Introduction
In recent years, acellular matrix scaffolds have
shown great potential in animal studies (1). Decellularized tissue grafts have been
used to promote regeneration of certain systems, including the skin
(2), liver (3), bone (4), heart (5), ovaries (6), cartilage (7) and peripheral nerves (8); however, few studies have attempted to
explore their potential in central nervous system repair (9). Our previous studies used a chemical
extraction method, involving Triton X-100 and sodium deoxycholate,
to successfully prepare acellular scaffolds (10,11).
The prepared acellular spinal cord scaffold has a three-dimensional
structure and excellent biocompatibility; however, the chemical
extraction method used to achieve complete decellularization was
unstable in early experiments. Notably, this method is capable of
inducing complete decellularization; however, it has a low
efficiency. Therefore, in order to improve decellularization and
efficiency, the preparation of acellular spinal cord stents must be
improved.
Stem cells are an alternative source of functional
nerve cells (12). Growing
evidence has suggested that stem cells can differentiate into
neuron-like cells in the appropriate microenvironment and when
stimulated by nerve growth factors (13,14).
Rat bone marrow mesenchymal stem cells (BMSCs) are a type of adult
stem cell; these cells are suitable for cell therapy, due to their
availability, rapid proliferation, pluripotency, successful
integration and innate tolerance in the host tissue (15). In addition, it has been reported
that BMSCs, under stimulation by the nourishing factors
neurotrophin-3 (NT-3), basic fibroblast growth factor (bFGF) and
epidermal growth factor (EGF), may differentiate into neuronal
cells, as verified by neuron-specific antibodies (14). However, the method by which BMSCs
differentiate into neuronal cells only be assessed in a limited way
in the two dimensions of cell culture plates, and how to
successfully cultivate acellular spinal cord stents requires
further investigation.
The present study hypothesized that 3D acellular
scaffolds derived from the rat spinal cord may provide a simulated
natural spinal microenvironment that facilitates the
differentiation of BMSCs into neuron-like cells in vitro.
Furthermore, compared with in the traditional stent group, the
benefits of the improved EDC crosslinking scaffold on BMSC adhesion
and differentiation were investigated. Furthermore, in this study,
an improved dynamic culture system with added trophic factors was
used to control the environmental conditions. Reverse
transcription-quantitative PCR (RT-qPCR) and immunostaining were
used to determine MSC differentiation into neuron-like cells. In
addition, scaffolds were surgically inserted into a rat model to
study their immunogenicity.
Materials and methods
Scaffold preparation and experimental
groups
Adult male SD rats, 50 days old, were purchased from
the animal center of Daping Hospital affiliated Army Medical
University (n=30; weight, ~250 g). The rats were housed at a
temperature of 25±1°C with a 12 h light/dark cycle, and access to
food and water was ad libitum. In the normal group, rats
were administered pentobarbital sodium (45 mg/kg body weight) via
intraperitoneal injection, after which ~20 mm of the thoracic
spinal cord was obtained from each animal. Spinal cord samples were
immersed in PBS (0.01 mol/l), washed clean of blood and then stored
at −70°C.
The traditional stent group was generated according
to a method previously described by Guo et al (10). Thoracic spinal cords were harvested
in the same manner as for the normal group. After gradient thawing
(−70, −20 and 4°C) the spinal cords were rinsed twice in a desktop
thermostat oscillator (25°C; 100 rpm 1 h/wash) in PBS.
Subsequently, PBS was replaced with 1% Triton X-100 (Sigma-Aldrich;
Merck KGaA) solution. The spinal cords were rinsed for 3 h at 25°C
with agitation, and were then rinsed again with washing solution
(0.01% PBS) three times (1 h/rinse). The solution was then replaced
with 1% sodium deoxycholate solution (Sigma-Aldrich; Merck KGaA)
for 3 h at 25°C with agitation. After this, the spinal cords were
rinsed with washing solution with agitation at 25°C three times (1
h/rinse). The nerve segments were again agitated in 1% Triton X-100
and 1% sodium deoxycholate solution. Finally, the segments were
washed a further three times at 25°C with agitation (1 h/wash) in a
0.01% PBS solution. The tissue segments were finally stored at
−20°C.
In the improved stents group, the following steps
were conducted: i) The thoracic spinal cord samples were extracted
according to the aforementioned method, and were immediately placed
in 1.5 ml microcentrifuge tubes. ii) The tubes were then placed in
liquid nitrogen for 2 min and placed in a water bath at 42°C for 8
min; ultra-pure water was added for 50 min and replaced every 25
min. iii) The ultra-pure water was removed and 1% Triton X-100 was
added to the samples and incubated for 12 h at 25°C; iv) ultra-pure
water was then added again for 30 min and incubated at 25°C, the
water was replaced every 10 min prior to being discarded. v) 1%
sodium deoxycholate was added and incubated for 12 h at 25°C, and
vi) ultra-pure water was added for 30 min and incubated at 25°C,
the water was replaced every 10 min. vii) EDC liquid (EDC:NHS, 5:2;
0.01 mol/l PBS, 0.5 g EDC and 0.2 g NHS; Sigma-Aldrich; Merck KGaA)
was added to the samples at room temperature for 10 h. Finally,
steps iii)-iv) were repeated in a desktop thermostat oscillator
(100 rpm) and all acellular spinal cord stents were stored at
−20°C.
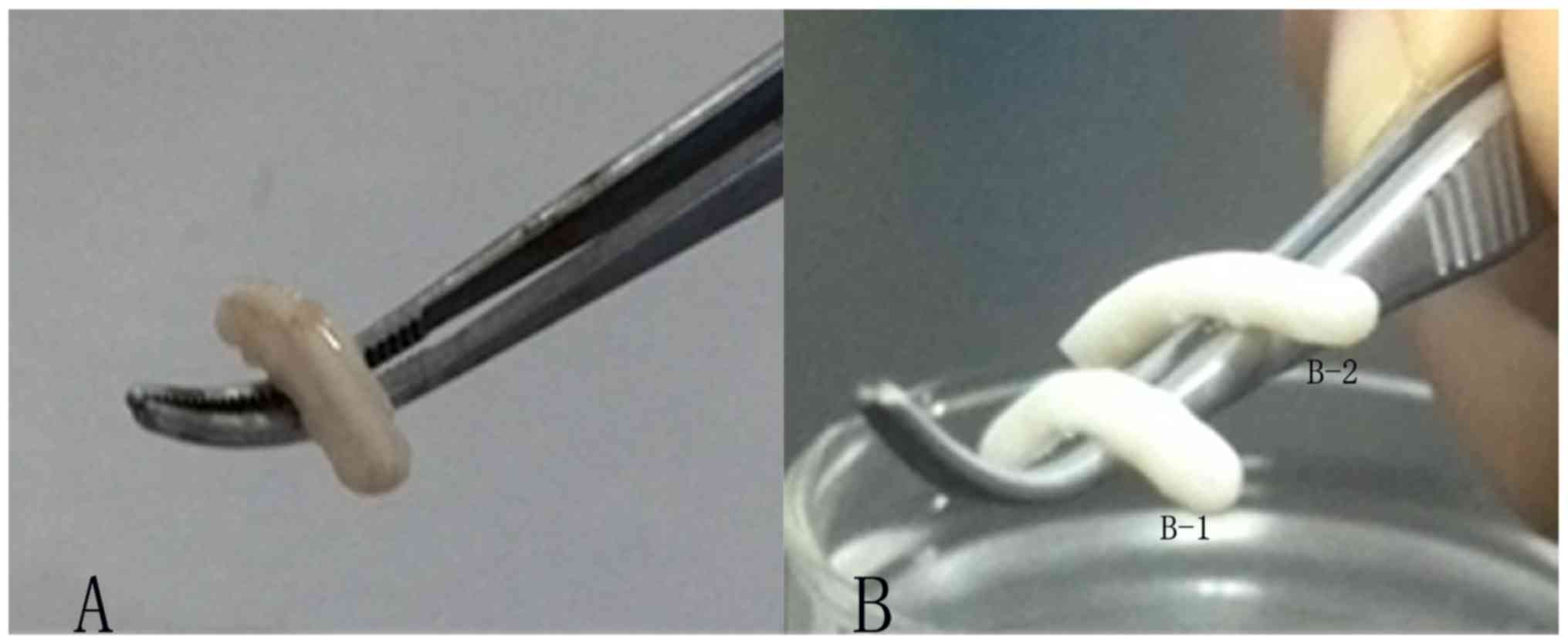
Gross morphology
The scaffolds obtained from all three groups were
observed and assessed for normal morphology, color, texture and
stiffness.
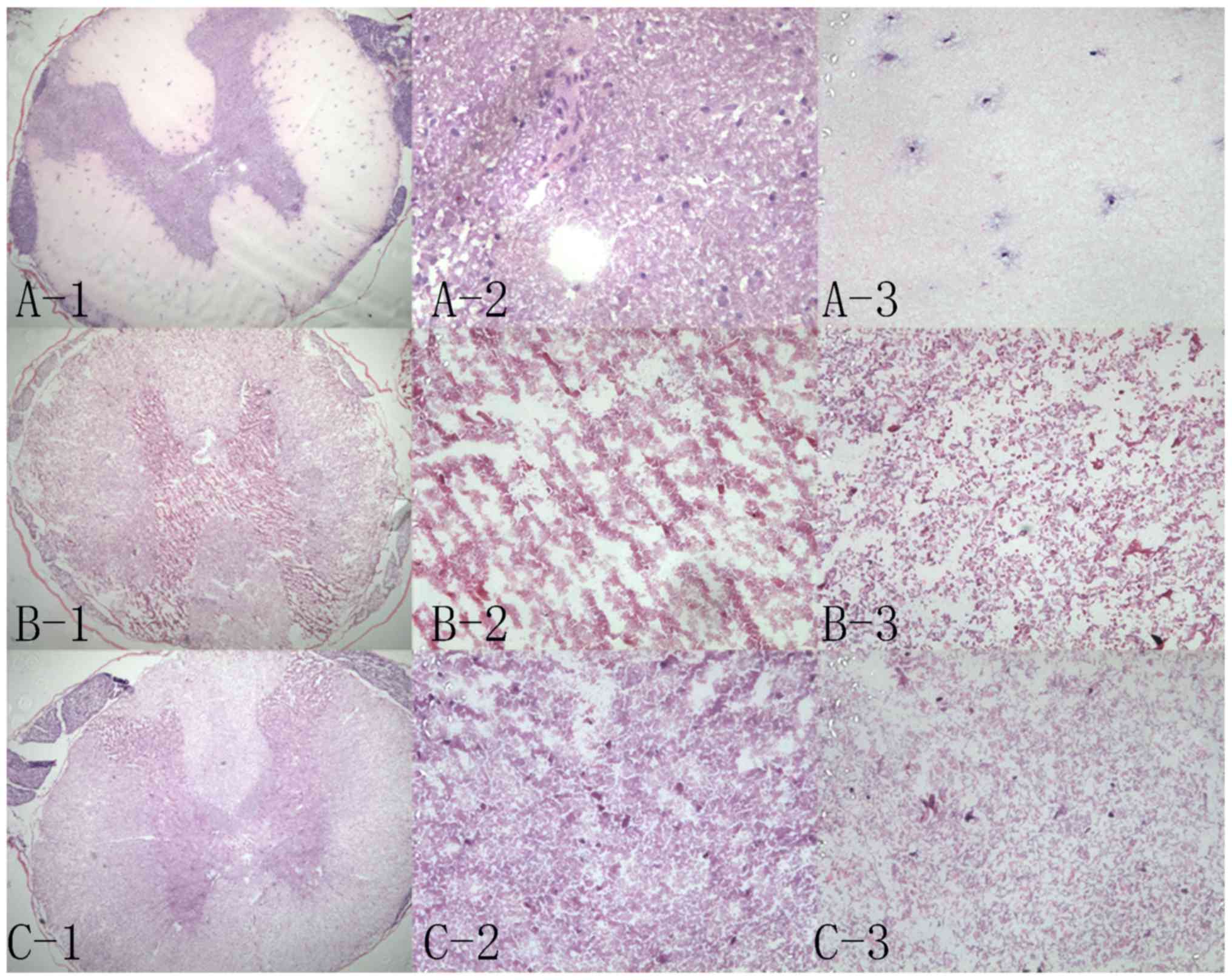
Hematoxylin and eosin (H&E)
staining
Scaffolds from the three groups (n=20/group) were
fixed with 4% paraformaldehyde (Beyotime Institute of
Biotechnology) for 1 h at 25°C, dehydrated and frozen; these
sections then underwent H&E staining. Residual cells and
external matrix retention was observed under an optical microscope
(magnification, ×50 and ×400). Cell residue evaluation criteria
were as follows: No residue or little debris, grade I; 1–5 residual
cells, grade II; 5–10 residual cells, grade III; >10 residual
cells, grade IV.
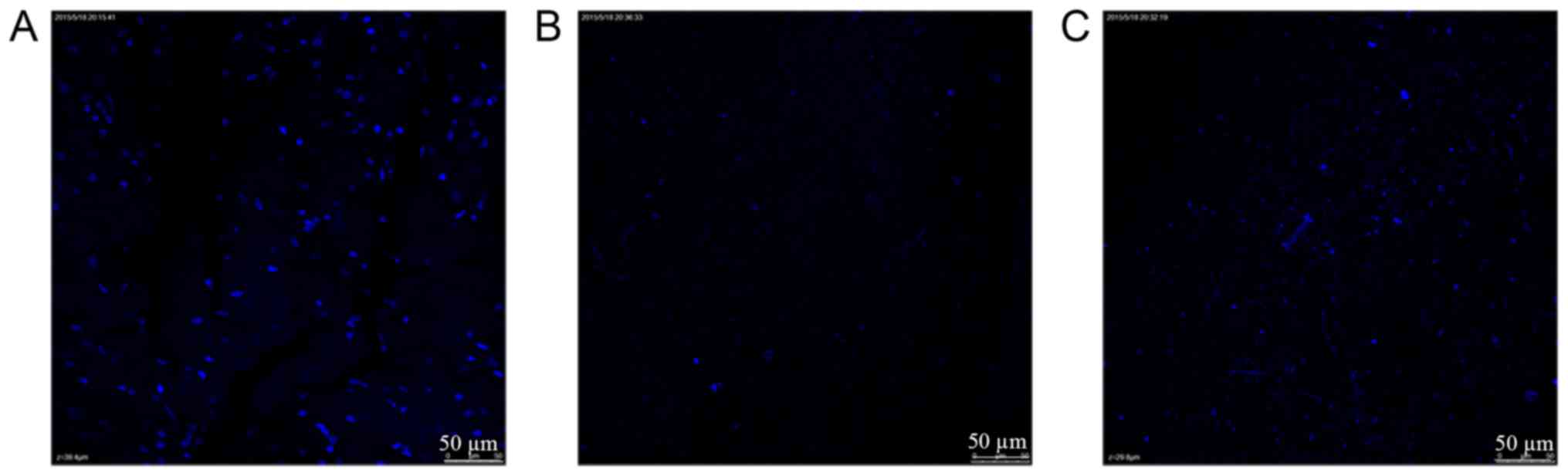
DAPI staining
Randomly selected normal spinal cord samples and
grade I scaffolds were placed in a 24-well plate, and treated as
follows: i) To each well, 2 ml 4% paraformaldehyde was added and
the scaffolds were fixed at room temperature for 30 min; ii)
paraformaldehyde was then removed and 2 ml 0.01 mol/l PBS was added
to a 24 well plate with agitation, which was rinsed for 5 min, the
PBS was discarded, and the process repeated. iii) Subsequently, 5
µg/ml DAPI (Sigma-Aldrich; Merck KGaA) was added to each well, the
plate was covered and incubated in the dark for 5 min at room
temperature; iv) DAPI was discarded and 2 ml 0.01 mol/l PBS was
added to each well with slight agitation, after which the plate was
rinsed for 10 min; this step was repeated until no more dye could
be removed. Cell residue was observed in random fields of view
using a Leica laser confocal microscope (Leica Microsystems GmbH)
and a normal light microscope. The present study verified whether
there was cell residue inside the scaffold.
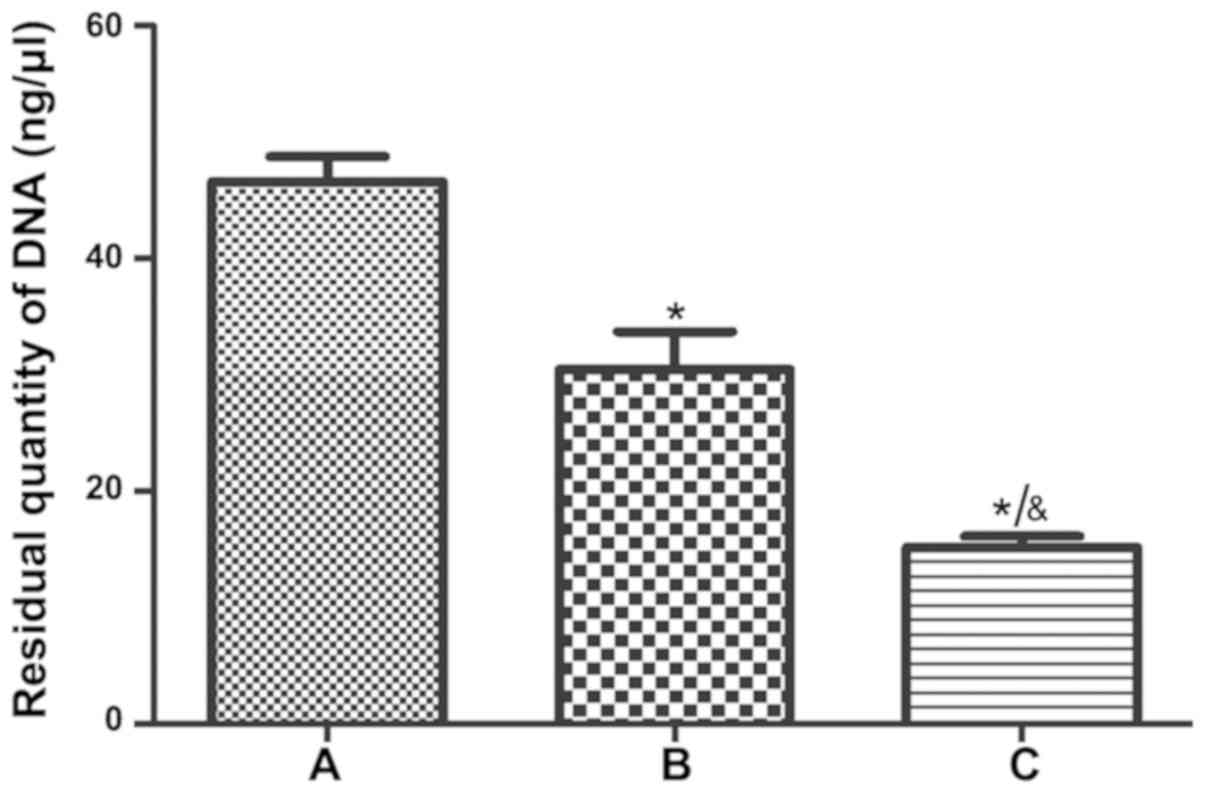
Detection of residual DNA content
A total of 10 scaffolds (300 µg) were selected from
each of the three groups, and were sorted after mixing and grinding
using a glass homogenizer; ~1/10 of the mixture was used to detect
DNA, according to the manufacturer's protocol (HiPure Tissue DNA
Mini kit; cat. no. D3121-02; Guangzhou Meiji Biotechnology Co.,
Ltd.). Briefly, the samples underwent the following steps: i)
Digestion and cleavage, and ii) column purification. The DNA
samples from the three groups were then subjected to DNA analysis
using a spectrophotometer (ND-2000C; NanoDrop Technologies; Thermo
Fisher Scientific, Inc.), according to the manufacturer's protocol.
The scaffolds underwent DNA extraction a further two times to
obtain another two batches of DNA; each batch of DNA was assessed
three times to obtain the mean, which was then used for statistical
analysis.
Scanning electron microscopy (SEM)
analysis of the scaffold ultrastructure
Scaffolds from the three groups were fixed in
glutaraldehyde (20 g/l) at 4°C for 1 h and the surface was exposed
to the following steps: Dehydration in graded ethanol series (30,
50, 70, 90, 95 and 100% each for 10 min); critical point drying and
spray-gold treatment. Images of the 3D ultrastructure of the
scaffolds were captured by SEM (Hitachi, Ltd.).
Scaffold immunogenicity analysis in
vivo
Bilateral surgery was conducted on 24 rats as
follows: Anesthesia was induced via an intraperitoneal injection of
sodium pentobarbital (30 mg/kg). At the surgical incision site on
the back, the skin was shaved and disinfected with iodophor
solution, after which, a 10-mm skin incision was made. A cavity was
made via blunt dissection. Scaffolds from the traditional and
improved groups were then implanted into the skin incision. Wounds
were sutured using cotton. At 1, 2, 3 and 4 weeks, tissues around
the stent that exhibited inflammation, and the residual stent, were
surgically obtained; the penetration of CD4+ cells into
the grafts was analyzed by immunohistochemistry. Tissues were
prepared from 5 µm frozen sections, were fixed with 4%
paraformaldehyde for 15 min at 25°C and 0.25% Triton was used to
permeabilize cells (10 min). Cells were washed twice with PBST and
blocked with 3% H2O2 (25°C for 30 min).
Antibodies used were as follows: CD4 monoclonal antibody (1:200;
cat. no. YM3070; ImmunoWay Biotechnology Company) and a goat
anti-mouse IgG horseradish peroxidase polymer secondary antibody
(1:500; cat. no. PV6002; OriGene Technologies, Inc.). Images were
captured using an Olympus light microscope (×400).
Culture of BMSCs with additional
trophic factors
A BMSC strain (RASMX-01001) was purchased directly
from Cyagen US, Inc. and cultured at 37°C in DMEM/F12 (HyClone; GE
Healthcare Life Sciences) containing 10% fetal bovine serum (FBS;
Gibco; Thermo Fisher Scientific, Inc.) and 0.2% ascorbic acid in an
incubator containing 5% CO2; the medium was changed
every 3 days. Cells were digested with 0.25% trypsin (HyClone; GE
Healthcare Life Sciences). Subsequently, the slides were
pre-embedded in polylysine (cat. no. P6407; Sigma-Aldrich; Merck
KGaA) and laminin (cat. no. L6274; Sigma-Aldrich; Merck KGaA),
placed in 24-well plates and cell culture medium was added. A
passage 5 MSC cell suspension was then added to the 24-well plate
at a concentration of 2×105. The medium was replaced
once cells reached 80% confluence. The experimental group was
cultured in 3 ml low-glucose DMEM (HyClone; GE Healthcare Life
Sciences) + 10 ng/ml NT-3 (cat. no. 450-3; Peprotech, Inc.) + 10
ng/ml bFGF (cat. no. 400-29; Peprotech, Inc.) + 10 ng/ml EGF (cat.
no. AF-400-25; Peprotech, Inc.) + 2% FBS (Gibco; Thermo Fisher
Scientific, Inc.) + 1% penicillin-streptomycin (HyClone; GE
Healthcare Life Sciences) + 1% N2 (Gibco; Thermo Fisher Scientific,
Inc.) + 1% glutamine (HyClone; GE Healthcare Life Sciences). The
control group was cultured with 3 ml low-glucose DMEM + 2% FBS + 1%
penicillin-streptomycin + 1% N2 + 1% glutamine. All groups were
cultured for 7 days.
BMSC adherence to scaffolds
The traditional and improved groups of acellular
spinal cord scaffolds are referred to as the traditional group and
improved group, respectively. Briefly, in the traditional and
improved groups, four scaffolds were analyzed. The stents were
trimmed to 1 cm, and incubated in PBS solution for 48 h at 4°C to
remove residual chemicals. Subsequently, the stents were
freeze-dried and stored in a sealed microcentrifuge tube, prior to
undergoing 60Co irradiation disinfection (dose, 16 Gy)
for sterilization; the stents were then stored at −20°C. Passage 3
BMSCs were selected for this analysis and were adjusted to a cell
density to 3.7×105/ml. Subsequently, sterilized stents
were placed in 24-well plates, and a micro-sampler was used to
inject 40 µl cell suspension into the interior and also onto the
surface, after which, 50 µl complete medium [DMEM/F12 (HyClone; GE
Healthcare Life Sciences) + 10% FBS (Gibco; Thermo Fisher
Scientific, Inc.) + 1% penicillin-streptomycin] was added and
incubated at 37°C for 4 h. Stents were then rinsed with PBS three
times, and fixed in 2 ml 4% paraformaldehyde at room temperature
for 30 min. Subsequently, the paraformaldehyde was discarded and
the stents were rinsed with PBS for a further three times. DAPI
(500 µl) was then added to each well for staining and the samples
were incubated in the dark for 5 min, before being rinsed a further
three times with PBS. Finally, a laser confocal microscope (Leica
Microsystems GmbH) was used to evaluate DAPI staining and
absorption. Each cell composite scaffold was imaged in three random
fields, and the average number of cells per field was
calculated.
Cell growth in scaffolds
The traditional and improved groups were evaluated
for cell differentiation (16).
Briefly, stents were pre-sterilized with 16 Gy 60Co
irradiation. The slides were pre-incubated with lysine
(Sigma-Aldrich; Merck KGaA) and laminin (Sigma-Aldrich; Merck
KGaA), and placed into a 24-well plate; the scaffolds were cut and
flattened suitably and were bonded with the cell slide via tissue
adhesion (cat. no. LOT215503N1; B.BRAUN AG). In addition, equal
weight scaffolds were adhered to a 6-well plate without the cell
slide, using the aforementioned method; the combination of
scaffolds and plates were pretreated with DMEM/F12 for 30 min prior
to seeding the scaffolds with cells. For the 24-well plates, a 3 µl
4×105 BMSC suspension was added directly to each well;
for the 6-well plates, a 20 µl 4×105 cell suspension was
seeded into each well. To promote cell adhesion, the plates were
incubated for 2 h at 37°C in a humidified atmosphere containing 5%
CO2, then 0.4 ml DMEM/F12 + 10% FBS was added to each
well of the 24-well plate, and 3 ml each well of the 6-well plate.
Plates were incubated for 72 h, prior to the addition of 0.4 ml
neurogenic induction medium (DMEM/low glucose + 2% FBS + 1% 10
ml/ml NT-3 + bFGF + EGF) to each well of the 24-well plates, and 3
ml to each well of the 6-well plates; the plates were incubated at
37°C for 7 days. The 24-well plates were used for
immunofluorescence. Cells grown in 6-well plates were digested,
washed and filtered, and then subjected to RT-qPCR analysis.
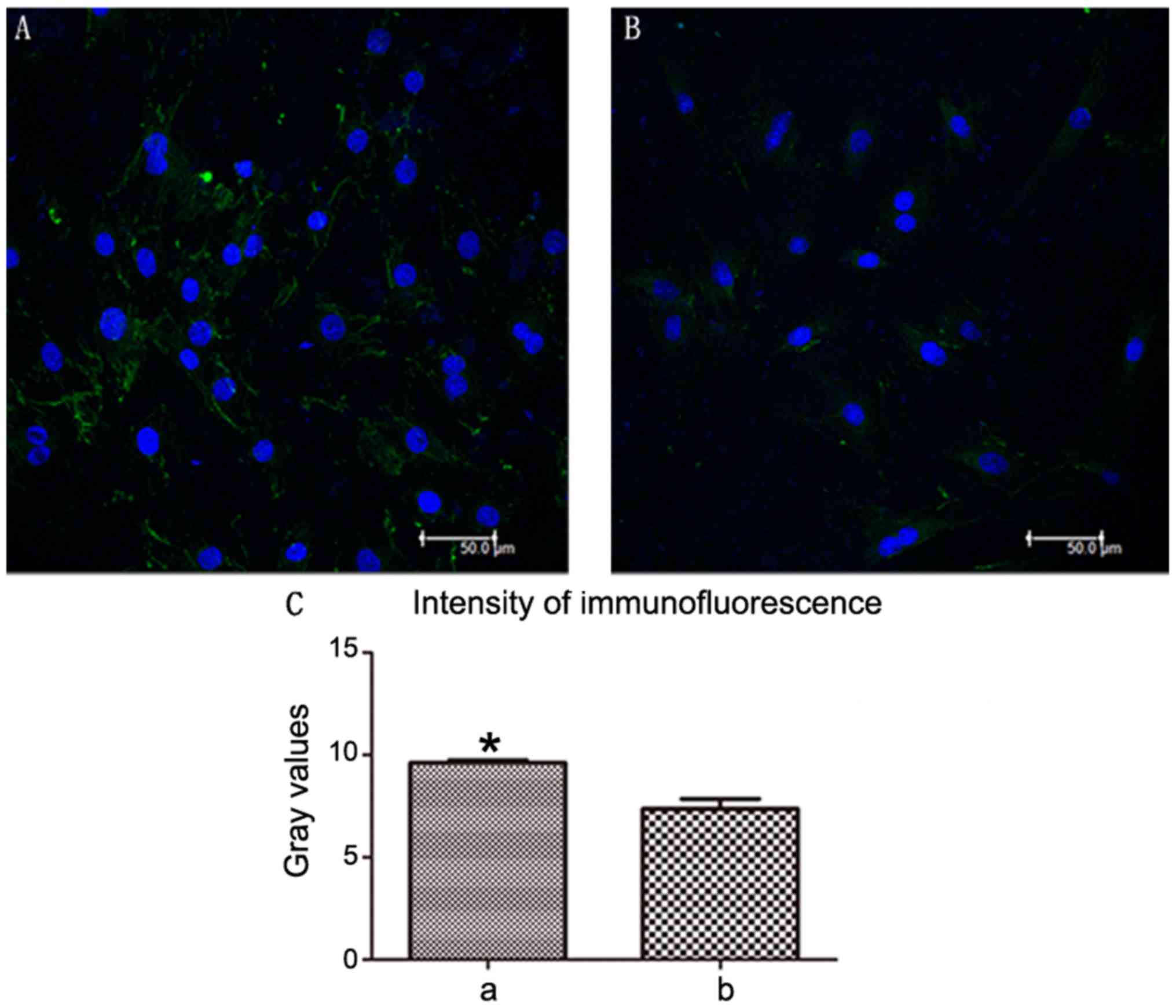
Cell differentiation in scaffolds
Cell differentiation in the scaffolds of the two
groups was analyzed by confocal microscopy. Briefly, cell-seeded
scaffolds (according to the aforementioned procedure) were washed
with PBS and fixed in 3.7% formaldehyde at 25°C for 20 min.
Subsequently, they were immersed in 0.1% Triton X-100 for 3 min and
washed again in PBS. The samples were stained overnight with a
primary antibody against Neurofilament heavy (Nefh; 1:50; cat. no.
ab82259; Abcam) at 4°C. Excess primary antibody was removed and the
scaffolds were washed three times in PBS, then incubated with an
Andy Fluor™ 488 goat anti-mouse IgG (H+L) antibody (1:100; cat. no.
L109A; GeneCopoeia, Inc.) at room temperature for 4 h. In addition,
cell nuclei were labeled with 20 mg/ml DAPI in the dark for 5 min.
Imaging experiments were performed under laser confocal microscopy
(Leica TCS SP5; Leica Microsystems GmbH). Integrated Performance
Primitives software (Intel Corporation) was used to select the
fluorescent region around each cell; five cells were randomly
selected from each image. The grayscale value was obtained by
calculating the brightness ratio of the area, which was done
automatically using the software. Average grayscale values were
obtained for each image. Each group had three average grayscale
values and these were plotted as a graph using GraphPad Prism 5.01
(GraphPad Software, Inc.).
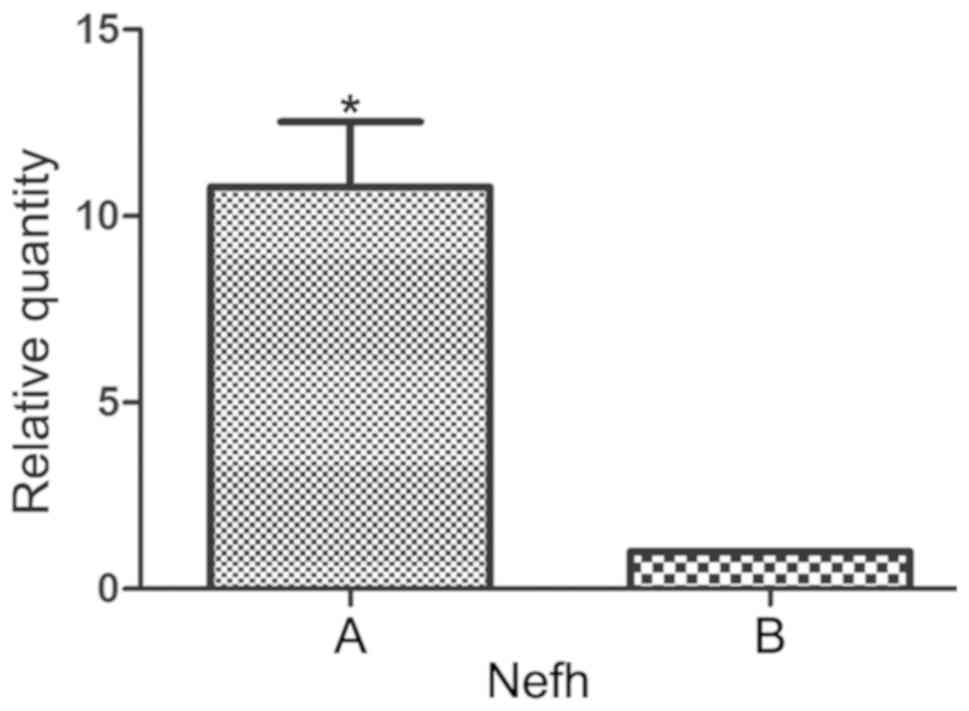
RT-qPCR analysis of cell
differentiation
Cells grown in 6-well plates from the two groups
were washed and RNA was extracted using RNAzol (GeneCopoeia, Inc.).
According to the manufacturer's protocol, an All-In-One™
First-Strand cDNA Synthesis kit (cat. no. AORT-0020; GeneCopoeia,
Inc.) was used for RT. Briefly, 1 µg total RNA was used for DNA
synthesis. qPCR was performed as follows: Initial denaturation at
95°C for 10 min; followed by 40 cycles at 95°C for 10 sec, 60°C for
20 sec and 72°C for 34 sec using an ViiA 7 Dx RT-PCR system
(Applied Biosystems; Thermo Fisher Scientific, Inc.). The mRNA
expression levels of GAPDH were used as an internal control.
Changes in expression were determined using the 2−ΔΔCq
method (17). The primer sequences
used included: Nefh (2 µM; cat. no. RQP048942; GeneCopoeia, Inc.)
and GAPDH (2 µM; cat. no. HQP006940; GeneCopoeia, Inc.).
Statistical analysis
Data are expressed as the mean ± standard deviation.
SPSS version 19 software (IBM Corp.) was used to analyze the data.
Comparisons among multiple groups were performed using one-way
ANOVA followed by Tukey's post hoc test. Comparisons between two
groups were performed using independent t-test. Comparisons between
two categorical variables were performed using χ2 test.
P<0.05 was considered to indicate a statistically significant
difference.
Results
General morphology
The morphology of the three groups was cylindrical,
milky white, with a certain degree of stiffness. Compared with the
stiffness of the normal spinal cord (Fig. 1A), the traditional (Fig. 1B-1) and improved groups (Fig. 1B-2) appeared weaker. However, the
improved group (Fig. 1B-2)
appeared slightly stronger than the traditional group (Fig. 1B-1).
Histological analysis
Results of H&E staining demonstrated that the
tissue structure of the normal spinal cord was compact (Fig. 2A-1); there were numerous neuronal
cells in the gray matter (Fig.
2A-2) and fewer neuronal cells in the white matter (Fig. 2A-3). The traditional group
exhibited a few cells in the local region (Fig. 2C-1-3), particularly in the central
area (Fig. 2C-2). Conversely, the
white matter was completely decellularized (Fig. 2C-3). The improved group (Fig. 2B-1-3) demonstrated superior
decellularization in the central area (Fig. 2B-2). For the two groups, 20 samples
were randomly selected. Using H&E scoring, the residual cells
in the cross-sections from all scaffolds were analyzed. In the
majority of improved scaffolds, there were ≤5 residual cells,
including in the gray and white matter; ~95% of scaffolds were
grade I+II. Conversely, in the majority of traditional scaffolds,
there were >10 residual cells; only 10% of scaffolds were grade
I+II (Table I). There was a
significant difference between the number of grade I+II scaffolds
in the traditional and improved groups (P<0.05).
 | Table I.Cell residue evaluation by
hematoxylin and eosin staining. |
Table I.
Cell residue evaluation by
hematoxylin and eosin staining.
| Group | Grade I | Grade II | Grade III | Grade IV | Grade I+II rate
(%) |
|---|
| Traditional | 1 | 1 | 0 | 18 | 10 |
| Improved | 16 | 3 | 0 | 1 | 95a |
DAPI staining
For laser confocal microscopy, many intact cells
were present and observed in the normal spinal cord (Fig. 3A). For the grade I scaffolds of the
traditional and improved groups (Fig.
3B and C), the internal layers exhibited few whole and broken
residual cells. Notably, for the grade I stents in the traditional
and improved groups, DAPI estimates were in accordance with those
from H&E staining. The EDC crosslinking method appeared to
efficiently decellularize stents.
DNA residue
After normal spinal cord tissue was treated by
different acellular methods, the DNA residue in the improved group
was less than that in the traditional group (Fig. 4); the decellularization method was
more efficient in the improved group than in the traditional
group.
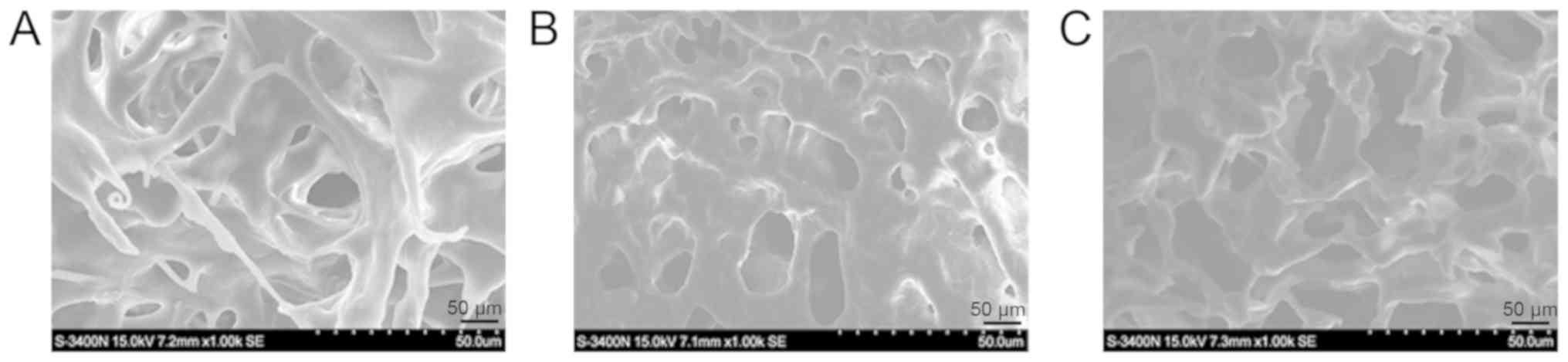
Electron microscopy
A tight 3D network and a complete extracellular
matrix was observed in normal spinal cord tissue (Fig. 5A). With regards to 3D structure,
the improved group (Fig. 5B)
exhibited a markedly tighter network than the traditional group
(Fig. 5C). Furthermore, the gross
appearance of the improved group was slightly more complete than
that of the traditional group.
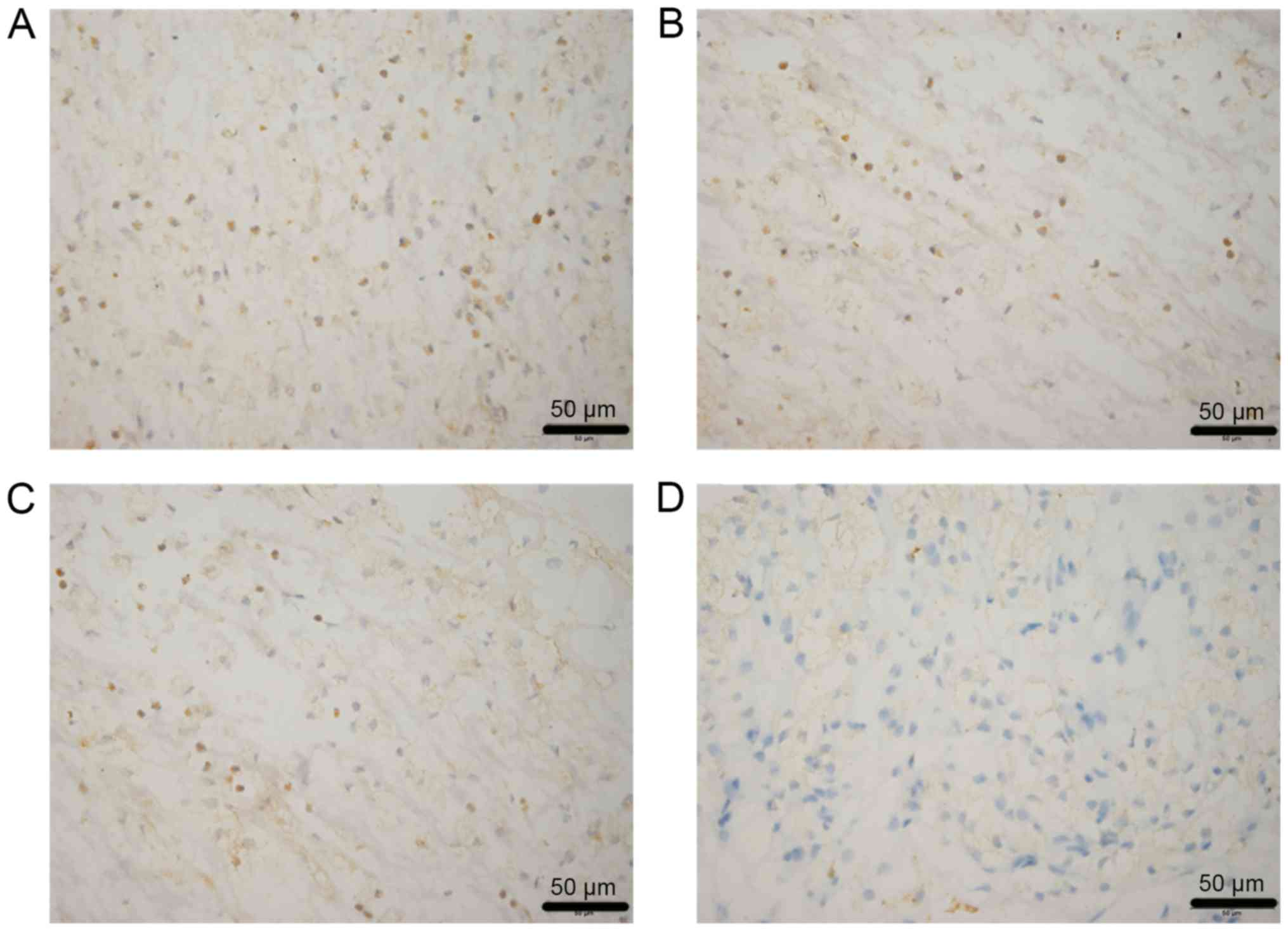
Immunogenicity analysis
Lymphocytes, neutrophils and fibroblasts were
detected in the two groups in vivo. After 2 weeks of
implantation, cell infiltration in the improved group (Fig. 6A) was markedly weaker than in the
traditional group (Fig. 6B). After
4 weeks, cell infiltration in the improved (Fig. 6C) and traditional groups (Fig. 6D) was gradually decreased; however,
the reduction in the improved group was more obvious.
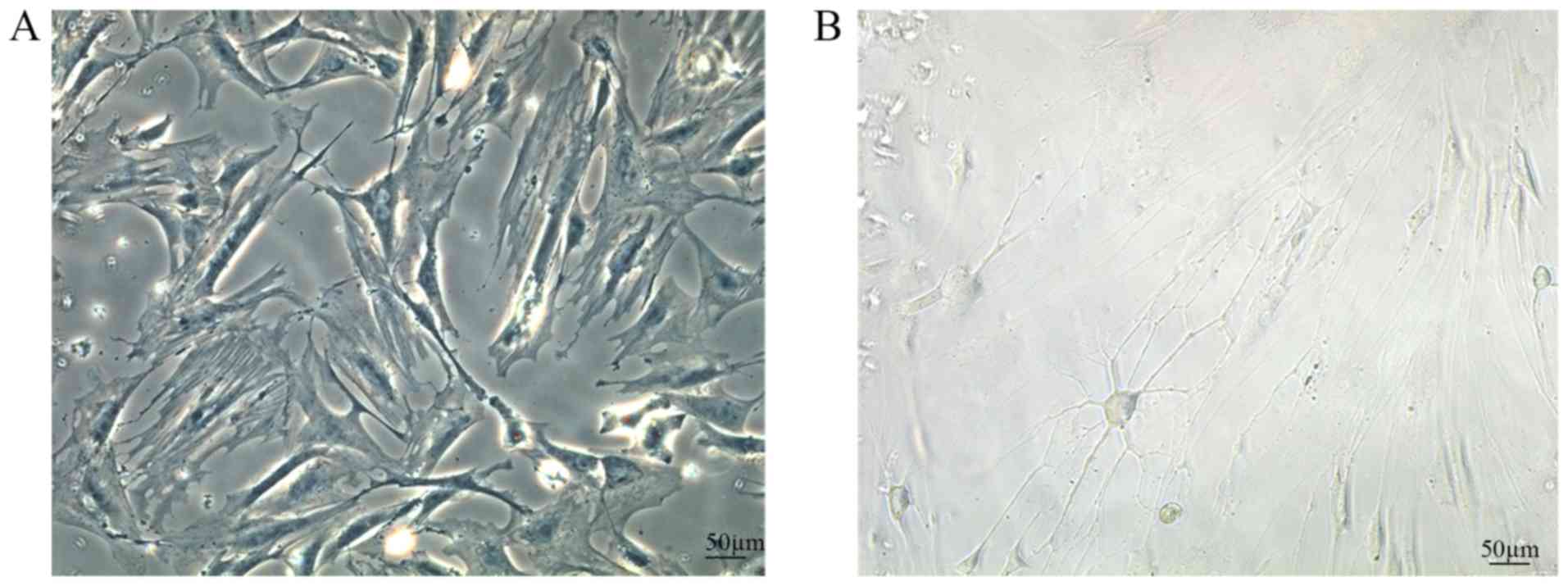
BMSC differentiation
After 7 days of culture, normal BMSCs (Fig. 7A) were adherent and had grown
closely with a regular pattern, and a long fusiform or triangular
shape. Following the addition of neurotrophic factors, BMSCs
differentiated into neuron-like cells. Notably, the nuclei had lost
their original fusiform shape, and the cells formed axon-like
structures and became interconnected (Fig. 7B).
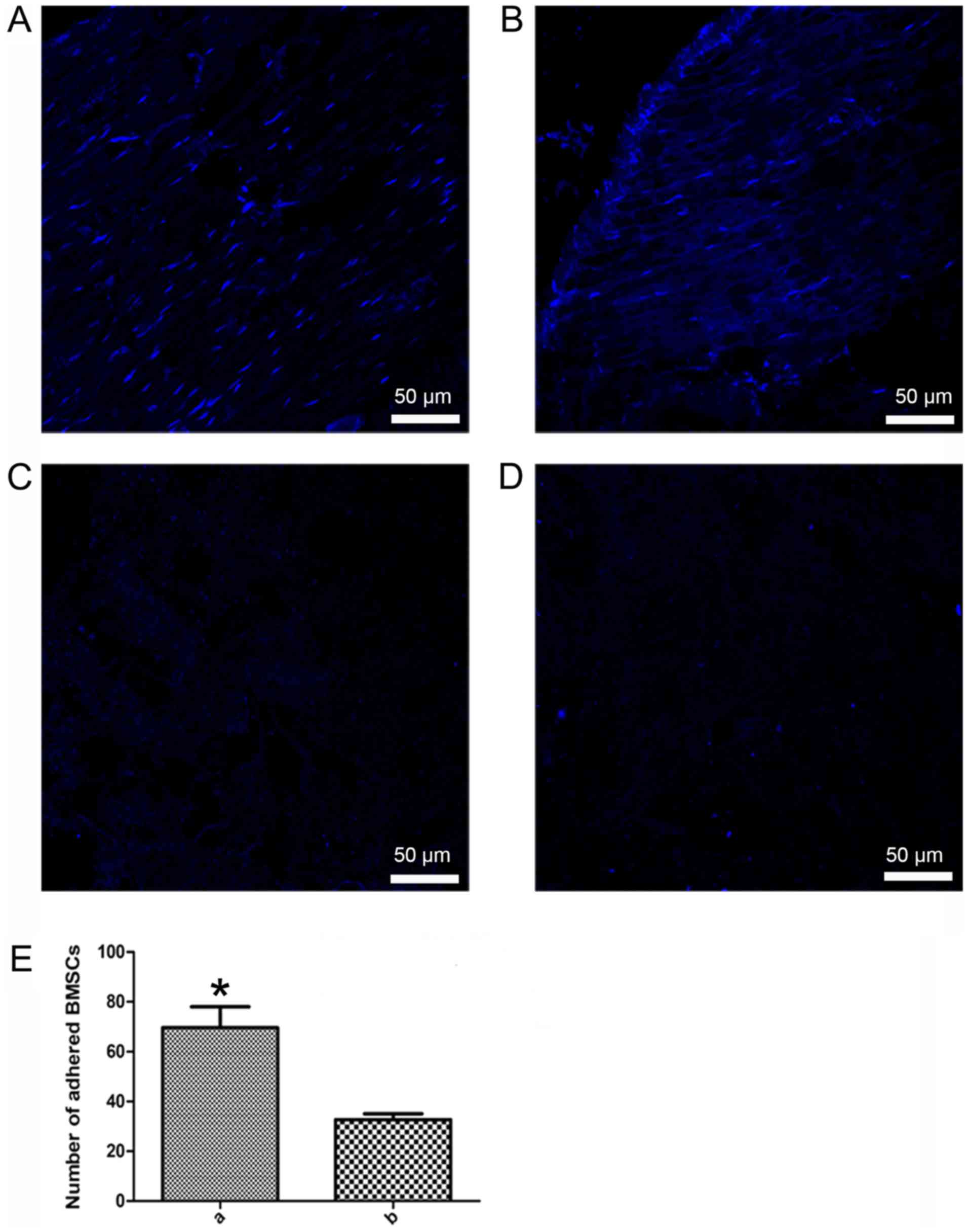
BMSC adhesion
After 4 h of culture, DAPI staining revealed that
the two groups exhibited nuclear fluorescence on the adhesive
scaffolds (Fig. 8A and B).
Furthermore, the number of adherent cells in the improved group
scaffolds (Fig. 8A) was greater
than in the traditional group scaffolds (Fig. 8B). The control group, with no BMSCs
added to the stents, exhibited no spotty nuclear fluorescence
(Fig. 8C and D). Cell adhesion to
scaffolds was significantly increased in the improved group
compared with in the traditional group (P<0.05, Fig. 8E).
BMSC differentiation
After 7 days of culture, MSCs could grow on the
surface of the traditional and improved scaffolds. After additional
supplementation with growth factors, MSCs were differentiated into
neuron-like cells on the scaffolds (Fig. 9A and B). The improved scaffolds
(Fig. 9A) were more favorable for
BMSC growth and differentiation than the traditional scaffolds
(Fig. 9B), as verified using an
NF-200 antibody. Additionally, NF-200-positive expression was
increased in the improved group compared with in the traditional
group (Fig. 9C).
Gene expression in differentiated
BMSCs
RT-qPCR was used to determine neuronal gene
expression in differentiated MSCs in the traditional and improved
groups. MSCs were seeded into scaffolds and cultured in neural
induction medium for 7 days. Subsequently, a key neuronal cell
marker was detected, Nefh. Nefh expression was increased in the
improved group compared with in the traditional group (Fig. 10).
Discussion
In spinal tissue engineering studies there are three
basic elements, including seed cells, scaffolds and tissue factors
(18). Tissue engineering
scaffolds include a wide variety of materials, and acellular matrix
scaffolds have demonstrated great potential in animal studies
(1,19). A recent preliminary study attempted
to ascertain the potential of acellular matrix scaffolds in central
nervous system repair (9). Guo
et al (10) successfully
prepared an acellular spinal cord scaffold using a chemical
extraction method, and confirmed the excellent characteristics of
the scaffold. In addition, Jiang et al (11) used genipin to crosslink the
scaffold to improve its mechanical properties and increase cell
adhesion to the scaffold. Previous studies have suggested that
acellular spinal cord scaffolds combined with BMSCs can promote
axonal regeneration and functional recovery in a spinal cord injury
model (20,21). In the present study, EDC
crosslinking combined with chemical extraction was used to prepare
acellular spinal cord scaffolds in the improved group; this led to
improved immunogenicity, as indicated by reduced infiltration, and
higher efficiency. Furthermore, the improved group exhibited
complete decellularization, as detected by H&E and DAPI
staining, and reduced DNA content. BMSCs have the potential to
proliferate and differentiate into osteogenic, chondrogenic,
adipogenic and neural cell lines (13,14,22).
In this study, MSCs were cultivated in acellular spinal cord
scaffolds and the following trophic factors were added to induce
adhesion and proliferation: 10 ng/ml NT-3, 10 ng/ml bFGF and 10
ng/ml EGF. Immunofluorescence and RT-qPCR verified that improved
group scaffolds promoted MSC adhesion, proliferation and
differentiation into neurons/neuron-like cells.
Chemical extraction and enzymatic methods are common
decellularization techniques (6,23,24).
However, the result of chemical extraction is often unstable, and
enzymatic approaches often excessively damage the tissue components
(25). The white matter of spinal
cord tissue contains few cells, whereas the central gray matter
contains more cells. With traditional decellularization methods,
the central gray matter cells can never be completely cleared;
however, with improved methods, namely EDC crosslinking and
chemical extraction, cells in both the white and grey matter can be
thoroughly removed. EDC/NHS is an effective protein crosslinking
agent (26). Previous studies have
reported that EDC crosslinking can increase the stability and
stiffness of scaffolds, to the point where they can resist
destruction by chemical extraction (16,27–30).
Preparation of the improved group scaffolds involved crosslinking
by EDC, which may increase the stability of scaffolds, allowing
them to pass through the next round of freeze-thawing and chemical
extraction intact.
BMSCs have the potential to differentiate into
multiple lineages. See et al (22) reported that MSCs cultured on
natural collagen scaffolds maintain the potential for multiple
differentiation. Previous studies demonstrated that BMSCs,
administered via the cerebrospinal fluid or intravenously, migrate
to the injured spinal cord, with the highest concentration at the
lesion center. Immunostaining of nestin indicated that BMSCs may
differentiate into neural cells, mature neurons or glial cells
(30,31). As BMSCs are useful for spinal cord
recovery after injury, they were selected as the seed cells in the
present study. NT-3 can specifically act on acute brain injury and
helps maintain neuron survival and promotes the repair of injured
nerves (32). NT-3, in combination
with bFGF and EGF, can promote MSC differentiation into neuron-like
cells (14). Therefore, these
three factors were selected to treat BMSCs seeded onto acellular
spinal cord scaffolds, in order to meet the requirements for spinal
cord tissue engineering.
EDC crosslinking was used to prepare the improved
scaffolds in this study. Haugh et al (33) reported that
collagen-glycosaminoglycan scaffolds crosslinked by EDC exhibit
improved cell attachment, proliferation and infiltration. Previous
studies have also made similar conclusions; that crosslinked
scaffolds are conducive to seed cell adhesion and proliferation
(34,35). These findings suggested that the
improved scaffolds may have potential in tissue engineering. Under
stimulation by NT-3, bFGF and EGF, BMSCs can differentiate into
neuron-like cells. This study used immunohistochemistry and RT-qPCR
to examine the expression levels of neuronal
differentiation-specific proteins and genes.
Immunohistochemistry was used to examine the
differentiation of MSCs into neuron-like cells. The neuron marker
NF-200 was used to detect differentiated neuron-like cells. As
determined using immunohistochemistry or RT-qPCR, the improved
group scaffolds out-performed the traditional group, promoting the
differentiation of MSCs into neuron-like cells. These findings may
be due to the improved group stents being crosslinked by EDC,
increasing toughness that may be associated with mechanical
properties. Banks et al (16) reported that EDC crosslinking
increases the mechanical properties of collagen scaffolds and
promotes the differentiation of adipose-derived MSCs into
osteoblasts without the need for additional growth factors.
Crosslinked scaffolds were also shown to facilitate seed cell
differentiation. Therefore, EDC crosslinking may increase the
mechanical properties of improved scaffolds; however, this study
did not measure the mechanical properties of the traditional and
improved scaffolds. PCR demonstrated a marked difference in the
expression levels of Nefh, indicating that, under stimulation by
NT-3, bFGF and EGF, and during the process of BMSC differentiation
into neuron-like cells, Nefh mRNA may be sensitive to alterations
in cell differentiation. It was suggested that Nefh mRNA may be
sensitive enough to measure BMSC differentiation into neuron-like
cells. The innovation of this study lies in the addition of NT-3,
bFGF and EGF to BMSCs, combined with improved decellularized spinal
cord scaffolds, and in demonstrating that the improved group was
conducive to the differentiation of BMSCs into neuron-like cells.
To the best of our knowledge, this study provided a novel approach
to the construction of scaffolds for spinal cord tissue
engineering.
The present study had some limitations. The first
limitation involved the addition of trophic factors to promote BMSC
differentiation: Neurotrophic factors often lose their protein
activity at ~37°C, so they need to be supplemented over time.
Another limitation was as follows: MSCs were differentiated into
neuron-like cells; however, although the general morphology of the
cells was consistent with neurons, and the differentiated
neuron-like cells were positive for NF-200 immunofluorescence, only
one neuronal protein marker was detected. In subsequent
experiments, numerous neuronal marker antibodies should be used to
verify MSC differentiation into neuronal cells.
To the best of our knowledge, this is the first
study to improve the preparation efficiency of acellular spinal
cord scaffolds. The results confirmed that EDC crosslinking
combined with chemical extraction methods may effectively improve
the efficiency of decellularization. After supplementing with
specific neurotrophic factors, BMSCs adhered to the acellular
spinal cord scaffolds, and were able to grow and differentiate into
neuron-like cells. Compared with the traditional group, the
improved group stents promoted the adhesion and differentiation of
BMSCs, and the improved group scaffold may have great potential for
spinal cord tissue engineering.
Acknowledgements
Not applicable.
Funding
The present study was supported by the National
Youth Science Foundation (grant no. 31000438) and the National
Natural Science Foundation of China (grant no. 81271362).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
TJ conceived and designed the experiments. HX, HY,
CS, YT and MY performed the experiments. HX, HY and XR analyzed the
data. XR and TJ contributed reagents and materials. HX, XR and TJ
wrote the paper and translated it into English.
Ethics approval and consent to
participate
The present study was conducted in accordance with
the Declaration of Helsinki and the National Institutes of Health
Guide for the Care and Use of Laboratory Animals. All experimental
protocols were approved by the Review Committee for the Use of
Animal Subjects of the Army Medical University (animal production
license number: SCXK-PLA-20120011; animal handling license number:
SYXK-PLA-20120031).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Baiguera S, Jungebluth P, Burns A, Mavilia
C, Haag J, De Coppi P and Macchiarini P: Tissue engineered human
tracheas for in vivo implantation. Biomaterials. 31:8931–8938.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Chen RN, Ho HO, Tsai YT and Sheu MT:
Process development of an acellular dermal matrix (ADM) for
biomedical applications. Biomaterials. 25:2679–2686. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ji R, Zhang N, You N, Li Q, Liu W, Jiang
N, Liu J, Zhang H, Wang D, Tao K and Dou K: The differentiation of
MSCs into functional hepatocyte-like cells in a liver biomatrix
scaffold and their transplantation into liver-fibrotic mice.
Biomaterials. 35:8995–9008
|
|
4
|
Woods T and Gratzer PF: Effectiveness of
three extraction techniques in the development of a decellularized
bone-anterior cruciate ligament-bone graft. Biomaterials.
36:7339–7349. 2005. View Article : Google Scholar
|
|
5
|
Sánchez PL, Fernández-Santos ME, Costanza
S, Climent AM, Moscoso I, Gonzalez-Nicolas MA, Sanz-Ruiz R,
Rodríguez H, Kren SM, Garrido G, et al: Acellular human heart
matrix: A critical step toward whole heart grafts. Biomaterials.
61:279–289. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Laronda MM, Jakus AE, Whelan KA, Wertheim
JA, Shah RN and Woodruff TK: Initiation of puberty in mice
following decellularized ovary transplant. Biomaterials. 50:20–29.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ravindran S, Kotecha M, Huang C, Ye A,
Pothirajan P, Yin Z, Magin R and George A: Biological and MRI
characterization of biomimetic ECM scaffolds for cartilage tissue
regeneration. Biomaterials. 78:58–70. 2015. View Article : Google Scholar
|
|
8
|
Cai M, Huang T, Hou B and Guo Y: Role of
demyelination efficiency within acellular nerve scaffolds during
nerve regeneration across peripheral defects. Biomed Res Int.
2017:46063872017. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Crapo PM, Medberry CJ, Reing JE, Tottey S,
van der Merwe Y, Jones KE and Badylak SF: Biologic scaffolds
composed of central nervous system. Biomaterials. 33:3539–3547.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Guo SZ, Ren XJ, Wu B and Jiang T:
Preparation of the acellular scaffold of the spinal cord and the
study of biocompatibility. Spinal Cord. 48:576–581. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Jiang T, Ren XJ, Tang JL, Yin H, Wang KJ
and Zhou CL: Preparation and characterization of
genipin-crosslinked rat acellular spinal cord scaffolds. Mater Sci
Eng C Mater Biol Appl. 33:3514–3521. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wang L, Wang ZH, Shen CY, You ML, Xiao JF
and Chen GO: Differentiation of human bone marrow mesenchymal stem
cells grown in terpolyesters of 3-hydroxyalkanoates scaffolds into
nerve cells. Biomaterials. 31:1691–1698. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhang K, Liu Z, Li G, Lai BQ, Qin LN, Ding
Y, Ruan JW, Zhang SX and Zeng YS: Electro-acupuncture promotes the
survival and differentiation of transplanted bone marrow
mesenchymal stem cells pre-induced with neurotrophin-3 and retinoic
acid in gelatin sponge scaffold after rat spinal cord transection.
Stem Cell Rev. 10:612–625. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Guan M, Xu Y, Wang W and Lin S:
Differentiation into neurons of rat bone marrow-derived mesenchymal
stem cells. Eur Cytokine Netw. 25:58–63. 2014.PubMed/NCBI
|
|
15
|
Parekkadan B and Milwid JM: Mesenchymal
stem cells as therapeutics. Annu Rev Biomed Eng. 12:87–117. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Banks JM, Mozdzen LC, Harley BA and Bailey
RC: The combined effects of matrix stiffness and growth factor
immobilization on the bioactivity and differentiation capabilities
of adipose-derived stem cells. Biomaterials. 35:8951–8959. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Dado D and Levenberg S: Cell-scaffold
mechanical interplay within engineered tissue. Semin Cell Deve
Biol. 20:656–664. 2009. View Article : Google Scholar
|
|
19
|
Kehoe S, Zhang XF and Boyd D: FDA approved
guidance conduits and wraps for peripheral nerve injury: A review
of materials and efficacy. Injury. 45:553–572. 2012. View Article : Google Scholar
|
|
20
|
Liu J, Chen J, Liu B, Yang C, Xie D, Zheng
X, Xu S, Chen T, Wang L, Zhang Z, et al: Acellular spinal cord
scaffold seeded with mesenchymal stem cells promotes long-distance
axon regeneration and functional recovery in spinal cord injured
rats. J Neurol Sci. 325:127–136. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Chen J, Zhang Z, Liu J, Zhou R, Zheng X,
Chen T, Wang L, Huang M, Yang C, Li Z, et al: Acellular spinal cord
scaffold seeded with bone marrow stromal cells protects tissue and
promotes functional recovery in spinal cord-injured rats. J
Neurosci Res. 92:307–317. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
See EY, Toh SL and Goh JC: Multilineage
potential of bone-marrow-derived mesenchymal stem cell cell sheets:
Implications for tissue engineering. Tissue Eng Part A.
16:1421–1431. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ngangan AV and McDevitt TC:
Acellularization of embryoid bodies via physical disruption
methods. Biomaterials. 30:1143–1149. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Burk J, Erbe I, Berner D, Kacza J, Kasper
C, Pfeiffer B, Winter K and Brehm W: Freeze-thaw cycles enhance
decellularization of large tendons. Tissue Eng Part C Methods.
20:276–284. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Grauss RW, Hazekamp MG, Oppenhuizen F, van
Munsteren CJ, Gittenberger-de Groot AC and DeRuiter MC:
Histological evaluation of decellularised porcine aortic valves:
Matrix changes due to different decellularisation methods. Eur J
CardioThoracic Surg. 27:566–571. 2005. View Article : Google Scholar
|
|
26
|
Huang GP, Shanmugasundaram S, Masih P,
Pandya D, Amara S, Collins G and Arinzeh TL: An investigation of
common crosslinking agents on the stability of electrospun collagen
scaffolds. J Biomed Mater Res A. 103:762–771. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Kozowska J and Sionkowska A: Effects of
different crosslinking methods on the properties of
collagen-calcium phosphate composite materials. Int J Biol
Macromol. 74:397–403. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Priyadarshani P, Li Y, Yang S and Yao L:
Injectable hydrogel provides growth-permissive environment for
human nucleus pulposus cells. J Biomed Mater Res A. 104:419–426.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Wang Y, Wang X, Shi J, Zhu R, Zhang J,
Zhang Z, Ma D, Hou Y, Lin F, Yang J and Mizuno M: A biomimetic silk
fibroin/sodium alginate composite scaffold for soft tissue
engineering. Sci Rep. 6:394772016. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Satake K, Lou J and Lenke LG: Migration of
mesenchymal stem cells through cerebrospinal fluid into injured
spinal cord tissue. Spine (Phila Pa 1976). 29:1971–1979. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Khalatbary AR and Tiraihi T: Localization
of bone marrow stromal cells in injured spinal cord treated by
intravenous route depends on the hemorrhagic lesions in traumatized
spinal tissues. Neurol Res. 29:21–26. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Liu T, Xu J, Chan BP and Chew SY:
Sustained release of neurotrophin-3 and chondroitinase ABC from
electrospun collagen nanofiber scaffold for spinal cord injury
repair. J Biomed Mater Res A. 100:236–242. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Haugh MG, Murphy CM, McKiernan RC,
Altenbuchner C and O'Brien FJ: Crosslinking and mechanical
properties significantly influence cell attachment, proliferation,
and migration within collagen glycosaminoglycan scaffolds. Tissue
Eng Part A. 17:1201–1208. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Thitiset T, Damrongsakkul S, Bunaprasert
T, Leeanansaksiri W and Honsawek S: Development of
collagen/demineralized bone powder scaffolds and periosteum-derived
cells for bone tissue engineering application. Int J Mol Sci.
14:2056–2071. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Liu C, McKenna FM, Liang H, Johnstone A
and Abel EW: Enhanced cell colonization of collagen scaffold by
ultraviolet/ozone surface processing. Tissue Eng Part C Methods.
16:1305–1314. 2010. View Article : Google Scholar : PubMed/NCBI
|