|
1
|
Fearon K, Strasser F, Anker SD, Bosaeus I,
Bruera E, Fainsinger RL, Jatoi A, Loprinzi C, MacDonald N,
Mantovani G, et al: Definition and classification of cancer
cachexia: An international consensus. Lancet Oncol. 12:489–495.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
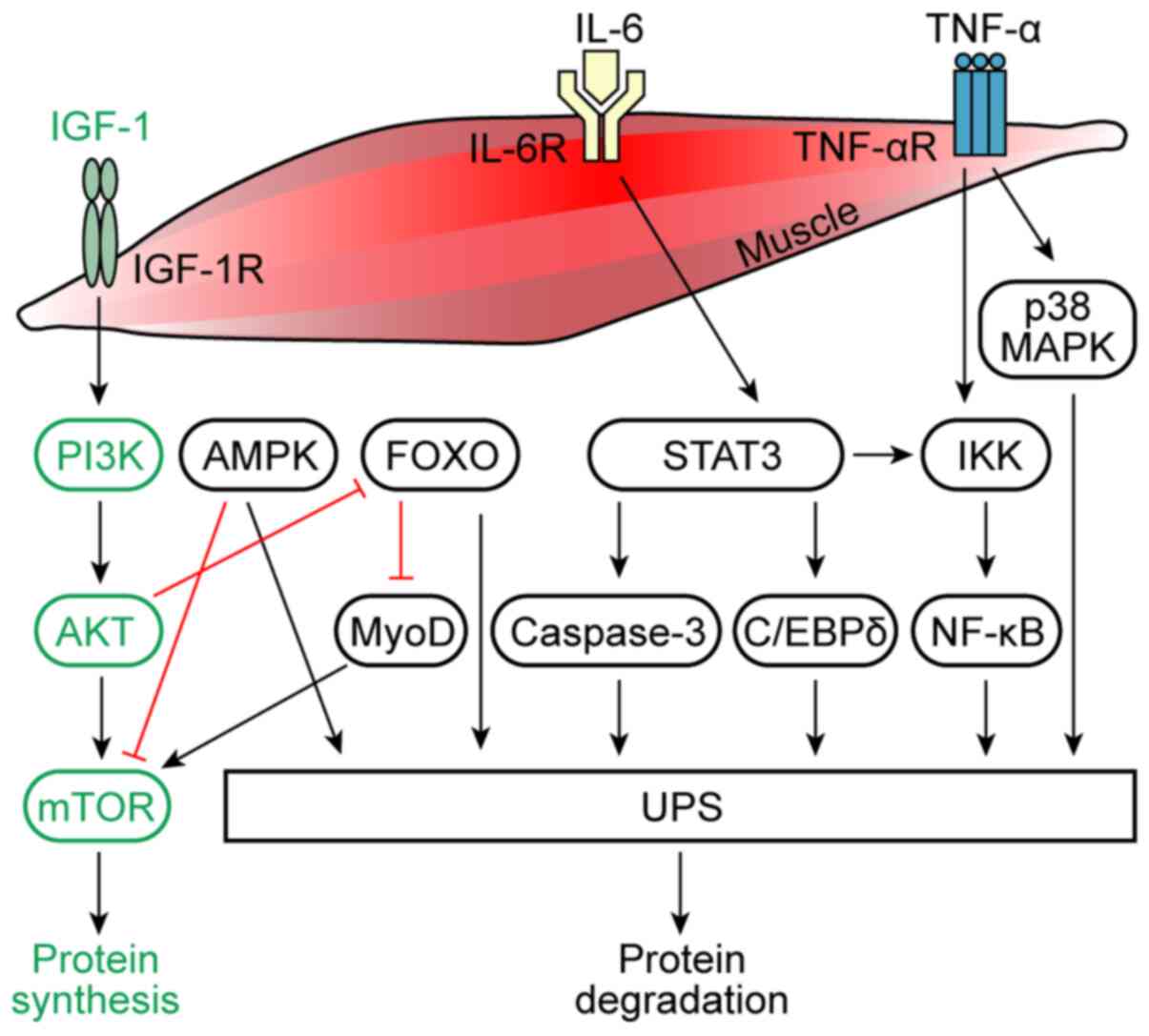
Blum D, Stene GB, Solheim TS, Fayers P,
Hjermstad MJ, Baracos VE, Fearon K, Strasser F and Kaasa S;
Euro-Impact: Validation of the consensus-definition for cancer
cachexia and evaluation of a classification model-a study based on
data from an international multicentre project (EPCRC-CSA). Ann
Oncol. 25:1635–1642. 2014. View Article : Google Scholar : PubMed/NCBI
|
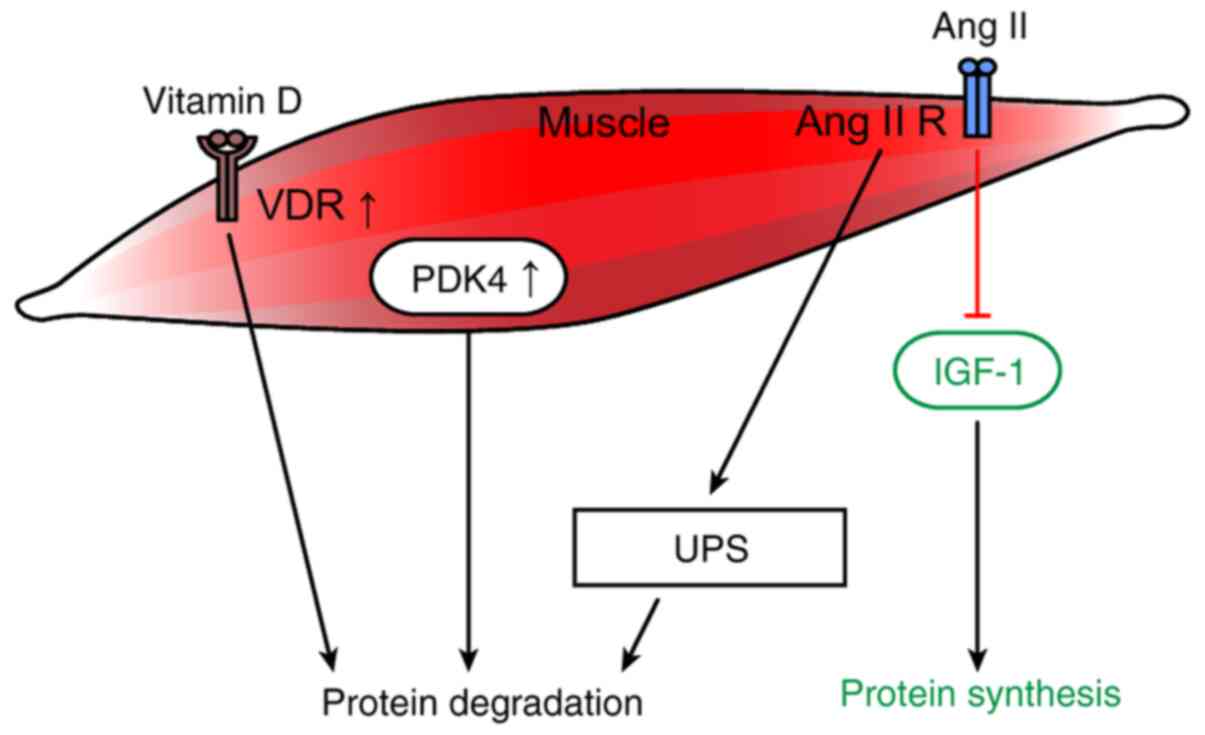
|
3
|
Baumgartner RN, Koehler KM, Gallagher D,
Romero L, Heymsfield SB, Ross RR, Garry PJ and Lindeman RD:
Epidemiology of sarcopenia among the elderly in New Mexico. Am J
Epidemiol. 147:755–763. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Emery PW, Edwards RH, Rennie MJ, Souhami
RL and Halliday D: Protein synthesis in muscle measured in vivo in
cachectic patients with cancer. Br Med J (Clin Res Ed).
289:584–586. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Warnold I, Lundholm K and Schersten T:
Energy balance and body composition in cancer patients. Cancer Res.
38:1801–1807. 1978.PubMed/NCBI
|
|
6
|
Chang VT, Xia Q and Kasimis B: The
functional assessment of anorexia/cachexia therapy (FAACT) appetite
scale in veteran cancer patients. J Support Oncol. 3:377–382.
2005.PubMed/NCBI
|
|
7
|
Martin L, Birdsell L, Macdonald N, Reiman
T, Clandinin MT, McCargar LJ, Murphy R, Ghosh S, Sawyer MB and
Baracos VE: Cancer cachexia in the age of obesity: Skeletal muscle
depletion is a powerful prognostic factor, independent of body mass
index. J Clin Oncol. 31:1539–1547. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Dewys WD, Begg C, Lavin PT, Band PR,
Bennett JM, Bertino JR, Cohen MH, Douglass HO Jr, Engstrom PF,
Ezdinli EZ, et al: Prognostic effect of weight loss prior to
chemotherapy in cancer patients. Eastern Cooperative Oncology
Group. Am J Med. 69:491–497. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Dunne RF, Roussel B, Culakova E, Pandya C,
Fleming FJ, Hensley B, Magnuson AM, Loh KP, Gilles M, Ramsdale E,
et al: Characterizing cancer cachexia in the geriatric oncology
population. J Geriatr Oncol. 10:415–419. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Sadeghi M, Keshavarz-Fathi M, Baracos V,
Arends J, Mahmoudi M and Rezaei N: Cancer cachexia: Diagnosis,
assessment, and treatment. Crit Rev Oncol Hematol. 127:91–104.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Tazi E and Errihani H: Treatment of
cachexia in oncology. Indian J Palliat Care. 16:129–137. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Li YP, Chen Y, John J, Moylan J, Jin B,
Mann DL and Reid MB: TNF-alpha acts via p38 MAPK to stimulate
expression of the ubiquitin ligase atrogin1/MAFbx in skeletal
muscle. FASEB J. 19:362–370. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bonetto A, Aydogdu T, Jin X, Zhang Z, Zhan
R, Puzis L, Koniaris LG and Zimmers TA: JAK/STAT3 pathway
inhibition blocks skeletal muscle wasting downstream of IL-6 and in
experimental cancer cachexia. Am J Physiol Endocrinol Metab.
303:E410–421. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
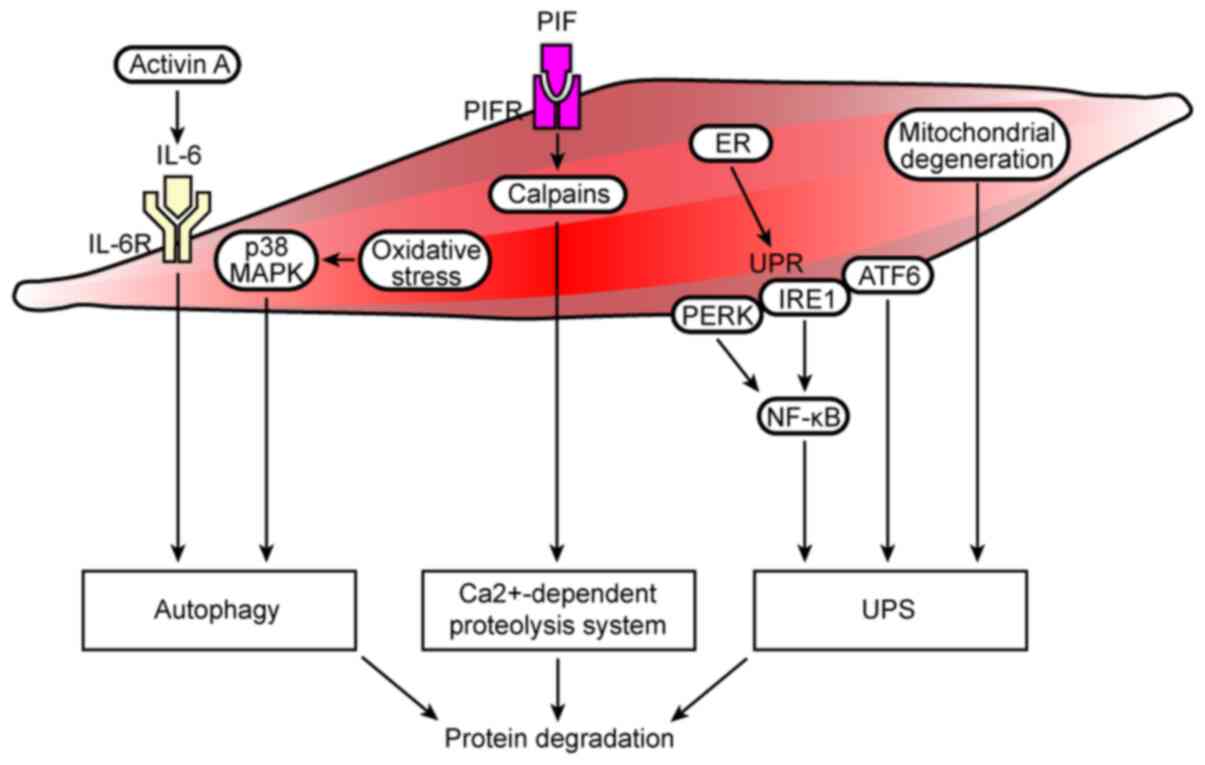
Braun TP, Zhu X, Szumowski M, Scott GD,
Grossberg AJ, Levasseur PR, Graham K, Khan S, Damaraju S, Colmers
WF, et al: Central nervous system inflammation induces muscle
atrophy via activation of the hypothalamic-pituitary-adrenal axis.
J Exp Med. 208:2449–2463. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Judge SM, Wu CL, Beharry AW, Roberts BM,
Ferreira LF, Kandarian SC and Judge AR: Genome-wide identification
of FoxO-dependent gene networks in skeletal muscle during C26
cancer cachexia. BMC Cancer. 14:9972014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Schmitt TL, Martignoni ME, Bachmann J,
Fechtner K, Friess H, Kinscherf R and Hildebrandt W: Activity of
the Akt-dependent anabolic and catabolic pathways in muscle and
liver samples in cancer-related cachexia. J Mol Med (Berl).
85:647–654. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Silva KA, Dong J, Dong Y, Dong Y, Schor N,
Tweardy DJ, Zhang L and Mitch WE: Inhibition of Stat3 activation
suppresses caspase-3 and the ubiquitin-proteasome system, leading
to preservation of muscle mass in cancer cachexia. J Biol Chem.
290:11177–11187. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Murton AJ, Maddocks M, Stephens FB,
Marimuthu K, England R and Wilcock A: Consequences of late-stage
non-small-cell lung cancer cachexia on muscle metabolic processes.
Clin Lung Cancer. 18:e1–e11. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Sugiyama M, Yamaki A, Furuya M, Inomata N,
Minamitake Y, Ohsuye K and Kangawa K: Ghrelin improves body weight
loss and skeletal muscle catabolism associated with angiotensin
II-induced cachexia in mice. Regul Pept. 178:21–28. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Costelli P, Muscaritoli M, Bossola M,
Penna F, Reffo P, Bonetto A, Busquets S, Bonelli G, Lopez-Soriano
FJ, Doglietto GB, et al: IGF-1 is downregulated in experimental
cancer cachexia. Am J Physiol Regul Integr Comp Physiol.
291:R674–683. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Yang J, Zhang Z, Zhang Y, Ni X, Zhang G,
Cui X, Liu M, Xu C, Zhang Q, Zhu H, et al: ZIP4 promotes muscle
wasting and cachexia in mice with orthotopic pancreatic tumors by
stimulating RAB27B-regulated release of extracellular vesicles from
cancer cells. Gastroenterology. 156:722–734.e6. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Pin F, Minero VG, Penna F, Muscaritoli M,
De Tullio R, Baccino FM and Costelli P: Interference with
Ca2+-dependent proteolysis does not alter the course of
muscle wasting in experimental cancer cachexia. Front Physiol.
8:2132017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Camperi A, Pin F, Costamagna D, Penna F,
Menduina ML, Aversa Z, Zimmers T, Verzaro R, Fittipaldi R, Caretti
G, et al: Vitamin D and VDR in cancer cachexia and muscle
regeneration. Oncotarget. 8:21778–21793. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Marzetti E, Lorenzi M, Landi F, Picca A,
Rosa F, Tanganelli F, Galli M, Doglietto GB, Pacelli F, Cesari M,
et al: Altered mitochondrial quality control signaling in muscle of
old gastric cancer patients with cachexia. Exp Gerontol. 87:92–99.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Williams A, Sun X, Fischer JE and
Hasselgren PO: The expression of genes in the ubiquitin-proteasome
proteolytic pathway is increased in skeletal muscle from patients
with cancer. Surgery. 126:744–750. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Doyle A, Zhang G, Abdel Fattah EA, Eissa
NT and Li YP: Toll-like receptor 4 mediates
lipopolysaccharide-induced muscle catabolism via coordinate
activation of ubiquitin-proteasome and autophagy-lysosome pathways.
FASEB J. 25:99–110. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Furuno K and Goldberg AL: The activation
of protein degradation in muscle by Ca2+ or muscle injury does not
involve a lysosomal mechanism. Biochem J. 237:859–864. 1986.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Lecker SH, Solomon V, Mitch WE and
Goldberg AL: Muscle protein breakdown and the critical role of the
ubiquitin-proteasome pathway in normal and disease states. J Nutr.
129 (Suppl 1):S227–S237. 1999. View Article : Google Scholar
|
|
29
|
White JP, Puppa MJ, Gao S, Sato S, Welle
SL and Carson JA: Muscle mTORC1 suppression by IL-6 during cancer
cachexia: A role for AMPK. Am J Physiol Endocrinol Metab.
304:E1042–E1052. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Li YP, Schwartz RJ, Waddell ID, Holloway
BR and Reid MB: Skeletal muscle myocytes undergo protein loss and
reactive oxygen-mediated NF-kappaB activation in response to tumor
necrosis factor alpha. FASEB J. 12:871–880. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Bohnert KR, Gallot YS, Sato S, Xiong G,
Hindi SM and Kumar A: Inhibition of ER stress and unfolding protein
response pathways causes skeletal muscle wasting during cancer
cachexia. FASEB J. 30:3053–3068. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Fontes-Oliveira CC, Busquets S, Toledo M,
Penna F, Paz Aylwin M, Sirisi S, Silva AP, Orpí M, García A, Sette
A, et al: Mitochondrial and sarcoplasmic reticulum abnormalities in
cancer cachexia: Altered energetic efficiency? Biochim Biophys
Acta. 1830:2770–2778. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Mondello P, Mian M, Aloisi C, Fama F,
Mondello S and Pitini V: Cancer cachexia syndrome: Pathogenesis,
diagnosis, and new therapeutic options. Nutr Cancer. 67:12–26.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Hershko A and Ciechanover A: The ubiquitin
system. Annu Rev Biochem. 67:425–479. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Hershko A and Ciechanover A: Mechanisms of
intracellular protein breakdown. Annu Rev Biochem. 51:335–364.
1982. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Haas AL and Rose IA: The mechanism of
ubiquitin activating enzyme. A kinetic and equilibrium analysis. J
Biol Chem. 257:10329–10337. 1982.PubMed/NCBI
|
|
37
|
Hershko A, Heller H, Elias S and
Ciechanover A: Components of ubiquitin-protein ligase system.
Resolution, affinity purification, and role in protein breakdown. J
Biol Chem. 258:8206–8214. 1983.PubMed/NCBI
|
|
38
|
Hershko A: The ubiquitin pathway for
protein degradation. Trends Biochem Sci. 16:265–268. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Reiss Y, Heller H and Hershko A: Binding
sites of ubiquitin-protein ligase. Binding of ubiquitin-protein
conjugates and of ubiquitin-carrier protein. J Biol Chem.
264:10378–10383. 1989.PubMed/NCBI
|
|
40
|
Voges D, Zwickl P and Baumeister W: The
26S proteasome: A molecular machine designed for controlled
proteolysis. Annu Rev Biochem. 68:1015–1068. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Glickman MH and Ciechanover A: The
ubiquitin-proteasome proteolytic pathway: Destruction for the sake
of construction. Physiol Rev. 82:373–428. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Rom O and Reznick AZ: The role of E3
ubiquitin-ligases MuRF-1 and MAFbx in loss of skeletal muscle mass.
Free Radic Biol Med. 98:218–230. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Cai D, Frantz JD, Tawa NE Jr, Melendez PA,
Oh BC, Lidov HG, Hasselgren PO, Frontera WR, Lee J, Glass DJ and
Shoelson SE: IKKbeta/NF-kappaB activation causes severe muscle
wasting in mice. Cell. 119:285–298. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Li W, Moylan JS, Chambers MA, Smith J and
Reid MB: Interleukin-1 stimulates catabolism in C2C12 myotubes. Am
J Physiol Cell Physiol. 297:C706–C714. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
McClung JM, Judge AR, Powers SK and Yan Z:
p38 MAPK links oxidative stress to autophagy-related gene
expression in cachectic muscle wasting. Am J Physiol Cell Physiol.
298:C542–C549. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Kaisari S, Rom O, Aizenbud D and Reznick
AZ: Involvement of NF-κB and muscle specific E3 ubiquitin ligase
MuRF1 in cigarette smoke-induced catabolism in C2 myotubes. Adv Exp
Med Biol. 788:7–17. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Patel HJ and Patel BM: TNF-α and cancer
cachexia: Molecular insights and clinical implications. Life Sci.
170:56–63. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Parajuli P, Kumar S, Loumaye A, Singh P,
Eragamreddy S, Nguyen TL, Ozkan S, Razzaque MS, Prunier C, Thissen
JP and Atfi A: Twist1 activation in muscle progenitor cells causes
muscle loss akin to cancer cachexia. Dev Cell. 45:712–725.e6. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Fry CS, Nayeem SZ, Dillon EL, Sarkar PS,
Tumurbaatar B, Urban RJ, Wright TJ, Sheffield-Moore M, Tilton RG
and Choudhary S: Glucocorticoids increase skeletal muscle NF-κB
inducing kinase (NIK): Links to muscle atrophy. Physiol Rep.
4:2016. View Article : Google Scholar
|
|
50
|
Gallot YS, Durieux AC, Castells J,
Desgeorges MM, Vernus B, Plantureux L, Rémond D, Jahnke VE, Lefai
E, Dardevet D, et al: Myostatin gene inactivation prevents skeletal
muscle wasting in cancer. Cancer Res. 74:7344–7356. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Bédard N, Jammoul S, Moore T, Wykes L,
Hallauer PL, Hastings KE, Stretch C, Baracos V, Chevalier S,
Plourde M, et al: Inactivation of the ubiquitin-specific protease
19 deubiquitinating enzyme protects against muscle wasting. FASEB
J. 29:3889–3898. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Lee H, Lee SJ, Bae GU, Baek NI and Ryu JH:
Canadine from corydalis turtschaninovii stimulates myoblast
differentiation and protects against myotube atrophy. Int J Mol
Sci. 18:27482017. View Article : Google Scholar
|
|
53
|
Chen L, Yang Q, Zhang H, Wan L, Xin B, Cao
Y, Zhang J and Guo C: Cryptotanshinone prevents muscle wasting in
CT26-induced cancer cachexia through inhibiting STAT3 signaling
pathway. J Ethnopharmacol. 260:1130662020. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Chong SW, Nguyet LM, Jiang YJ and Korzh V:
The chemokine Sdf-1 and its receptor Cxcr4 are required for
formation of muscle in zebrafish. BMC Dev Biol. 7:542007.
View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Melchionna R, Di Carlo A, De Mori R,
Cappuzzello C, Barberi L, Musarò A, Cencioni C, Fujii N, Tamamura
H, Crescenzi M, et al: Induction of myogenic differentiation by
SDF-1 via CXCR4 and CXCR7 receptors. Muscle Nerve. 41:828–835.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Bobadilla M, Sainz N, Abizanda G, Orbe J,
Rodriguez JA, Páramo JA, Prósper F and Pérez-Ruiz A: The CXCR4/SDF1
axis improves muscle regeneration through MMP-10 activity. Stem
Cells Dev. 23:1417–1427. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Martinelli GB, Olivari D, Re Cecconi AD,
Talamini L, Ottoboni L, Lecker SH, Stretch C, Baracos VE, Bathe OF,
Resovi A, et al: Activation of the SDF1/CXCR4 pathway retards
muscle atrophy during cancer cachexia. Oncogene. 35:6212–6222.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Winbanks CE, Murphy KT, Bernardo BC, Qian
H, Liu Y, Sepulveda PV, Beyer C, Hagg A, Thomson RE, Chen JL, et
al: Smad7 gene delivery prevents muscle wasting associated with
cancer cachexia in mice. Sci Transl Med. 8:348ra3982016. View Article : Google Scholar
|
|
59
|
Stephens NA, Gallagher IJ, Rooyackers O,
Skipworth RJ, Tan BH, Marstrand T, Ross JA, Guttridge DC, Lundell
L, Fearon KC and Timmons JA: Using transcriptomics to identify and
validate novel biomarkers of human skeletal muscle cancer cachexia.
Genome Med. 2:12010. View
Article : Google Scholar : PubMed/NCBI
|
|
60
|
Eskiler GG, Bezdegumeli E, Ozman Z, Ozkan
AD, Bilir C, Kucukakca BN, Ince MN, Men AY, Aktas O, Horoz YE, et
al: IL-6 mediated JAK/STAT3 signaling pathway in cancer patients
with cachexia. Bratisl Lek Listy. 66:819–826. 2019.PubMed/NCBI
|
|
61
|
Pin F, Barreto R, Kitase Y, Mitra S, Erne
CE, Novinger LJ, Zimmers TA, Couch ME, Bonewald LF and Bonetto A:
Growth of ovarian cancer xenografts causes loss of muscle and bone
mass: A new model for the study of cancer cachexia. J Cachexia
Sarcopenia Muscle. 9:685–700. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Grabiec AM, Korchynskyi O, Tak PP and
Reedquist KA: Histone deacetylase inhibitors suppress rheumatoid
arthritis fibroblast-like synoviocyte and macrophage IL-6
production by accelerating mRNA decay. Ann Rheum Dis. 71:424–431.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Ma F, Li Y, Jia L, Han Y, Cheng J, Li H,
Qi Y and Du J: Macrophage-stimulated cardiac fibroblast production
of IL-6 is essential for TGF β/Smad activation and cardiac fibrosis
induced by angiotensin II. PLoS One. 7:e351442012. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Miki S, Iwano M, Miki Y, Yamamoto M, Tang
B, Yokokawa K, Sonoda T, Hirano T and Kishimoto T: Interleukin-6
(IL-6) functions as an in vitro autocrine growth factor in renal
cell carcinomas. FEBS Lett. 250:607–610. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Iwase S, Murakami T, Saito Y and Nakagawa
K: Steep elevation of blood interleukin-6 (IL-6) associated only
with late stages of cachexia in cancer patients. Eur Cytokine Netw.
15:312–316. 2004.PubMed/NCBI
|
|
66
|
Fujimoto-Ouchi K, Onuma E, Shirane M, Mori
K and Tanaka Y: Capecitabine improves cancer cachexia and
normalizes IL-6 and PTHrP levels in mouse cancer cachexia models.
Cancer Chemother Pharmacol. 59:807–815. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
White JP, Baltgalvis KA, Puppa MJ, Sato S,
Baynes JW and Carson JA: Muscle oxidative capacity during
IL-6-dependent cancer cachexia. Am J Physiol Regul Integr Comp
Physiol. 300:R201–R211. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Op den Kamp CM, Gosker HR, Lagarde S, Tan
DY, Snepvangers FJ, Dingemans AM, Langen RC and Schols AM:
Preserved muscle oxidative metabolic phenotype in newly diagnosed
non-small cell lung cancer cachexia. J Cachexia Sarcopenia Muscle.
6:164–173. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Siddiqui RA and Williams JF: Tentative
identification of the toxohormones of cancer cachexia: Roles of
vasopressin, prostaglandin E2 and cachectin-TNF. Biochem Int.
20:787–797. 1990.PubMed/NCBI
|
|
70
|
Llovera M, García-Martínez C,
López-Soriano J, Carbó N, Agell N, López-Soriano FJ and Argiles JM:
Role of TNF receptor 1 in protein turnover during cancer cachexia
using gene knockout mice. Mol Cell Endocrinol. 142:183–189. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Powrozek T, Mlak R, Brzozowska A, Mazurek
M, Golebiowski P and Malecka-Massalska T: Relationship between
TNF-α −1031T/C gene polymorphism, plasma level of TNF-α, and risk
of cachexia in head and neck cancer patients. J Cancer Res Clin
Oncol. 144:1423–1434. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Llovera M, García-Martínez C, Agell N,
López-Soriano FJ and Argilés JM: TNF can directly induce the
expression of ubiquitin-dependent proteolytic system in rat soleus
muscles. Biochem Biophys Res Commun. 230:238–241. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Matsuyama T, Ishikawa T, Okayama T, Oka K,
Adachi S, Mizushima K, Kimura R, Okajima M, Sakai H, Sakamoto N, et
al: Tumor inoculation site affects the development of cancer
cachexia and muscle wasting. Int J Cancer. 137:2558–2565. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Mu X, Agarwal R, March D, Rothenberg A,
Voigt C, Tebbets J, Huard J and Weiss K: Notch signaling mediates
skeletal muscle atrophy in cancer cachexia caused by osteosarcoma.
Sarcoma. 2016:37581622016. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Cannon T, Shores C, Yin X, Dahlman J,
Guttridge D, Lai V, George J, Buzkova P and Couch M:
Immunocompetent murine model of cancer cachexia for head and neck
squamous cell carcinoma. Head Neck. 30:320–326. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Mi L, Lin J, Zheng H, Xu X, Zhang J and
Zhang D: Bacterial translocation contributes to cachexia from
locally advanced gastric cancer. Hepatogastroenterology.
59:2348–2351. 2012.PubMed/NCBI
|
|
77
|
Kumar S, Kishimoto H, Chua HL, Badve S,
Miller KD, Bigsby RM and Nakshatri H: Interleukin-1 alpha promotes
tumor growth and cachexia in MCF-7 ×enograft model of breast
cancer. Am J Pathol. 163:2531–2541. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Zheng R, Huang S, Zhu J, Lin W, Xu H and
Zheng X: Leucine attenuates muscle atrophy and autophagosome
formation by activating PI3K/AKT/mTOR signaling pathway in rotator
cuff tears. Cell Tissue Res. 378:113–125. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Lee S, Kim MB, Kim C and Hwang JK: Whole
grain cereal attenuates obesity-induced muscle atrophy by
activating the PI3K/Akt pathway in obese C57BL/6N mice. Food Sci
Biotechnol. 27:159–168. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Ma XM and Blenis J: Molecular mechanisms
of mTOR-mediated translational control. Nat Rev Mol Cell Biol.
10:307–318. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Jiang BH, Aoki M, Zheng JZ, Li J and Vogt
PK: Myogenic signaling of phosphatidylinositol 3-kinase requires
the serine-threonine kinase Akt/protein kinase B. Proc Natl Acad
Sci USA. 96:2077–2081. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Price DJ, Grove JR, Calvo V, Avruch J and
Bierer BE: Rapamycin-induced inhibition of the 70-kilodalton S6
protein kinase. Science. 257:973–977. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Chung J, Kuo CJ, Crabtree GR and Blenis J:
Rapamycin-FKBP specifically blocks growth-dependent activation of
and signaling by the 70 kd S6 protein kinases. Cell. 69:1227–1236.
1992. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Lin TA, Kong X, Saltiel AR, Blackshear PJ
and Lawrence JC Jr: Control of PHAS-I by insulin in 3T3-L1
adipocytes. Synthesis, degradation, and phosphorylation by a
rapamycin-sensitive and mitogen-activated protein
kinase-independent pathway. J Biol Chem. 270:18531–18538. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Graves LM, Bornfeldt KE, Argast GM, Krebs
EG, Kong X, Lin TA and Lawrence JC Jr: cAMP- and
rapamycin-sensitive regulation of the association of eukaryotic
initiation factor 4E and the translational regulator PHAS-I in
aortic smooth muscle cells. Proc Natl Acad Sci USA. 92:7222–7226.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Stitt TN, Drujan D, Clarke BA, Panaro F,
Timofeyva Y, Kline WO, Gonzalez M, Yancopoulos GD and Glass D: The
IGF-1/PI3K/Akt pathway prevents expression of muscle
atrophy-induced ubiquitin ligases by inhibiting FOXO transcription
factors. Mol Cell. 14:395–403. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Sandri M, Sandri C, Gilbert A, Skurk C,
Calabria E, Picard A, Walsh K, Schiaffino S, Lecker SH and Goldberg
AL: Foxo transcription factors induce the atrophy-related ubiquitin
ligase atrogin-1 and cause skeletal muscle atrophy. Cell.
117:399–412. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Manne ND, Lima M, Enos RT, Wehner P,
Carson JA and Blough E: Altered cardiac muscle mTOR regulation
during the progression of cancer cachexia in the ApcMin/+ mouse.
Int J Oncol. 42:2134–2140. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Ge Y, Wu AL, Warnes C, Liu J, Zhang C,
Kawasome H, Terada N, Boppart MD, Schoenherr CJ and Chen J: mTOR
regulates skeletal muscle regeneration in vivo through
kinase-dependent and kinase-independent mechanisms. Am J Physiol
Cell Physiol. 297:C1434–C1444. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Zimmers TA, Fishel ML and Bonetto A: STAT3
in the systemic inflammation of cancer cachexia. Semin Cell Dev
Biol. 54:28–41. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Bonetto A, Aydogdu T, Kunzevitzky N,
Guttridge DC, Khuri S, Koniaris LG and Zimmers TA: STAT3 activation
in skeletal muscle links muscle wasting and the acute phase
response in cancer cachexia. PLoS One. 6:e225382011. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Ma JF, Sanchez BJ, Hall DT, Tremblay AK,
Di Marco S and Gallouzi IE: STAT3 promotes IFNγ/TNFα-induced muscle
wasting in an NF-κB-dependent and IL-6-independent manner. EMBO Mol
Med. 9:622–637. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Ghosh S and Karin M: Missing pieces in the
NF-kappaB puzzle. Cell. 109 (Suppl 1):S81–S96. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Hayden MS and Ghosh S: NF-kappaB in
immunobiology. Cell Res. 21:223–244. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Thoma A and Lightfoot AP: NF-kB and
inflammatory cytokine signalling: Role in skeletal muscle atrophy.
Adv Exp Med Biol. 1088:267–279. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Di Marco S, Mazroui R, Dallaire P, Chittur
S, Tenenbaum SA, Radzioch D, Marette A and Gallouzi IE: NF-kappa
B-mediated MyoD decay during muscle wasting requires nitric oxide
synthase mRNA stabilization, HuR protein, and nitric oxide release.
Mol Cell Biol. 25:6533–6545. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Cuenda A and Rousseau S: p38 MAP-kinases
pathway regulation, function and role in human diseases. Biochim
Biophys Acta. 1773:1358–1375. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Kim J, Won KJ, Lee HM, Hwang BY, Bae YM,
Choi WS, Song H, Lim KW, Lee CK and Kim B: p38 MAPK participates in
muscle-specific RING finger 1-mediated atrophy in cast-immobilized
rat gastrocnemius muscle. Korean J Physiol Pharmacol. 13:491–496.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Ryu Y, Lee D, Jung SH, Lee KJ, Jin H, Kim
SJ, Lee HM, Kim B and Won KJ: Sabinene prevents skeletal muscle
atrophy by inhibiting the MAPK-MuRF-1 pathway in rats. Int J Mol
Sci. 20:49552019. View Article : Google Scholar
|
|
100
|
Belova SP, Mochalova EP, Kostrominova TY,
Shenkman BS and Nemirovskaya TL: P38α-MAPK signaling inhibition
attenuates soleus atrophy during early stages of muscle unloading.
Int J Mol Sci. 21:27562020. View Article : Google Scholar
|
|
101
|
Girven M, Dugdale HF, Owens DJ, Hughes DC,
Stewart CE and Sharples AP: l-glutamine improves skeletal muscle
cell differentiation and prevents myotube atrophy after cytokine
(TNF-α) stress via reduced p38 MAPK signal transduction. J Cell
Physiol. 231:2720–2732. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Morales MG, Olguin H, Di Capua G, Brandan
E, Simon F and Cabello-Verrugio C: Endotoxin-induced skeletal
muscle wasting is prevented by angiotensin-(1–7) through a p38
MAPK-dependent mechanism. Clin Sci (Lond). 129:461–476. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
103
|
O'Neill BT, Bhardwaj G, Penniman CM,
Krumpoch MT, Suarez Beltran PA, Klaus K, Poro K, Li M, Pan H,
Dreyfuss JM, et al: FoxO transcription factors are critical
regulators of diabetes-related muscle atrophy. Diabetes.
68:556–570. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Liu CM, Yang Z, Liu CW, Wang R, Tien P,
Dale R and Sun LQ: Effect of RNA oligonucleotide targeting Foxo-1
on muscle growth in normal and cancer cachexia mice. Cancer Gene
Ther. 14:945–952. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Blackwell TA, Cervenka I, Khatri B, Brown
JL, Rosa-Caldwell ME, Lee DE, Perry RA Jr, Brown LA, Haynie WS,
Wiggs MP, et al: Transcriptomic analysis of the development of
skeletal muscle atrophy in cancer-cachexia in tumor-bearing mice.
Physiol Genomics. 50:1071–1082. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Marchildon F, Lamarche E, Lala-Tabbert N,
St-Louis C and Wiper-Bergeron N: Expression of CCAAT/enhancer
binding protein beta in muscle satellite cells inhibits myogenesis
in cancer cachexia. PLoS One. 10:e01455832015. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Freire PP, Fernandez GJ, Cury SS, de
Moraes D, Oliveira JS, de Oliveira G, Dal-Pai-Silva M, Dos Reis PP
and Carvalho RF: The pathway to cancer cachexia: MicroRNA-regulated
networks in muscle wasting based on integrative meta-analysis. Int
J Mol Sci. 20:2019. View Article : Google Scholar
|
|
108
|
Lee DE, Brown JL, Rosa-Caldwell ME,
Blackwell TA, Perry RA Jr, Brown LA, Khatri B, Seo D, Bottje WG,
Washington TA, et al: Cancer cachexia-induced muscle atrophy:
Evidence for alterations in microRNAs important for muscle size.
Physiol Genomics. 49:253–260. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Sandri M: Autophagy in health and disease.
3. Involvement of autophagy in muscle atrophy. Am J Physiol Cell
Physiol. 298:C1291–C1297. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Bargiela A, Cerro-Herreros E,
Fernandez-Costa JM, Vilchez JJ, Llamusi B and Artero R: Increased
autophagy and apoptosis contribute to muscle atrophy in a myotonic
dystrophy type 1 Drosophila model. Dis Model Mech. 8:679–690. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Pettersen K, Andersen S, Degen S, Tadini
V, Grosjean J, Hatakeyama S, Tesfahun AN, Moestue S, Kim J, Nonstad
U, et al: Cancer cachexia associates with a systemic
autophagy-inducing activity mimicked by cancer cell-derived IL-6
trans-signaling. Sci Rep. 7:20462017. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Penna F, Ballarò R, Martinez-Cristobal P,
Sala D, Sebastian D, Busquets S, Muscaritoli M, Argilés JM,
Costelli P and Zorzano A: Autophagy exacerbates muscle wasting in
cancer cachexia and impairs mitochondrial function. J Mol Biol.
431:2674–2686. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Pettersen K, Andersen S, van der Veen A,
Nonstad U, Hatakeyama S, Lambert C, Lach-Trifilieff E, Moestue S,
Kim J, Grønberg BH, et al: Autocrine activin A signalling in
ovarian cancer cells regulates secretion of interleukin 6,
autophagy, and cachexia. J Cachexia Sarcopenia Muscle. 11:195–207.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Mirza KA and Tisdale MJ: Role of
Ca2+ in proteolysis-inducing factor (PIF)-induced
atrophy of skeletal muscle. Cell Signal. 24:2118–2122. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Kozutsumi Y, Segal M, Normington K,
Gething MJ and Sambrook J: The presence of malfolded proteins in
the endoplasmic reticulum signals the induction of
glucose-regulated proteins. Nature. 332:462–464. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Bohnert KR, McMillan JD and Kumar A:
Emerging roles of ER stress and unfolded protein response pathways
in skeletal muscle health and disease. J Cell Physiol. 233:67–78.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Liu CY, Schröder M and Kaufman RJ:
Ligand-independent dimerization activates the stress response
kinases IRE1 and PERK in the lumen of the endoplasmic reticulum. J
Biol Chem. 275:24881–24885. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Bertolotti A, Zhang Y, Hendershot LM,
Harding HP and Ron D: Dynamic interaction of BiP and ER stress
transducers in the unfolded-protein response. Nat Cell Biol.
2:326–332. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Yoshida H, Matsui T, Yamamoto A, Okada T
and Mori K: XBP1 mRNA is induced by ATF6 and spliced by IRE1 in
response to ER stress to produce a highly active transcription
factor. Cell. 107:881–891. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Shen J, Chen X, Hendershot L and Prywes R:
ER stress regulation of ATF6 localization by dissociation of
BiP/GRP78 binding and unmasking of Golgi localization signals. Dev
Cell. 3:99–111. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Roy A and Kumar A: ER stress and unfolded
protein response in cancer cachexia. Cancers (Basel). 11:19292019.
View Article : Google Scholar
|
|
122
|
Wu J and Kaufman RJ: From acute ER stress
to physiological roles of the Unfolded Protein Response. Cell Death
Differ. 13:374–384. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Isaac ST, Tan TC and Polly P: Endoplasmic
reticulum stress, calcium dysregulation and altered protein
translation: Intersection of processes that contribute to cancer
cachexia induced skeletal muscle wasting. Curr Drug Targets.
17:1140–1146. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Barreiro E, Salazar-Degracia A,
Sancho-Muñoz A and Gea J: Endoplasmic reticulum stress and unfolded
protein response profile in quadriceps of sarcopenic patients with
respiratory diseases. J Cell Physiol. 234:11315–11329. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Tam AB, Mercado EL, Hoffmann A and Niwa M:
ER stress activates NF-κB by integrating functions of basal IKK
activity, IRE1 and PERK. PLoS One. 7:e450782012. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
White JP, Puppa MJ, Sato S, Gao S, Price
RL, Baynes JW, Kostek MC, Matesic LE and Carson JA: IL-6 regulation
on skeletal muscle mitochondrial remodeling during cancer cachexia
in the ApcMin/+ mouse. Skelet Muscle. 2:142012. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Brown JL, Rosa-Caldwell ME, Lee DE,
Blackwell TA, Brown LA, Perry RA, Haynie WS, Hardee JP, Carson JA,
Wiggs MP, et al: Mitochondrial degeneration precedes the
development of muscle atrophy in progression of cancer cachexia in
tumour-bearing mice. J Cachexia Sarcopenia Muscle. 8:926–938. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
128
|
VanderVeen BN, Fix DK and Carson JA:
Disrupted skeletal muscle mitochondrial dynamics, mitophagy, and
biogenesis during cancer cachexia: A role for inflammation. Oxid
Med Cell Longev. 2017:32920872017. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
van der Ende M, Grefte S, Plas R,
Meijerink J, Witkamp RF, Keijer J and van Norren K: Mitochondrial
dynamics in cancer-induced cachexia. Biochim Biophys Acta Rev
Cancer. 1870:137–150. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Dave DT and Patel BM: Mitochondrial
metabolism in cancer cachexia: Novel drug target. Curr Drug Metab.
20:1141–1153. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Neyroud D, Nosacka RL, Judge AR and Hepple
RT: Colon 26 adenocarcinoma (C26)-induced cancer cachexia impairs
skeletal muscle mitochondrial function and content. J Muscle Res
Cell Motil. 40:59–65. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Pin F, Novinger LJ, Huot JR, Harris RA,
Couch ME, O'Connell TM and Bonetto A: PDK4 drives metabolic
alterations and muscle atrophy in cancer cachexia. FASEB J.
33:7778–7790. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Du Bois P, Pablo Tortola C, Lodka D, Kny
M, Schmidt F, Song K, Schmidt S, Bassel-Duby R, Olson EN and
Fielitz J: Angiotensin II induces skeletal muscle atrophy by
activating TFEB-mediated MuRF1 expression. Circ Res. 117:424–436.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Kadoguchi T, Kinugawa S, Takada S,
Fukushima A, Furihata T, Homma T, Masaki Y, Mizushima W, Nishikawa
M, Takahashi M, et al: Angiotensin II can directly induce
mitochondrial dysfunction, decrease oxidative fibre number and
induce atrophy in mouse hindlimb skeletal muscle. Exp Physiol.
100:312–322. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Cisternas F, Morales MG, Meneses C, Simon
F, Brandan E, Abrigo J, Vazquez Y and Cabello-Verrugio C:
Angiotensin-(1–7) decreases skeletal muscle atrophy induced by
angiotensin II through a Mas receptor-dependent mechanism. Clin Sci
(Lond). 128:307–319. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Yoshida T, Tabony AM, Galvez S, Mitch WE,
Higashi Y, Sukhanov S and Delafontaine P: Molecular mechanisms and
signaling pathways of angiotensin II-induced muscle wasting:
Potential therapeutic targets for cardiac cachexia. Int J Biochem
Cell Biol. 45:2322–2332. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Penafuerte CA, Gagnon B, Sirois J, Murphy
J, MacDonald N and Tremblay ML: Identification of
neutrophil-derived proteases and angiotensin II as biomarkers of
cancer cachexia. Br J Cancer. 114:680–687. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Cai X, Zhu C, Xu Y, Jing Y, Yuan Y, Wang
L, Wang S, Zhu X, Gao P, Zhang Y, et al: Alpha-ketoglutarate
promotes skeletal muscle hypertrophy and protein synthesis through
Akt/mTOR signaling pathways. Sci Rep. 6:268022016. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Liu D, Qiao X, Ge Z, Shang Y, Li Y, Wang
W, Chen M, Si S and Chen SZ: IMB0901 inhibits muscle atrophy
induced by cancer cachexia through MSTN signaling pathway. Skelet
Muscle. 9:82019. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Bae T, Jang J, Lee H, Song J, Chae S, Park
M, Son CG, Yoon S and Yoon Y: Paeonia lactiflora root extract
suppresses cancer cachexia by down-regulating muscular NF-κB
signalling and muscle-specific E3 ubiquitin ligases in
cancer-bearing mice. J Ethnopharmacol. 246:1122222020. View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Levolger S, Wiemer EAC, van Vugt JLA,
Huisman SA, van Vledder MG, van Damme-van Engel S, Ambagtsheer G,
IJzermans JNM and de Bruin RWF: Inhibition of activin-like kinase
4/5 attenuates cancer cachexia associated muscle wasting. Sci Rep.
9:98262019. View Article : Google Scholar : PubMed/NCBI
|
|
142
|
An JM, Kang EA, Han YM, Oh JY, Lee DY,
Choi SH, Kim DH and Hahm KB: Dietary intake of probiotic kimchi
ameliorated IL-6-driven cancer cachexia. J Clin Biochem Nutr.
65:109–117. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Liu H, Li L, Zou J, Zhou T, Wang B, Sun H
and Yu S: Coix seed oil ameliorates cancer cachexia by
counteracting muscle loss and fat lipolysis. BMC Complement Altern
Med. 19:2672019. View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Terawaki K, Sawada Y, Kashiwase Y,
Hashimoto H, Yoshimura M, Suzuki M, Miyano K, Sudo Y, Shiraishi S,
Higami Y, et al: New cancer cachexia rat model generated by
implantation of a peritoneal dissemination-derived human stomach
cancer cell line. Am J Physiol Endocrinol Metab. 306:E373–E387.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Xi QL, Zhang B, Jiang Y, Zhang HS, Meng
QY, Chen Y, Han YS, Zhuang QL, Han J, Wang HY, et al: Mitofusin-2
prevents skeletal muscle wasting in cancer cachexia. Oncol Lett.
12:4013–4020. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
146
|
Toledo M, Busquets S, Penna F, Zhou X,
Marmonti E, Betancourt A, Massa D, López-Soriano FJ, Han HQ and
Argilés JM: Complete reversal of muscle wasting in experimental
cancer cachexia: Additive effects of activin type II receptor
inhibition and beta-2 agonist. Int J Cancer. 138:2021–2029. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
147
|
Khamoui AV, Park BS, Kim DH, Yeh MC, Oh
SL, Elam ML, Jo E, Arjmandi BH, Salazar G, Grant SC, et al: Aerobic
and resistance training dependent skeletal muscle plasticity in the
colon-26 murine model of cancer cachexia. Metabolism. 65:685–698.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
148
|
Tanaka M, Sugimoto K, Fujimoto T, Xie K,
Takahashi T, Akasaka H, Kurinami H, Yasunobe Y, Matsumoto T, Fujino
H and Rakugi H: Preventive effects of low-intensity exercise on
cancer cachexia-induced muscle atrophy. FASEB J. 33:7852–7862.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
149
|
Zhang Y, Han X, Ouyang B, Wu Z, Yu H, Wang
Y, Liu G and Ji X: Chinese herbal medicine Baoyuan Jiedu decoction
inhibited muscle atrophy of cancer cachexia through Atrogin-l and
MuRF-1. Evid Based Complement Alternat Med.
2017:62683782017.PubMed/NCBI
|
|
150
|
Sun R, Zhang S, Hu W, Lu X, Lou N, Yang Z,
Chen S, Zhang X and Yang H: Valproic acid attenuates skeletal
muscle wasting by inhibiting C/EBPbeta-regulated atrogin1
expression in cancer cachexia. Am J Physiol Cell Physiol.
311:C101–C115. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
151
|
Zhuang P, Zhang J, Wang Y, Zhang M, Song
L, Lu Z, Zhang L, Zhang F, Wang J, Zhang Y, et al: Reversal of
muscle atrophy by Zhimu and Huangbai herb pair via activation of
IGF-1/Akt and autophagy signal in cancer cachexia. Support Care
Cancer. 24:1189–1198. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
152
|
Chen JM, Yang TT, Cheng TS, Hsiao TF,
Chang PM, Leu JY, Wang FS, Hsu SL, Huang CF and Lai JM: Modified
Sijunzi decoction can alleviate cisplatin-induced toxicity and
prolong the survival time of cachectic mice by recovering muscle
atrophy. J Ethnopharmacol. 233:47–55. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
153
|
Molanouri Shamsi M, Chekachak S, Soudi S,
Quinn LS, Ranjbar K, Chenari J, Yazdi MH and Mahdavi M: Combined
effect of aerobic interval training and selenium nanoparticles on
expression of IL-15 and IL-10/TNF-α ratio in skeletal muscle of 4T1
breast cancer mice with cachexia. Cytokine. 90:100–108. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
154
|
Salazar-Degracia A, Busquets S, Argilés
JM, Bargalló-Gispert N, López-Soriano FJ and Barreiro E: Effects of
the beta2 agonist formoterol on atrophy signaling, autophagy, and
muscle phenotype in respiratory and limb muscles of rats with
cancer-induced cachexia. Biochimie. 149:79–91. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
155
|
Pretto F, Ghilardi C, Moschetta M, Bassi
A, Rovida A, Scarlato V, Talamini L, Fiordaliso F, Bisighini C,
Damia G, et al: Sunitinib prevents cachexia and prolongs survival
of mice bearing renal cancer by restraining STAT3 and MuRF-1
activation in muscle. Oncotarget. 6:3043–3054. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
156
|
Miao C, Lv Y, Zhang W, Chai X, Feng L,
Fang Y, Liu X and Zhang X: Pyrrolidine dithiocarbamate (PDTC)
attenuates cancer cachexia by affecting muscle atrophy and fat
lipolysis. Front Pharmacol. 8:9152017. View Article : Google Scholar : PubMed/NCBI
|
|
157
|
Kadoguchi T, Takada S, Yokota T, Furihata
T, Matsumoto J, Tsuda M, Mizushima W, Fukushima A, Okita K and
Kinugawa S: Deletion of NAD(P)H oxidase 2 prevents angiotensin
II-induced skeletal muscle atrophy. Biomed Res Int.
2018:31949172018. View Article : Google Scholar : PubMed/NCBI
|
|
158
|
Bosaeus I: Nutritional support in
multimodal therapy for cancer cachexia. Support Care Cancer.
16:447–451. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
159
|
Amano K, Morita T, Miyamoto J, Uno T,
Katayama H and Tatara R: Perception of need for nutritional support
in advanced cancer patients with cachexia: A survey in palliative
care settings. Support Care Cancer. 26:2793–2799. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
160
|
McClement S: Cancer anorexia-cachexia
syndrome: Psychological effect on the patient and family. J Wound
Ostomy Continence Nurs. 32:264–268. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
161
|
Zhang WL, Li N, Shen Q, Fan M, Guo XD,
Zhang XW, Zhang Z and Liu X: Establishment of a mouse model of
cancer cachexia with spleen deficiency syndrome and the effects of
atractylenolide I. Acta Pharmacol Sin. 41:237–248. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
162
|
Kang HJ, Jeong MK, Park SJ, Jun HJ and Yoo
HS: Efficacy and safety of Yukgunja-Tang for treating anorexia in
patients with cancer: The protocol for a pilot, randomized,
controlled trial. Medicine (Baltimore). 98:e169502019. View Article : Google Scholar : PubMed/NCBI
|