Introduction
Diabetes mellitus (DM) has become a global public
health problem increasing each year and the management of diabetic
patients requires extensive resources and care (1). It is estimated that diabetes will
affect roughly 55% of old adults in the next two decades and is
thus considered a major human health problem (2). Patients with DM exhibit vascular
damage, as well as kidney and nerve injury (2,3). DM
has also been associated with chronic kidney disease (CKD), which
exacerbates into renal ischemia/reperfusion (I/R) injury (RI/RI)
(3–5). Physicians and scientists have made
efforts in identifying novel therapeutic targets to mitigate the
complications of DM.
Signaling pathways have evolved over years in many
species (6), for instance during
kidney development. Wnt signaling has been shown to function in
renal injury (7,8). Notch signaling activation is involved
in renal injury and glomerular disease (9). Blocking the Notch signaling pathway
has been proven to be effective in rescuing the damage incurred in
diabetic conditions (10). One
main discovery is that induction of Notch signaling triggers cell
death, which further harms tissue activity (11). However, the underlying mechanism of
Notch signaling in this diabetic model remains to be
elucidated.
To explore the mechanism of Notch signaling in renal
function in diabetic models, the present study used a streptozocin
(STZ)-induced RI/RI diabetic rat model.
N-[N-(3,5-difluorophenacetyl)-L-alanyl]-S-phenylglycine t-butyl
ester (DAPT), a γ-secretase inhibitor of Notch signaling, was
administered to animals to examine potential recovery in renal
injury. Cisplatin has been reported to induce Notch signaling
(12) and thus whether the
induction of Notch signaling can be inhibited by DAPT was tested.
Its function in renal function and tissue recovery was assessed in
a diabetic rat model to provide novel insights on DAPT for
potential use in translational clinical studies.
Materials and methods
Diabetic animal models
A total of 60 Sprague-Dawley male rats (weight:
250–260 g; age: 8 weeks) were obtained from The Shanghai Animal
Center. The rats were housed under climate-controlled conditions
with a 12-h light/dark cycle and provided with standard food and
water ad libitum for 10 days. The rats were randomly dived
into two groups; one the control group (n=10) and the remainder the
experimental group (n=50), used for the generation of diabetic rat
model. The experimental group fasted for 12 h and then a single
dose of STZ (dissolved in citrate buffer, pH 4.5, 60 mg/kg body
weight) (13) was injected into
the abdominal cavity of rats to generate an STZ-induced diabetic
rat model. The control group were injected with citrate buffer (pH
4.5). After 72 h, the tail blood was collected to test the levels
of serum glucose and those with serum glucose concentrations of
>16.7 mmol/l were deemed diabetic rats. After 1 week of
observation, the diabetic rats were used in subsequent experiments,
apart from 6 rats which died due to side effect of STZ injection
and four rats were not successful for the diabetic rat model. All
the experiments complied with the guidance by the animal use and
care of The First Affiliated Hospital of Zhengzhou University and
the agents were approved by the ethical committee of animal care
and use.
Experimental groups
A total of 40 STZ-induced diabetic rats were housed
for 16 weeks and randomly assigned into four groups: i)
Sham-operated group (sham group), where rats were only treated by
separating the bilateral renal arteries and veins and then treated
with 10% dimethyl sulfoxide (DMSO, 1 ml/kg bw, i.v.) (14–16);
ii) RI/RI group (vehicle group), where the rats were treated with
ischemia through clamping the bilateral renal arteries and veins
for 45 min followed by 24 h reperfusion with DMSO (1 ml/kg bw,
i.v.); iii) I/R+ DAPT group (DAPT group), where DAPT (dissolved in
DMSO, 15 mg/kg) was administered as a pretreatment for rats via a
single-dose injection into the abdominal cavity at 30 min prior to
the I/R procedure; and iv) I/R+ DAPT + cisplatin group (Cisplatin
group), where cisplatin (15 mg/kg) was intraperitoneally
administered to rats at 24 h prior the I/R procedure and DAPT was
administered to the animals in the same way as the DAPT group.
Animal experiments were performed in accordance with the Guide for
the Care and Use of Laboratory Animals of Zhengzhou University. The
protocol was approved by the Committee on the Ethics of Animal
Experiments of Zhengzhou University.
Tissue collections
Following reperfusion for 24 h, the animals were
euthanized using CO2 in a flow rate lower than 30%
chamber vol/min and then decapitated to collect blood samples from
the abdominal aorta. The collected tissues were centrifuged at
4,000 × g at 4°C for 20 min to isolate the sera. The entire kidneys
were removed and weighed and immediately placed on dry ice or kept
at −80°C until further analysis. The kidneys from each group were
homogenized in cold normal saline and centrifuged at 4,000 × g at
4°C for 20 min to obtain the supernatant, which was used for the
determination of various parameters.
Renal damage examination
Renal function was evaluated based on the analysis
of blood urea nitrogen (BUN) and serum creatinine (SCr). The
concentration of BUN and SCr were analyzed using an automatic
biochemistry analyzer (Hitachi 76000; Hitachi High-Technologies
Corporation) according to the manufacturer's protocols.
Analysis of anti-oxidation in renal
tissues
Superoxide dismutase (SOD) activity and
malondialdehyde (MDA) content in kidney tissues were used as two
anti-oxidative markers. SOD activity and MDA were respectively
examined at wavelengths of 550 nm and 532 nm according to the
xanthine oxidase and thiobarbituric acid method (Roche Diagnostics
GmbH). The level of lipid peroxides was expressed as U of SOD/mg
protein and nmol of MDA/mg protein.
ELISA
Tumor necrosis factor (TNF) α, interleukin (IL) 10
and hypoxia-inducible factor (HIF) 1a levels in kidney tissues were
assessed. TNF-α (cat. no. ab4607; Abcam) and IL-10 (cat. no.
ab108872; Abcam) levels were measured using ELISA kits according to
the manufacturer's protocols. For the HIF1a evaluation, the
quantitative sandwich ELISA method (cat. no. MAN0014317; Thermo
Fisher Scientific, Inc.) following the manufacturer's protocols was
performed to test the level of HIF1a in diabetic rat model.
Briefly, HIF1A standards and samples are captured by a polyclonal
HIF1A antibody on the pre-coated plate and detected using a
biotinylated monoclonal HIF1A antibody reactive to epitopes other
than the capture antibody. The biotinylated detection antibody is
then bound to streptavidin-HRP, which catalyzes the conversion of
TMB to a colored derivative. Color development is linear for the
assay's dynamic range and directly proportional to the amount of
HIF1A present in the sample, and the absorbance was measured on a
plate reader at 450–550 nm.
Western blotting
Protein levels were examined by western blotting.
Briefly, ~200 µg kidney proteins were extracted with T-PER Tissue
Protein Extraction Reagent (cat. no. 78510; Thermo Fisher
Scientific, Inc.) and separated 10% SDS-PAGE. The proteins were
transferred to nitrocellulose membranes. After blocking with 5%
bovine serum in TBS buffer containing 0.1% Tween 20 (TBST) for 1 h,
the membranes were incubated at 4°C overnight with the following
primary antibodies: IL-10 (1:500; cat. no. ab34843; Abcam), TNF-α
(1:500; cat. no. ab6671; Abcam) and HIF1A (1:1,000; cat. no.
ab243861; Abcam). Following three washes with TBST buffer, the
membrane was incubated with the AP-conjugated secondary anti-rabbit
antibody at 4°C overnight and then further developed using BCIP/NBT
(Roche Diagnostics GmbH) to visualize the bands. The protein
β-actin was used as a control to confirm equal loading of protein
in the gel lanes and to correct western blot signals. Images were
captured using a GelView system (Carolina Biological Supply
Company).
Reverse transcription-quantitative
(RT-q)PCR
Kidney tissues (40–60 mg) were frozen in liquid
nitrogen and 1 ml of TRIzol® was added (Invitrogen;
Thermo Fisher Scientific, Inc.). Total RNA isolation was performed
as previously described (17).
First-strand cDNA was performed using Superscript II RNase
H− Reverse Transcriptase (Invitrogen; Thermo Fisher
Scientific, Inc.). qPCR was performed using the SYBR Select Master
Mix (cat. no. 4472908; Thermo Fisher Scientific, Inc.). Different
primers were used to analyze the levels of target genes: Notch1,
mRNA forward primer: 5′-GATGGCCTCAATGGGTACAAG-3′ and reverse
primer: 5′-TCGTTGTTGTTGATGTCACAGT-3′; Notch2, forward primer:
5′-GAGAAAAACCGCTGTCAGAATGG-3′; reverse primer:
5′-GGTGGAGTATTGGCAGTCCTC-3′; Notch3, mRNA forward primer:
5′-AGTGCCGATCTGGTACAACTT-3′; reverse primer:
5′-CACTACGGGGTTCTCACACA-3′; Jagged-1, mRNA forward primer:
5′-AACTGGTACCGGTGCGAA-3′ and reverse primer:
5′-TGATGCAAGATCTCCCTGAAAC-3′ primers; HES-1, forward primer:
5′-CGACACCGGACAAACCAAA-3′, reverse primer:
5′-GAATGTCTGCCTTCTCCAGCTT-3′; and GAPDH, forward primer:
5′-GCAAGAGAGAGGCCCTCAG-3′, reverse primer:
5′-TGTGAGGGAGATGCTCAGTG-3′. The standard conditions for qPCR were:
50°C for 10 min and 95°C for 2 min; followed by 50 cycles of
denaturation at 95°C for 15 sec and 45 sec annealing/elongation at
58°C or 60°C. Relative genes expressions were calculated using the
2−∆∆Cq method and the housekeeping gene GAPDH was used
as an internal control.
Statistical analysis
Data are presented as the mean ± standard deviation,
and analyzed using SPPS 18.0 (SPSS, Inc.). Comparisons between
groups were performed using one-way ANOVA followed by Bonferroni's
post hoc test. Unpaired Student t-test was used to analyze the
significance between groups. P<0.05 was considered to indicate a
statistically significant difference.
Results
Renal function analysis of STZ-induced
diabetic rats
The levels of BUN and SCr were examined to evaluate
changes of renal function. BUN and SCr levels significantly
increased in the RI/RI (vehicle group) compared with the sham
group, which was roughly five-fold higher. However, BUN and SCr
levels in the DAPT and DAPT-cisplatin groups decreased, and those
of the DAPT-cisplatin group slightly increased compared with the
DAPT group, suggesting that cisplatin-induced Notch signaling was
blocked by DAPT (Table I).
 | Table I.Serum level of BUN and SCr in
streptozocin-induced diabetic rats. |
Table I.
Serum level of BUN and SCr in
streptozocin-induced diabetic rats.
| Groups | BUN, mmol/l | SCr, µmol/l |
|---|
| Sham | 6.88±0.43 | 27.86±2.53 |
| Vehicle |
36.50±3.19a |
118.96±5.15a |
| DAPT |
20.19±2.43a,b |
52.29±5.14a,b |
| DAPT + Cisplatin |
25.51±2.72a,c |
77.34±6.40a,c |
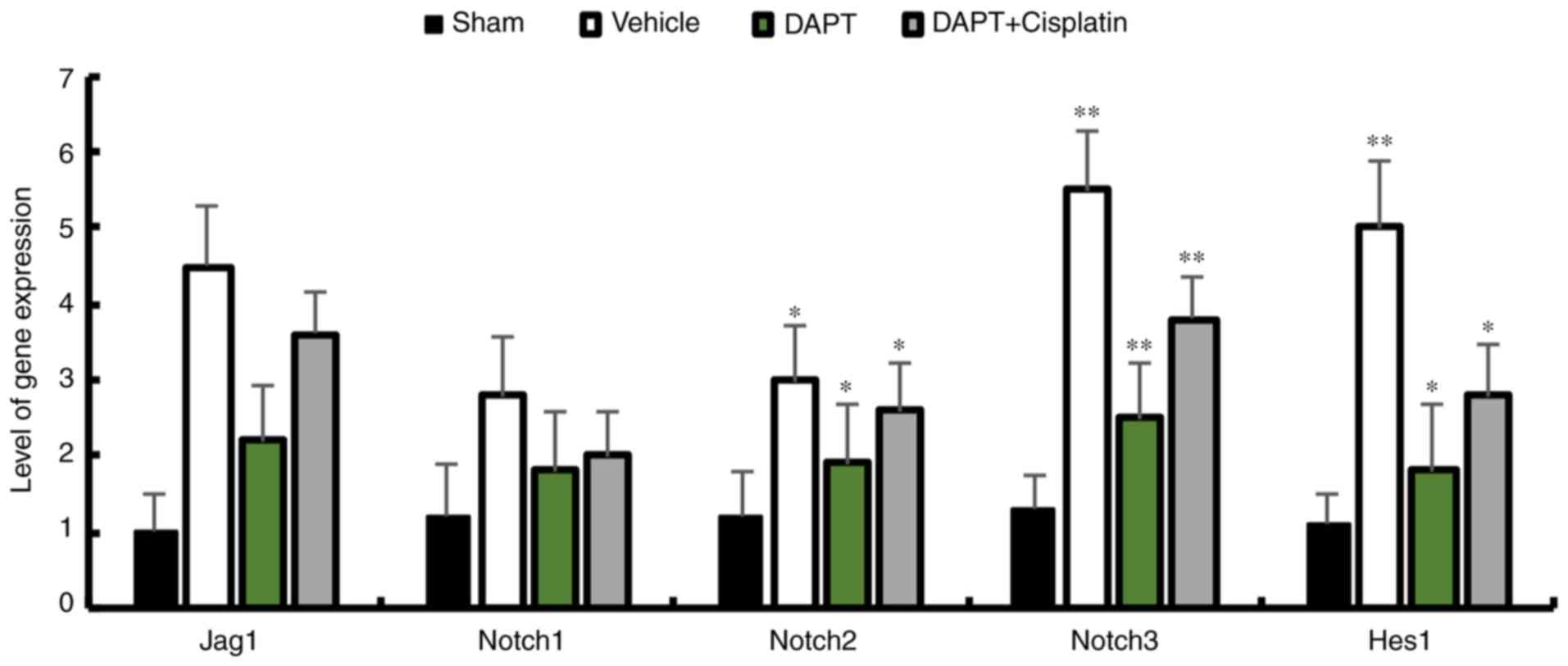
Activation of Notch signaling in a
diabetic rat model induced by cisplatin
To investigate whether DAPT is sufficient to inhibit
the expression of Notch signaling components in STZ-induced
diabetic rats, the expression patterns of Jagged1, Notch1, Notch2,
Notch3 and Hes1 were analyzed. The data demonstrated that DAPT can
significantly reduce the expression of Notch signaling components.
DAPT is the inhibitor that was used to block the Notch signaling
pathway and injecting DAPT induced the downregulation of Jagged1,
Notch 1–3 and Hes1 in the renal tissues of STZ-induced diabetic
rats, whereas the injection of cisplatin, which is an activator of
the Notch signaling pathway, followed by DAPT injection
demonstrated similar reductions in the expression of Notch
signaling components in diabetic rats (Fig. 1). This data indicates that the
upregulation of Notch signaling is reduced in renal tissue after
DAPT treatment.
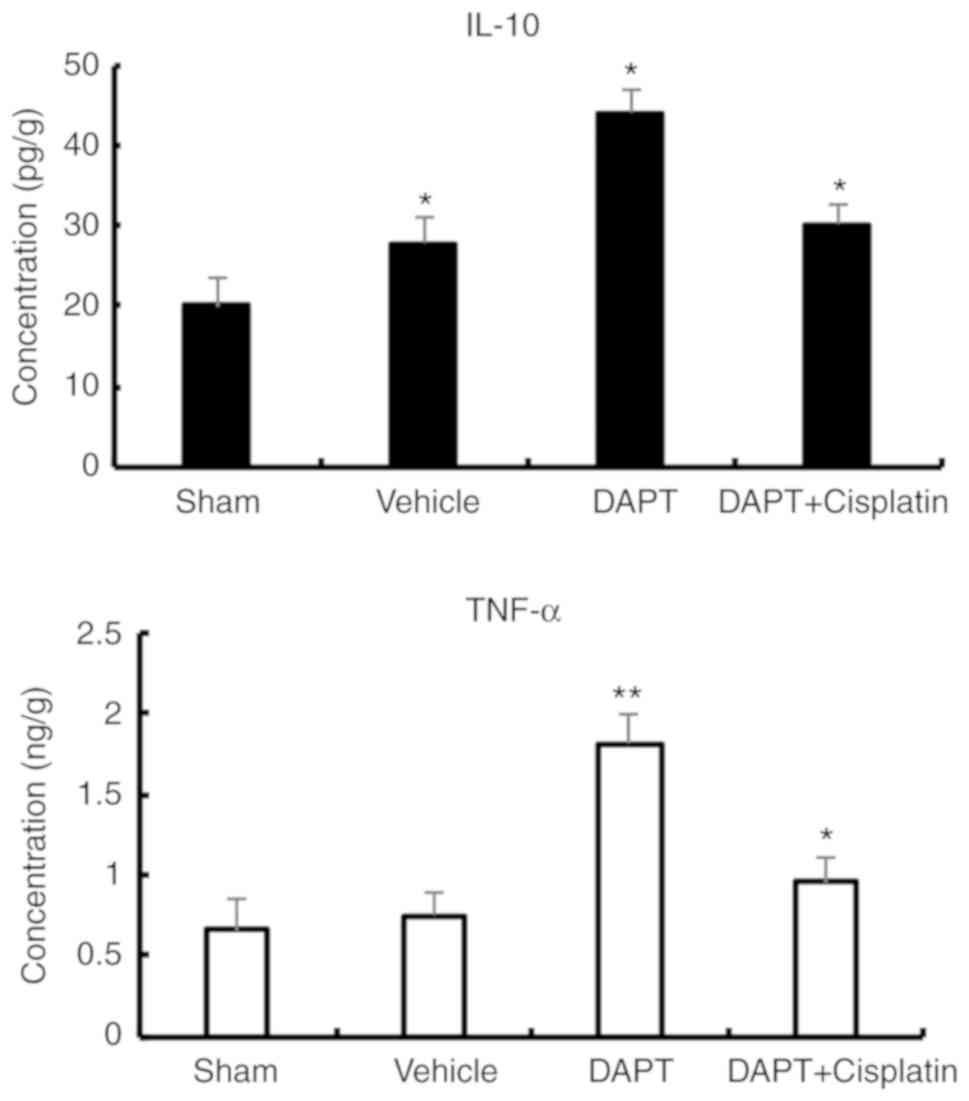
DAPT influences inflammatory factors
in SZT-induced diabetic rats
Inflammatory factors have been previously reported
to be associated with renal dysfunction in diabetic rats (18,19).
The expression of IL-10 (an anti-inflammatory factor) and TNF-α (a
pro-inflammatory factor) was examined in the present study. In the
vehicle group, the levels of IL-10 (20.01±9.26 pg/g vs. 27.87±3.17
pg/g, P<0.01) and TNF-α (0.66±0.11 ng/g vs. 0.45±0.07 ng/g,
P<0.01) were slightly significantly higher than the sham group
(Fig. 2). After treatment with
DAPT, IL-10 expression significantly increased by roughly two-fold
compared with the vehicle rats (44.15±9.53 pg/g vs. 20.01±9.26
pg/g) and the concentration of TNF-α significantly increased by
roughly three-fold (1.81±0.09 ng/g, P<0.01) compared with the
vehicle group. In the DAPT + cisplatin group, IL-10 (30.13±3.21
ng/g) and TNF-α (0.95±0.12 ng/g) decreased compared with the DAPT
group (Fig. 2), suggesting that
DAPT may function through the regulation of inflammatory factors to
reduce the damage in ischemia-reperfusion injury in diabetic
rats.
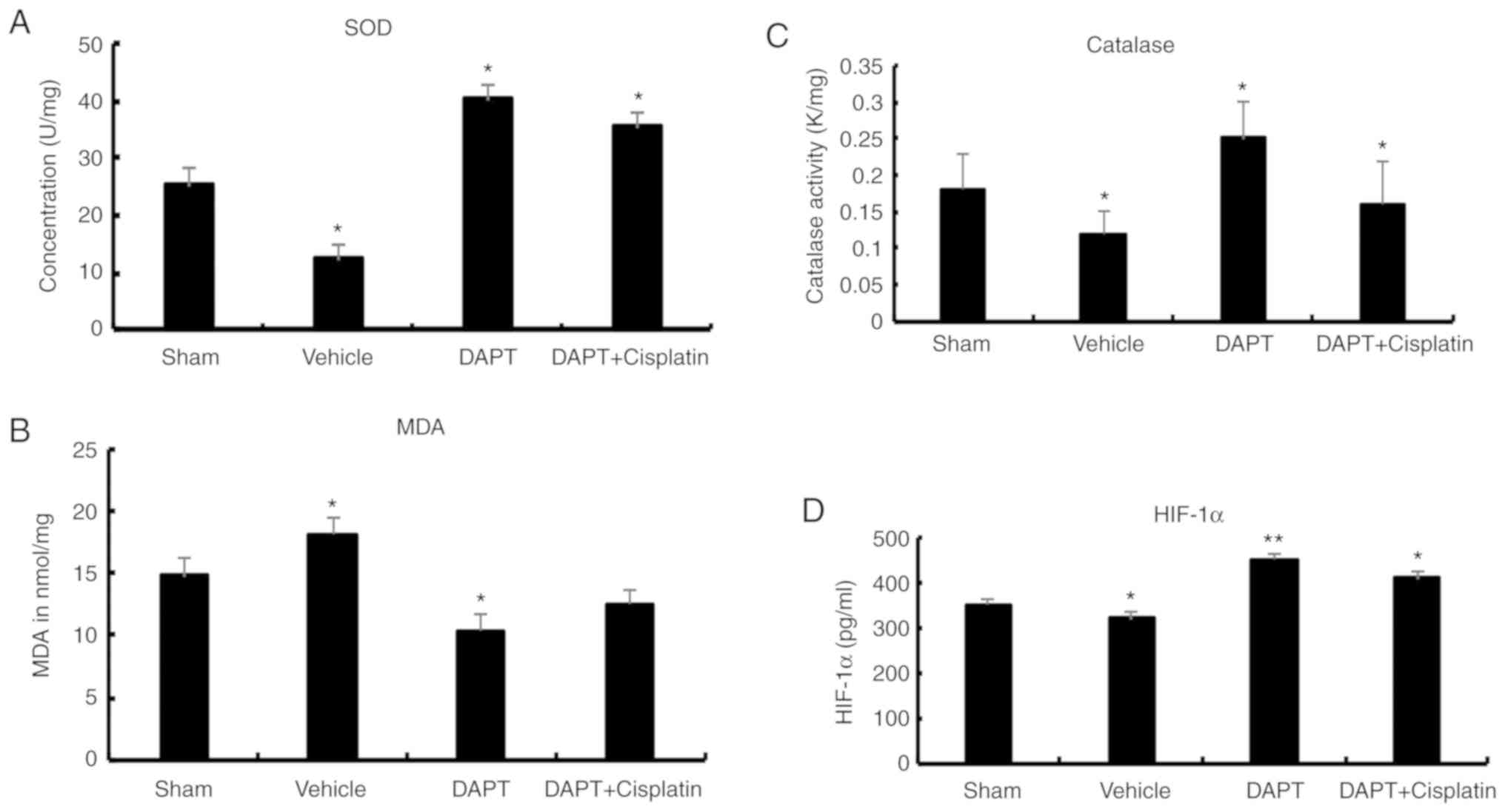
DAPT attenuates oxidation and HIF
levels in STZ-induced diabetic rats
To further explore the effects of DAPT on oxidation,
biomarkers for oxidative stress were analyzed. In the vehicle
group, SOD activity in the renal tissues significantly decreased
compared with the sham group (12.32±2.50 U/mg vs. 25.16±3.21 U/mg,
P<0.01). After DAPT treatment, the DAPT group exhibited a
significant increase in SOD activity (40.2±1.47 U/mg) in the renal
tissues compared with the vehicle group (P<0.01). In the DAPT +
Cisplatin group, SOD activity significantly decreased compared with
the DAPT group (35.2±2.45 U/mg) (P<0.05) but was still higher
than the vehicle group (Fig.
3).
Similarly, in the vehicle group, MDA levels
increased compared with the sham group (18.08±1.33 nmol/mg vs.
14.78±1.50 nmol/mg, P<0.05). In the DAPT group, MDA levels
significantly decreased (10.33±1.47 nmol/mg) in the renal tissues
compared with those of the vehicle group (P<0.01). In the DAPT +
Cisplatin group, MDA levels decreased compared with the DAPT group,
although this was not statistically significant (1.21±0.06 nmol/mg,
P>0.05; Fig. 3).
In the vehicle group, the level of catalase activity
decreased compared with the sham group (0.12±0.03 K/mg vs.
0.18±0.05 K/mg, P<0.05). In the DAPT group, catalase levels
(0.25±0.05 K/mg) significantly decreased in the renal tissues
(P<0.01). In the DAPT + Cisplatin group, the level of catalase
activity significantly decreased compared with the DAPT group
(0.16±0.06, P<0.05; Fig.
3).
HIF-1α expression decreased in the vehicle group
compared with the sham group (320±12.8 pg/ml vs. 350±12.5 pg/ml,
P<0.05). A significant increase in HIF-1α expression (450±15.3
pg/ml) was observed in the renal tissues after treatment with DAPT
(P<0.01). In the DAPT + Cisplatin group, HIF-1α expression
levels significantly decreased compared with the DAPT group
(410±14.8 pg/ml, P<0.05; Fig.
3).
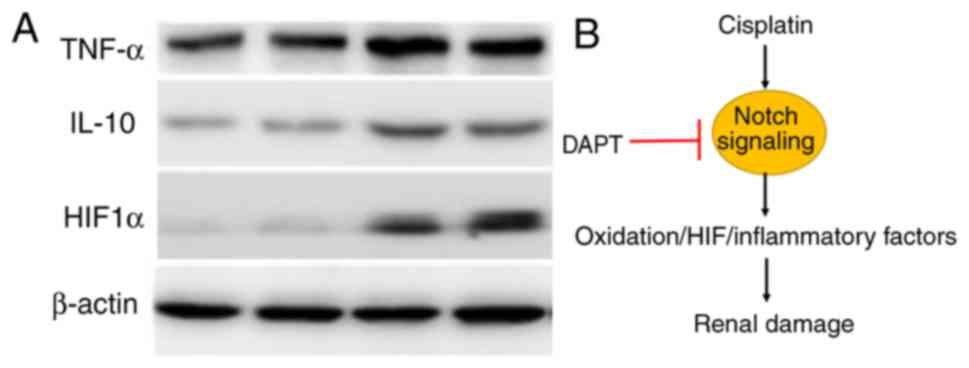
Western blotting confirms the function
of DAPT in diabetic rats
Western blotting using kidney tissue confirmed TNF-α
level in renal tissues in different groups, but the IL-10 levels
between DAPT and DAPT + Cisplatin group do not demonstrate a
significant difference. Based on the data, DAPT is sufficient to
induce the level in ischemia-reperfusion injury in diabetic rats
(Fig. 4A). HIF-1α was
significantly expressed in the DAPT groups (Fig. 4A). Overall, our data indicated that
DAPT is a suitable factor in reducing renal damage in
ischemia-reperfusion injury in STZ-induced diabetic rats via the
inhibition of Notch signaling (Fig.
4B).
Discussion
DM is a serious challenge to human health and often
leads to CKD, exacerbating RI/RI (20). Finding a suitable target to rescue
potential renal injury in diabetes animal models is thus
imperative. To date, several molecules have been investigated for
their effects in mitigating renal injury in different models. The
Wnt signaling pathway has been shown to be an ideal target for
rescuing renal function in diabetic rat models (21). The inhibitor GSK-3β has been tested
for its effects in ischemic diseases and TDZD-8 has been shown to
reduce I/R injury by inhibiting inflammation and cell apoptosis
(22–24). Notch signaling is an evolutionarily
conserved signaling system in cell-cell communications that can
regulate cell fate during development. Notch signaling serves a
critical role in nephron formation and segmentation and has been
reported to be involved in kidney disease. In mouse models, Notch
signaling in adult mice has been shown to be pathogenic, leading to
defective differentiation of podocytes, cell apoptosis and
ultimately renal failure. Blocking the Notch signaling pathway
using γ-secretase inhibitors has been shown to reduce the levels of
Notch signaling components in nephrons and podocytes (25). The present study provided further
evidence that blocking Notch signaling can rescue the renal defects
in STZ-induced diabetic rats, indicating that this may potentially
be utilized as a therapeutic approach. However, whether the
combination of signaling pathways such as Wnt and Notch can produce
more promising therapeutic effects, as well as how these signaling
pathways coordinate the regulation of renal function in diabetic
models, remains unclear.
Several previous studies have used DAPT to modulate
the Notch signaling pathway in diabetic models (11,25–27).
DAPT treatment has been shown to enhance neovascularization and
reperfusion in diabetic mice (28). DAPT has also been shown to be
effective in the treatment of diabetic neuropathic pain (29). Renal damage is alleviated after
DAPT injection (30). Further
evidence has indicated that the Jagged1/Notch signaling pathway
serves a critical role in TGF-β2-induced EMT in human RPE cells
(31). The Notch pathway may
precipitate diabetic nephropathy via TGF-β activation (32) and the Notch1/Hes1-Pten/Akt
signaling pathway is involved in a diabetic myocardium (33). Notch signaling has been shown to
serve a protective role in RI/RI-associated inflammation and
apoptosis (34). The present study
demonstrated that DAPT treatment can increase the levels of
inflammatory factors as well as anti-oxidative activities and
HIF-1a expression, which in turn reduce renal ischemia-reperfusion
injury in STZ-induced diabetic rats, thus providing novel insights
into the protective role of DAPT in renal function in diabetic
models. Although our data demonstrated promising application of
DAPT in the recovery of renal damage in I/R injury in STZ-induced
diabetic rats, we should be cautious of the potential side effect
of Notch inhibition as this intercellular signaling serves myriad
roles during development and physiology in vertebrates.
DAPT is a suitable therapeutic target to mitigate
mitigates RI/RI in STZ-induced diabetic rats. The role of DAPT in
renal function may in part work through the regulation on oxidative
stress, inflammatory activity and the HIF-1a.
Acknowledgements
Not applicable.
Funding
The present study was supported by research grants
to Professor Xiaokai Duan from The Medicine Technologies R&D
Program of Henan Province (grant no. 2018020733), The Medicine
Education Research Program of Henan Province (grant no.
Wjlx2018291) and support from The Health Commission of Henan
Province.
Availability of data and materials
All data generated or analyzed during the present
study are included in this published article.
Authors' contributions
XD and GQ designed the experiments, performed the
data analysis and wrote the manuscript.
Ethics approval and consent to
participate
All the experiments complied with the guidance by
the animal use and care of The First Affiliated Hospital of
Zhengzhou University and the agents were approved by the Ethical
Committee of Animal Care and Use. The protocol was approved by the
Committee on the Ethics of Animal Experiments of Zhengzhou
University.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Olokoba AB, Obateru OA and Olokoba LB:
Type 2 diabetes mellitus: A review of current trends. Oman Med J.
27:269–273. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Caspersen CJ, Thomas GD, Boseman LA,
Beckles GL and Albright AL: Aging, diabetes, and the public health
system in the United States. Am J Public Health. 102:1482–1497.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
O'Gara PT, Kushner FG, Ascheim DD, Casey
DE Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM,
Franklin BA, et al: 2013 ACCF/AHA guideline for the management of
ST-elevation myocardial infarction: A report of the American
college of cardiology foundation/American heart association task
force on practice guidelines. Circulation. 127:e362–e425.
2013.PubMed/NCBI
|
|
4
|
Tong F, Luo L and Liu DJ: Effect of
intervention in mast cell function before reperfusion on renal
ischemia-reperfusion injury in rats. Kidney Blood Press Res.
41:335–344. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Feng W, Tang R, Ye X, Xue C and Liao Y:
Identification of genes and pathways associated with kidney
ischemia-reperfusion injury by bioinformatics analyses. Kidney
Blood Press Res. 41:48–54. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wu T, Chen G, Tian F and Liu HX:
Contribution of cranial neural crest cells to mouse skull
development. Int J Dev Biol. 61:495–503. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Shen X, Hu B, Xu G, Chen F, Ma R, Zhang N,
Liu J, Ma X, Zhu J, Wu Y and Shen R: Activation of Nrf2/HO-1
pathway by glycogen synthase kinase-3β inhibition attenuates renal
ischemia/reperfusion injury in diabetic rats. Kidney Blood Press
Res. 42:369–378. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hu B, Wu Y, Liu J, Shen X, Tong F, Xu G
and Shen R: GSK-3beta inhibitor induces expression of Nrf2/TrxR2
signaling pathway to protect against renal ischemia/reperfusion
injury in diabetic rats. Kidney Blood Press Res. 41:937–946. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zhang J, Li B, Zheng Z, Kang T, Zeng M,
Liu Y and Xia B: Protective effects of Notch1 signaling activation
against high glucose-induced myocardial cell injury: Analysis of
its mechanisms of action. Int J Mol Med. 36:897–903. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Koshizaka M, Takemoto M, Sato S, Tokuyama
H, Fujimoto M, Okabe E, Ishibashi R, Ishikawa T, Tsurutani Y,
Onishi S, et al: An angiotensin II type 1 receptor blocker prevents
renal injury via inhibition of the Notch pathway in Ins2 Akita
diabetic mice. Exp Diabetes Res. 2012:1598742012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bonegio R and Susztak K: Notch signaling
in diabetic nephropathy. Exp Cell Res. 318:986–992. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Soni H, Matthews AT, Pallikkuth S,
Gangaraju R and Adebiyi A: γ-secretase inhibitor DAPT mitigates
cisplatin-induced acute kidney injury by suppressing Notch1
signaling. J Cell Mol Med. 23:260–270. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ramos-Lobo AM, Buonfiglio DC and
Cipolla-Neto J: Streptozotocin-induced diabetes disrupts the body
temperature daily rhythm in rats. Diabetol Metab Syndr. 7:392015.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Njomen GB, Kamgang R, Oyono JL and Njikam
N: Antioxidant potential of the methanol-methylene chloride extract
of Terminalia glaucescens leaves on mice liver in
streptozotocin-induced stress. Indian J Pharmacol. 40:266–270.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Mus LM, Denecker G, Speleman F and Roman
BI: Vehicle development, pharmacokinetics and toxicity of the
anti-invasive agent 4-fluoro-3′,4′,5′-trimethoxychalcone in
rodents. PLoS One. 13:e01925482018. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Pearsall EA, Cheng R, Matsuzaki S, Zhou K,
Ding L, Ahn B, Kinter M, Humphries KM, Quiambao AB, Farjo RA and Ma
JX: Neuroprotective effects of PPARα in retinopathy of type 1
diabetes. PLoS One. 14:e02083992019. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hu B, Wu T, Zhao Y, Xu G, Shen R and Chen
G: Physiological signatures of dual embryonic origins in mouse
skull vault. Cell Physiol Biochem. 43:2525–2534. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Furuya F, Ishii T and Kitamura K: Chronic
inflammation and progression of diabetic kidney disease. Contrib
Nephrol. 198:33–39. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Garcia-Garcia PM, Getino-Melián MA,
Dominguez-Pimentel V and Navarro-González JF: Inflammation in
diabetic kidney disease. World J Diabetes. 5:431–443. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kazancioğlu R: Risk factors for chronic
kidney disease: An update. Kidney Int Suppl (2011). 3:368–371.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Liu W, Liang X and Yang D: The effects of
Chinese medicine on activation of Wnt/β-catenin signal pathway
under high glucose condition. Evid Based Complement Alternat Med.
2015:2951352015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Cuzzocrea S, Mazzon E, Esposito E, Muià C,
Abdelrahman M, Di Paola R, Crisafulli C, Bramanti P and Thiemermann
C: Glycogen synthase kinase-3beta inhibition attenuates the
development of ischaemia/reperfusion injury of the gut. Intensive
Care Med. 33:880–893. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Collino M, Thiemermann C, Mastrocola R,
Gallicchio M, Benetti E, Miglio G, Castiglia S, Danni O, Murch O,
Dianzani C, et al: Treatment with the glycogen synthase
kinase-3beta inhibitor, TDZD-8, affects transient cerebral
ischemia/reperfusion injury in the rat hippocampus. Shock.
30:299–307. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Gui B, Hua F, Chen J, Xu Z, Sun H and Qian
Y: Protective effects of pretreatment with oleanolic acid in rats
in the acute phase of hepatic ischemia-reperfusion injury: Role of
the PI3K/Akt pathway. Mediators Inflamm. 2014:4518262014.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Niranjan T, Murea M and Susztak K: The
pathogenic role of Notch activation in podocytes. Nephron Exp
Nephrol. 111:e73–e79. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Lin CL, Wang FS, Hsu YC, Chen CN, Tseng
MJ, Saleem MA, Chang PJ and Wang JY: Modulation of notch-1
signaling alleviates vascular endothelial growth factor-mediated
diabetic nephropathy. Diabetes. 59:1915–1925. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Marquez-Exposito L, Cantero-Navarro E,
Lavoz C, Fierro-Fernández M, Poveda J, Rayego-Mateos S,
Rodrigues-Diez RR, Morgado-Pascual JL, Orejudo M, Mezzano S and
Ruiz-Ortega M: Could Notch signaling pathway be a potential
therapeutic option in renal diseases? Nefrologia. 38:466–475.
2018.(In English, Spanish). View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Cao L, Arany PR, Kim J, Rivera-Feliciano
J, Wang YS, He Z, Rask-Madsen C, King GL and Mooney DJ: Modulating
Notch signaling to enhance neovascularization and reperfusion in
diabetic mice. Biomaterials. 31:9048–9056. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Yang C, Gao J, Wu B, Yan N, Li H, Ren Y,
Kan Y, Liang J, Jiao Y and Yu Y: Minocycline attenuates the
development of diabetic neuropathy by inhibiting spinal cord Notch
signaling in rat. Biomed Pharmacother. 94:380–385. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
He Y, Zhang M, Wu Y, Jiang H, Fu H, Cai Y,
Xu Z, Liu C, Chen B and Yang T: Aberrant activation of Notch-1
signaling inhibits podocyte restoration after islet transplantation
in a rat model of diabetic nephropathy. Cell Death Dis. 9:9502018.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Chen X, Xiao W, Liu X, Zeng M, Luo L, Wu
M, Ye S and Liu Y: Blockade of Jagged/Notch pathway abrogates
transforming growth factor β2-induced epithelial-mesenchymal
transition in human retinal pigment epithelium cells. Curr Mol Med.
14:523–534. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Liu L, Gao C, Chen G, Li X, Li J, Wan Q
and Xu Y: Notch signaling molecules activate TGF-β in rat mesangial
cells under high glucose conditions. J Diabetes Res.
2013:9797022013. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Yu L, Li Z, Dong X, Xue X, Liu Y, Xu S,
Zhang J, Han J, Yang Y and Wang H: Polydatin protects diabetic
heart against ischemia-reperfusion injury via Notch1/Hes1-mediated
activation of Pten/Akt signaling. Oxid Med Cell Longev.
2018:27506952018. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Huang R, Zhou Q, Veeraragoo P, Yu H and
Xiao Z: Notch2/Hes-1 pathway plays an important role in renal
ischemia and reperfusion injury-associated inflammation and
apoptosis and the γ-secretase inhibitor DAPT has a nephroprotective
effect. Ren Fail. 33:207–216. 2011. View Article : Google Scholar : PubMed/NCBI
|