rank test was
performed to compute the difference between survival-associated
curves. Cox proportional hazard regression models were applied to
establish univariate and multivariate survival analysis for
evaluating the independent prognostic factors. GraphPad Prism 5
(GraphPad Software, Inc., La Jolla, CA, USA) and SPSS 22.0 (IBM,
Corps., Armonk, NY USA) were employed to conduct the statistical
analysis. Chi-square test was performed to evaluate the
clinicopathological features (Table
I) and survival status (Fig.
2) of ACTL8 in HNSCC patients. A student's t-test (for two
group samples) and one-way analysis of variance followed by
Dunnett-t post-hoc test (for multiple group samples) were performed
to compare the normally distributed data. All data in this study
were expressed as the mean ± standard deviation. P<0.05 was
considered to indicate a statistically significant difference.
Results
High expression of ACTL8 in HNSCC is
associated with a poor prognosis
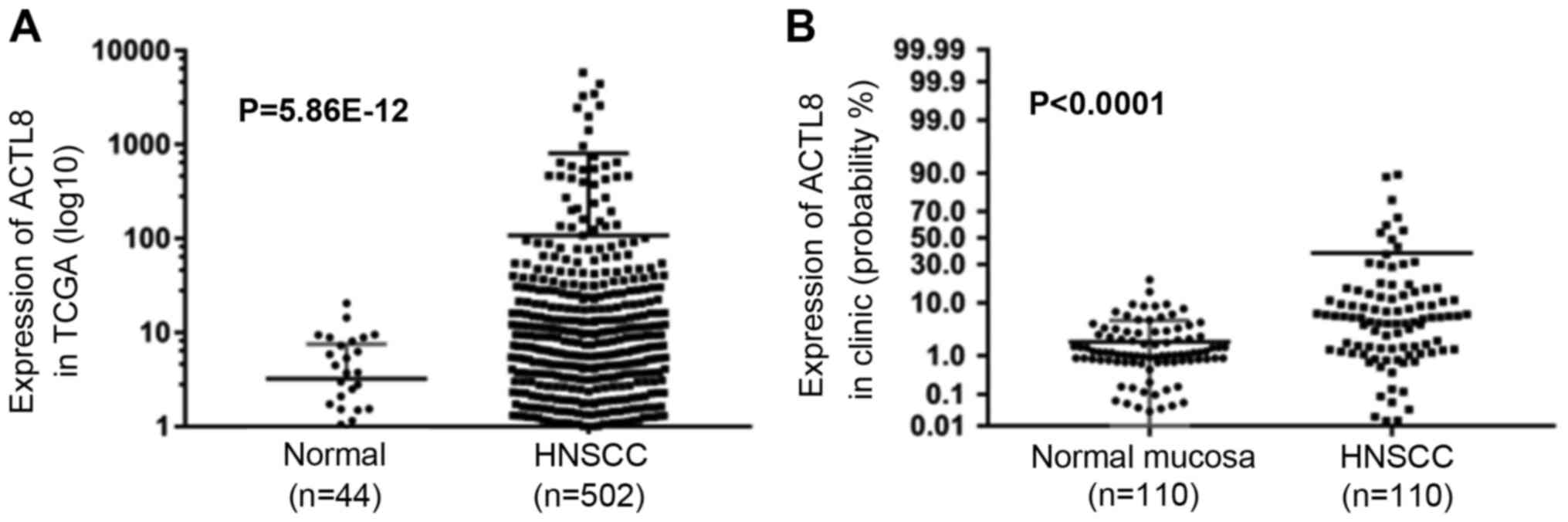
To identify the expression level of ACTL8 in HNSCC,
expression of ACTL8 was analyzed in TCGA datasets and the collected
HNSCC patients. Fig. 1A
demonstrated the expression in normal and HNSCC samples, high
expression was demonstrated in the HNSCC patients compared with the
control group (P=5.86×10−12). Notably, compared to the
expression levels in the normal mucosa group, ACTL8 in clinical
samples of HNSCC was also highly expressed (<0.0001; Fig. 1B). Pearson's chi-squared test was
applied to assess the correlation between ACTL8 expression and
clinicopathological features. It is demonstrated in Table I that there is a significant
association between ACTL8 expression with node metastasis (P=0.002)
and pathological grade (P=0.021). Whereas, the correlation between
ACTL8 expression with other clinical parameters was not
demonstrated (all P>0.05).
To further confirm the potential associations
between ACTL8 expression and prognosis of HNSCC patients, the
associations between ACTL8 expression and clinical outcomes were
measured. The Kaplan-Meier method using a log-rank test was
conducted to measure the association between ACTL8 expression and
survival status. The results in Fig.
2 demonstrated that the survival rates of HNSCC patients
between high ACTL8 expression and low ACTL8 expression groups were
significantly different, suggesting that HNSCC patients with ACTL8
high expression have a poor prognosis (χ2=6.512,
P=0.011). The univariate analysis was performed to investigate the
prognostic factors. As presented in Table III, the ACTL8 expression
(P=0.013), pathological-stage (P<0.0001), tumor status
(P<0.0001), distant metastasis (P<0.0001) and node metastasis
(P=0.008) were all the prognostic factors. Therefore, to further
confirm an independent risk factor, multivariate analysis was
conducted. Consequently, it was demonstrated that ACTL8 expression
(P=0.029) and distant metastasis could be considered as an
independent risk factor for overall survival in patients with
HNSCC.
 | Table III.Univariate and multivariate survival
analysis for head and neck squamous cell carcinoma patients. |
Table III.
Univariate and multivariate survival
analysis for head and neck squamous cell carcinoma patients.
|
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|---|
| Variables | P-value | HR | 95% CI | P-value | HR | 95% CI |
|---|
| ACTL8 expression
(high/low) | 0.013a | 2.370 | 1.199–4.684 | 0.029a | 2.277 | 1.090–4.757 |
| Pathological-stage
(I+II/III+IV) | 0.000a | 4.725 | 2.218–10.065 | 0.718 | 1.513 | 0.159–14.367 |
| Tumor status
(T1+T2/T3+T4) | 0.000a | 4.824 | 2.329–9.990 | 0.290 | 3.111 | 0.381–25.417 |
| Distant metastasis
(M0/M1) | 0.000a | 12.490 | 3.359–46.446 | 0.011a | 6.613 | 1.538–28.442 |
| Node metastasis
(N0/N1+N2+N3) | 0.008a | 2.771 | 1.309–5.864 | 0.824 | 0.895 | 0.339–2.365 |
Effect of ACTL8 gene on HNSCC PCI-13
cells
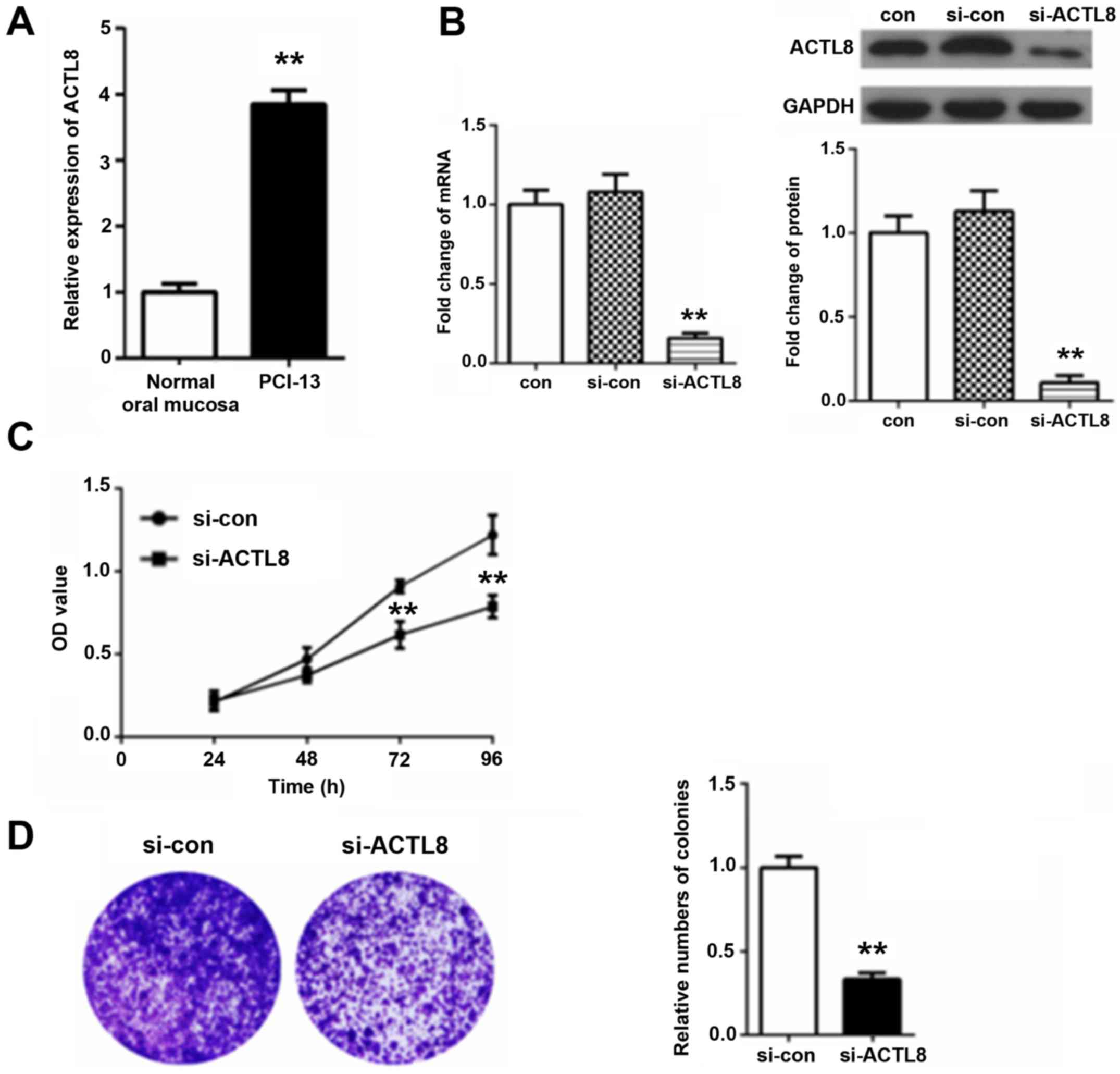
RT-qPCR method results in Fig. 3A demonstrated that ACTL8 expression
in PCI-13 cells was significantly increased compared with the
normal oral mucosa group (P<0.01). To further confirm the
function of ACTL8 in HNSCC PCI-13 cells, the ACTL8 siRNA was
transfected into the HNSCC PCI-13 cell line. Following 72 h
transfection, total RNA and proteins were extracted for performing
RT-qPCR and western blot assays. The results in Fig. 3B demonstrated that there was no
statistical difference between the blank control and interference
control. Additionally, the expression level of ACTL8 mRNA and
protein in si-ACTL8 group was significantly decreased by comparing
the si-con group (P<0.01).
In addition, the effect of ACTL8 knockout on the
proliferation of PCI-13 cells was further analyzed. A CCK-8 assay
was used to measure the proliferative activity (Fig. 3C). Consequently, compared with the
si-con group, the viability of PCI-13 in si-ACTL8 group was
inhibited, inhibition reaching significantly levels at 72 and 96 h
(P<0.01). Furthermore, the results of colony formation assays in
Fig. 3D demonstrated that the
relative number of colonies for PCI-13 cells treated with ACTL8
siRNA was significantly reduced comparing with the si-con
group (P<0.01), demonstrating that ACTL8 knockout inhibited the
colony formation rate of PCI-13 cells. These results suggest that
knockdown of ACTL8 contributes to inhibit the proliferation of
PCI-13 cells.
ACTL8 knockout suppresses invasion and
migration of PCI-13 cells
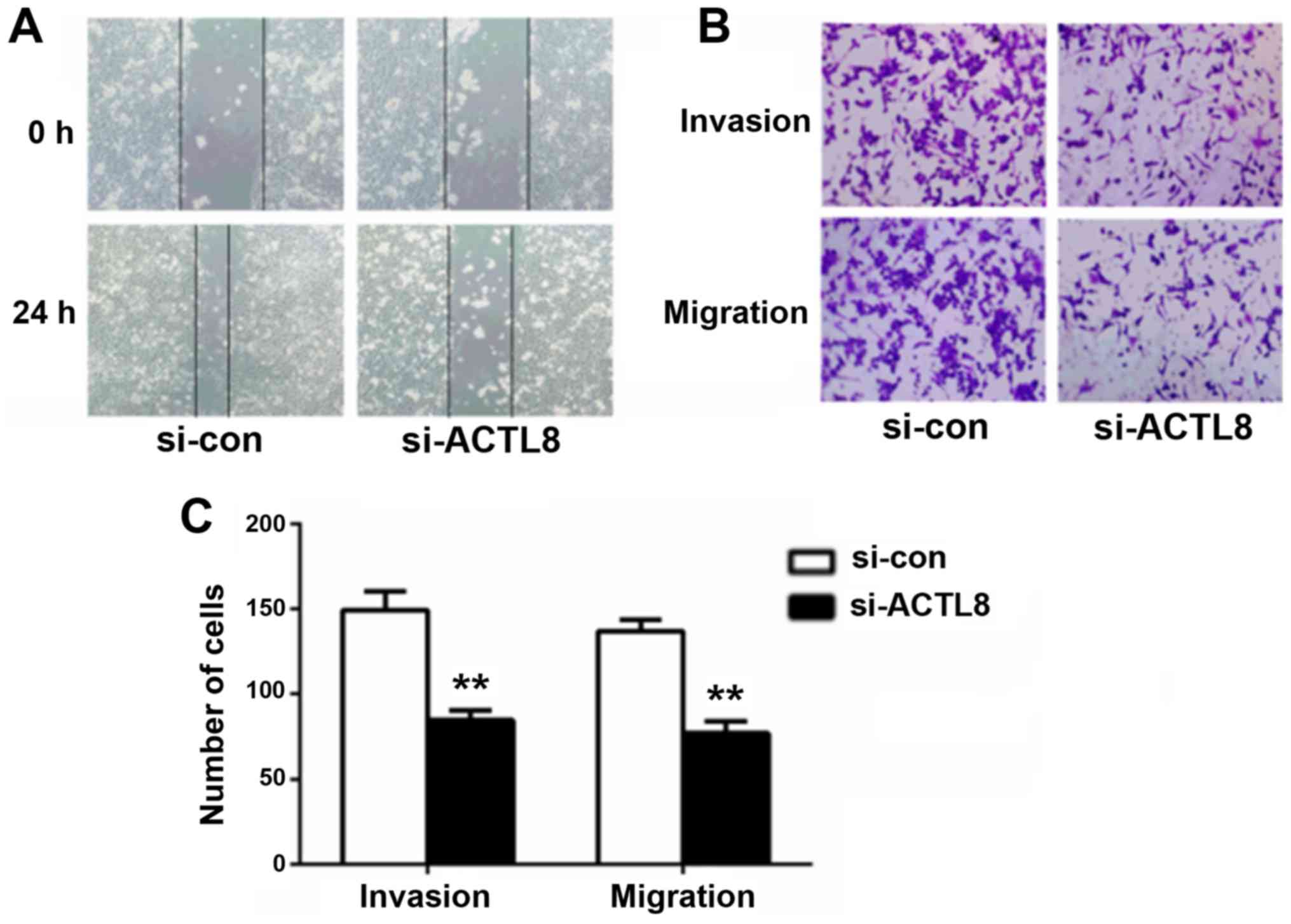
Considering the correlation between ACTL8 expression
and lymph node metastasis in human HNSCC, it can be hypothesized
that ACTL8 may serve a role in the invasion and migration of HNSCC
cells. Therefore, wound healing and transwell assays were conducted
to evaluate the effects of ACTL8 on HNSCC PCI-13 cells metastasis.
Compared with the si-con group, the healing capacity for cells
treated with si-ACTL8 following 24 h artificial scratching was
decreased (P<0.05; Fig. 4A).
The results of the transwell assay in Fig. 4B and C demonstrated that the
numbers of invasive and migrated cells following interference with
ACTL8 siRNA were significantly reduced compared with the
si-con group (P<0.01). ACTL8 knockout efficiently decreased the
invasion and migration capacity in HNSCC cells in vitro.
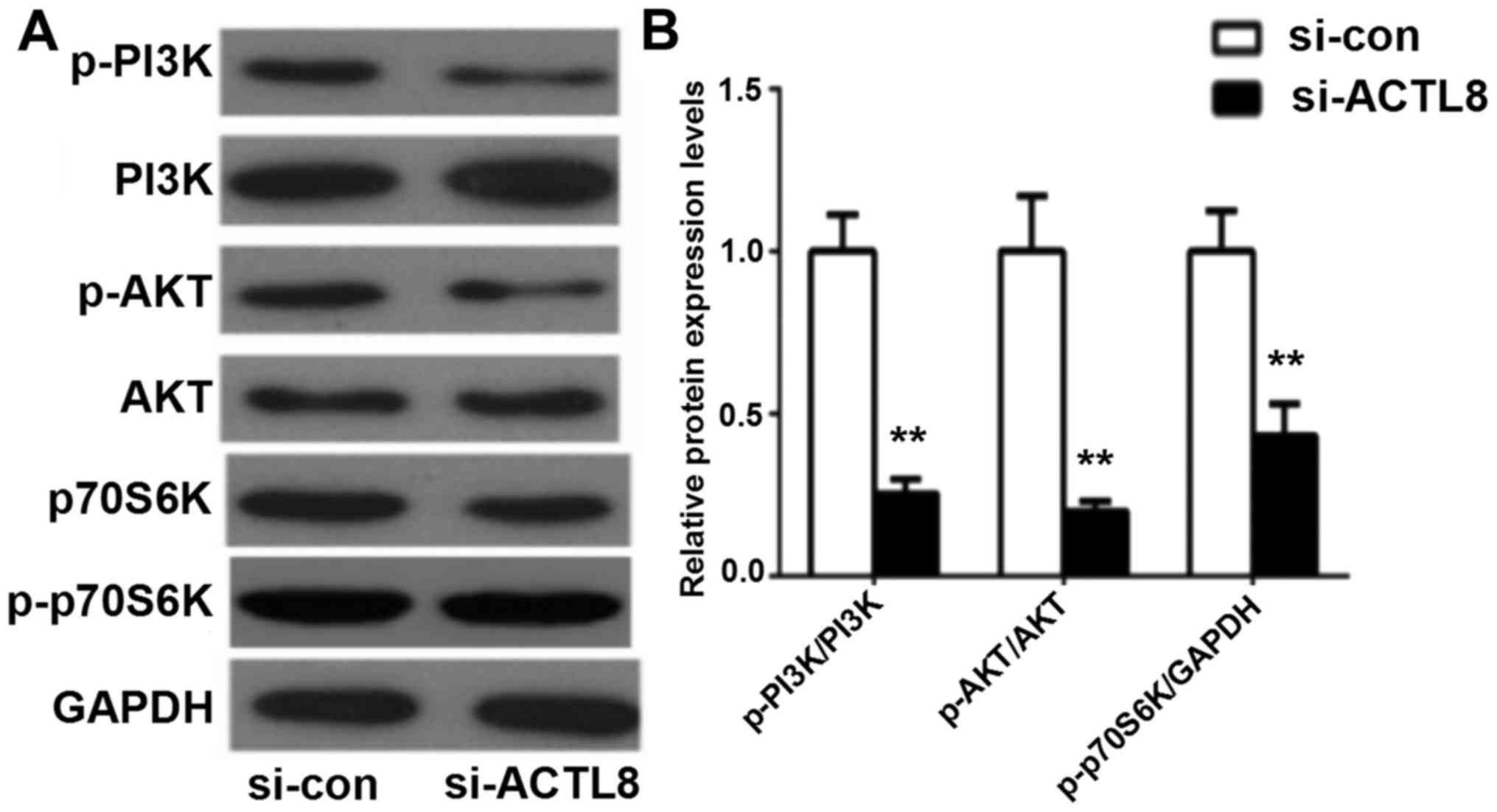
ACTL8 knockout inhibits the activation
of the PI3K/AKT signaling pathway
The above studies indicate that ACTL8 suppressed the
proliferative, invasive and migratory abilities of PCI-13 cells in
HNSCC in vitro, whereas the underlying mechanisms remain
unclear. The dysregulation of the PI3K/AKT signaling pathway is
involved in a number of biological processes of various human
diseases. PI3K/AKT signaling pathway has been reported to be
activated in HNSCC and serve an important role in cell growth and
survival (11). In the present
study, western blotting assay was used to measure the expression of
the key proteins in PI3K/AKT signaling pathway following
transfection of ACTL8 siRNA into the HNSCC PCI-13 cell line.
Western blot results in Fig. 5
revealed that ACTL8 knockout significantly decreased the levels of
phosphorylated PI3K and AKT, as well as p70S6K in PCI-13 cells
compared with the si-con group (all P<0.01). Therefore, these
results suggest that knockdown of ACTL8 may inhibit cell
proliferation, invasion and migration by suppressing the activation
of the PI3K/AKT signaling pathway in PCI-13 cells.
Discussion
HNSCC is one of the most common types of human
cancer worldwide. It has the potential for early metastasis and is
associated with a low survival rate (12). Currently, the prevention of
locoregional tumor relapse is still a major challenge for the
management of advanced HNSCC (13). Therefore, the investigation of
novel prognostic biomarkers is of great importance for preventing
tumor recurrence and metastasis and improving prognosis in patients
with HNSCC (14).
The expression levels of CTA genes have been
reported to be different in different tumor cells and the increased
expression of CTA genes is an indicative of disease progression and
poor prognosis (15,16). Previously, CTA has been considered
as targets of immune responses that were induced by cytotoxic T
cells in certain tumors (17,18).
For example, members of CTA family MAGEA and NY-ESO-1/CTAG1B have
been applied in clinical trials, including lung cancer and melanoma
(19,20). Additionally, Ipilimumab, the
monoclonal antibody of ACTL4, has been used at the clinical trial
phase (21). ACTL8, one of the CTA
family has few studies in tumors. Freitas et al (7) noticed that ACTL8 is highly expressed
in glioblastoma, but has no connection with the patient's survival.
Additionally, Yao et al (8)
studied the expression of the CTA gene ACTL8 in the basal subtype
of breast cancer. However, the association between ACTL8 and
tumorigenesis as well as prognosis in tumors remains unclear.
Therefore, expression levels of ACTL8 in HNSCC were investigated in
this study. The expression of ACTL8 in HNSCC was analyzed from the
collected TCGA datasets and clinical tissue samples. The results
indicated that ACTL8 in HNSCC tissues was highly expressed.
Additionally, high expression in cells was also detected by RT-qPCR
assay. Subsequently, the prognosis analysis was conducted, results
demonstrated that the expression of ACTL8 in HNSCC could be an
independent prediction factor and associated with the lymph node
metastasis and tumor grade. Based on the siRNA strategy, a PCI-13
cell model with ACTL8 knockdown was established to analyze the
functions of ACTL8 in HNSCC. As a result, due to the downregulation
of ACTL8 expression in PCI-13 cells, the proliferation and colony
formation rate of PCI-13 cells was decreased. In addition, the
wound-healing assay and transwell method demonstrated that
knockdown of ACTL8 suppressed the invasive and migratory capacity
of PCI-13 cells. Therefore, all the above results suggest that
ACTL8 can be considered as a potential target for HNSCC
therapy.
The PI3K/AKT signaling pathway is one of the most
important intracellular signaling pathways, which has been
demonstrated to be involved in the proliferation, angiogenesis,
invasion and migration of tumor cells (22). It has been reported that
alterations in crucial proteins of the PI3K/AKT signaling pathway
have been involved in the progression of HNSCC (23). PI3K is an intracellular
phosphatidylinositol kinase involved in various cellular functions,
including cell proliferation, differentiation, apoptosis and growth
(24,25). AKT is an effector protein in the
downstream of PI3K, which has been demonstrated to be important in
carcinogenesis (26). In the
present study, the expression levels of key proteins in PI3K/AKT
signaling pathway were detected using a western blot assay. The
results indicated that the expression levels of phosphorylated PI3K
and AKT were reduced in PCI-13 cells transfected by ACTL8 siRNA. In
addition, the downstream action target of the PI3K/AKT signaling
pathway, p70S6K, serves a crucial role in translation initiation,
cell metastasis, protein synthesis and cell cycle (27,28).
Similarly, the expression levels of p70S6 K in the PI3K/AKT
signaling pathway were deceased following si-ACTL8 transfection in
the present study. These results indicate that ACTL8 may be
involved in HNSCC cell motility via the PI3K/AKT signaling
pathway.
In conclusion, in the present study, ACTL8 was
observed to be highly expressed in HNSCC and was associated with a
poor prognosis. In addition, upon transfecting ACTL8 siRNA into
HNSCC PCI-13 cells, the proliferative, invasive and migratory
capacities of PCI-13 cells were inhibited, which may be associated
with the inhibition of the activation of the PI3K/AKT signaling
pathway. These results indicate that high expression of ACTL8
promotes the proliferation, invasion and migration of PCI-13 cells.
Therefore, ACTL8 may be a potential prognosis marker and a novel
therapeutic target for human HNSCC.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
BL and LM designed the study, and wrote and revised
the manuscript. BL and JZ performed the study and analyzed the
data. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The present study obtained the informed consent of
all patients and was approved by the Jinan Central Hospital
Affiliated to Shandong University Medical Ethics Committee.
Patient consent for publication
The present study obtained the informed consent of
all patients.
Competing interests
The authors declare they have no competing
interests.
References
|
1
|
Agrawal N, Frederick MJ, Pickering CR,
Bettegowda C, Chang K, Li RJ, Fakhry C, Xie TX, Zhang J, Wang J, et
al: Exome sequencing of head and neck squamous cell carcinoma
reveals inactivating mutations in NOTCH1. Science. 333:1154–1157.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Pries R, Nitsch S and Wollenberg B: Role
of cytokines in head and neck squamous cell carcinoma. Expert Rev
Anticancer Ther. 6:1195–1203. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Stacy DR, Ely K, Massion PP, Yarbrough WG,
Hallahan DE, Sekhar KR and Freeman ML: Increased expression of
nuclear factor E2 p45-related factor 2 (NRF2) in head and neck
squamous cell carcinomas. Head Neck. 28:813–818. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Scanlan MJ, Simpson AJ and Old LJ: The
cancer/testis genes: Review, standardization and commentary. Cancer
Immun. 4:12004.PubMed/NCBI
|
|
5
|
Phuphanich S, Wheeler CJ, Rudnick JD,
Mazer M, Wang H, Nuño MA, Richardson JE, Fan X, Ji J, Chu RM, et
al: Phase I trial of a multi-epitope-pulsed dendritic cell vaccine
for patients with newly diagnosed glioblastoma. Cancer Immunol
Immunother. 62:125–135. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Atanackovic D, Blum I, Cao Y, Wenzel S,
Bartels K, Faltz C, Hossfeld DK, Hegewisch-Becker S, Bokemeyer C
and Leuwer R: Expression of cancer-testis antigens as possible
targets for antigen-specific immunotherapy in head and neck
squamous cell carcinoma. Cancer Biol Ther. 5:1218–1225. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Freitas M, Malheiros S, Stávale JN, Biassi
TP, Zamunér FT, de Souza Begnami M, Soares FA and Vettore AL:
Expression of cancer/testis antigens is correlated with improved
survival in glioblastoma. Oncotarget. 4:636–646. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yao J, Caballero OL, Yung WK, Weinstein
JN, Riggins GJ, Strausberg RL and Zhao Q: Tumor subtype-specific
cancer-testis antigens as potential biomarkers and
immunotherapeutic targets for cancers. Cancer Immunol Res.
2:371–379. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Jin Y, Jin C, Wennerberg J, Mertens F and
Höglund M: Cytogenetic and fluorescence in situ hybridization
characterization of chromosome 1 rearrangements in head and neck
carcinomas delineate a target region for deletions within
1p11-1p13. Cancer Res. 58:5859–5865. 1998.PubMed/NCBI
|
|
10
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Giudice FS and Squarize CH: The
determinants of head and neck cancer: Unmasking the PI3K pathway
mutations. J Carcinog Mutagen. (Suppl 5):(pii): 0032013.PubMed/NCBI
|
|
12
|
Nohata N, Sone Y, Hanazawa T, Fuse M,
Kikkawa N, Yoshino H, Chiyomaru T, Kawakami K, Enokida H, Nakagawa
M, et al: miR-1 as a tumor suppressive microRNA targeting TAGLN2 in
head and neck squamous cell carcinoma. Oncotarget. 2:29–42. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
De Castro G, Dos Anjos CH, Lalami Y and
Awada A: Clinical trial design in advanced head and neck cancer:
From past experiences to future perspectives. Clin Invest.
2:473–481. 2012. View Article : Google Scholar
|
|
14
|
Le Tourneau C, Faivre S and Siu LL:
Molecular targeted herapy of head and neck cancer: Review and
clinical development challenges. Eur J Cancer. 43:2457–2466. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Dhodapkar MV, Osman K, Teruya-Feldstein J,
Filippa D, Hedvat CV, Iversen K, Kolb D, Geller MD, Hassoun H,
Kewalramani T, et al: Expression of cancer/testis (CT) antigens
MAGE-A1, MAGE-A3, MAGE-A4, CT-7 and NY-ESO-1 in malignant
gammopathies is heterogeneous and correlates with site, stage and
risk status of disease. Cancer Immun. 3:92003.PubMed/NCBI
|
|
16
|
Balafoutas D, Zur HA, Mayer S, Hirschfeld
M, Jaeger M, Denschlag D, Gitsch G, Jungbluth A and Stickeler E:
Cancer testis antigens and NY-BR-1 expression in primary breast
cancer: Prognostic and therapeutic implications. BMC Cancer.
13:2712013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Taylor M, Bolton LM, Johnson P, Elliott T
and Murray N: Breast cancer is a promising target for vaccination
using cancer-testis antigens known to elicit immune responses.
Breast Cancer Res. 9:R462007. View
Article : Google Scholar : PubMed/NCBI
|
|
18
|
Atanackovic D, Arfsten J, Cao Y, Gnjatic
S, Schnieders F, Bartels K, Schilling G, Faltz C, Wolschke C,
Dierlamm J, et al: Cancer-testis antigens are commonly expressed in
multiple myeloma and induce systemic immunity following allogeneic
stem cell transplantation. Blood. 109:1103–1112. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Atanackovic D, Altorki NK, Cao Y, Ritter
E, Ferrara CA, Ritter G, Hoffman EW, Bokemeyer C, Old LJ and
Gnjatic S: Booster vaccination of cancer patients with MAGE-A3
protein reveals long-term immunological memory or tolerance
depending on priming. Proc Natl Acad Sci USA. 105:1650–1655. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Fourcade J, Sun Z, Pagliano O, Chauvin JM,
Sander C, Janjic B, Tarhini AA, Tawbi HA, Kirkwood JM, Moschos S,
et al: PD-1 and Tim-3 regulate the expansion of tumor
antigen-specific CD8+ T cells induced by melanoma
vaccines. Cancer Res. 74:1045–1055. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Postow MA, Luke JJ, Bluth MJ, Ramaiya N,
Panageas KS, Lawrence DP, Ibrahim N, Flaherty KT, Sullivan RJ, Ott
PA, et al: Ipilimumab for patients with advanced mucosal melanoma.
Oncologist. 18:726–732. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Britschgi A, Andraos R, Brinkhaus H,
Klebba I, Romanet V, Müller U, Murakami M, Radimerski T and
Bentires-Alj M: JAK2/STAT5 Inhibition circumvents resistance to
PI3K/mTOR blockade: A rationale for cotargeting these pathways in
metastatic breast cancer. Cancer Cell. 22:796–811. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Yang S, Ji Q, Chang B, Wang Y, Zhu Y, Li
D, Huang C, Wang Y, Sun G, Zhang L, et al: STC2 promotes head and
neck squamous cell carcinoma metastasis through modulating the
PI3K/AKT/Snail signaling. Oncotarget. 8:5976–5991. 2017.PubMed/NCBI
|
|
24
|
Zheng W, Nagaraju G, Liu Z and Liu K:
Functional roles of the phosphatidylinositol 3-kinases (PI3Ks)
signaling in the mammalian ovary. Mol Cell Endocrinol. 356:24–30.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Okkenhaug K and Vanhaesebroeck B: PI3K in
lymphocyte development, differentiation and activation. Nat Rev
Immunol. 3:317–330. 2003. View
Article : Google Scholar : PubMed/NCBI
|
|
26
|
Yuan TL and Cantley LC: PI3K pathway
alterations in cancer: Variations on a theme. Oncogene.
27:5497–5510. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zhao XF and Gartenhaus RB: Phospho-p70S6K
and cdc2/cdk1 as therapeutic targets for diffuse large B-cell
lymphoma. Expert Opin Ther Targets. 13:1085–1093. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Wang F, Qiu Y, Zhang HM, Hanson P, Ye X,
Zhao G, Xie R, Tong L and Yang D: Heat shock protein 70 promotes
coxsackievirus B3 translation initiation and elongation via
Akt-mTORC1 pathway depending on activation of p70S6K and Cdc2. Cell
Microbiol. 2017. View Article : Google Scholar :
|