Introduction
Diffuse large B cell lymphoma (DLBCL) is the most
common type of adult lymphoma (1).
B cell lymphomas are heterogeneously categorized in terms of
clinical manifestations, histomorphology, immunophenotyping and
prognosis (1). Our group has
recorded 1,831 lymphoma cases between 2008 and 2018 (data not
published). Of the non-Hodgkin lymphoma, the most common type was
DLBCL (45.6%; 741/1,625), which is higher than that of the China
and other Western countries (30-35%) (2–4).
According to the cell-of-origin classification, DLBCL can be
divided into two main molecular subtypes, defined by gene
expression profiling: Germinal center B cell like (GCB), Activated
B cell like (ABC) (5,6). DLBCL often involves various nodal and
extranodal sites. There are a number of large B cell lymphoma
(LBCL) subtypes, including primary central nervous system (PCNSL),
primary testicular lymphoma (PTL) and primary mediastinal B cell
lymphoma (PMBL) (7–9).
A combined treatment regimen of rituximab,
cyclophosphamide, doxorubicin, vincristine and prednisone (R-CHOP)
can significantly improve the prognosis of most patients (10). However, due to individual
differences and tumor cell resistance, recurrence occurs in
one-third of patients, causing them to enter the advanced phase of
DLBCL after treatment (11).
Increased interest in DLBCL led to Ngo et al (12) to discover the role of myeloid
differentiation factor 88 (MYD88) L265P as a disease-relevant
driver gene. MYD88 is a soluble adaptor protein in the cytoplasm
for inflammatory signaling pathways downstream of members of the
Toll-like receptor (TLR) and interleukin (IL)-1 that mainly
mediates the cellular signal transduction of the TLR, IL-1 receptor
(R) and IL-18R, so MYD88 plays a key role in innate immunity
(13–15). Ngo et al (12) found that in DLBCL, L265P mutation
occurs at position 794 of the coding sequence of MYD88, resulting
in the missense mutation of leucine to proline at position 265 in
the coding region of MYD88 protein, which abnormally activates the
IL-1R-mediated NF-κB, MAPK and JAK-STAT3 signaling pathways, and
leads to tumorigenesis (16).
Subsequently, it was demonstrated that the MYD88
mutation can be used to identify a molecular subgroup of patients
with DLBCL that have poorer prognosis rates (17). MYD88 L265P mutation also occurs in
a subtype of PCNSL associated with poor prognosis (18,19).
Pham-Ledard et al (20)
found that the gene mutation rate was 59% in DLBCL, leg type
(DLBCL-LT), and the prognosis was poor. Furthermore, Kraan et
al (21) found the MYD88
mutation in 68% of PTL tumors analyzed. MYD88 L265P mutations have
also been observed in other hematological diseases, such as
lymphoplasmacytic lymphoma/Waldenström's macroglobulinemia, IgM
monoclonal gammopathy of undetermined significance, marginal zone
lymphoma and chronic lymphocytic leukemia (22–24).
Schmitz et al (25) found four DLBCL genotype subtypes,
namely, MCD (based on the co-occurrence of MYD88, L265P and CD79B
mutations), BN2 (based on BCL6 fusions and NOTCH2 mutations), N1
(based on NOTCH1 mutations) and EZB (based on EZH2 mutations and
BCL2 translocations), and poorer prognosis rates in patients with
MCD and N1 subtypes. Weber et al (26) proposed immunotherapy for MYD88
L265P mutant tumors. It has been hypothesized that DLBCL could be
treated with MYD88 L265P peptide as a novel tumor-specific antigen
to induce cytotoxic T cell reaction (26). Hence, developing therapeutic agents
for this mutation is becoming increasingly important.
The frequency of MYD88 mutations at the protein and
molecular level was assessed in tumor tissue samples from 100
patients diagnosed with DLBCL, following which a correlation
analysis was performed to analyze clinicopathological
characteristics. Therefore, this study provides a comprehensive
summary of the methods used to detect MYD88 at different levels of
expression, and explores the prognostic value of MYD88 and other
clinicopathological parameters in DLBCL.
Materials and methods
Study cohort
Tumor tissues were collected from 100 patients with
DLBCL at The First Affiliated Hospital of Xinjiang Medical
University (Urumqi, China) and considered as formaldehyde-fixed
paraffin-embedded (FFPE) archival specimens between August 2010 and
July 2018. According to the 2016 World Health Organization
diagnostic criteria of hematopoietic and lymphoid tissue tumors
(27), two senior pathologists
(Professor Xinxia Li and Professor Wei Zhang) reviewed the cases
and collected clinicopathological data in the Department of
Pathology of The First Affiliated Hospital of Xinjiang Medical
University. Patients were followed up for 79 months. The study
protocol was approved by the Ethics Review Board of The First
Affiliated Hospital of Xinjiang Medical University. Written
informed consent was obtained from participants. All of the
procedures were performed in accordance with the Declaration of
Helsinki and relevant policies in China (28).
Immunohistochemistry (IHC)
A total of 100 FFPE tissue samples from patients
with DLBCL were immersed in 4% paraformaldehyde for 4 h at room
temperature and assembled into a tissue microarray with a core
diameter of 2 mm, cut to a thickness of 3 µm, and heat treated with
EDTA antigen retrieval solution (pH=8.0; cat. no. ZLI-9079; Beijing
Zhongshan Golden Bridge Biological Technology Co., Ltd.) for 20
min. Samples were blocked with 3% peroxide-hydrogen for 10 min at
room temperature for endogenous peroxidase ablation and then
incubated with the mouse anti-MYD88 (1:700; cat. no. ab133739;
Abcam) and diluted in PBS (0.01 M PBS, pH=7.4), for 1 h at 37°C.
Secondary antibody (anti-mouse IgG; cat. no. PV-6000; Beijing
Zhongshan Golden Bridge Biological Technology Co., Ltd.) was then
added and incubated for 30 min at 37°C. Coloration with
3,3-diaminobenzidin was performed at room temperature in the dark
for 10 min. MYD88 was localized in the cytoplasm of lymphoma cells.
IHC analysis (Leica DM3000; light microscope; magnification, ×40)
was based on the immunohistochemical scoring system (29), which was classified into negative
and positive. Staining intensity was scored as follows: i) 0,
negative; ii) 1, weak; iii) 2, moderate; iv) 3, intense. The extent
of staining was scored as follows: i) 0, 0% of tumor area stained;
ii) 1, <10%; iii) 2, 10–50%; iv) 3, >50%. These two scores
were summed to give each sample a final score ranging from 0 to 6.
The final scores of 0 to 1 and 2 to 6 were considered as negative
and positive MYD88 expression, respectively.
Other related immunohistochemical markers were
examined using a Roche VENTANA Benchmark XT automated
immunohistochemical staining instrument (Roche Diagnostics). The
primary antibodies used against p53, CD10, CD30, myeloma-associated
antigen-1 (MUM-1), Bcl-2, c-Myc, CD20, Bcl-6 and proliferation
marker protein Ki-67 (Ki-67) are presented in Table SI. The specific details of the
experimental method for these other related immunohistochemical
markers are the same as aforementioned for the MYD88 antibody
incubation.
DNA isolation
FFPE tissues were cut into 10 µm-thick sections, and
the most lymphoma-cell-rich area was dissected using a scalpel.
Total genomic DNA was subsequently extracted with a QIAamp DNA FFPE
tissue kit (cat. no. 56404; Qiagen, Inc.), according to the
manufacturer's instructions, and was quantified
spectrophotometrically using an Invitrogen Qubit 2.0 Fluorometer
(Thermo Fisher Scientific, Inc.). The concentration and optical
density ratio of the DNA solution were calculated using a Quawell
Q5000 UV–Vis Spectrophotometer (Quawell Technology, Inc.). All
samples were immediately stored at −80°C for further analysis.
Droplet digital polymerase chain
reaction (DDPCR) for the detection of MYD88 L265P mutation
The Bio-Rad QX200 Droplet Digital PCR system
(Bio-Rad Laboratories, Inc.) was used to perform DDPCR. The primers
of MYD88 were synthesized by Shanghai Yuanqi Biomedical Technology
Co., Ltd., as follows: Forward, 5′-CTTGGCTTGCAGGTGCC-3′ and
reverse, 5′-CTTTCTTCATTGCCTTGTACTTGATG-3′ (amplified fragment size
of 63 base pairs). In each DDPCR reaction, two probes were used
(Invitrogen; Thermo Fisher Scientific, Inc.), a FAM-labeled probe
for the MYD88 L265P mutation (5′-FAM-AGAAGCGACCGATCC-MGB-BHQ-3′)and
a VIC-labeled probe for the MYD88 L265P wild-type allele
(5′-VIC-AGAAGCGACTGATCC-MGB-BHQ-3′). The reaction volume was 20 µl
(4 µl DDPCR reaction solution, 10 µl DDPCR mix 3, 6 µl template).
PCR was performed in a Veriti™ Thermal Cycler (Thermo Fisher
Scientific, Inc.) using the following conditions: 95°C for 10 min;
followed by 40 cycles of 94°C for 15 sec and 58°C for 60 sec; and a
final extension at 98°C for 10 min. After thermocycling, the
96-well plate was put in the plate holder and read in the QX200
Droplet Digital PCR system, and based on positive droplets and
according to the Poisson distribution, the absolute copy number of
the MYD88 L265P and wild-type MYD88 alleles was calculated using
QuantaSoft™ analysis software (version 1.7.4.0917; Bio-Rad
Laboratories, Inc.). The positive control was a plasmid and the
negative control was distilled water. The following method was used
to judge whether expression was positive or negative: i) Positive,
mutation frequency ≥1% and ≥3 droplets fall in the ‘Ch1+Ch2-’
region; ii) negative, <3 droplets fall in the ‘Ch1+’ region and
<5 droplets fall in the ‘Ch2+’ region [Ch1, mutation copy
number; Ch2, wild-type copy number; Ch1+Ch2, genomic DNA copy
number; and Ch1/(Ch1+Ch2), mutation frequency]. Green droplets
depict wild-type droplets (Ch1-/Ch2+) region, gray droplets depict
negative droplets without detectable DNA (Ch1-/Ch2-) region and
orange droplets depict double positive droplets (Ch1+/Ch2+)
region.
Routine blood tests
Routine blood tests were measured using overnight
fasting blood samples (1 ml) collected from an antecubital vein
between 7 am and 9 am, drawing the blood into a test tube
containing an anticoagulant (EDTA) to prevent clotting. The
measurement of blood components was automated using an automatic
blood cell analyzer (cat. no. BC5000; Shenzhen Mindray Bio-Medical
Electronics Co., Ltd.; http://www.mindray.com/au/index.html). Blood tests
were used to measure blood components, such as monocyte,
neutrophil, lymphocyte, platelet and hemoglobin.
Statistical analysis
Statistical analyses were performed using SPSS 17.0
software (SPSS, Inc.). Chi-square test was conducted to analyze the
correlation between clinicopathological parameters and indicators.
Progression-free survival (PFS) was calculated as the time since
the date of diagnosis. Overall survival (OS) was determined as the
date of diagnosis to the date of death by any cause. PFS and OS
were determined through univariate (Kaplan-Meier) and multivariate
analyses (Cox proportional hazard model) for survival analysis and
survival curve mapping. Data for crossing of survival curves were
analyzed using the statistical packages R (The R Foundation;
http://www.r-project.org; version 3.4.3) and
Empower R (www.empowerstats.com; X&Y solutions,
Inc.).P<0.05 was considered to indicate a statistically
significant difference.
Results
Clinicopathological
characteristics
A total of 100 patients with DLBCL were included in
the present study, this consisted of 41 female participants and 59
male participants with a median age of 59 years (25–88 years).
Among them, 37% (37/100) had DLBCL in the lymph nodes and 63.0%
(63/100) had DLBCL in extranodal sites. The central nervous system
(CNS) was the most common extranodal site in the patients of the
present study (24/63, 38.1%). Nine patients had a gastrointestinal
tract lesion (14.29%), eight had head and neck lesions (12.70%),
five had retroperitoneal lesions (7.94%), four had soft tissue
lesions (6.35%), four had joint lesions (6.35%), three had
testicular lesions (4.76%), and six patients had breast, kidney,
adrenal gland, uterus, spleen and skin cases (1.59%, 1/63)
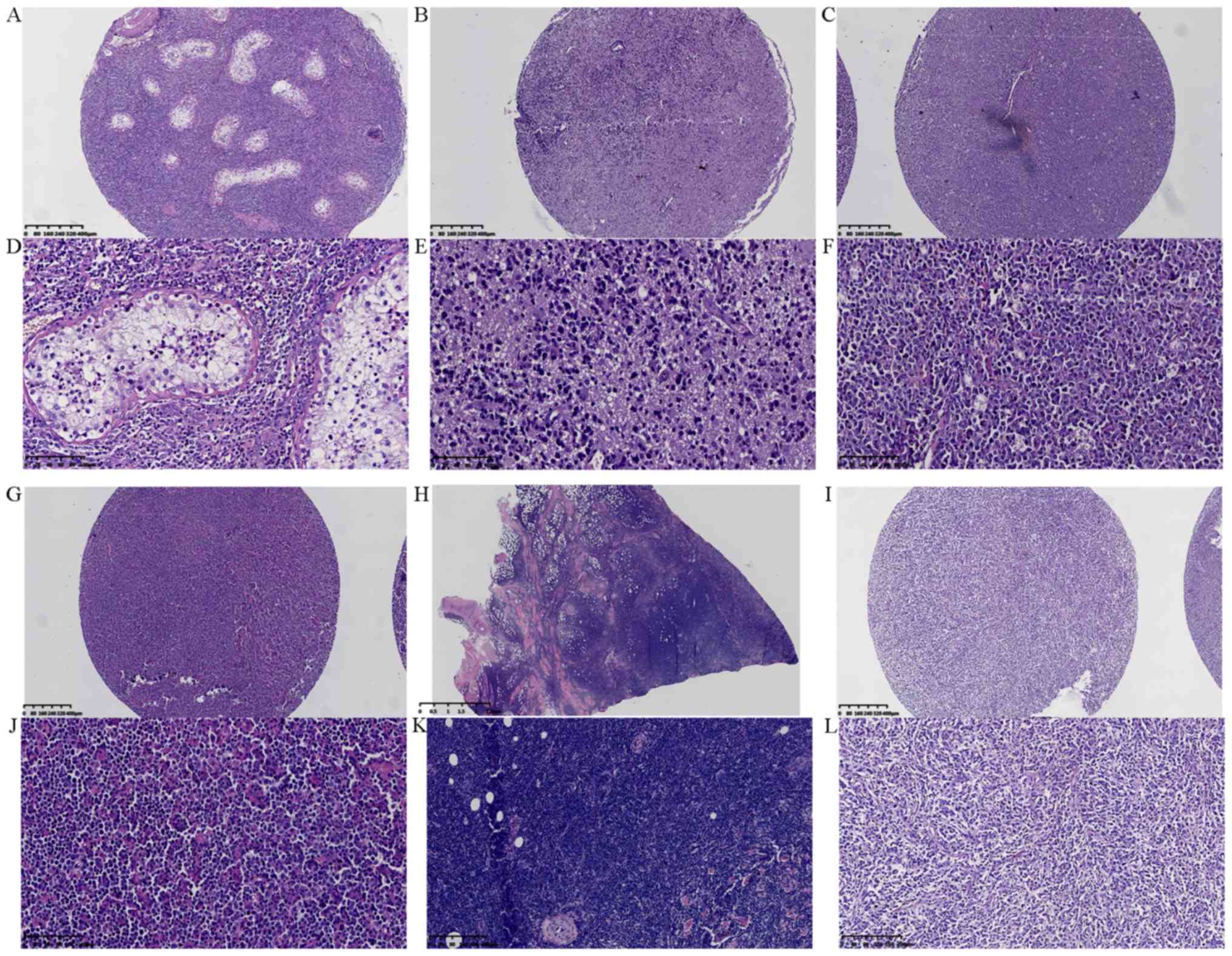
(Fig. 1A-L). Routine blood tests
were used to measure lymphocytes, monocytes, neutrophils,
hemoglobin and platelet counts. Lymphocyte/monocyte count ratio
(LMR) and neutrophil/lymphocyte count ratio (NLR) were set at 2.71
and 2.81, respectively, to assess the prognosis of patients
(30). The baseline clinical
characteristics of 100 patients with DLBCL in this study are shown
in Table SII.
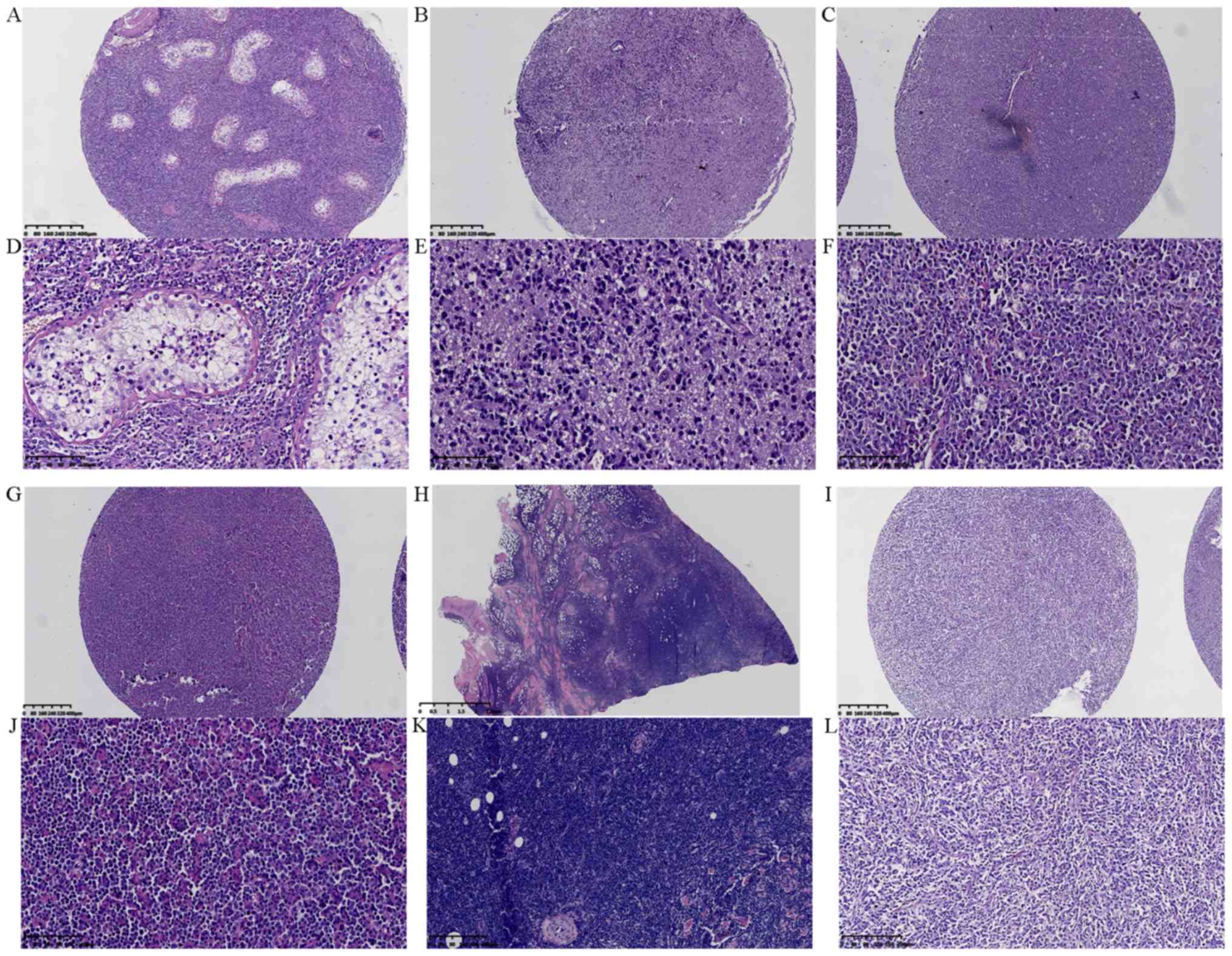 | Figure 1.Morphological observation of lesions
in various sites of diffuse large B cell lymphoma by hematoxylin
and eosin staining. (A) Testis at magnification, ×40. (B) Central
nervous system at magnification, ×40. (C) Lymph node at
magnification, ×40. (D) Testis at magnification, ×200. (E) Central
nervous system at magnification, ×200. (F) Lymph node at
magnification, ×200. (G) Tongue at magnification, ×40. (H) Skin at
magnification, ×40. (I) Gastrointestinal tract at magnification,
×40. (J) Tongue at magnification, ×200. (K) Skin at magnification,
×100. (L) Gastrointestinal tract at magnification, ×100. |
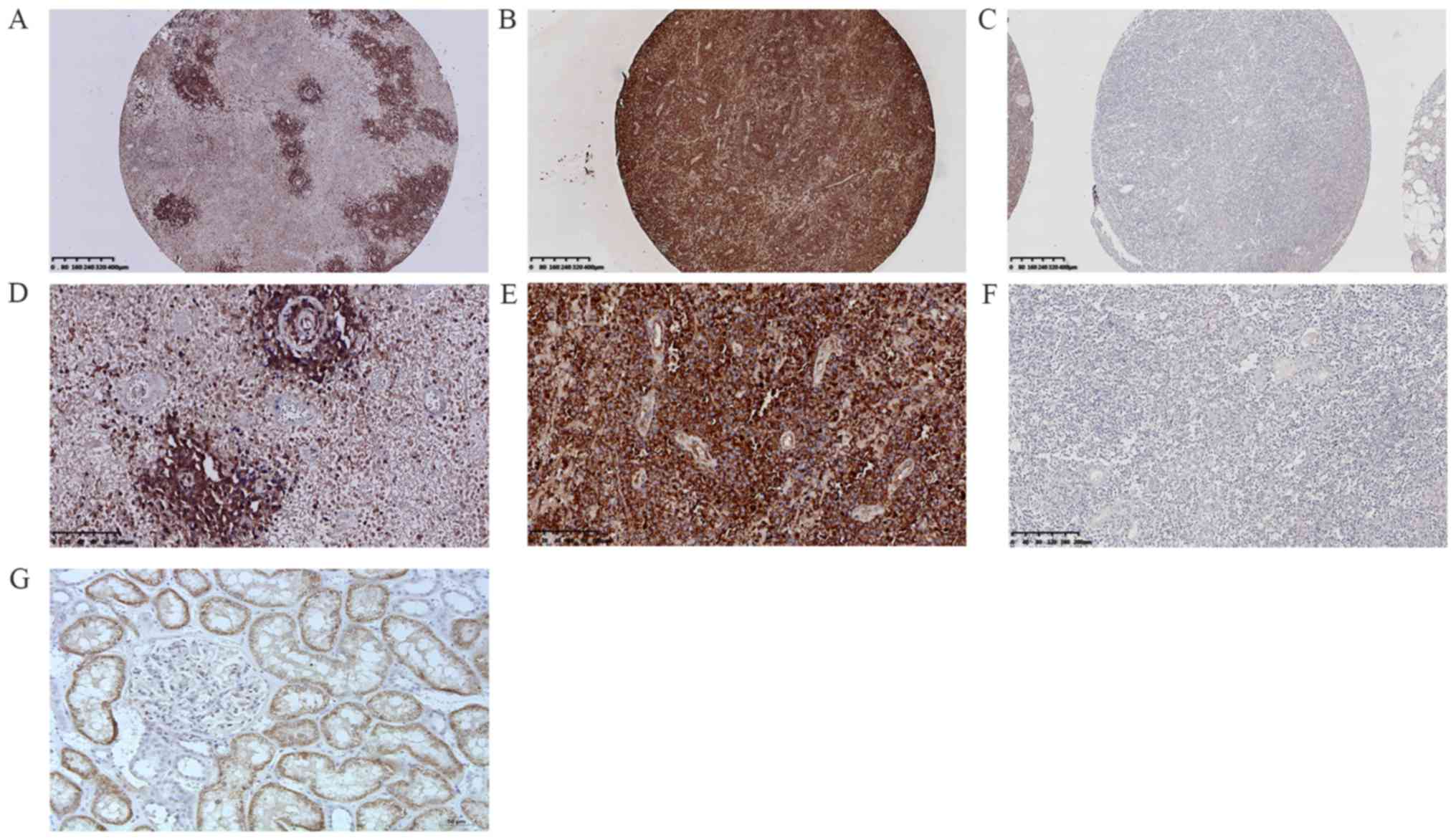
IHC of patients with DLBCL
The patients were divided into 64 cases of ABC
subtype DLBCL (ABC-DLBCL; 64%, 64/100) and 36 cases of GCB subtype
DLBCL (GCB-DLBCL; 36%, 36/100) using the Hans classification scheme
(ABC:GCB; 1.8:1). Protein expression and gene mutations were
investigated in 100 DLBCL cases. First, a frequent rate of protein
expression was observed in 38% of cases (38/100) (Fig. 2A-G). Second, positive MYD88
expression was found in 43.75% (28/64) and 27.78% (10/36) of
ABC-DLBCL and GCB-DLBCL cases, respectively. Positive MYD88
expression was observed in 32.43% (12/37) and 41.27% (26/63) of
lymph node DLBCL and extranodal DLBCL cases, respectively. For
positive MYD88 expression in extranodal sites of DLBCL, the
following data were observed: 22.23% (14/63) in the CNS, 6.35%
(4/63) in the head and neck, 3.17% (2/63) in the joints, 3.17%
(2/63) in the testes, 1.59% (1/63) in the gastrointestinal tract,
1.59% (1/63) in the retroperitoneal organs, 1.59% (1/63) in the
breast, and 1.59% (1/63) in the kidney. Positive MYD88 expression
was also found in 51.52% of Bcl-2 ≥70% cases (17/33), 39.62% of p53
expression cases (21/53), 35.71% of Bcl-6 expression cases (30/84),
32.14% of Ki-67 ≥60% expression cases (27/84), 35.29% of c-Myc ≥40%
cases (12/34), 33.33% of double expression (DE; c-Myc ≥40% and
Bcl-2 ≥70%) cases (4/12), and 22.22% of CD30 expression cases (2/9)
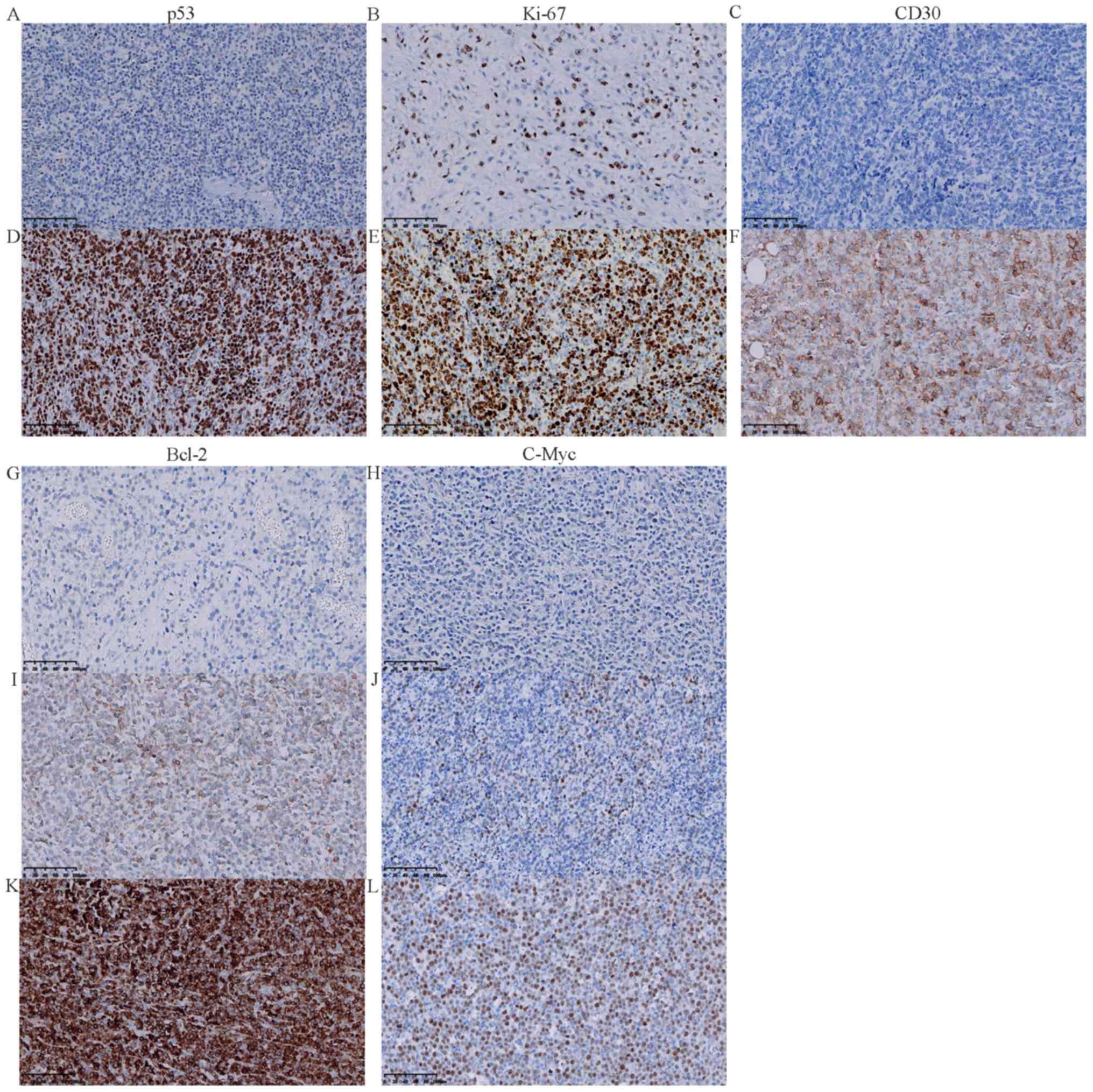
(Tables I and II; Fig.
3A-L).
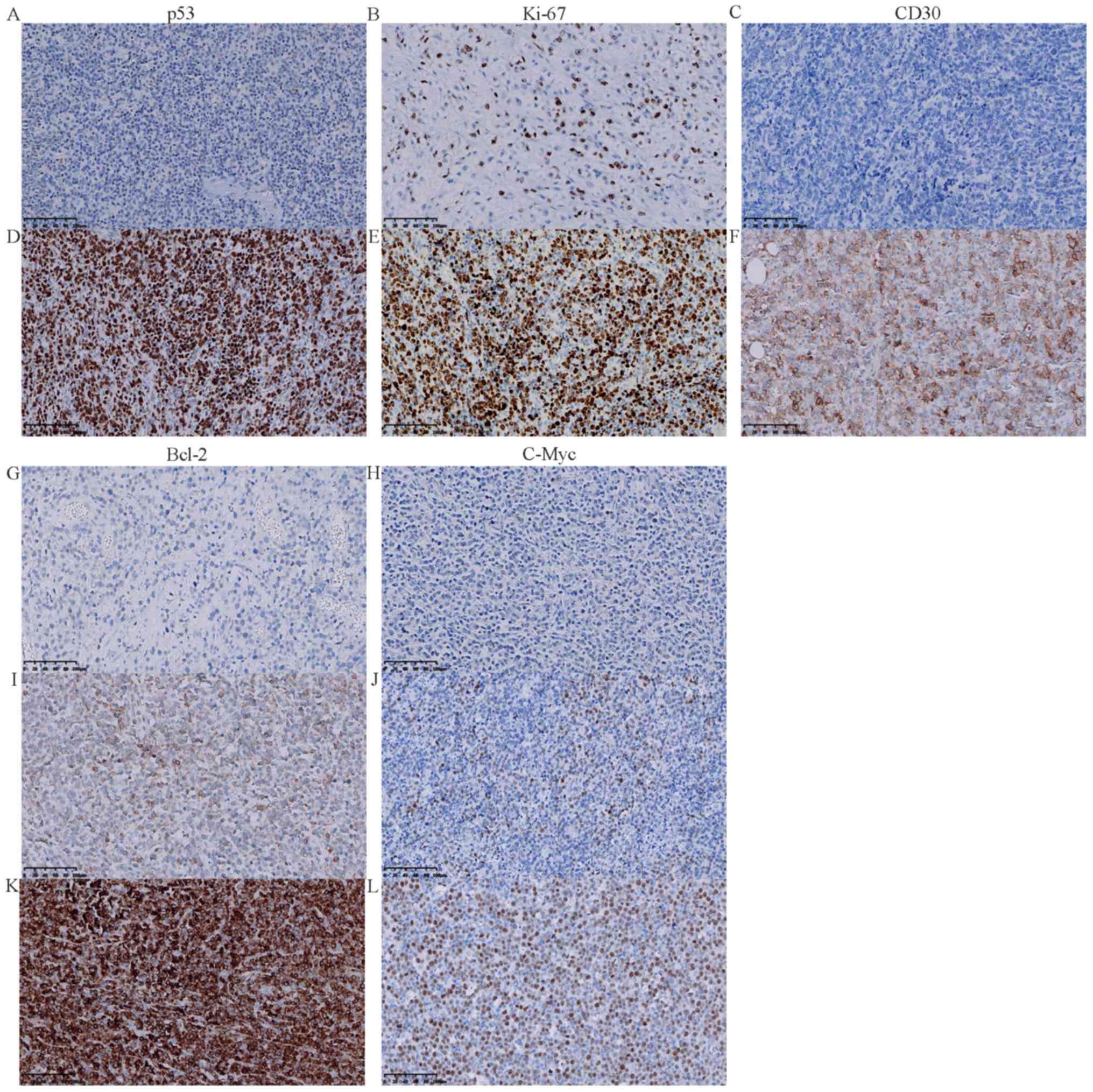 | Figure 3.Immunohistochemistry staining for
p53, Ki-67, CD30, c-Myc and Bcl-2 in diffuse large B cell lymphoma
specimens. (A) Negative expression of p53 (magnification, ×200).
(B) Low expression of Ki-67 (<80%) in the nucleus
(magnification, ×200). (C) Negative expression of CD30
(magnification, ×200). (D) Positive expression of p53 in the
nucleus (magnification, ×200). (E) High expression of Ki-67 (≥80%)
in the nucleus (magnification, ×200). (F) Positive expression of
CD30 in the cell membrane (magnification, ×200). (G) Negative
expression of Bcl-2 (magnification, ×200). (H) Negative expression
of c-Myc (magnification, ×200). (I) Low expression of Bcl-2
(<70%) in the cell membrane (magnification, ×200). (J) Low
expression of c-Myc (<40%) (magnification, ×200). (K) High
expression of Bcl-2 (≥70%) in the cell membrane (magnification,
×200). (L) High expression of c-Myc (≥40%) in the nucleus
(magnification, ×200). MYD88, myeloid differentiation factor 88;
Ki-67, proliferation marker protein Ki-67. |
 | Table I.Correlation of MYD88 mutation and
MYD88 expression with clinicopathological characteristics. |
Table I.
Correlation of MYD88 mutation and
MYD88 expression with clinicopathological characteristics.
|
| MYD88 mutation |
|
| MYD88
expression |
|
|
|---|
|
|
|
|
|
|
|
|
|---|
| Clinicopathological
characteristics | WT (n=71) | MUT (n=29) | χ2 | P-value | Negative
(n=62) | Positive
(n=38) | χ2 | P-value |
|---|
| Age (n=100) |
|
<60 | 40 | 17 | 0.044 | 0.834 | 36 | 21 | 0.075 | 0.784 |
|
≥60 | 31 | 12 |
|
| 26 | 17 |
|
|
| Sex (n=100) |
|
Male | 44 | 15 | 0.894 | 0.344 | 42 | 17 | 5.155 | 0.023a |
|
Female | 27 | 14 |
|
| 20 | 21 |
|
|
| Location
(n=100) |
|
Nodal | 31 | 6 | 4.661 | 0.031a | 25 | 12 | 0.773 | 0.379 |
|
Extranodal | 40 | 23 |
|
| 37 | 26 |
|
|
| Extranodal
involvement (n=63) |
|
CNS | 8 | 16 | 15.213 | 0a | 10 | 14 | 4.657 | 0.031a |
| Other
(centrum, testis, soft tissue, skin, spleen, breast) | 32 | 7 |
|
| 27 | 12 |
|
|
| Hans' algorithm
(n=100) |
|
GCB | 28 | 8 | 1.255 | 0.263 | 26 | 10 | 2.495 | 0.114 |
|
ABC | 43 | 21 |
|
| 36 | 28 |
|
|
| Ann-Arbor stage
(n=100) |
| Low
(I–II) | 23 | 1 | 9.458 | 0.002a | 14 | 10 | 2.495 | 0.671 |
| High
(III–IV) | 48 | 28 |
|
| 48 | 28 |
|
|
| β2-MB (n=55) |
|
Normal | 9 | 9 | 8.496 | 0.004a | 8 | 10 | 0.278 | 0.039a |
| Above
normal | 32 | 5 |
|
| 27 | 10 |
|
|
| B symptom
(n=100) |
|
Absent | 55 | 27 | 3.412 | 0.065 | 51 | 31 | 0.007 | 0.932 |
|
Present | 16 | 2 |
|
| 11 | 7 |
|
|
| ECOG performance
status score (n=100) |
|
<2 | 45 | 8 | 10.59 | 0.001a | 34 | 19 | 0.221 | 0.638 |
| ≥2 | 26 | 21 |
|
| 28 | 19 |
|
|
| LDH level
(n=99) |
|
Normal | 46 | 20 | 0.398 | 0.528 | 41 | 25 | 0.022 | 0.883 |
| Above
normal | 25 | 8 |
|
| 21 | 12 |
|
|
| NCCN-IPI
(n=100) |
| Low
risk (0–1) | 7 | 2 | 12.099 | 0.07 | 6 | 3 | 2.271 | 0.518 |
| Low
intermediate risk (2–3) | 47 | 10 |
|
| 36 | 21 |
|
|
| High
intermediate risk (4–5) | 15 | 13 |
|
| 18 | 10 |
|
|
| High
risk (≥6) | 2 | 4 |
|
| 2 | 4 |
|
|
| Survival status
(n=100) |
|
Died | 29 | 16 | 1.743 | 0.418 | 23 | 22 | 6.348 | 0.042a |
|
Alive | 38 | 12 |
|
| 37 | 13 |
|
|
| Status
unknown | 4 | 1 |
|
| 2 | 3 |
|
|
| Progression-free
survival (n=69) |
| 3 | 3 | 3 | 1.807 | 0.166 | 2 | 4 | 0.484 | 0.487 |
| 5 | 0 | 1 | 1.064 | 0.144 | 0 | 1 | 1.234 | 0.267 |
| Overall survival
(n=95) |
| 3 | 21 | 6 | 1.807 | 0.179 | 21 | 6 | 4.772 | 0.029a |
| 5 | 13 | 3 | 1.064 | 0.302 | 13 | 3 | 2.107 | 0.1 |
 | Table II.Correlation between MYD88 and other
IHC indicators. |
Table II.
Correlation between MYD88 and other
IHC indicators.
|
| MYD88 mutation | Chi-square
test | MYD88
expression | Chi-square
test |
|---|
|
|
|
|
|
|
|---|
| Gene | WT (n=71) | MUT (n=29) | χ2 | P-value | Negative
(n=62) | Positive
(n=38) | χ2 | P-value |
|---|
| CD10 (n=100) |
|
Positive | 18 | 6 |
|
| 17 | 7 |
|
|
|
Negative | 53 | 23 | 0.245 | 0.62 | 45 | 31 | 1.046 | 0.306 |
| Bcl-6 (n=100) |
|
Positive | 63 | 21 |
|
| 54 | 30 |
|
|
|
Negative | 8 | 7 | 2.946 | 0.086 | 8 | 7 | 0.652 | 0.419 |
| MUM-1 (n=99) |
|
Positive | 55 | 25 |
|
| 47 | 33 |
|
|
|
Negative | 16 | 3 | 1.809 | 0.179 | 15 | 4 | 2.676 | 0.102 |
| Bcl-2 (n=98) |
|
≥70% | 20 | 13 |
|
| 16 | 17 |
|
|
|
<70% | 20 | 6 | 2.855 | 0.24 | 22 | 4 | 8.373 | 0.015a |
| Myc (n=94) |
|
≥40% | 26 | 8 |
|
| 22 | 12 |
|
|
|
<40% | 15 | 8 | 1.051 | 0.591 | 10 | 13 | 4.512 | 0.105 |
| Myc (≥40%) and
Bcl-2 (≥70%) DE (n=94) |
|
Positive | 10 | 2 |
|
| 8 | 4 |
|
|
|
Negative | 61 | 27 | 1.007 | 0.316 | 54 | 34 | 0.126 | 0.723 |
| CD30 (n=100) |
|
Positive | 7 | 2 |
|
| 7 | 2 |
|
|
|
Negative | 64 | 27 | 0.221 | 0.639 | 55 | 36 | 1.045 | 0.307 |
| p53 (n=91) |
|
Positive | 39 | 14 |
|
| 32 | 21 |
|
|
|
Negative | 27 | 11 | 0.071 | 0.79 | 24 | 14 | 0.072 | 0.788 |
| Ki-67 (n=100) |
|
≥60% | 60 | 24 |
|
| 57 | 27 |
|
|
|
<60% | 11 | 5 | 0.047 | 0.829 | 5 | 11 | 7.645 | 0.006a |
| MYD88 expression
(n=100) |
|
Positive | 18 | 20 |
|
|
|
|
|
|
|
Negative | 53 | 9 | 18.101 | 0a |
|
|
|
|
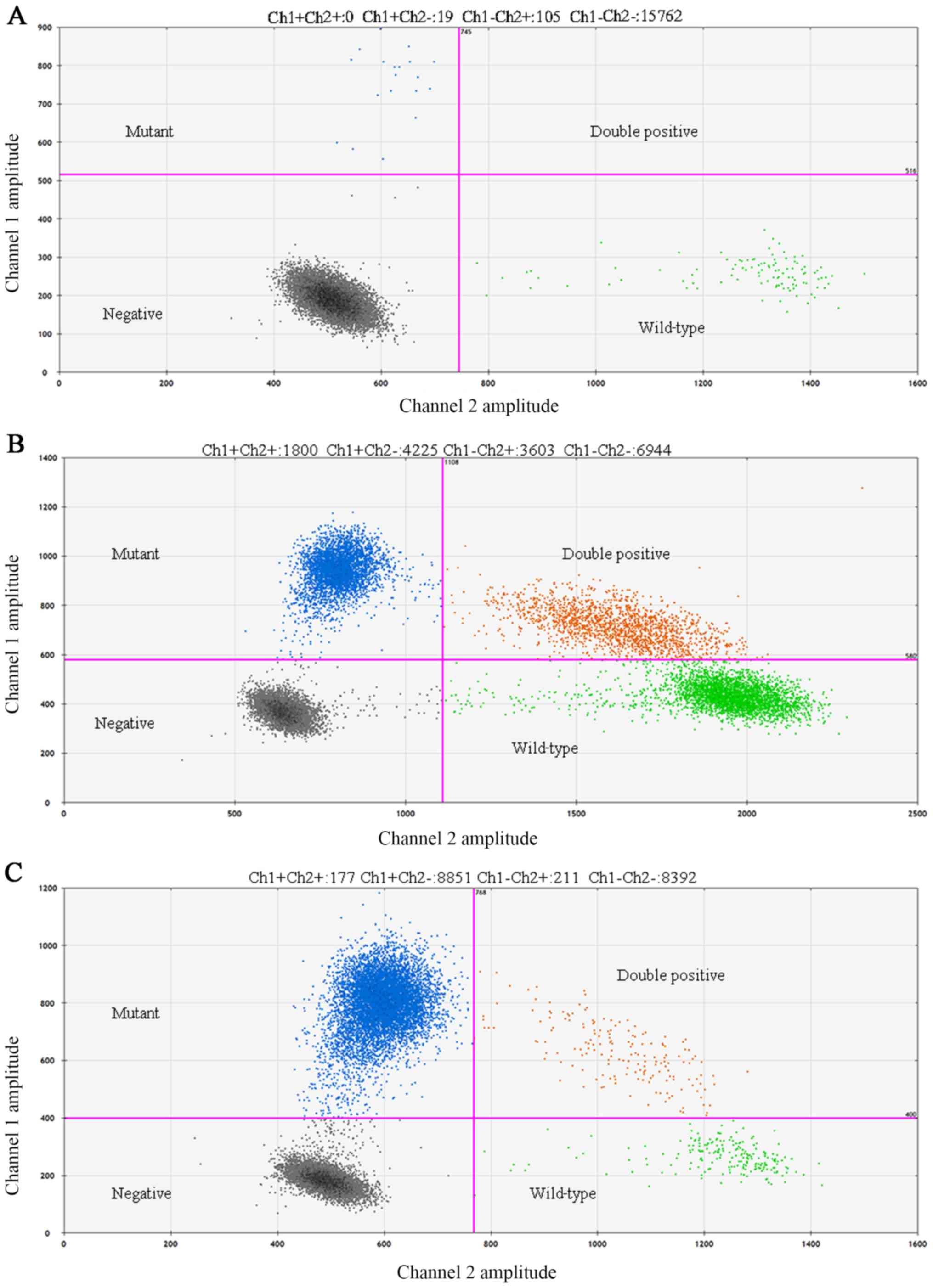
Detection of MYD88 L265P mutation in
DLBCL
DDPCR was performed on 100 DLBCL cases, and a
frequent rate of gene mutations was observed in 29% of cases
(29/100) (Fig. 4A-C). MYD88 L265P
was found in 32.81% (21/64) and 22.22% (8/36) of ABC-DLBCL and
GCB-DLBCL cases, respectively. MYD88 L265P mutation was also
observed in 16.22% (6/37) of nodal DLBCL and 36.5% (23/63) of
extranodal DLBCL. Furthermore, the mutation rate was 25.40% (16/63)
in the CNS, 3.17% (2/63) in the head and neck, and 4.76% (3/63) in
the joints. MYD88 L265P mutation was also observed in 39.39% of
Bcl-2 ≥70% cases (13/33), 26.42% of p53 expression cases (14/53),
25% of Bcl-6-expression cases (21/84), 28.57% of Ki-67 ≥60%
expression cases (24/84), 23.53% of c-Myc ≥40% cases (8/34), 16.66%
of DE cases (2/12) and 22.22% of CD30 expression cases (2/9),
66.67% of PT-DLBCL cases (2/3). The mutation rate of MYD88 in PCNSL
was 66.67% (16/24). Additionally, the coincidence rate (73%,
co-negative 53%, co-positive 20%) was analyzed by comparing the IHC
and DDPCR detection of protein expression and gene mutation
(Fig. S1).The clinical
characteristics and follow-up of 29 patients with DLBCL with MYD88
L265P mutation are summarized in Table III.
 | Table III.Clinical characteristics and
follow-up of patients with diffuse large B cell lymphoma with MYD88
L265P mutation. |
Table III.
Clinical characteristics and
follow-up of patients with diffuse large B cell lymphoma with MYD88
L265P mutation.
| Case | Age (year) | Primary site | Stage | Subtype | Initial
treatment | Survival
status | Follow up
(months) | DDPCR | IHC |
|---|
| 1 | 75 | Joint | IA | ABC | CHOP | Passed away | 79 | 31.3% L265P
Mut | Positive |
| 2 | 60 | CNS | IVA | ABC | R-CHOP + MTX | Alive | 63 | 35.8% L265P
Mut | Negative |
| 3 | 46 | LN | IVB | ABC | R-CHOP + PBSCT | Alive | 61 | 0.14% L265P
Mut | Positive |
| 4 | 69 | Testis | IIIA | ABC | Surgery | Passed away | 46 | 45.1% L265P
Mut | Positive |
| 5 | 60 | Joint | IVA | GCB | Surgery | Alive | 51 | 14.0% L265P
Mut | Positive |
| 6 | 66 | LN | IVA | ABC | Unknown | Unknown |
| 55.0% L265P
Mut | Positive |
| 7 | 82 | LN | IVA | ABC | MTX | Passed away | 1 | 69.1% L265P
Mut | Positive |
| 8 | 59 | Head and neck | IVA | ABC | R-CHOP | Alive | 48 | 22.9% L265P
Mut | Negative |
| 9 | 65 | CNS | IVA | GCB | Unknown | Passed away | 2 | 42.8% L265P
Mut | Negative |
| 10 | 50 | CNS | IVA | ABC | Unknown | Passed away | 1 | 74.8% L265P
Mut | Positive |
| 11 | 51 | CNS | IVA | ABC | Unknown | Passed away | 20 | 25.0% L265P
Mut | Positive |
| 12 | 72 | CNS | IVA | ABC | Unknown | Passed away | 1 | 50.9% L265P
Mut | Positive |
| 13 | 46 | CNS | IVA | ABC | R-CHOP + MTX | Alive | 26 | 96.6% L265P
Mut | Positive |
| 14 | 75 | LN | IIIA | ABC | Surgery | Passed away | 1 | 44.7% L265P
Mut | Negative |
| 15 | 40 | CNS | IVA | ABC | Unknown | Alive | 22 | 0.31% L265P
Mut | Positive |
| 16 | 53 | CNS | IVA | ABC | MTX + TMZ | Passed away | 8 | 44.3% L265P
Mut | Positive |
| 17 | 60 | Head and neck | IVA | GCB | R-CHOP | CR | 21 | 35.7% L265P
Mut | Positive |
| 18 | 50 | LN | IIIB | ABC | Unknown | Passed away | 13 | 0.16% L265P
Mut | Positive |
| 19 | 64 | LN | IVA | ABC | Unknown | Passed away | 2 | 83.7% L265P
Mut | Negative |
| 20 | 55 | CNS | IVA | GCB | R-CHOP + MTX | Passed away | 5 | 95.8% L265P
Mut | Positive |
| 21 | 72 | CNS | IVA | ABC | MTX | Passed away | 10 | 45.7% L265P
Mut | Positive |
| 22 | 53 | CNS | IVA | ABC | Surgery | Alive | 12 | 38.8% L265P
Mut | Positive |
| 23 | 54 | CNS | IVA | GCB | Surgery | Alive | 8 | 32.7% L265P
Mut | Negative |
| 24 | 61 | CNS | IVA | GCB | Surgery | Alive | 3 | 58.3% L265P
Mut | Negative |
| 25 | 59 | CNS | IVA | ABC | Surgery | Alive | 1 | 25.2% L265P
Mut | Positive |
| 26 | 59 | CNS | IVA | ABC | Surgery | Passed away | 45 | 96.99% L265P
Mut | Negative |
| 27 | 64 | CNS | IVA | GCB | R-CHOP + MTX +
TMZ | Passed away | 2 | 53.4% L265P
Mut | Positive |
| 28 | 54 | Joint | IVA | GCB | Unknown | Passed away | 6 | 52.7% L265P
Mut | Negative |
| 29 | 69 | Testis | IVA | ABC | Unknown | Alive | 12 | 42.8% L265P
Mut | Positive |
Follow-up
During the follow-up period of 1–79 months, 45
patients (45%) were followed up until they passed away due to
lymphoma, 5 patients were lost and 50 patients survived. The median
and average survival times were 15 and 26.3 months, respectively.
The 3- and 5-year OS rates of patients with DLBCL were 28.42%
(27/95) and 16.84% (16/95), respectively. The average survival time
of patients treated with rituximab-based multi-agent chemotherapy
was longer (R-CHOP vs. CHOP; 32.5 vs. 23.15 months)
Among patients with positive MYD88 protein
expression, 22 patients passed away (57.89%, 22/38) and 13 survived
(34.21%, 13/38). The median and average survival times were 11 and
17.3 months, respectively. The 3- and 5-year OS rates were 15.79%
(6/38) and 7.89% (3/38), respectively.
Among patients with MYD88 L265P mutation, 16 passed
away (55.17%, 16/29) and 12 survived (41.38%, 12/29). The median
and average survival times were 9 and 17.5 months, respectively.
The 3- and 5-year OS rates were 20.69% (6/29) and 7.89% (3/29),
respectively.
Data analysis and statistics
Chi-square test analysis showed that positive MYD88
expression was significantly associated with sex (female; P=0.023),
extranodal site (CNS; P=0.031), β2-microglobulin (β2-MG; normal;
P=0.039), high expression of Bcl-2 (≥70%) and survival status
(passed away; P=0.042). MYD88 L265P mutation was significantly
related to extranodal site (CNS; P<0.001), β2-MG (normal;
P=0.004), Ann-Arbor stage (stages III–IV; P=0.002) and Eastern
Cooperative Oncology Group performance status (ECOG PS) score (≥2;
P=0.001) (Table I).
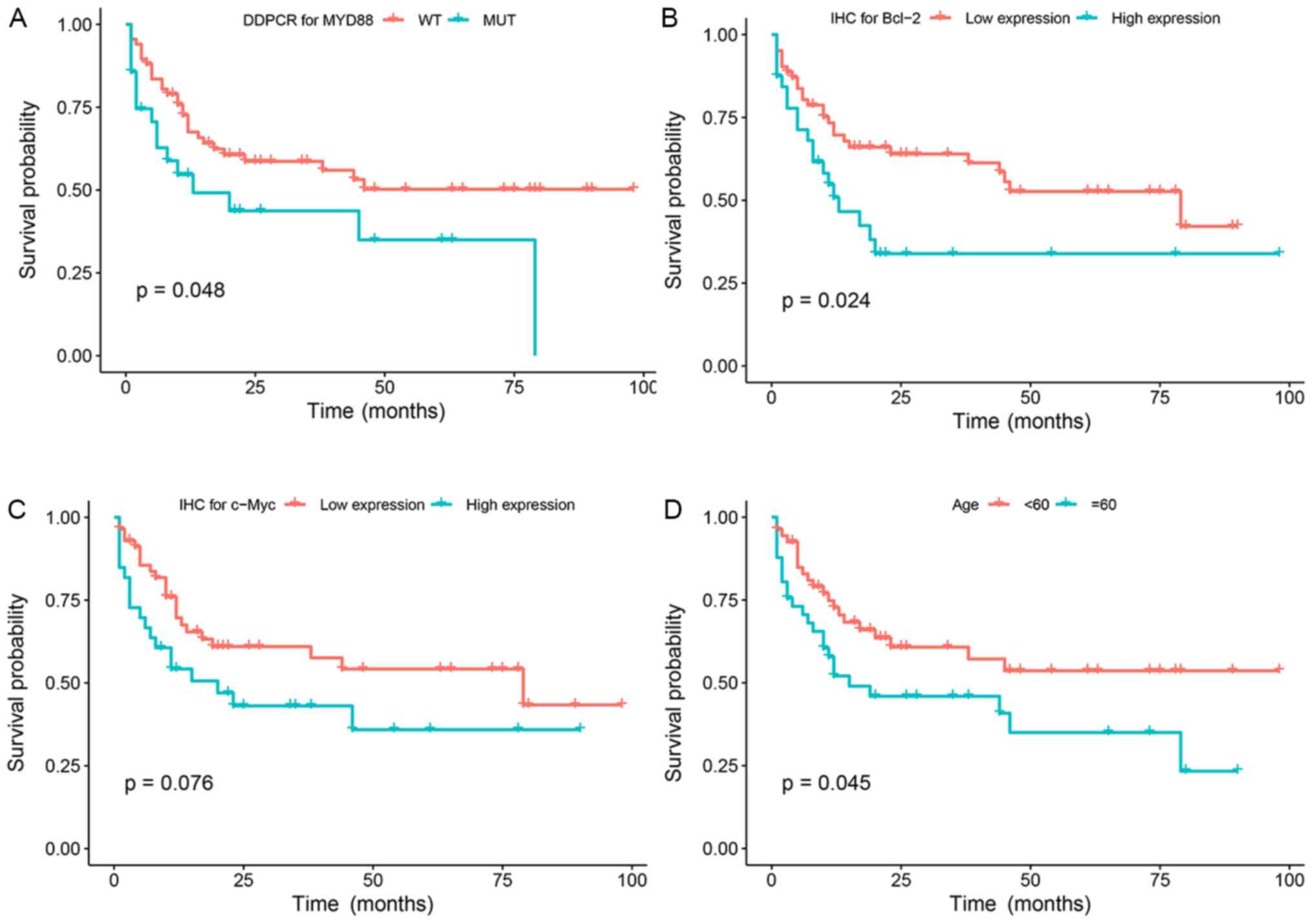
In univariate analysis, age (≥60 years), high levels
of lactic acid dehydrogenase (LDH), low lymphocyte count, rituximab
treatment, high Bcl-2 expression (≥70%), MYD88 expression and MYD88
L265P mutation were significant prognostic factors for OS. In
multivariate analysis, when NCCN-IPI was controlled, MYD88 positive
expression [HR, 1.855, 95% confidence interval (CI), 0.991–3.470],
age ≥60 years (HR, 1.982, 95% CI, 1.065–3.688), high NLR (HR,
0.518, 95% CI, 0.2276–0.969) were the independent prognostic
factors affecting the OS of patients (P<0.05). However, MYD88
L265P mutation was not an independent prognostic factor of OS
(P=0.07) (Table IV; Fig. 5A-G).
 | Table IV.Clinicopathological characteristics
affecting PFS and OS. |
Table IV.
Clinicopathological characteristics
affecting PFS and OS.
|
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|---|
| Clinicopathological
characteristics | PFS P-value | OS P-value | PFS HR (95%
CI) | OS P-value | HR (95% CI) | P-value |
|---|
| Age |
| <60
vs. ≥60 | 0.286 |
0.045a |
|
| 1.982
(1.065–3.688) | 0.031a |
| Sex (n=100) |
| Male
vs. female | 0.452 | 0.393 |
|
|
|
|
| Extranodal
involvement |
| CNS vs.
other | 0.535 | 0.146 |
|
|
|
|
| Ann-Arbor
stage |
| Low (I–II) vs. high
(III–IV) | 0.899 | 0.621 |
|
|
|
|
| β2-MB (n=55) |
| Normal
vs. above normal | 0.732 | 0.981 |
|
|
|
|
| B symptom
(n=100) |
| Absent
vs. present | 0.359 | 0.872 |
|
|
|
|
| ECOG performance
status (n=100) |
| <2
vs. ≥2 | 0.267 | 0.526 |
|
|
|
|
| LDH level
(n=99) |
| Normal
vs. above normal | 0.883 | 0.03a |
|
|
| 0.241 |
| Ann-Arbor
stage |
| GCB vs.
ABC | 0.5 | 0.763 |
|
|
| 0.625 |
| Therapy (n=53) |
|
Rituximab | 0.299 | 0.002a |
|
|
|
|
|
Others |
| IHC |
| Bcl-6
(n=100) | 0.365 | 0.541 |
|
|
|
|
| Bcl-2
≥70 vs. <70% (n=98) | 0.576 | 0.024a |
|
|
| 0.218 |
| c-Myc
≥40 vs. <40% (n=94) | 0.782 | 0.076 |
|
|
|
|
| c-Myc
(≥40%)/BCL-2 (≥70%) co-expression (n=94) | 0.707 | 0.64 |
|
|
|
|
| p53
(n=91) | 0.685 | 0.618 |
|
|
|
|
| Ki-67
(≥60 vs. <60% (n=100) | 0.169 | 0.914 |
|
|
|
|
| MYD88
positive vs. negative expression (n=100) | 0.796 | 0.0017a |
|
| 1.855
(0.991–3.470) | 0.05a |
| MYD88
MUT vs. WT (n=100) | 0.624 | 0.048a |
|
|
| 0.308 |
| Hematologic
indicators (n=100) |
|
Monocyte count (normal vs. low
vs. high) | 0.274 | 0.454 |
|
|
|
|
|
Neutrophil count (normal vs.
low vs. high) | 0.237 | 0.399 |
|
|
|
|
|
Lymphocyte count (normal vs.
< normal | 0.145 | 0.0045a |
|
|
| 0.109 |
|
Platelet count (normal vs. low
vs. high) | 0.811 | 0.276 |
|
|
|
|
|
Hemoglobin (normal vs.
low) | 0.668 | 0.68 |
|
|
|
|
|
High-NLR (≥2.81) vs. low-NLR
(<2.81) | 0.776 | 0.053 |
|
| 0.518
(0.2276–0.969) | 0.04a |
|
High-LMR (≥2.71) vs. low-LMR
(<2.71) | 0.280 | 0.083 |
|
|
|
|
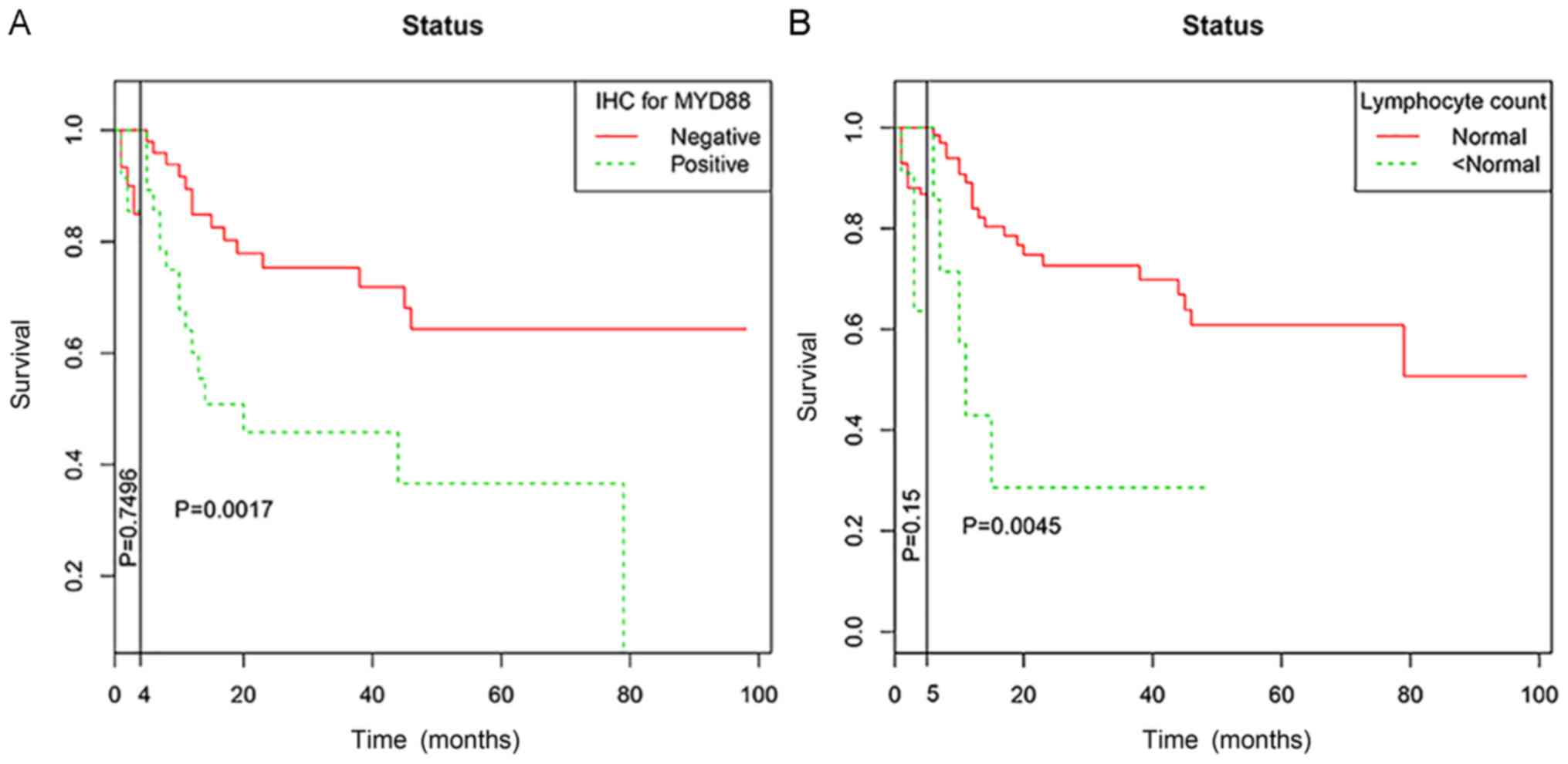
As for the crossing of survival curves in univariate
analysis, landmark analysis was performed according to a landmark
point at 4 months for MYD88 expression and 5 months for lymphocyte
count, with the statistical differences in survival rates
calculated separately for events that occurred up to landmark point
time after randomization, events that occurred between landmark
point time and the end of the follow-up period (Fig. 6).
Discussion
In the present study, expression of MYD88 in DLBCL
was investigated using IHC and DDPCR. IHC was used to detect
protein expression of MYD88. Only a few studies have reported on
using IHC to detect MYD88 protein expression. Choi et al
(29) found that MYD88 was
overexpressed in 38.7% (48/124) of DLBCL cases. This finding was
consistent with the results of the present study (38%).
Furthermore, positive expression of MYD88 was correlated with sex,
β2-MG and survival status. The correlation with sex and β2-MG has
yet to be proposed, and the underlying mechanisms should be studied
further. Notably, positive MYD88 expression was positively
correlated with high expression of Bcl-2 in the present study,
which could indicate that MYD88 and Bcl-2 inhibit tumor cell
apoptosis, promote tumor cell proliferation, enhance the role of
other oncogenes and induce lymphoma. Bcl-2 protein accelerates the
growth of lymphoma and promotes the resistance of tumor cells to
chemotherapy drugs (31,32). Positive MYD88 expression was
positively correlated with high Ki-67 expression. This finding
suggested that MYD88 may inhibit tumor cell apoptosis and promote
tumor proliferation.
Meanwhile, the mutation of MYD88 L265P was studied
at a molecular level by DDPCR. Previous studies have provided
evidence that the MYD88 L265P mutation is associated with a poor
prognosis in patients with DLBCL who have been treated with
standard R-CHOP immunochemotherapy (19,33,34).
These findings are in agreement with the present results. However,
some studies have demonstrated that the mutation of MYD88 does not
affect the OS rate of patients with lymphoma (35,36).
Therefore, this topic needs further investigation. In previous
studies, the MYD88 L265P mutation was found in 6.5–19% of DLBCL
cases (12,19,29).
In the present study, the MYD88 L265P mutation was found in 29% of
patients with DLBCL. This mutation was also positively correlated
with the ECOG score; patients with a higher score had a higher
mutation rate compared with those with a lower score (72.4 vs.
27.6%). An ECOG score is an index used to understand the general
health status, tolerance to treatment and physical status of
patients. Lee et al (37)
performed a meta-analysis on the MYD88 L265P gene mutation in
lymphoma and found that MYD88 L265P mutation is related to age,
prognosis and immunophenotyping, but it is not related to clinical
stage and sex. The present results revealed that this gene mutation
is associated with Ann-Arbor staging, which may be associated with
a large proportion of PCNSL, thereby increasing the mutation rate
of patients in stages III–IV.
In the current study, the MYD88 L265P mutation was
found to be common in extranodal DLBCL, including the CNS and
testes, and associated with poor prognosis. However, the MYD88
L265P mutation was not an independent prognostic factor of OS
(P=0.07). The survival time of the elderly patients was shorter
(P<0.05), which might be related to a decrease in immune system
function and tolerance to chemotherapeutic drugs. Patients might
also be affected by primary diseases other than lymphoma. By
comparison, patients with PCNSL were more likely to present
advanced-stage diseases and were associated with a lower average
survival (17.4 months) compared with patients with nodal DLBCL
(23.8 months). This observation might be related to the special
growth site of the tumor. Tumors occurring in the brain are
affected by the blood-brain barrier, which could decrease the
efficacy of chemotherapy. Patients with high LDH levels had poor
prognosis rates, which might be related to the metabolism of tumor
cells in patients with lymphoma. The enhanced glycolysis and
necrotic tumor tissues in patients with lymphoma can increase serum
LDH levels. LDH levels can also be used as an independent
prognostic factor of various tumors, such as breast cancer and
renal cell carcinoma (38,39). The effect of NCCN-IPI score on the
survival time of patients indicates that the prognosis of patients
with a high score is poor (40).
The relationship between indicators in the blood and prognosis of
pre-treated patients with DLBCL were analyzed. Patients with low
and high lymphocyte counts had a poorer prognosis, possibly because
lymphocytes also play an important role in antitumor immunity.
Given the lack of sufficient antitumor immunity, lymphocyte
downregulation can promote tumor recurrence and metastasis
(41). High NLR was found to be an
independent prognostic factor affecting the OS of patients.
Previous studies demonstrated that high NLR is related to an
increase in monocyte chemoattractant protein-1, IL-1R-α, IL-6,
IL-7, IL-8, IL-12 and IL-17 in the peripheral blood (42,43).
These cytokines can establish and maintain an immune
microenvironment that promotes tumor invasion. The poor prognosis
of DLBCL caused by high NLR may be related to the immune
microenvironment. In the present study, the expression and mutation
of MYD88 were not significantly correlated with PFS. These findings
might be due to the number of patients who could be followed up.
MYD88 has a high mutation rate at protein and molecular levels in
ABC-DLBCL and PCNSL, and the mutation rate is high in ABC-DLBCL
with poor prognosis (44). This
result might be related to the key role of MYD88 protein in the
NF-κB pathway, overexpression can lead to the aberrant activation
of this pathway (12,45,46),
although the activation of the NF-κB pathway maintains the activity
of ABC-DLBCL cells it is unable to maintain the activity of
GCB-DLBCL cells (47). The MYD88
mutation in patients with ABC-DLBCL and PCNSL is of great
significance to evaluate the prognosis of DLBCL, suggesting that
this is a potential therapeutic target with immunotherapies. It has
previously been reported that the MYD88 mutation rate of primary
testicular diffuse large B cell lymphoma (PT-DLBCL) is 68%, and
associated with a poor survival (21,48,49).
Mutations were detected in three patients with PT-DLBCL (2/3) in
the present study. During the follow-up of these three patients,
one patient with the mutation passed away and the other gave up
treatment, and the wild-type patient survived until the end of the
follow-up. As the sample size used for PT-DLBCL was small, specific
conclusions about this finding cannot be made. The mutation rate of
MYD88 in PCNSL was 66.67% (16/24). A positive correlation was
observed between them, but the mutation did not affect OS and PFS
in patients. Studies have reported that MYD88 L265P mutation occurs
in PCNSL with poor prognosis (50,51).
The present study also included one patient with primary cutaneous
DLBCL-LT, which was detected as the MYD88 wild-type. DLBCL-LT was
the most aggressive primary cutaneous B cell lymphoma subtype and
was associated with an increased risk of extracutaneous spread and
poor prognosis. In previous studies, the MYD88 mutation rate of
DLBCL-LT is reported to be 59%, and prognosis is poor (20,52).
Our group has recorded 1,831 lymphoma cases in our
department over the past 10 years, and it was found that the
incidence of DLBCL was as high as 57% (741/1,294) in B cell
lymphoma (Fig. S2A and B). This
is consistent with the findings of Li et al (53) who revealed that the incidence of
DLBCL is 50.18% (3,328/6,632).
These results indicated that MYD88 protein is highly
expressed in PCNSL, which could be observed easily, especially in
tumor cells around blood vessels. Our data would support that the
hypothesis that MYD88 had a function of labeling tumor cells.
However, when MYD88 protein expression in DLBCL occurred in lymph
nodes, some problems, such as non-specific background coloring and
false positive in some cases, were encountered.
Different techniques, such as Sanger sequencing and
allele-specific quantitative PCR, have been used to detect MYD88
mutations in lymphoma (23).
However, these methods require large samples and cannot be used as
routine detection methods. DDPCR is a highly sensitive gene
mutation detection technique with a low DNA requirement. DDPCR is a
valuable method in current diagnostic parameters, especially when
the available amount of DNA is limited. It is suitable for
screening bone marrow, peripheral blood cells, circulating free DNA
and minimal residual disease (54,55).
It is also a highly reliable method that can be applied to detect
MYD88 gene mutations in cerebrospinal fluid even when the DNA input
is low (56). To the best of the
authors' knowledge, this is the first time that the DDPCR technique
has been applied to detect a MYD88 mutation in DLBCL FFPE tumor
tissues and been used to compare the results with IHC data. The
coincidence rate of the results of MYD88 expression between IHC and
DDPCR results was 73% (73/100). However, statistical analysis
showed that the protein expression of MYD88 was positively
correlated with the MYD88 L265P mutation, suggesting that using IHC
to detect MYD88 expression could also be used as a preliminary
screening method for lymphoma.
In conclusion, IHC and DDPCR were performed to study
the protein expression and mutation rates of MYD88 in DLBCL. These
analyses revealed that the expression and mutation rates of MYD88
were higher in ABC-DLBCL compared with those of GCB-DLBCL. The
expression of MYD88 protein was related to the high expression of
Bcl-2 and Ki-67, indicating that MYD88 was related to tumor
proliferation. MYD88 mutation was associated with β2-MG, Ann-Arbor
staging and ECOG PS score. The expression and mutation of MYD88
protein were related to OS but not to PFS. The poor prognosis of
patients with DLBCL was related to age, LDH level, lymphocyte
count, NLR, treatment with rituximab and high Bcl-2 expression.
MYD88 was associated with shortened survival, and might ultimately
provide the molecular tools for immunotherapy assessment, and
identify the patients at an increased risk of associated DLBCL
events. The main limitation of the present study is that it was
conducted at a single center so the sample was too small to reach
firm conclusions. Therefore, further verification is needed in a
larger sample.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
This work was supported by the project of National
Natural Science Foundation of China (grant no. 81660036).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JN, XL and ZM conceived and designed the study; SL,
AN and GA performed the experiments; WC, HG and LSJ analyzed the
data; WZ and ZM interpreted the data. JN wrote the manuscript; JN,
XL and WZ gave final approval of the version to be published. All
authors read and approved the manuscript.
Ethics approval and consent to
participate
The study protocol was approved by the Ethics Review
Board of The First Affiliated Hospital of Xinjiang Medical
University (approval no. 20160218-13). Written informed consent was
obtained from all participants. All of the procedures were
performed in accordance with the Declaration of Helsinki and
relevant policies in China.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Swerdlow SH, Campo E, Harris NL, Jaffe ES,
Pileri SA, Stein H and Thiele J: WHO Classification of tumours of
haematopoietic and lymphoid tissues. 4th. International Agency for
Research on Cancer; Lyon: 2017
|
|
2
|
Li XQ, Li GD, Gao ZF, Zhou XG and Zhu XZ:
Distribution pattern of lymphoma subtypes in China: A nationwide
multicenter study of 10002 cases. Zhen Duan Xue Li Lun Yu Shi Jian
Bian Ji Bu. 25–29. 2012.
|
|
3
|
Al-Hamadani M, Habermann TM, Cerhan JR,
Macon WR, Maurer MJ and Go RS: Non-Hodgkin lymphoma subtype
distribution, geodemographic patterns, and survival in the US: A
longitudinal analysis of the National Cancer Data Base from 1998 to
2011. Am J Hematol. 90:790–795. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Szumeraciećkiewicz A, Gałązka K, Szpor J,
Rymkiewicz G, Jesionek-Kupnicka D, Gruchała A,
Ziarkiewicz-Wróblewska B, Poniatowska-Broniek G, Demczuk S and
Prochorec-Sobieszek M: Distribution of lymphomas in Poland
according to World Health Organization classification: Analysis of
11718 cases from National Histopathological Lymphoma Register
project - the Polish Lymphoma Research Group study. Int J Clin Exp
Pathol. 7:3280–3286. 2014.PubMed/NCBI
|
|
5
|
Wright G, Tan B, Rosenwald A, Hurt EH,
Wiestner A and Staudt LM: A gene expression-based method to
diagnose clinically distinct subgroups of diffuse large B cell
lymphoma. Proc Natl Acad Sci USA. 100:9991–9996. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Alizadeh AA, Eisen MB, Davis RE, Ma C,
Lossos IS, Rosenwald A, Boldrick JC, Sabet H, Tran T, Yu X, et al:
Distinct types of diffuse large B-cell lymphoma identified by gene
expression profiling. Nature. 403:503–511. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Rubenstein JL, Gupta NK, Mannis GN,
Lamarre AK and Treseler P: How I treat CNS lymphomas. Blood.
122:2318–2330. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Johnson S, Feldman M and Krishnamurthi V:
Primary testicular lymphoma. J Urol. 193:315–316. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Horne MJ and Adeniran AJ: Primary diffuse
large B-cell lymphoma of the testis. Arch Pathol Lab Med.
135:1363–1367. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yanga LI, Liu ZG and Hao LC: Effectiveness
and safety of rituximab plus CHOP chemotherapy for treating
non-Hodgkin lymphoma among Chinese people: A meta-analysis. J Evid
Based Med. 11:112–116. 2011.
|
|
11
|
Van Den NesteE, Schmitz N, Mounier N, Gill
D, Linch D, Trneny M, Bouadballah R, Radford J, Bargetzi M, Ribrag
V, et al: Outcomes of diffuse large B-cell lymphoma patients
relapsing after autologous stem cell transplantation: An analysis
of patients included in the CORAL study. Bone Marrow Transplant.
52:216–221. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ngo VN, Young RM, Schmitz R, Jhavar S,
Xiao W, Lim KH, Kohlhammer H, Xu W, Yang Y, Zhao H, et al:
Oncogenically active MYD88 mutations in human lymphoma. Nature.
470:115–119. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
O'Neill LA, Fitzgerald KA and Bowie AG:
The Toll-IL-1 receptor adaptor family grows to five members. Trends
Immunol. 24:286–290. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Motshwene PG, Moncrieffe MC, Grossmann JG,
Kao C, Ayaluru M, Sandercock AM, Robinson CV, Latz E and Gay NJ: An
oligomeric signaling platform formed by the Toll-like receptor
signal transducers MyD88 and IRAK-4. J Biol Chem. 284:25404–25411.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Gay NJ, Symmons MF, Gangloff M and Bryant
CE: Assembly and localization of Toll-like receptor signalling
complexes. Nat Rev Immunol. 14:546–558. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Jardin F: Next generation sequencing and
the management of diffuse large B-cell lymphoma: From whole exome
analysis to targeted therapy. Discov Med. 18:51–65. 2014.PubMed/NCBI
|
|
17
|
Vermaat JS, Somers SF, de Wreede LC, Kraan
W, de Groen RA, Schrader AM, Kerver ED, Scheepstra CG, Berenschot
H, Deenik W, et al: MYD88 mutations identify a molecular subgroup
of diffuse large B-cell lymphoma with an unfavourable prognosis.
Haematologica. 105:424–434. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Montesinos-Rongen M, Godlewska E, Brunn A,
Wiestler OD, Siebert R and Deckert M: Activating L265P mutations of
the MYD88 gene are common in primary central nervous system
lymphoma. Acta Neuropathol. 122:791–792. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Takano S, Hattori K, Ishikawa E, Narita Y,
Iwadate Y, Yamaguchi F, Nagane M, Akimoto J, Oka H, Tanaka S, et
al: MyD88 mutation in the elderly predicts a poor prognosis in
primary CNS lymphoma: Multi-institutional analysis. World
Neurosurg. 112:e69–e73. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Pham-Ledard A, Beylot-Barry M, Barbe C,
Leduc M, Petrella T, Vergier B, Martinez F, Cappellen D, Merlio JP
and Grange F: High frequency and clinical prognostic value of MYD88
L265P mutation in primary cutaneous diffuse large B-cell lymphoma,
leg-type. JAMA Dermatol. 150:1173–1179. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kraan W, van Keimpema M, Horlings HM,
Schilder-Tol EJ, Oud ME, Noorduyn LA, Kluin PM, Kersten MJ,
Spaargaren M and Pals ST: High prevalence of oncogenic MYD88 and
CD79B mutations in primary testicular diffuse large B-cell
lymphoma. Leukemia. 28:719–720. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Varettoni M, Arcaini L, Zibellini S,
Boveri E, Rattotti S, Riboni R, Corso A, Orlandi E, Bonfichi M,
Gotti M, et al: Prevalence and clinical significance of the MYD88
(L265P) somatic mutation in Waldenstrom's macroglobulinemia and
related lymphoid neoplasms. Blood. 121:2522–2528. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Xu L, Hunter ZR, Yang G, Zhou Y, Cao Y,
Liu X, Morra E, Trojani A, Greco A, Arcaini L, et al: MYD88 L265P
in Waldenström macroglobulinemia, immunoglobulin M monoclonal
gammopathy, and other B-cell lymphoproliferative disorders using
conventional and quantitative allele-specific polymerase chain
reaction. Blood. 121:2051–2058. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Treon SP, Xu L, Yang G, Zhou Y, Liu X, Cao
Y, Sheehy P, Manning RJ, Patterson CJ, Tripsas C, et al: MYD88
L265P somatic mutation in Waldenström's macroglobulinemia. N Engl J
Med. 367:826–833. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Schmitz R, Wright GW, Huang DW, Johnson
CA, Phelan JD, Wang JQ, Roulland S, Kasbekar M, Young RM, Shaffer
AL, et al: Genetics and Pathogenesis of Diffuse Large B-Cell
Lymphoma. N Engl J Med. 378:1396–1407. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Weber AN, Cardona Gloria Y, Çınar Ö,
Reinhardt HC, Pezzutto A and Wolz OO: Oncogenic MYD88 mutations in
lymphoma: Novel insights and therapeutic possibilities. Cancer
Immunol Immunother. 67:1797–1807. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Arber DA, Orazi A, Hasserjian R, Thiele J,
Borowitz MJ, Le Beau MM, Bloomfield CD, Cazzola M and Vardiman JW:
The 2016 revision to the World Health Organization classification
of myeloid neoplasms and acute leukemia. Blood. 127:2391–2405.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
World Medical Association, . World Medical
Association Declaration of Helsinki: Ethical Principles for Medical
Research Involving Human Subjects. JAMA. 310:2191–2194. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Choi JW, Kim Y, Lee JH and Kim YS: MYD88
expression and L265P mutation in diffuse large B-cell lymphoma.
Human Pathology. 44:1375–1381. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Wang J, Gao K, Lei W, Dong L, Xuan Q, Feng
M, Wang J, Ye X, Jin T, Zhang Z, et al: Lymphocyte-to-monocyte
ratio is associated with prognosis of diffuse large B-cell
lymphoma: Correlation with CD163 positive M2 type tumor-associated
macrophages, not PD-1 positive tumor-infiltrating lymphocytes.
Oncotarget. 8:5414–5425. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Hermine O, Haioun C, Lepage E, dAgay MF,
Briere J, Lavignac C, Fillet G, Salles G, Marolleau JP, Diebold J,
et al: Prognostic Significance of bcl-2 Protein Expression in
Aggressive Non-Hodkin's Lymphoma. Blood. 87:265–272. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Reed JC, Miyashita T, Takayama S, Wang HG,
Sato T, Krajewski S, Aimé-Sempé C, Bodrug S, Kitada S and Hanada M:
BCL-2 family proteins: Regulators of cell death involved in the
pathogenesis of cancer and resistance to therapy. J Cell Biochem.
60:23–32. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Xu Y, Li J, Ouyang J, Li J, Xu J, Zhang Q,
Yang Y, Zhou M, Wang J, Zhang C, et al: Prognostic relevance of
protein expression, clinical factors, and MYD88 mutation in primary
bone lymphoma. Oncotarget. 8:65609–65619. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Treon SP, Gustine J, Xu L, Manning RJ,
Tsakmaklis N, Demos M, Meid K, Guerrera ML, Munshi M, Chan G, et
al: MYD88 wild-type Waldenstrom Macroglobulinaemia: Differential
diagnosis, risk of histological transformation, andoverall
survival. Br J Haematol. 180:1802017.
|
|
35
|
Abeykoon JP, Paludo J, King RL, Ansell SM,
Gertz MA, LaPlant BR, Halvorson AE, Gonsalves WI, Dingli D, Fang H,
et al: MYD88 mutation status does not impact overall survival in
Waldenström macroglobulinemia. Am J Hematol. 93:187–194. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Lee YS, Liu J, Fricano KA, Webb EM,
Toolsie DR, Jones S, Rhoads JA, Vij R, Cashen AF, Abboud CN, et al:
Lack of a prognostic impact of the MyD88 L265P mutation for diffuse
Large B cell lymphoma patients undergoing autologous stem cell
transplantation. Biol Blood Marrow Transplant. 23:2199–2204. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Lee JH, Jeong H, Choi JW, Oh H and Kim YS:
Clinicopathologic significance of MYD88 L265P mutation in diffuse
large B-cell lymphoma: A meta-analysis. Sci Rep. 7:17852017.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Dong T, Liu Z, Xuan Q, Wang Z, Ma W and
Zhang Q: Tumor LDH-A expression and serum LDH status are two
metabolic predictors for triple negative breast cancer brain
metastasis. Sci Rep. 7:60692017. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Motzer RJ, Escudier B, Bukowski R, Rini
BI, Hutson TE, Barrios CH, Lin X, Fly K, Matczak E and Gore ME:
Prognostic factors for survival in 1059 patients treated with
sunitinib for metastatic renal cell carcinoma. Br J Cancer.
108:2470–2477. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Biccler J, Eloranta S, de Nully Brown P,
Frederiksen H, Jerkeman M, Smedby KE, Bøgsted M and El-Galaly TC:
Simplicity at the cost of predictive accuracy in diffuse large
B-cell lymphoma: A critical assessment of the R-IPI, IPI, and
NCCN-IPI. Cancer Med. 7:114–122. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Stotz M, Pichler M, Absenger G, Szkandera
J, Arminger F, Schaberl-Moser R, Samonigg H, Stojakovic T and
Gerger A: The preoperative lymphocyte to monocyte ratio predicts
clinical outcome in patients with stage III colon cancer. Br J
Cancer. 110:435–440. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Motomura T, Shirabe K, Mano Y, Muto J,
Toshima T, Umemoto Y, Fukuhara T, Uchiyama H, Ikegami T, Yoshizumi
T, et al: Neutrophil-lymphocyte ratio reflects hepatocellular
carcinoma recurrence after liver transplantation via inflammatory
microenvironment. J Hepatol. 58:58–64. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Kantola T, Klintrup K, Väyrynen JP,
Vornanen J, Bloigu R, Karhu T, Herzig KH, Näpänkangas J, Mäkelä J,
Karttunen TJ, et al: Stage-dependent alterations of the serum
cytokine pattern in colorectal carcinoma. Br J Cancer.
107:1729–1736. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Hans CP, Weisenburger DD, Greiner TC,
Gascoyne RD, Delabie J, Ott G, Müller-Hermelink HK, Campo E,
Braziel RM, Jaffe ES, et al: Confirmation of the molecular
classification of diffuse large B-cell lymphoma by
immunohistochemistry using a tissue microarray. Blood. 103:275–282.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Davis RE, Ngo VN, Lenz G, Tolar P, Young
RM, Romesser PB, Kohlhammer H, Lamy L, Zhao H, Yang Y, et al:
Chronic active B-cell-receptor signalling in diffuse large B-cell
lymphoma. Nature. 463:88–92. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Compagno M, Lim WK, Grunn A, Nandula SV,
Brahmachary M, Shen Q, Bertoni F, Ponzoni M, Scandurra M, Califano
A, et al: Mutations of multiple genes cause deregulation of
NF-kappaB in diffuse large B-cell lymphoma. Nature. 459:717–721.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Davis RE, Brown KD, Siebenlist U and
Staudt LM: Constitutive nuclear factor kappaB activity is required
for survival of activated B cell-like diffuse large B cell lymphoma
cells. J Exp Med. 194:1861–1874. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Frick M, Bettstetter M, Bertz S,
Schwarz-Furlan S, Hartmann A, Richter T, Lenze D, Hummel M,
Dreyling M, Lenz G, et al: Mutational frequencies of CD79B and
MYD88 vary greatly between primary testicular DLBCL and
gastrointestinal DLBCL. Leuk Lymphoma. 59:1260–1263. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Chapuy B, Roemer MG, Stewart C, Tan Y, Abo
RP, Zhang L, Dunford AJ, Meredith DM, Thorner AR, Jordanova ES, et
al: Targetable genetic features of primary testicular and primary
central nervous system lymphomas. Blood. 127:869–881. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Ollila TA and Olszewski AJ: Extranodal
diffuse large B cell lymphoma: Molecular features, prognosis, and
risk of central nervous system recurrence. Curr Treat Options
Oncol. 19:382018. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Hattori K, Sakata-Yanagimoto M, Okoshi Y,
Goshima Y, Yanagimoto S, Nakamoto-Matsubara R, Sato T, Noguchi M,
Takano S, Ishikawa E, et al: MYD88 (L265P) mutation is associated
with an unfavourable outcome of primary central nervous system
lymphoma. Br J Haematol. 177:492–494. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Fox LC, Yannakou CK, Ryland G, Lade S,
Dickinson M, Campbell BA and Prince HM: Molecular mechanisms of
disease progression in primary cutaneous diffuse large B-cell
lymphoma, leg type during ibrutinib therapy. Int J Mol Sci.
19:17582018. View Article : Google Scholar
|
|
53
|
Li XQ, Li GD, Gao ZF, Zhou XG and Zhu XZ:
Distribution pattern of lymphoma subtypes in China: A nationwide
multicenter study of 10002 cases. J Diagn Concepts Pract.
11:111–115. 2012.
|
|
54
|
Komatsubara KM and Sacher AG: Circulating
tumor DNA as a liquid biopsy: Current clinical applications and
future directions. Oncology (Williston Park). 31:618–627.
2017.PubMed/NCBI
|
|
55
|
Drandi D, Genuardi E, Dogliotti I,
Ferrante M, Jiménez C, Guerrini F, Schirico ML, Mantoan B, Vittorio
Muccio V, Lia G, et al: Highly sensitive MYD88L265P mutation
detection by droplet digital PCR in Waldenström macroglobulinemia.
Haematologica. 103:1029–1037. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Hiemcke-Jiwa LS, Minnema MC, Radersma-van
Loon JH, Jiwa NM, de Boer M, Leguit RJ, de Weger RA and Huibers MM:
The use of droplet digital PCR in liquid biopsies: A highly
sensitive technique for MYD88 p.(L265P) detection in cerebrospinal
fluid. Hematol Oncol. 36:429–435. 2018. View Article : Google Scholar : PubMed/NCBI
|