|
1
|
Hammond N, Kumar A, Kaur P, Tirupakuzhi
Vijayaraghavan BK, Ghosh A, Grattan S, Jha V, Mathai D and
Venkatesh B; Sepsis in India Prevalence Study (SIPS) Investigator
Network, : Estimates of sepsis prevalence and outcomes in adult
patients in the ICU in India: A cross-sectional Study. Chest.
161:1543–1554. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Salomão R, Ferreira BL, Salomão MC, Santos
SS, Azevedo LCP and Brunialti MKC: Sepsis: Evolving concepts and
challenges. Braz J Med Biol Res. 52:e85952019. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Shankar-Hari M, Phillips G, Levy ML,
Seymour CW, Liu VX, Deutschman CS, Angus DC, Rubenfeld GD and
Singer M; Sepsis Definitions Task Force, : Developing a new
definition and assessing new clinical criteria for septic shock:
For the third international consensus definitions for sepsis and
septic shock (sepsis-3). JAMA. 315:775–787. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bone RC, Balk RA, Cerra FB, Dellinger RP,
Fein AM, Knaus WA, Schein RM and Sibbald WJ: Definitions for sepsis
and organ failure and guidelines for the use of innovative
therapies in sepsis. The ACCP/SCCM consensus conference committee.
American college of chest physicians/society of critical care
medicine. Chest. 101:1644–1655. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Makic MBF and Bridges E: CE: Managing
sepsis and septic shock: Current guidelines and definitions. Am J
Nurs. 118:34–39. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Delano MJ and Ward PA: The immune system's
role in sepsis progression, resolution, and long-term outcome.
Immunol Rev. 274:330–353. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Antonucci E, Fiaccadori E, Donadello K,
Taccone FS, Franchi F and Scolletta S: Myocardial depression in
sepsis: From pathogenesis to clinical manifestations and treatment.
J Crit Care. 29:500–511. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Rello J, Valenzuela-Sánchez F,
Ruiz-Rodriguez M and Moyano S: Sepsis: A review of advances in
management. Adv Ther. 34:2393–2411. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Skirecki T and Cavaillon JM: Inner sensors
of endotoxin-implications for sepsis research and therapy. FEMS
Microbiol Rev. 43:239–256. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Torres L, Pickkers P and van der Poll T:
Sepsis-induced immunosuppression. Annu Rev Physiol. 84:157–181.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ehrman RR, Sullivan AN, Favot MJ, Sherwin
RL, Reynolds CA, Abidov A and Levy PD: Pathophysiology,
echocardiographic evaluation, biomarker findings, and prognostic
implications of septic cardiomyopathy: A review of the literature.
Crit Care. 22:1122018. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Purcarea A and Sovaila S: Sepsis, a 2020
review for the internist. Rom J Intern Med. 58:129–137.
2020.PubMed/NCBI
|
|
13
|
Gotts JE and Matthay MA: Sepsis:
Pathophysiology and clinical management. BMJ. 353:i15852016.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Huang M, Cai S and Su J: The pathogenesis
of sepsis and potential therapeutic targets. Int J Mol Sci.
20:53762019. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ackerman MH, Ahrens T, Kelly J and
Pontillo A: Sepsis. Crit Care Nurs Clin North Am. 33:407–418. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
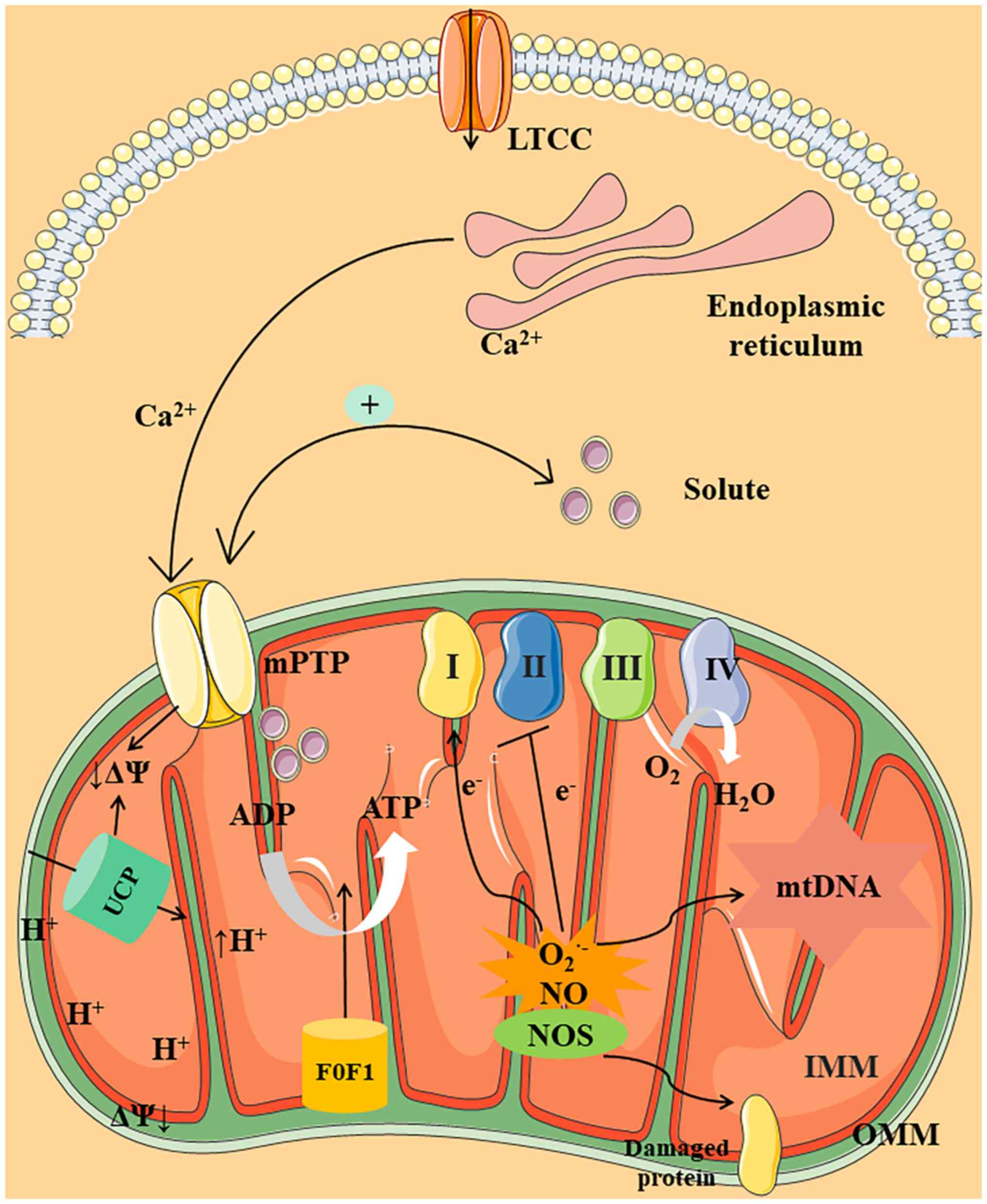
Zhang H, Feng YW and Yao YM: Potential
therapy strategy: Targeting mitochondrial dysfunction in sepsis.
Mil Med Res. 5:412018.PubMed/NCBI
|
|
17
|
Cheung R, Pizza G, Chabosseau P, Rolando
D, Tomas A, Burgoyne T, Wu Z, Salowka A, Thapa A, Macklin A, et al:
Glucose-dependent miR-125b is a negative regulator of β-cell
function. Diabetes. 71:1525–1545. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Doke T and Susztak K: The multifaceted
role of kidney tubule mitochondrial dysfunction in kidney disease
development. Trends Cell Biol. 32:841–853. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Park K and Lee MS: Essential role of
lysosomal Ca2+-mediated TFEB activation in mitophagy and functional
adaptation of pancreatic β-cells to metabolic stress. Autophagy.
18:3043–3045. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Eldeeb MA, Thomas RA, Ragheb MA, Fallahi A
and Fon EA: Mitochondrial quality control in health and in
Parkinson's disease. Physiol Rev. 102:1721–1755. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hocaoglu H and Sieber M: Mitochondrial
respiratory quiescence: A new model for examining the role of
mitochondrial metabolism in development. Semin Cell Dev Biol.
138:94–103. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Subramanian GN, Yeo AJ, Gatei MH, Coman DJ
and Lavin MF: Metabolic stress and mitochondrial dysfunction in
ataxia-telangiectasia. Antioxidants (Basel). 11:6532022. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Joffre J and Hellman J: Oxidative stress
and endothelial dysfunction in sepsis and acute inflammation.
Antioxid Redox Signal. 35:1291–1307. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Doi K, Leelahavanichkul A, Yuen PST and
Star RA: Animal models of sepsis and sepsis-induced kidney injury.
J Clin Invest. 119:2868–2878. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Salari S, Ghorbanpour A, Marefati N,
Baluchnejadmojarad T and Roghani M: Therapeutic effect of lycopene
in lipopolysaccharide nephrotoxicity through alleviation of
mitochondrial dysfunction, inflammation, and oxidative stress. Mol
Biol Rep. 49:8429–8438. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
de Souza Stork S, Hübner M, Biehl E,
Danielski LG, Bonfante S, Joaquim L, Denicol T, Cidreira T, Pacheco
A, Bagio E, et al: Diabetes exacerbates sepsis-induced
neuroinflammation and brain mitochondrial dysfunction.
Inflammation. 45:2352–2367. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Soriano FG, Nogueira AC, Caldini EG, Lins
MH, Teixeira AC, Cappi SB, Lotufo PA, Bernik MM, Zsengellér Z, Chen
M and Szabó C: Potential role of poly(adenosine
5′-diphosphate-ribose) polymerase activation in the pathogenesis of
myocardial contractile dysfunction associated with human septic
shock. Crit Care Med. 34:1073–1079. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Galley HF: Oxidative stress and
mitochondrial dysfunction in sepsis. Br J Anaesth. 107:57–64. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Cimolai MC, Alvarez S, Bode C and Bugger
H: Mitochondrial mechanisms in septic cardiomyopathy. Int J Mol
Sci. 16:17763–17778. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Lee S, Xu H, Van Vleck A, Mawla AM, Li AM,
Ye J, Huising MO and Annes JP: β-Cell succinate dehydrogenase
deficiency triggers metabolic dysfunction and insulinopenic
diabetes. Diabetes. 71:1439–1453. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Hu J, Cheng Y, Chen P, Huang Z and Yang L:
Caffeine citrate protects against sepsis-associated encephalopathy
and inhibits the UCP2/NLRP3 axis in astrocytes. J Interferon
Cytokine Res. 42:267–278. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Huang Q, Ding Y, Fang C, Wang H and Kong
L: The emerging role of ferroptosis in sepsis, opportunity or
challenge? Infect Drug Resist. 16:5551–5562. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Ji L, He Q, Liu Y, Deng Y, Xie M, Luo K,
Cai X, Zuo Y, Wu W, Li Q, et al: Ketone body β-hydroxybutyrate
prevents myocardial oxidative stress in septic cardiomyopathy. Oxid
Med Cell Longev. 2022:25138372022. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Zhao H, Lin X, Chen Q, Wang X, Wu Y and
Zhao X: Quercetin inhibits the NOX2/ROS-mediated NF-κB/TXNIP
signaling pathway to ameliorate pyroptosis of cardiomyocytes to
relieve sepsis-induced cardiomyopathy. Toxicol Appl Pharmacol.
477:1166722023. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Liu Z, Pan H, Zhang Y, Zheng Z, Xiao W,
Hong X, Chen F, Peng X, Pei Y, Rong J, et al: Ginsenoside-Rg1
attenuates sepsis-induced cardiac dysfunction by modulating
mitochondrial damage via the P2X7 receptor-mediated Akt/GSK-3β
signaling pathway. J Biochem Mol Toxicol. 36:e228852022. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Wang J, Yang S, Jing G, Wang Q, Zeng C,
Song X and Li X: Inhibition of ferroptosis protects
sepsis-associated encephalopathy. Cytokine. 161:1560782023.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Vanasco V, Saez T, Magnani ND, Pereyra L,
Marchini T, Corach A, Vaccaro MI, Corach D, Evelson P and Alvarez
S: Cardiac mitochondrial biogenesis in endotoxemia is not
accompanied by mitochondrial function recovery. Free Radic Biol
Med. 77:1–9. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Burgoyne J, Rudyk O, Mayr M and Eaton P:
Nitrosative protein oxidation is modulated during early
endotoxemia. Nitric Oxide. 25:118–124. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Boveris A, Alvarez S and Navarro A: The
role of mitochondrial nitric oxide synthase in inflammation and
septic shock. Free Radic Biol Med. 33:1186–1193. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Escames G, López L, Ortiz F, López A,
García JA, Ros E and Acuña-Castroviejo D: Attenuation of cardiac
mitochondrial dysfunction by melatonin in septic mice. FEBS J.
274:2135–2147. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
van de Sandt AM, Windler R, Gödecke A,
Ohlig J, Zander S, Reinartz M, Graf J, van Faassen EE, Rassaf T,
Schrader J, et al: Endothelial NOS (NOS3) impairs myocardial
function in developing sepsis. Basic Res Cardiol. 108:3302013.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
McCall CE, Zhu X, Zabalawi M, Long D,
Quinn MA, Yoza BK, Stacpoole PW and Vachharajani V: Sepsis,
pyruvate, and mitochondria energy supply chain shortage. J Leukoc
Biol. 112:1509–1514. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Joshi MS, Julian MW, Huff JE, Bauer JA,
Xia Y and Crouser ED: Calcineurin regulates myocardial function
during acute endotoxemia. Am J Respir Crit Care Med. 173:999–1007.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Giorgio V, von Stockum S, Antoniel M,
Fabbro A, Fogolari F, Forte M, Glick GD, Petronilli V, Zoratti M,
Szabó I, et al: Dimers of mitochondrial ATP synthase form the
permeability transition pore. Proc Natl Acad Sci USA.
110:5887–5892. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Giorgio V, Guo L, Bassot C, Petronilli V
and Bernardi P: Calcium and regulation of the mitochondrial
permeability transition. Cell Calcium. 70:56–63. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Bernardi P: The mitochondrial permeability
transition pore: A mystery solved? Front Physiol. 4:952013.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Rasola A and Bernardi P: Mitochondrial
permeability transition in Ca(2+)-dependent apoptosis and necrosis.
Cell Calcium. 50:222–233. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Takeuchi A, Kim B and Matsuoka S: The
destiny of Ca(2+) released by mitochondria. J Physiol Sci.
65:11–24. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Halestrap AP: Calcium, mitochondria and
reperfusion injury: A pore way to die. Biochem Soc Trans.
34:232–237. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Bernardi P and Di Lisa F: The
mitochondrial permeability transition pore: Molecular nature and
role as a target in cardioprotection. J Mol Cell Cardiol.
78:100–106. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Ballard-Croft C, Maass DL, Sikes PJ and
Horton JW: Sepsis and burn complicated by sepsis alter cardiac
transporter expression. Burns. 33:72–80. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Hassoun SM, Marechal X, Montaigne D,
Bouazza Y, Decoster B, Lancel S and Neviere R: Prevention of
endotoxin-induced sarcoplasmic reticulum calcium leak improves
mitochondrial and myocardial dysfunction. Crit Care Med.
36:2590–2596. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Supinski GS, Murphy MP and Callahan LA:
MitoQ administration prevents endotoxin-induced cardiac
dysfunction. Am J Physiol Regul Integr Comp Physiol.
297:R1095–R1102. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Zang QS, Sadek H, Maass DL, Martinez B, Ma
L, Kilgore JA, Williams NS, Frantz DE, Wigginton JG, Nwariaku FE,
et al: Specific inhibition of mitochondrial oxidative stress
suppresses inflammation and improves cardiac function in a rat
pneumonia-related sepsis model. Am J Physiol Heart Circ Physiol.
302:H1847–H1859. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Vanasco V, Cimolai MC, Evelson P and
Alvarez S: The oxidative stress and the mitochondrial dysfunction
caused by endotoxemia are prevented by alpha-lipoic acid. Free
Radic Res. 42:815–823. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Vandewalle J and Libert C: Sepsis: A
failing starvation response. Trends Endocrinol Metab. 33:292–304.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Lelubre C and Vincent JL: Mechanisms and
treatment of organ failure in sepsis. Nat Rev Nephrol. 14:417–427.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Collins K and Huen SC: Metabolism and
nutrition in sepsis: In need of a paradigm shift. Nephron. Sep
13–2023.(Epub ahead of print). View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Wolowczuk I, Verwaerde C, Viltart O,
Delanoye A, Delacre M, Pot B and Grangette C: Feeding our immune
system: Impact on metabolism. Clin Dev Immunol. 2008:6398032008.
View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Rittig N, Bach E, Thomsen HH, Pedersen SB,
Nielsen TS, Jørgensen JO, Jessen N and Møller N: Regulation of
lipolysis and adipose tissue signaling during acute
endotoxin-induced inflammation: A human randomized crossover trial.
PLoS One. 11:e01621672016. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
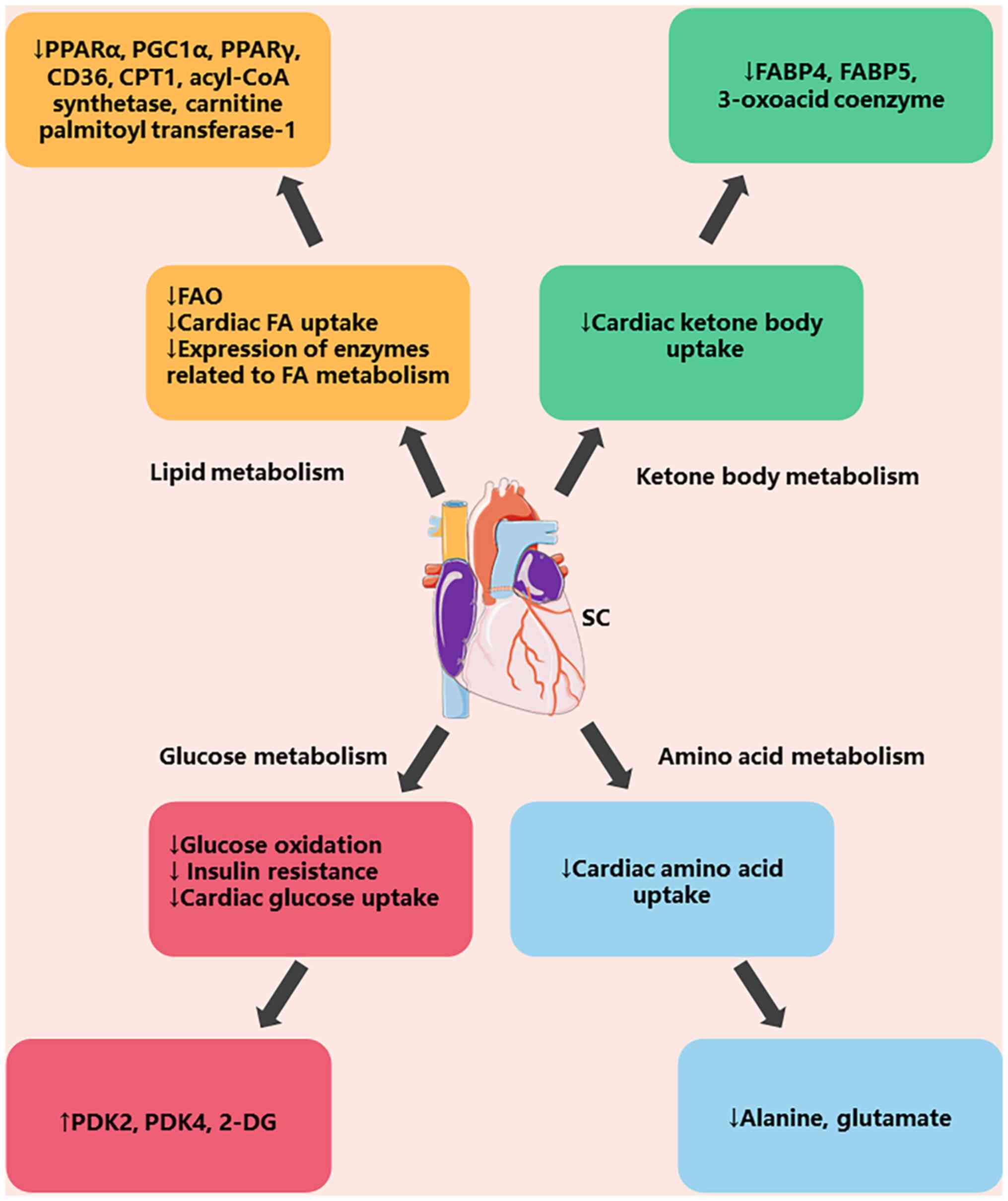
Drosatos K, Drosatos-Tampakaki Z, Khan R,
Homma S, Schulze PC, Zannis VI and Goldberg IJ: Inhibition of
c-Jun-N-terminal kinase increases cardiac peroxisome
proliferator-activated receptor alpha expression and fatty acid
oxidation and prevents lipopolysaccharide-induced heart
dysfunction. J Biol Chem. 286:36331–36339. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Wang W, Xu RL, He P and Chen R: MAR1
suppresses inflammatory response in LPS-induced RAW 264.7
macrophages and human primary peripheral blood mononuclear cells
via the SIRT1/PGC-1α/PPAR-γ pathway. J Inflamm (Lond). 18:82021.
View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Drosatos K, Khan RS, Trent CM, Jiang H,
Son NH, Blaner WS, Homma S, Schulze PC and Goldberg IJ: Peroxisome
proliferator-activated receptor-γ activation prevents
sepsis-related cardiac dysfunction and mortality in mice. Circ
Heart Fail. 6:550–562. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Sharma S, Adrogue JV, Golfman L, Uray I,
Lemm J, Youker K, Noon GP, Frazier OH and Taegtmeyer H:
Intramyocardial lipid accumulation in the failing human heart
resembles the lipotoxic rat heart. FASEB J. 18:1692–1700. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Memon RA, Fuller J, Moser AH, Smith PJ,
Feingold KR and Grunfeld C: In vivo regulation of acyl-CoA
synthetase mRNA and activity by endotoxin and cytokines. Am J
Physiol. 275:E64–E72. 1998.PubMed/NCBI
|
|
66
|
Feingold K, Kim M, Shigenaga J, Moser A
and Grunfeld C: Altered expression of nuclear hormone receptors and
coactivators in mouse heart during the acute-phase response. Am J
Physiol Endocrinol Metab. 286:E201–E207. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Rossi MA, Celes MRN, Prado CM and Saggioro
FP: Myocardial structural changes in long-term human severe
sepsis/septic shock may be responsible for cardiac dysfunction.
Shock. 27:10–18. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Koskinas J, Gomatos IP, Tiniakos DG, Memos
N, Boutsikou M, Garatzioti A, Archimandritis A and Betrosian A:
Liver histology in ICU patients dying from sepsis: A
clinico-pathological study. World J Gastroenterol. 14:1389–1393.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Shimazu T, Hirschey MD, Newman J, He W,
Shirakawa K, Le Moan N, Grueter CA, Lim H, Saunders LR, Stevens RD,
et al: Suppression of oxidative stress by β-hydroxybutyrate, an
endogenous histone deacetylase inhibitor. Science. 339:211–214.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Aubert G, Martin OJ, Horton JL, Lai L,
Vega RB, Leone TC, Koves T, Gardell SJ, Krüger M, Hoppel CL, et al:
The failing heart relies on ketone bodies as a fuel. Circulation.
133:698–705. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Wang A, Huen SC, Luan HH, Yu S, Zhang C,
Gallezot JD, Booth CJ and Medzhitov R: Opposing effects of fasting
metabolism on tissue tolerance in bacterial and viral inflammation.
Cell. 166:1512–1525.e12. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Umbarawan Y, Syamsunarno MRAA, Obinata H,
Yamaguchi A, Sunaga H, Matsui H, Hishiki T, Matsuura T, Koitabashi
N, Obokata M, et al: Robust suppression of cardiac energy
catabolism with marked accumulation of energy substrates during
lipopolysaccharide-induced cardiac dysfunction in mice. Metabolism.
77:47–57. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Soni S, Martens MD, Takahara S, Silver HL,
Maayah ZH, Ussher JR, Ferdaoussi M and Dyck JRB: Exogenous ketone
ester administration attenuates systemic inflammation and reduces
organ damage in a lipopolysaccharide model of sepsis. Biochim
Biophys Acta Mol Basis Dis. 1868:1665072022. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Dhainaut JF, Huyghebaert MF, Monsallier
JF, Lefevre G, Dall'Ava-Santucci J, Brunet F, Villemant D, Carli A
and Raichvarg D: Coronary hemodynamics and myocardial metabolism of
lactate, free fatty acids, glucose, and ketones in patients with
septic shock. Circulation. 75:533–541. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Chew MS, Shekar K, Brand BA, Norin C and
Barnett AG: Depletion of myocardial glucose is observed during
endotoxemic but not hemorrhagic shock in a porcine model. Crit
Care. 17:R1642013. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Liu T, Wen Z, Shao L, Cui Y, Tang X, Miao
H, Shi J, Jiang L, Feng S, Zhao Y, et al: ATF4 knockdown in
macrophage impairs glycolysis and mediates immune tolerance by
targeting HK2 and HIF-1α ubiquitination in sepsis. Clin Immunol.
254:1096982023. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Standage SW, Bennion BG, Knowles TO, Ledee
DR, Portman MA, McGuire JK, Liles WC and Olson AK: PPARα augments
heart function and cardiac fatty acid oxidation in early
experimental polymicrobial sepsis. Am J Physiol Heart Circ Physiol.
312:H239–H249. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Zheng Z, Ma H, Zhang X, Tu F, Wang X, Ha
T, Fan M, Liu L, Xu J, Yu K, et al: Enhanced glycolytic metabolism
contributes to cardiac dysfunction in polymicrobial sepsis. J
Infect Dis. 215:1396–1406. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Lang CH, Frost RA, Jefferson LS, Kimball
SR and Vary TC: Endotoxin-induced decrease in muscle protein
synthesis is associated with changes in eIF2B, eIF4E, and IGF-I. Am
J Physiol Endocrinol Metab. 278:E1133–E1143. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Lang CH, Frost RA, Nairn AC, MacLean DA
and Vary TC: TNF-alpha impairs heart and skeletal muscle protein
synthesis by altering translation initiation. Am J Physiol
Endocrinol Metab. 282:E336–E347. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Plank LD and Hill GL: Sequential metabolic
changes following induction of systemic inflammatory response in
patients with severe sepsis or major blunt trauma. World J Surg.
24:630–638. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Warner BW, Hummel RP III, Hasselgren PO,
James JH and Fischer JE: Inhibited amino acid uptake in skeletal
muscle during starvation. JPEN J Parenter Enteral Nutr. 13:344–348.
1989. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Zhang Q, Bao X, Cui M, Wang C, Ji J, Jing
J, Zhou X, Chen K and Tang L: Identification and validation of key
biomarkers based on RNA methylation genes in sepsis. Front Immunol.
14:12318982023. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Hotchkiss RS, Song SK, Neil JJ, Chen RD,
Manchester JK, Karl IE, Lowry OH and Ackerman JJ: Sepsis does not
impair tricarboxylic acid cycle in the heart. Am J Physiol.
260:C50–C57. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Sun S, Wang D, Dong D, Xu L, Xie M, Wang
Y, Ni T, Jiang W, Zhu X, Ning N, et al: Altered intestinal
microbiome and metabolome correspond to the clinical outcome of
sepsis. Crit Care. 27:1272023. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Chang WH and Lai AG: The pan-cancer
mutational landscape of the PPAR pathway reveals universal patterns
of dysregulated metabolism and interactions with tumor immunity and
hypoxia. Ann N Y Acad Sci. 1448:65–82. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Anghel SI and Wahli W: Fat poetry: A
kingdom for PPAR gamma. Cell Res. 17:486–511. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Christodoulides C and Vidal-Puig A: PPARs
and adipocyte function. Mol Cell Endocrinol. 318:61–68. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Villarroel-Vicente C, Gutiérrez-Palomo S,
Ferri J, Cortes D and Cabedo N: Natural products and analogs as
preventive agents for metabolic syndrome via peroxisome
proliferator-activated receptors: An overview. Eur J Med Chem.
221:1135352021. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
von Knethen A, Soller M and Brüne B:
Peroxisome proliferator-activated receptor gamma (PPAR gamma) and
sepsis. Arch Immunol Ther Exp (Warsz). 55:19–25. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Li Z, Jia Y, Feng Y, Cui R, Wang Z, Qu K,
Liu C and Zhang J: Methane-rich saline protects against
sepsis-induced liver damage by regulating the PPAR-γ/NF-κB
signaling pathway. Shock. 52:e163–e172. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Gong W, Zhu H, Lu L, Hou Y and Dou H: A
benzenediamine analog FC-99 drives M2 macrophage polarization and
alleviates lipopolysaccharide-(LPS-) induced liver injury.
Mediators Inflamm. 2019:78230692019. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Wen Q, Miao J, Lau N, Zhang C, Ye P, Du S,
Mei L, Weng H, Xu Q, Liu X, et al: Rhein attenuates
lipopolysaccharide-primed inflammation through NF-κB inhibition in
RAW264.7 cells: targeting the PPAR-γ signal pathway. Can J Physiol
Pharmacol. 98:357–365. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Xia H, Ge Y, Wang F, Ming Y, Wu Z, Wang J,
Sun S, Huang S, Chen M, Xiao W and Yao S: Protectin DX ameliorates
inflammation in sepsis-induced acute lung injury through mediating
PPARγ/NF-κB pathway. Immunol Res. 68:280–288. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Chen Q, Shao X, He Y, Lu E, Zhu L and Tang
W: Norisoboldine attenuates sepsis-induced acute lung injury by
modulating macrophage polarization via PKM2/HIF-1α/PGC-1α pathway.
Biol Pharm Bull. 44:1536–1547. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Zhu XX, Wang X, Jiao SY, Liu Y, Shi L, Xu
Q, Wang JJ, Chen YE, Zhang Q, Song YT, et al: Cardiomyocyte
peroxisome proliferator-activated receptor α prevents septic
cardiomyopathy via improving mitochondrial function. Acta Pharmacol
Sin. Jun 16–2023.(Epub ahead of print).
|
|
97
|
Chen W, Wang Y, Zhou Y, Xu Y, Bo X and Wu
J: M1 macrophages increase endothelial permeability and enhance p38
phosphorylation via PPAR-γ/CXCL13-CXCR5 in sepsis. Int Arch Allergy
Immunol. 183:997–1006. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Mitchell S, Vargas J and Hoffmann A:
Signaling via the NFκB system. Wiley Interdiscip Rev Syst Biol Med.
8:227–241. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Somensi N, Rabelo TK, Guimarães AG,
Quintans-Junior LJ, de Souza Araújo AA, Moreira JCF and Gelain DP:
Carvacrol suppresses LPS-induced pro-inflammatory activation in RAW
264.7 macrophages through ERK1/2 and NF-kB pathway. Int
Immunopharmacol. 75:1057432019. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Liu B, Wu Y, Wang Y, Cheng Y, Yao L, Liu
Y, Qian H, Yang H and Shen F: NF-κB p65 Knock-down inhibits TF,
PAI-1 and promotes activated protein C production in
lipopolysaccharide-stimulated alveolar epithelial cells type II.
Exp Lung Res. 44:241–251. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Wu Z, Chen J, Zhao W, Zhuo CH and Chen Q:
Inhibition of miR-181a attenuates sepsis-induced inflammation and
apoptosis by activating Nrf2 and inhibiting NF-κB pathways via
targeting SIRT1. Kaohsiung J Med Sci. 37:200–207. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Liu SF and Malik AB: NF-kappa B activation
as a pathological mechanism of septic shock and inflammation. Am J
Physiol Lung Cell Mol Physiol. 290:L622–L645. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Zang B and Wang L: Synthesis and
protective effect of pyrazole conjugated imidazo[1,2-a]pyrazine
derivatives against acute lung injury in sepsis rats via
attenuation of NF-κB, oxidative stress, and apoptosis. Acta Pharm.
73:341–362. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Cao L and Yang K: Paeoniflorin attenuated
TREM-1-mediated inflammation in THP-1 cells. J Healthc Eng.
2022:70516432022. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Wang X, Xu T, Jin J, Ting Gao MM, Wan B,
Gong M, Bai L, Lv T and Song Y: Topotecan reduces sepsis-induced
acute lung injury and decreases the inflammatory response via the
inhibition of the NF-κB signaling pathway. Pulm Circ.
12:e120702022. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Franco JH, Chen X and Pan ZK: Novel
treatments targeting the dysregulated cell signaling pathway during
sepsis. J Cell Signal. 2:228–234. 2021.PubMed/NCBI
|
|
107
|
Ruan W, Ji X, Qin Y, Zhang X, Wan X, Zhu
C, Lv C, Hu C, Zhou J, Lu L and Guo X: Harmine alleviated
sepsis-induced cardiac dysfunction by modulating macrophage
polarization via the STAT/MAPK/NF-κB pathway. Front Cell Dev Biol.
9:7922572022. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Dang X, Huan X, Du X, Chen X, Bi M, Yan C,
Jiao Q and Jiang H: Correlation of ferroptosis and other types of
cell death in neurodegenerative diseases. Neurosci Bull.
38:938–952. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
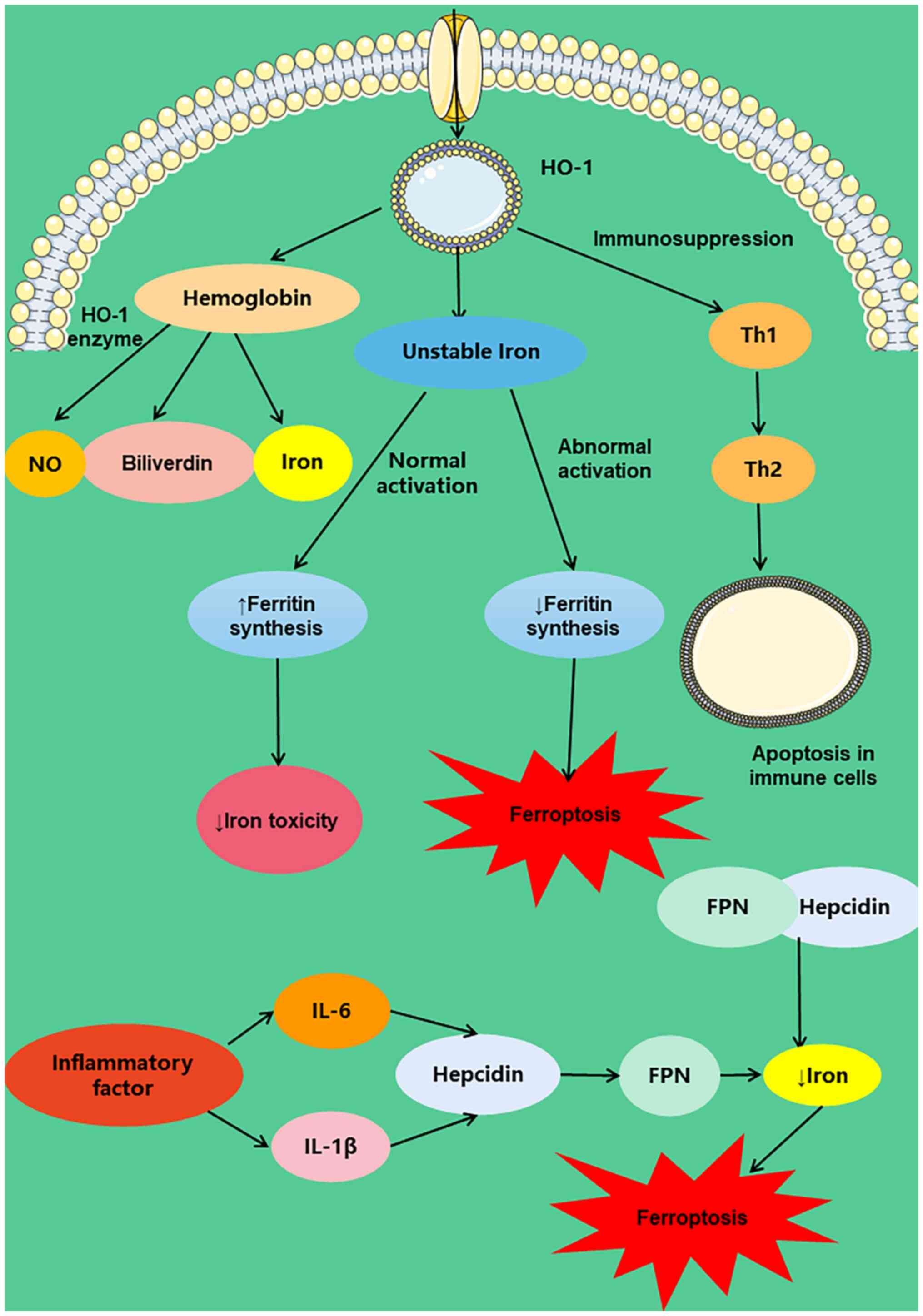
Kim J and Wessling-Resnick M: The role of
iron metabolism in lung inflammation and injury. J Allergy Ther. 3
(Suppl 4):S0042012.
|
|
110
|
de Lima VM, Batista BB and da Silva Neto
JF: The regulatory protein ChuP connects heme and
siderophore-mediated iron acquisition systems required for
chromobacterium violaceum virulence. Front Cell Infect Microbiol.
12:8735362022. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Englert FA, Seidel RA, Galler K, Gouveia
Z, Soares MP, Neugebauer U, Clemens MG, Sponholz C, Heinemann SH,
Pohnert G, et al: Labile heme impairs hepatic microcirculation and
promotes hepatic injury. Arch Biochem Biophys. 672:1080752019.
View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Stefanson AL and Bakovic M: Falcarinol Is
a potent inducer of heme oxygenase-1 and was more effective than
sulforaphane in attenuating intestinal inflammation at
diet-achievable doses. Oxid Med Cell Longev. 2018:31535272018.
View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Yoon SJ, Kim SJ and Lee SM: Overexpression
of HO-1 contributes to sepsis-induced immunosuppression by
modulating the Th1/Th2 balance and regulatory T-cell function. J
Infect Dis. 215:1608–1618. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Puentes-Pardo JD, Moreno-SanJuan S, Carazo
Á and León J: Heme oxygenase-1 in gastrointestinal tract health and
disease. Antioxidants (Basel). 9:12142020. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Fernández-Mendívil C, Luengo E,
Trigo-Alonso P, García-Magro N, Negredo P and López MG: Protective
role of microglial HO-1 blockade in aging: Implication of iron
metabolism. Redox Biol. 38:1017892021. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Qiao B, Sugianto P, Fung E,
Del-Castillo-Rueda A, Moran-Jimenez MJ, Ganz T and Nemeth E:
Hepcidin-induced endocytosis of ferroportin is dependent on
ferroportin ubiquitination. Cell Metab. 15:918–924. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Cross JH, Jarjou O, Mohammed NI, Gomez SR,
Touray BJB, Kessler NJ, Prentice AM and Cerami C: Iron homeostasis
in full-term, normal birthweight Gambian neonates over the first
week of life. Sci Rep. 13:103492023. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Drakesmith H and Prentice AM: Hepcidin and
the iron-infection axis. Science. 338:768–772. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Scindia Y, Wlazlo E, Leeds J, Loi V,
Ledesma J, Cechova S, Ghias E and Swaminathan S: Protective role of
hepcidin in polymicrobial sepsis and acute kidney injury. Front
Pharmacol. 10:6152019. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Deng Q, Yang S, Sun L, Dong K, Li Y, Wu S
and Huang R: Salmonella effector SpvB aggravates dysregulation of
systemic iron metabolism via modulating the hepcidin-ferroportin
axis. Gut Microbes. 13:1–18. 2021. View Article : Google Scholar
|
|
121
|
Czempik PF and Wiórek A: Iron deficiency
in sepsis patients based on reticulocyte hemoglobin and hepcidin
concentration: A prospective cohort study. Arch Med Sci.
19:805–809. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Martinon F, Burns K and Tschopp J: The
inflammasome: A molecular platform triggering activation of
inflammatory caspases and processing of proIL-beta. Mol Cell.
10:417–426. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Shi J, Zhao Y, Wang K, Shi X, Wang Y,
Huang H, Zhuang Y, Cai T, Wang F and Shao F: Cleavage of GSDMD by
inflammatory caspases determines pyroptotic cell death. Nature.
526:660–665. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Feng Y, Li M, Yangzhong X, Zhang X, Zu A,
Hou Y, Li L and Sun S: Pyroptosis in inflammation-related
respiratory disease. J Physiol Biochem. 78:721–737. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Man SM, Karki R and Kanneganti TD:
Molecular mechanisms and functions of pyroptosis, inflammatory
caspases and inflammasomes in infectious diseases. Immunol Rev.
277:61–75. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Zeng C, Duan F, Hu J, Luo B, Huang B, Lou
X, Sun X, Li H, Zhang X, Yin S and Tan H: NLRP3
inflammasome-mediated pyroptosis contributes to the pathogenesis of
non-ischemic dilated cardiomyopathy. Redox Biol. 34:1015232020.
View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Wu S, Liao J, Hu G, Yan L, Su X, Ye J,
Zhang C, Tian T, Wang H and Wang Y: Corilagin alleviates
LPS-induced sepsis through inhibiting pyroptosis via targeting TIR
domain of MyD88 and binding CARD of ASC in macrophages. Biochem
Pharmacol. 1158062023.(Epub ahead of print). View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Dai S, Ye B, Zhong L, Chen Y, Hong G, Zhao
G, Su L and Lu Z: GSDMD mediates LPS-induced septic myocardial
dysfunction by regulating ROS-dependent NLRP3 inflammasome
activation. Front Cell Dev Biol. 9:7794322021. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Meng L, Gu T, Wang J, Zhang H and Nan C:
Knockdown of PHLDA1 alleviates sepsis-induced acute lung injury by
downregulating NLRP3 inflammasome activation. Allergol Immunopathol
(Madr). 51:41–47. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Li W, Shen X, Feng S, Liu Y, Zhao H, Zhou
G, Sang M, Sun X, Jiao R and Liu F: BRD4 inhibition by JQ1 protects
against LPS-induced cardiac dysfunction by inhibiting activation of
NLRP3 inflammasomes. Mol Biol Rep. 49:8197–8207. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Zhao M, Zheng Z, Zhang P, Xu Y, Zhang J,
Peng S, Liu J, Pan W, Yin Z, Xu S, et al: IL-30 protects against
sepsis-induced myocardial dysfunction by inhibiting
pro-inflammatory macrophage polarization and pyroptosis. iScience.
26:1075442023. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Nong Y, Wei X and Yu D: Inflammatory
mechanisms and intervention strategies for sepsis-induced
myocardial dysfunction. Immun Inflamm Dis. 11:e8602023. View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Lima MR and Silva D: Septic
cardiomyopathy: A narrative review. Rev Port Cardiol. 42:471–481.
2023.(In English, Portuguese). View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Nadamuni M, Venable AH and Huen SC: When a
calorie isn't just a calorie: A revised look at nutrition in
critically ill patients with sepsis and acute kidney injury. Curr
Opin Nephrol Hypertens. 31:358–366. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Costa NA, Pereira AG, Sugizaki CSA, Vieira
NM, Garcia LR, de Paiva SAR, Zornoff LAM, Azevedo PS, Polegato BF
and Minicucci MF: Insights into thiamine supplementation in
patients with septic shock. Front Med (Lausanne). 8:8051992022.
View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Huo L, Liu C, Yuan Y, Liu X and Cao Q:
Pharmacological inhibition of ferroptosis as a therapeutic target
for sepsis-associated organ damage. Eur J Med Chem. 257:1154382023.
View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Zhou P, Zhang S, Wang M and Zhou J: The
induction mechanism of ferroptosis, necroptosis, and pyroptosis in
inflammatory bowel disease, colorectal cancer, and intestinal
injury. Biomolecules. 13:8202023. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Wu J, Lan Y, Wu J and Zhu K:
Sepsis-induced acute lung injury is alleviated by small molecules
from dietary plants via pyroptosis modulation. J Agric Food Chem.
71:12153–12166. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Perveen I, Bukhari B, Najeeb M, Nazir S,
Faridi TA, Farooq M, Ahmad QU, Abusalah MAHA, ALjaraedah TY, Alraei
WY, et al: Hydrogen therapy and its future prospects for
ameliorating COVID-19: Clinical applications, efficacy, and
modality. Biomedicines. 11:18922023. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Expert Panel on Urological Imaging, .
Smith AD, Nikolaidis P, Khatri G, Chong ST, De Leon AD, Ganeshan D,
Gore JL, Gupta RT, Kwun R, et al: ACR appropriateness
criteria® acute pyelonephritis: 2022 Update. J Am Coll
Radiol. 19((11S)): S224–S239. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Diaconescu B, Uranues S, Fingerhut A,
Vartic M, Zago M, Kurihara H, Latifi R, Popa D, Leppäniemi A,
Tilsed J, et al: The bucharest ESTES consensus statement on
peritonitis. Eur J Trauma Emerg Surg. 46:1005–1023. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
142
|
Evans L, Rhodes A, Alhazzani W, Antonelli
M, Coopersmith CM, French C, Machado FR, Mcintyre L, Ostermann M,
Prescott HC, et al: Surviving sepsis campaign: International
guidelines for management of sepsis and septic shock 2021.
Intensive Care Med. 47:1181–1247. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Annane D, Pastores SM, Rochwerg B, Arlt W,
Balk RA, Beishuizen A, Briegel J, Carcillo J, Christ-Crain M,
Cooper MS, et al: Guidelines for the diagnosis and management of
critical illness-related corticosteroid insufficiency (CIRCI) in
critically ill patients (Part I): Society of critical care medicine
(SCCM) and European society of intensive care medicine (ESICM)
2017. Intensive Care Med. 43:1751–1763. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Marik PE, Pastores SM, Annane D, Meduri
GU, Sprung CL, Arlt W, Keh D, Briegel J, Beishuizen A, Dimopoulou
I, et al: Recommendations for the diagnosis and management of
corticosteroid insufficiency in critically ill adult patients:
Consensus statements from an international task force by the
American college of critical care medicine. Crit Care Med.
36:1937–1949. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Zhong G, Han Y, Zhu Q, Xu M, Chang X, Chen
M, Men L, Zhang Q and Wang L: The effects of Xuebijing injection
combined with ulinastatin as adjunctive therapy on sepsis: An
overview of systematic review and meta-analysis. Medicine
(Baltimore). 101:e311962022. View Article : Google Scholar : PubMed/NCBI
|
|
146
|
Xiaoxia Q, Cheng C, Minjian W, Huilin C,
Zhen L, Yuedong Y and Xingyu Z: Effect of integrative medicines on
28-day mortality from sepsis: A systematic review and network
meta-analysis. Eur Rev Med Pharmacol Sci. 26:664–677.
2022.PubMed/NCBI
|