|
1
|
Chai Y, Jiang X, Ito Y, Bringas P Jr, Han
J, Rowitch DH, Soriano P, McMahon AP and Sucov HM: Fate of the
mammalian cranial neural crest during tooth and mandibular
morphogenesis. Development. 127:1671–1679. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Chen G, Sun Q, Xie L, Jiang Z, Feng L, Yu
M, Guo W and Tian W: Comparison of the odontogenic differentiation
potential of dental follicle, dental papilla, and cranial neural
crest cells. J Endod. 41:1091–1099. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bastos VC, Gomez RS and Gomes CC:
Revisiting the human dental follicle: From tooth development to its
association with unerupted or impacted teeth and pathological
changes. Dev Dyn. 251:408–423. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
4
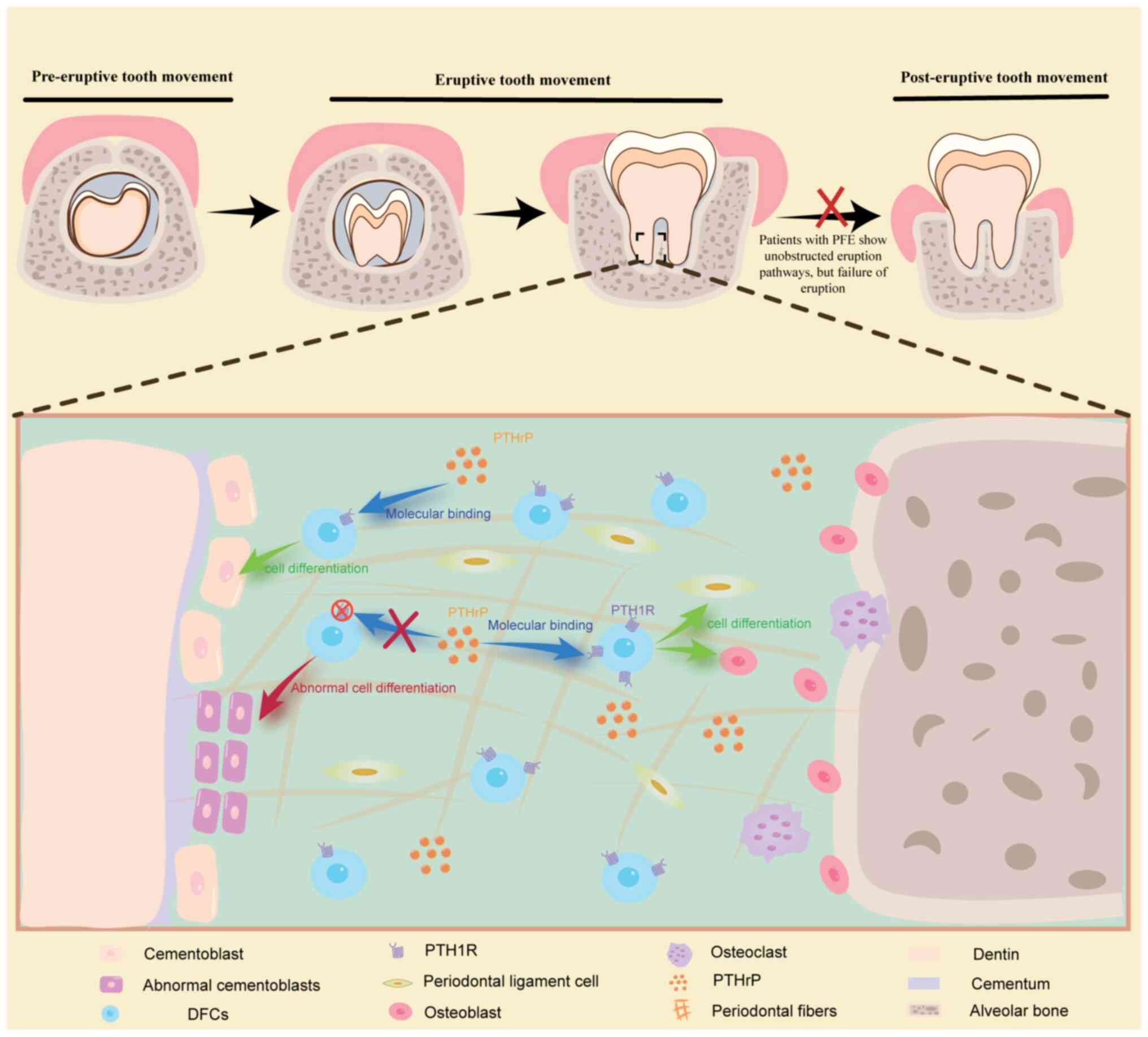
|
Wise GE and Yao S: Regional differences of
expression of bone morphogenetic protein-2 and RANKL in the rat
dental follicle. Eur J Oral Sci. 114:512–516. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Zhou T, Pan J, Wu P, Huang R, Du W, Zhou
Y, Wan M, Fan Y, Xu X, Zhou X, et al: Dental follicle cells: roles
in development and beyond. Stem Cells Int. 2019:91596052019.
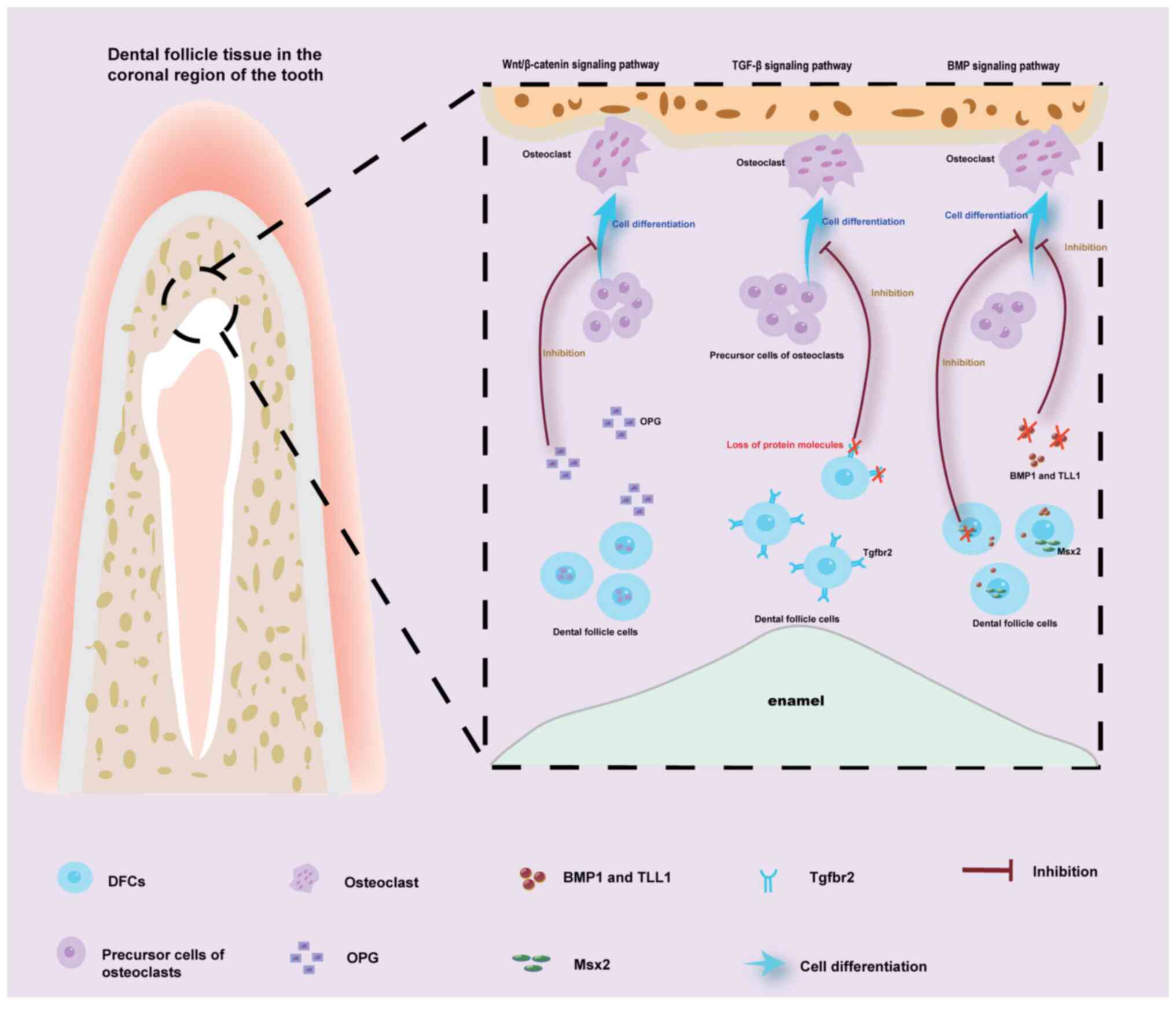
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
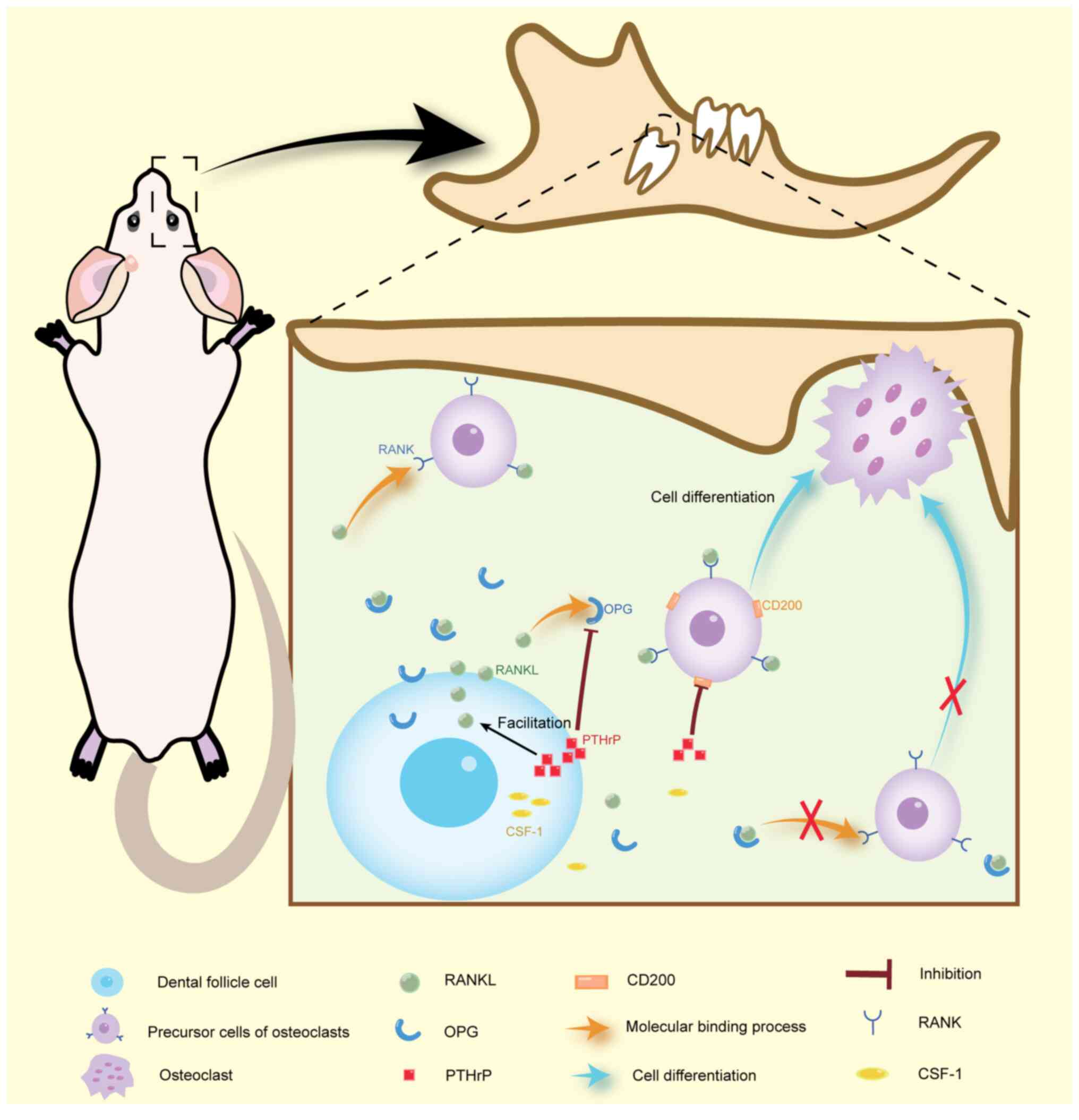
Morsczeck C, Götz W, Schierholz J,
Zeilhofer F, Kühn U, Möhl C, Sippel C and Hoffmann KH: Isolation of
precursor cells (PCs) from human dental follicle of wisdom teeth.
Matrix Biol. 24:155–165. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Bi R, Lyu P, Song Y, Li P, Song D, Cui C
and Fan Y: Function of dental follicle progenitor/stem cells and
their potential in regenerative medicine: From mechanisms to
applications. Biomolecules. 11:9972021. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yao S, Pan F, Prpic V and Wise GE:
Differentiation of stem cells in the dental follicle. J Dent Res.
87:767–771. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Liu J, Yu F, Sun Y, Jiang B, Zhang W, Yang
J, Xu GT, Liang A and Liu S: Concise reviews: Characteristics and
potential applications of human dental tissue-derived mesenchymal
stem cells. Stem Cells. 33:627–638. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Morsczeck C, Völlner F, Saugspier M,
Brandl C, Reichert TE, Driemel O and Schmalz G: Comparison of human
dental follicle cells (DFCs) and stem cells from human exfoliated
deciduous teeth (SHED) after neural differentiation in vitro. Clin
Oral Investig. 14:433–440. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Richman JM: Shedding new light on the
mysteries of tooth eruption. Proc Natl Acad Sci USA. 116:353–355.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zeng L, He H, Sun M, Gong X, Zhou M, Hong
Y, Wu Y, Chen X and Chen Q: Runx2 and Nell-1 in dental follicle
progenitor cells regulate bone remodeling and tooth eruption. Stem
Cell Res Ther. 13:4862022. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yu Y, Cui C, Guan SY, Xu RS, Zheng LW,
Zhou XD and Fan Y: Function of orofacial stem cells in tooth
eruption: An evolving perspective. Chin J Dent Res. 24:143–152.
2021.PubMed/NCBI
|
|
14
|
Suri L, Gagari E and Vastardis H: Delayed
tooth eruption: Pathogenesis, diagnosis, and treatment. A
literature review. Am J Orthod Dentofacial Orthop. 126:432–445.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Marks SC Jr and Cahill DR: Regional
control by the dental follicle of alterations in alveolar bone
metabolism during tooth eruption. J Oral Pathol. 16:164–169. 1987.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Cahill DR and Marks SC Jr: Tooth eruption:
Evidence for the central role of the dental follicle. J Oral
Pathol. 9:189–200. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Roulias P, Kalantzis N, Doukaki D, Pachiou
A, Karamesinis K, Damanakis G, Gizani S and Tsolakis AI: Teeth
eruption disorders: A critical review. Children (Basel).
9:7712022.PubMed/NCBI
|
|
18
|
Rasmussen P and Kotsaki A: Inherited
retarded eruption in the permanent dentition. J Clin Pediatr Dent.
21:205–211. 1997.PubMed/NCBI
|
|
19
|
Raghoebar GM, Boering G, Vissink A and
Stegenga B: Eruption disturbances of permanent molars: A review. J
Oral Pathol Med. 20:159–166. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Raghoebar GM, Boering G and Vissink A:
Clinical, radiographic and histological characteristics of
secondary retention of permanent molars. J Dent. 19:164–170. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Jain S, Raza M, Sharma P and Kumar P:
Unraveling impacted maxillary incisors: The why, when, and how. Int
J Clin Pediatr Dent. 14:149–157. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Morsczeck C, De Pellegrin M, Reck A and
Reichert TE: Evaluation of current studies to elucidate processes
in dental follicle cells driving osteogenic differentiation.
Biomedicines. 11:27872023. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Oosterkamp BC, Ockeloen CW, Carels CE and
Kuijpers-Jagtman AM: Tooth eruption disturbances and syndromes. Ned
Tijdschr Tandheelkd. 121:233–238. 2014.(In Dutch). View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Wise GE: Cellular and molecular basis of
tooth eruption. Orthod Craniofac Res. 12:67–73. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Wise GE, Frazier-Bowers S and D'Souza RN:
Cellular, molecular, and genetic determinants of tooth eruption.
Crit Rev Oral Biol Med. 13:323–334. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Li XX, Wang MT, Wu ZF, Sun Q, Ono N,
Nagata M, Zang XL and Ono W: Etiological mechanisms and
genetic/biological modulation related to PTH1R in primary failure
of tooth eruption. Calcif Tissue Int. Jun 4–2024.(Epub ahead of
print). View Article : Google Scholar
|
|
27
|
Guo X and Duan X: Genotype-phenotype
analysis of selective failure of tooth eruption-A systematic
review. Clin Genet. 104:287–297. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Hanisch M, Hanisch L, Kleinheinz J and
Jung S: Primary failure of eruption (PFE): A systematic review.
Head Face Med. 14:52018. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Yamaguchi T, Hosomichi K, Shirota T,
Miyamoto Y, Ono W and Ono N: Primary failure of tooth eruption:
Etiology and management. Jpn Dent Sci Rev. 58:258–267. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Librizzi M, Naselli F, Abruscato G,
Luparello C and Caradonna F: Parathyroid hormone related protein
(PTHrP)-associated molecular signatures in tissue differentiation
and non-tumoral diseases. Biology (Basel). 12:9502023.PubMed/NCBI
|
|
31
|
Wysolmerski JJ, Broadus AE, Zhou J, Fuchs
E, Milstone LM and Philbrick WM: Overexpression of parathyroid
hormone-related protein in the skin of transgenic mice interferes
with hair follicle development. Proc Natl Acad Sci USA.
91:1133–1137. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Wysolmerski JJ, McCaughern-Carucci JF,
Daifotis AG, Broadus AE and Philbrick WM: Overexpression of
parathyroid hormone-related protein or parathyroid hormone in
transgenic mice impairs branching morphogenesis during mammary
gland development. Development. 121:3539–3547. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Vasavada RC, Cavaliere C, D'Ercole AJ,
Dann P, Burtis WJ, Madlener AL, Zawalich K, Zawalich W, Philbrick W
and Stewart AF: Overexpression of parathyroid hormone-related
protein in the pancreatic islets of transgenic mice causes islet
hyperplasia, hyperinsulinemia, and hypoglycemia. J Biol Chem.
271:1200–1208. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Foley J, Longely BJ, Wysolmerski JJ,
Dreyer BE, Broadus AE and Philbrick WM: PTHrP regulates epidermal
differentiation in adult mice. J Invest Dermatol. 111:1122–1128.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Nagata M, Ono N and Ono W: Mesenchymal
progenitor regulation of tooth eruption: A view from PTHrP. J Dent
Res. 99:133–142. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Zhang J, Liao L, Li Y, Xu Y, Guo W, Tian W
and Zou S: Parathyroid hormone-related peptide (1–34) promotes
tooth eruption and inhibits osteogenesis of dental follicle cells
during tooth development. J Cell Physiol. 234:11900–11911. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Obara N, Suzuki Y and Takeda M: Gene
expression of beta-catenin is up-regulated in inner dental
epithelium and enamel knots during molar tooth morphogenesis in the
mouse. Cell Tissue Res. 325:197–201. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
MacDonald BT, Tamai K and He X:
Wnt/beta-catenin signaling: Components, mechanisms, and diseases.
Dev Cell. 17:9–26. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Wodarz A and Nusse R: Mechanisms of Wnt
signaling in development. Annu Rev Cell Dev Biol. 14:59–88. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Ouyang H, McCauley LK, Berry JE, Saygin
NE, Tokiyasu Y and Somerman MJ: Parathyroid hormone-related protein
regulates extracellular matrix gene expression in cementoblasts and
inhibits cementoblast-mediated mineralization in vitro. J Bone
Miner Res. 15:2140–2153. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Philbrick WM, Dreyer BE, Nakchbandi IA and
Karaplis AC: Parathyroid hormone-related protein is required for
tooth eruption. Proc Natl Acad Sci USA. 95:11846–11851. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Heinrich J, Bsoul S, Barnes J, Woodruff K
and Abboud S: CSF-1, RANKL and OPG regulate osteoclastogenesis
during murine tooth eruption. Arch Oral Biol. 50:897–908. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Ibáñez L, Nácher-Juan J, Terencio MC,
Ferrándiz ML and Alcaraz MJ: Osteostatin inhibits
M-CSF+RANKL-induced human osteoclast differentiation by modulating
NFATc1. Int J Mol Sci. 23:85512022. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Shiyan H, Nanquan R, Shuhao X and Xiaobing
L: Research progress on the cellular and molecular mechanisms of
tooth eruption. Hua Xi Kou Qiang Yi Xue Za Zhi. 34:317–321.
2016.(In Chinese). PubMed/NCBI
|
|
45
|
Udagawa N, Koide M, Nakamura M, Nakamichi
Y, Yamashita T, Uehara S, Kobayashi Y, Furuya Y, Yasuda H, Fukuda C
and Tsuda E: Osteoclast differentiation by RANKL and OPG signaling
pathways. J Bone Miner Metab. 39:19–26. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Huang H, Wang J, Zhang Y, Zhu G, Li YP,
Ping J and Chen W: Bone resorption deficiency affects tooth root
development in RANKL mutant mice due to attenuated IGF-1 signaling
in radicular odontoblasts. Bone. 114:161–171. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Cui W, Cuartas E, Ke J, Zhang Q, Einarsson
HB, Sedgwick JD, Li J and Vignery A: CD200 and its receptor,
CD200R, modulate bone mass via the differentiation of osteoclasts.
Proc Natl Acad Sci USA. 104:14436–14441. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Ono W, Sakagami N, Nishimori S, Ono N and
Kronenberg HM: Parathyroid hormone receptor signalling in
osterix-expressing mesenchymal progenitors is essential for tooth
root formation. Nat Commun. 7:112772016. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Dean T, Vilardaga JP, Potts JT Jr and
Gardella TJ: Altered selectivity of parathyroid hormone (PTH) and
PTH-related protein (PTHrP) for distinct conformations of the
PTH/PTHrP receptor. Mol Endocrinol. 22:156–166. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Martin TJ, Sims NA and Seeman E:
Physiological and pharmacological roles of PTH and PTHrP in bone
using their shared receptor, PTH1R. Endocr Rev. 42:383–406. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Aziz S, Hermann NV, Dunø M, Risom L,
Daugaard-Jensen J and Kreiborg S: Primary failure of eruption of
teeth in two siblings with a novel mutation in the PTH1R gene. Eur
Arch Paediatr Dent. 20:295–300. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Kanno CM, de Oliveira JA, Garcia JF, Roth
H and Weber BH: Twenty-year follow-up of a familial case of
PTH1R-associated primary failure of tooth eruption. Am J Orthod
Dentofacial Orthop. 151:598–606. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Frazier-Bowers SA, Simmons D, Wright JT,
Proffit WR and Ackerman JL: Primary failure of eruption and PTH1R:
The importance of a genetic diagnosis for orthodontic treatment
planning. Am J Orthod Dentofacial Orthop. 137:160–161. e1–e7. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Stutz C, Wagner D, Gros CI, Sayeh A,
Gegout H, Kuchler-Bopp S and Strub M: Primary failure of eruption
and tooth resorption. Orthod Fr. 93:283–288. 2022.(In French).
PubMed/NCBI
|
|
55
|
Decker E, Stellzig-Eisenhauer A, Fiebig
BS, Rau C, Kress W, Saar K, Rüschendorf F, Hubner N, Grimm T and
Weber BH: PTHR1 loss-of-function mutations in familial,
nonsyndromic primary failure of tooth eruption. Am J Hum Genet.
83:781–786. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Wise GE and King GJ: Mechanisms of tooth
eruption and orthodontic tooth movement. J Dent Res. 87:414–434.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Wise GE, Yao S and Henk WG: Bone formation
as a potential motive force of tooth eruption in the rat molar.
Clin Anat. 20:632–639. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Li J, Parada C and Chai Y: Cellular and
molecular mechanisms of tooth root development. Development.
144:374–384. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Takahashi A, Nagata M, Gupta A, Matsushita
Y, Yamaguchi T, Mizuhashi K, Maki K, Ruellas AC, Cevidanes LS,
Kronenberg HM, et al: Autocrine regulation of mesenchymal
progenitor cell fates orchestrates tooth eruption. Proc Natl Acad
Sci USA. 116:575–580. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Tokavanich N, Gupta A, Nagata M, Takahashi
A, Matsushita Y, Yatabe M, Ruellas A, Cevidanes L, Maki K,
Yamaguchi T, et al: A three-dimensional analysis of primary failure
of eruption in humans and mice. Oral Dis. 26:391–400. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Wang XP: Tooth eruption without roots. J
Dent Res. 92:212–214. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Vuong LT and Mlodzik M: Different
strategies by distinct Wnt-signaling pathways in activating a
nuclear transcriptional response. Curr Top Dev Biol. 149:59–89.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Tokavanich N, Wein MN, English JD, Ono N
and Ono W: The role of Wnt signaling in postnatal tooth root
development. Front Dent Med. 2:7691342021. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Liu F, Chu EY, Watt B, Zhang Y, Gallant
NM, Andl T, Yang SH, Lu MM, Piccolo S, Schmidt-Ullrich R, et al:
Wnt/beta-catenin signaling directs multiple stages of tooth
morphogenesis. Dev Biol. 313:210–224. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Zhang R, Yang G, Wu X, Xie J, Yang X and
Li T: Disruption of Wnt/β-catenin signaling in odontoblasts and
cementoblasts arrests tooth root development in postnatal mouse
teeth. Int J Biol Sci. 9:228–236. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Weivoda MM, Ruan M, Hachfeld CM, Pederson
L, Howe A, Davey RA, Zajac JD, Kobayashi Y, Williams BO, Westendorf
JJ, et al: Wnt signaling inhibits osteoclast differentiation by
activating canonical and noncanonical cAMP/PKA pathways. J Bone
Miner Res. 31:65–75. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Wei W, Zeve D, Suh JM, Wang X, Du Y,
Zerwekh JE, Dechow PC, Graff JM and Wan Y: Biphasic and
dosage-dependent regulation of osteoclastogenesis by β-catenin. Mol
Cell Biol. 31:4706–4719. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Kim TH, Bae CH, Jang EH, Yoon CY, Bae Y,
Ko SO, Taketo MM and Cho ES: Col1a1-cre mediated activation of
β-catenin leads to aberrant dento-alveolar complex formation. Anat
Cell Biol. 45:193–202. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Glass DA II, Bialek P, Ahn JD, Starbuck M,
Patel MS, Clevers H, Taketo MM, Long F, McMahon AP, Lang RA and
Karsenty G: Canonical Wnt signaling in differentiated osteoblasts
controls osteoclast differentiation. Dev Cell. 8:751–764. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Nie B, Zhang SY, Guan SM, Zhou SQ and Fang
X: Role of Wnt/β-catenin pathway in the arterial medial
calcification and its effect on the OPG/RANKL system. Curr Med Sci.
39:28–36. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Kim TH, Lee JY, Baek JA, Lee JC, Yang X,
Taketo MM, Jiang R and Cho ES: Constitutive stabilization of
ß-catenin in the dental mesenchyme leads to excessive dentin and
cementum formation. Biochem Biophys Res Commun. 412:549–555. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Wu Y, Yuan X, Perez KC, Hyman S, Wang L,
Pellegrini G, Salmon B, Bellido T and Helms JA: Aberrantly elevated
Wnt signaling is responsible for cementum overgrowth and dental
ankylosis. Bone. 122:176–183. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Bennett CN, Longo KA, Wright WS, Suva LJ,
Lane TF, Hankenson KD and MacDougald OA: Regulation of
osteoblastogenesis and bone mass by Wnt10b. Proc Natl Acad Sci USA.
102:3324–3329. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Bennett CN, Ouyang H, Ma YL, Zeng Q, Gerin
I, Sousa KM, Lane TF, Krishnan V, Hankenson KD and MacDougald OA:
Wnt10b increases postnatal bone formation by enhancing osteoblast
differentiation. J Bone Miner Res. 22:1924–1932. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Thesleff I and Nieminen P: Tooth
morphogenesis and cell differentiation. Curr Opin Cell Biol.
8:844–850. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Sui BD, Zheng CX, Zhao WM, Xuan K, Li B
and Jin Y: Mesenchymal condensation in tooth development and
regeneration: A focus on translational aspects of organogenesis.
Physiol Rev. 103:1899–1964. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Wang Y, Cox MK, Coricor G, MacDougall M
and Serra R: Inactivation of Tgfbr2 in Osterix-Cre expressing
dental mesenchyme disrupts molar root formation. Dev Biol.
382:27–37. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Massagué J: TGF-beta signal transduction.
Annu Rev Biochem. 67:753–791. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Ko SO, Chung IH, Xu X, Oka S, Zhao H, Cho
ES, Deng C and Chai Y: Smad4 is required to regulate the fate of
cranial neural crest cells. Dev Biol. 312:435–447. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Gao Y, Yang G, Weng T, Du J, Wang X, Zhou
J, Wang S and Yang X: Disruption of Smad4 in odontoblasts causes
multiple keratocystic odontogenic tumors and tooth malformation in
mice. Mol Cell Biol. 29:5941–5951. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Beederman M, Lamplot JD, Nan G, Wang J,
Liu X, Yin L, Li R, Shui W, Zhang H, Kim SH, et al: BMP signaling
in mesenchymal stem cell differentiation and bone formation. J
Biomed Sci Eng. 6:32–52. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Fabregat I, Herrera B and Sánchez A:
Editorial special issue TGF-beta/BMP signaling pathway. Cells.
9:23632020. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Rakian A, Yang WC, Gluhak-Heinrich J, Cui
Y, Harris MA, Villarreal D, Feng JQ, Macdougall M and Harris SE:
Bone morphogenetic protein-2 gene controls tooth root development
in coordination with formation of the periodontium. Int J Oral Sci.
5:75–84. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Wang J, Muir AM, Ren Y, Massoudi D,
Greenspan DS and Feng JQ: Essential roles of bone morphogenetic
protein-1 and mammalian tolloid-like 1 in postnatal root dentin
formation. J Endod. 43:109–115. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Ge G and Greenspan DS: Developmental roles
of the BMP1/TLD metalloproteinases. Birth Defects Res C Embryo
Today. 78:47–68. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Malik Z, Roth DM, Eaton F, Theodor JM and
Graf D: Mesenchymal Bmp7 controls onset of tooth mineralization: A
novel way to regulate molar cusp shape. Front Physiol. 11:6982020.
View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Semba I, Nonaka K, Takahashi I, Takahashi
K, Dashner R, Shum L, Nuckolls GH and Slavkin HC:
Positionally-dependent chondrogenesis induced by BMP4 is
co-regulated by Sox9 and Msx2. Dev Dyn. 217:401–414. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Cai C, Wang J, Huo N, Wen L, Xue P and
Huang Y: Msx2 plays an important role in BMP6-induced osteogenic
differentiation of two mesenchymal cell lines: C3H10T1/2 and C2C12.
Regen Ther. 14:245–251. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Aïoub M, Lézot F, Molla M, Castaneda B,
Robert B, Goubin G, Néfussi JR and Berdal A: Msx2 -/- transgenic
mice develop compound amelogenesis imperfecta, dentinogenesis
imperfecta and periodental osteopetrosis. Bone. 41:851–859. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Hosoya A, Shalehin N, Takebe H, Shimo T
and Irie K: Sonic hedgehog signaling and tooth development. Int J
Mol Sci. 21:15872020. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Nakatomi M, Morita I, Eto K and Ota MS:
Sonic hedgehog signaling is important in tooth root development. J
Dent Res. 85:427–431. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Jain P and Rathee M: Anatomy, Head and
Neck, Tooth Eruption. StatPearls [Internet]. StatPearls Publishing;
Treasure Island, FL: 2024, https://www.ncbi.nlm.nih.gov/books/NBK549878/
|
|
93
|
Kasugai S, Suzuki S, Shibata S, Yasui S,
Amano H and Ogura H: Measurements of the isometric contractile
forces generated by dog periodontal ligament fibroblasts in vitro.
Arch Oral Biol. 35:597–601. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Kalliala E and Taskinen PJ: Cleidocranial
dysostosis. Report of six typical cases and one atypical case. Oral
Surg Oral Med Oral Pathol. 15:808–822. 1962. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Shih-Wei Cheng E, Tsuji M, Suzuki S and
Moriyama K: An overview of the intraoral features and craniofacial
morphology of growing and adult Japanese cleidocranial dysplasia
subjects. Eur J Orthod. 44:711–722. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Jaruga A, Hordyjewska E, Kandzierski G and
Tylzanowski P: Cleidocranial dysplasia and RUNX2-clinical
phenotype-genotype correlation. Clin Genet. 90:393–402. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Komori T: Regulation of proliferation,
differentiation and functions of osteoblasts by Runx2. Int J Mol
Sci. 20:16942019. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Harada H, Tagashira S, Fujiwara M, Ogawa
S, Katsumata T, Yamaguchi A, Komori T and Nakatsuka M: Cbfa1
isoforms exert functional differences in osteoblast
differentiation. J Biol Chem. 274:6972–6978. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Komori T, Yagi H, Nomura S, Yamaguchi A,
Sasaki K, Deguchi K, Shimizu Y, Bronson RT, Gao YH, Inada M, et al:
Targeted disruption of Cbfa1 results in a complete lack of bone
formation owing to maturational arrest of osteoblasts. Cell.
89:755–764. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Otto F, Thornell AP, Crompton T, Denzel A,
Gilmour KC, Rosewell IR, Stamp GW, Beddington RS, Mundlos S, Olsen
BR, et al: Cbfa1, a candidate gene for cleidocranial dysplasia
syndrome, is essential for osteoblast differentiation and bone
development. Cell. 89:765–771. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Yoda S, Suda N, Kitahara Y, Komori T and
Ohyama K: Delayed tooth eruption and suppressed osteoclast number
in the eruption pathway of heterozygous Runx2/Cbfa1 knockout mice.
Arch Oral Biol. 49:435–442. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
D'Souza RN, Aberg T, Gaikwad J, Cavender
A, Owen M, Karsenty G and Thesleff I: Cbfa1 is required for
epithelial-mesenchymal interactions regulating tooth development in
mice. Development. 126:2911–2920. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Bronckers AL, Engelse MA, Cavender A,
Gaikwad J and D'Souza RN: Cell-specific patterns of Cbfa1 mRNA and
protein expression in postnatal murine dental tissues. Mech Dev.
101:255–258. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Liu Y, Sun X, Zhang X, Wang X, Zhang C and
Zheng S: RUNX2 mutation impairs osteogenic differentiation of
dental follicle cells. Arch Oral Biol. 97:156–164. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Nadyrshina DD and Khusainova RI: Clinical,
genetic aspects and molecular pathogenesis of osteopetrosis.
Vavilovskii Zhurnal Genet Selektsii. 27:383–392. 2023.PubMed/NCBI
|
|
106
|
Aker M, Rouvinski A, Hashavia S, Ta-Shma
A, Shaag A, Zenvirt S, Israel S, Weintraub M, Taraboulos A,
Bar-Shavit Z and Elpeleg O: An SNX10 mutation causes malignant
osteopetrosis of infancy. J Med Genet. 49:221–226. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Keng LT and Liang SK: Albers-Schönberg
disease. Korean J Intern Med. 34:1167–1168. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Luzzi V, Consoli G, Daryanani V, Santoro
G, Sfasciotti GL and Polimeni A: Malignant infantile osteopetrosis:
Dental effects in paediatric patients. Case reports. Eur J Paediatr
Dent. 7:39–44. 2006.PubMed/NCBI
|
|
109
|
Sobacchi C, Schulz A, Coxon FP, Villa A
and Helfrich MH: Osteopetrosis: Genetics, treatment and new
insights into osteoclast function. Nat Rev Endocrinol. 9:522–536.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Polgreen LE, Imel EA and Econs MJ:
Autosomal dominant osteopetrosis. Bone. 170:1167232023. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Wang H, Pan M, Ni J, Zhang Y, Zhang Y, Gao
S, Liu J, Wang Z, Zhang R, He H, et al: ClC-7 deficiency impairs
tooth development and eruption. Sci Rep. 6:199712016. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Xue Y, Wang W, Mao T and Duan X: Report of
two Chinese patients suffering from CLCN7-related osteopetrosis and
root dysplasia. J Craniomaxillofac Surg. 40:416–420. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Wise GE, Lumpkin SJ, Huang H and Zhang Q:
Osteoprotegerin and osteoclast differentiation factor in tooth
eruption. J Dent Res. 79:1937–1942. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Suzuki T, Suda N and Ohyama K:
Osteoclastogenesis during mouse tooth germ development is mediated
by receptor activator of NFKappa-B ligand (RANKL). J Bone Miner
Metab. 22:185–191. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Yasuda H: Discovery of the RANKL/RANK/OPG
system. J Bone Miner Metab. 39:2–11. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Morsczeck C, Moehl C, Götz W, Heredia A,
Schäffer TE, Eckstein N, Sippel C and Hoffmann KH: In vitro
differentiation of human dental follicle cells with dexamethasone
and insulin. Cell Biol Int. 29:567–575. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Nagpal R, Goyal RB, Priyadarshini K,
Kashyap S, Sharma M, Sinha R and Sharma N: Mucopolysaccharidosis: A
broad review. Indian J Ophthalmol. 70:2249–2261. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Smith KS, Hallett KB, Hall RK, Wardrop RW
and Firth N: Mucopolysaccharidosis: MPS VI and associated delayed
tooth eruption. Int J Oral Maxillofac Surg. 24:176–180. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Andersson HC: 50 Years ago in the journal
of pediatrics: Hurler's disease, Morquio's disease and related
mucopolysaccharidoses. J Pediatr. 167:3372015. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Costa-Motta FM, Bender F, Acosta A,
Abé-Sandes K, Machado T, Bomfim T, Boa Sorte T, da Silva D, Bittles
A, Giugliani R and Leistner-Segal S: A community-based study of
mucopolysaccharidosis type VI in Brazil: The influence of founder
effect, endogamy and consanguinity. Hum Hered. 77:189–196. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Vairo F, Federhen A, Baldo G, Riegel M,
Burin M, Leistner-Segal S and Giugliani R: Diagnostic and treatment
strategies in mucopolysaccharidosis VI. Appl Clin Genet. 8:245–255.
2015.PubMed/NCBI
|
|
122
|
Tomanin R, Karageorgos L, Zanetti A,
Al-Sayed M, Bailey M, Miller N, Sakuraba H and Hopwood JJ:
Mucopolysaccharidosis type VI (MPS VI) and molecular analysis:
Review and classification of published variants in the ARSB gene.
Hum Mutat. 39:1788–1802. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Alpöz AR, Coker M, Celen E, Ersin NK,
Gökçen D, van Diggelenc OP and Huijmansc JG: The oral
manifestations of Maroteaux-Lamy syndrome (mucopolysaccharidosis
VI): A case report. Oral Surg Oral Med Oral Pathol Oral Radiol
Endod. 101:632–637. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Simancas Escorcia V, Guillou C, Abbad L,
Derrien L, Rodrigues Rezende Costa C, Cannaya V, Benassarou M,
Chatziantoniou C, Berdal A, Acevedo AC, et al: Pathogenesis of
enamel-renal syndrome associated gingival fibromatosis: A proteomic
approach. Front Endocrinol (Lausanne). 12:7525682021. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Roomaney IA, Kabbashi S and Chetty M:
Enamel renal syndrome: Protocol for a scoping review. JMIR Res
Protoc. 10:e297022021. View
Article : Google Scholar : PubMed/NCBI
|
|
126
|
Crawford PJ, Aldred M and Bloch-Zupan A:
Amelogenesis imperfecta. Orphanet J Rare Dis. 2:172007. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Farias MLM, Ornela GO, de Andrade RS,
Martelli DRB, Dias VO and Júnior HM: Enamel renal syndrome: A
systematic review. Indian J Nephrol. 31:1–8. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Khalifa R, Kammoun R, Mansour L, Ben Alaya
T and Ghoul S: Enamel renal syndrome: A case report with
calcifications in pulp, gingivae, dental follicle and kidneys. Spec
Care Dentist. 44:722–728. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
de la Dure-Molla M, Quentric M, Yamaguti
PM, Acevedo AC, Mighell AJ, Vikkula M, Huckert M, Berdal A and
Bloch-Zupan A: Pathognomonic oral profile of enamel renal syndrome
(ERS) caused by recessive FAM20A mutations. Orphanet J Rare Dis.
9:842014. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Wang SK, Aref P, Hu Y, Milkovich RN,
Simmer JP, El-Khateeb M, Daggag H, Baqain ZH and Hu JC: FAM20A
mutations can cause enamel-renal syndrome (ERS). PLoS Genet.
9:e10033022013. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Wang SK, Reid BM, Dugan SL, Roggenbuck JA,
Read L, Aref P, Taheri AP, Yeganeh MZ, Simmer JP and Hu JC: FAM20A
mutations associated with enamel renal syndrome. J Dent Res.
93:42–48. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Nitayavardhana I, Theerapanon T,
Srichomthong C, Piwluang S, Wichadakul D, Porntaveetus T and
Shotelersuk V: Four novel mutations of FAM20A in amelogenesis
imperfecta type IG and review of literature for its genotype and
phenotype spectra. Mol Genet Genomics. 295:923–931. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Normand de la Tranchade I, Bonarek H,
Marteau JM, Boileau MJ and Nancy J: Amelogenesis imperfecta and
nephrocalcinosis: A new case of this rare syndrome. J Clin Pediatr
Dent. 27:171–175. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Alhilou A, Beddis HP, Mighell AJ and Durey
K: Dentin dysplasia: Diagnostic challenges. BMJ Case Rep.
2018:bcr20172239422018. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Shields ED, Bixler D and el-Kafrawy AM: A
proposed classification for heritable human dentine defects with a
description of a new entity. Arch Oral Biol. 18:543–553. 1973.
View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Akhil Jose EJ, Palathingal P, Baby D and
Thachil JM: Dentin dysplasia type I: A rare case report. J Oral
Maxillofac Pathol. 23:3092019. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Barron MJ, McDonnell ST, Mackie I and
Dixon MJ: Hereditary dentine disorders: Dentinogenesis imperfecta
and dentine dysplasia. Orphanet J Rare Dis. 3:312008. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Chen D, Li X, Lu F, Wang Y, Xiong F and Li
Q: Dentin dysplasia type I-a dental disease with genetic
heterogeneity. Oral Dis. 25:439–446. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Kalk WW, Batenburg RH and Vissink A:
Dentin dysplasia type I: Five cases within one family. Oral Surg
Oral Med Oral Pathol Oral Radiol Endod. 86:175–178. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Song YL and Bian Z: Recognition on dentin
dysplasia type II. Zhonghua Kou Qiang Yi Xue Za Zhi. 58:766–771.
2023.(In Chinese). PubMed/NCBI
|
|
141
|
Yang Q, Chen D, Xiong F, Chen D, Liu C,
Liu Y, Yu Q, Xiong J, Liu J, Li K, et al: A splicing mutation in
VPS4B causes dentin dysplasia I. J Med Genet. 53:624–633. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
142
|
Bloch-Zupan A, Jamet X, Etard C, Laugel V,
Muller J, Geoffroy V, Strauss JP, Pelletier V, Marion V, Poch O, et
al: Homozygosity mapping and candidate prioritization identify
mutations, missed by whole-exome sequencing, in SMOC2, causing
major dental developmental defects. Am J Hum Genet. 89:773–781.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Xiong F, Ji Z, Liu Y, Zhang Y, Hu L, Yang
Q, Qiu Q, Zhao L, Chen D, Tian Z, et al: Mutation in SSUH2 causes
autosomal-dominant dentin dysplasia type I. Hum Mutat. 38:95–104.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Handa K, Saito M, Yamauchi M, Kiyono T,
Sato S, Teranaka T and Sampath Narayanan A: Cementum matrix
formation in vivo by cultured dental follicle cells. Bone.
31:606–611. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Li Q, Lu F, Chen T, Zhang K, Lu Y, Li X,
Wang Y, Liu L, Tian Q, Xiong F and Chen D: VPS4B mutation impairs
the osteogenic differentiation of dental follicle cells derived
from a patient with dentin dysplasia type I. Int J Oral Sci.
12:222020. View Article : Google Scholar : PubMed/NCBI
|
|
146
|
Zegarelli EV, Kutscher AH, Applebaum E and
Archard HO: Odontodysplasia. Oral Surg Oral Med Oral Pathol.
16:187–193. 1963. View Article : Google Scholar : PubMed/NCBI
|
|
147
|
Crawford PJ and Aldred MJ: Regional
odontodysplasia: A bibliography. J Oral Pathol Med. 18:251–263.
1989. View Article : Google Scholar : PubMed/NCBI
|
|
148
|
Nijakowski K, Woś P and Surdacka A:
Regional odontodysplasia: A systematic review of case reports. Int
J Environ Res Public Health. 19:16832022. View Article : Google Scholar : PubMed/NCBI
|
|
149
|
Alotaibi O, Alotaibi G and Alfawaz N:
Regional odontodysplasia: An analysis of 161 cases from 1953 to
2017. Saudi Dent J. 31:306–310. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
150
|
Marques AC, Castro WH and do Carmo MA:
Regional odontodysplasia: An unusual case with a conservative
approach. Br Dent J. 186:522–524. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
151
|
Rushton MA: Odontodysplasia: ‘Ghost
teeth’. Br Dent J. 119:109–113. 1965.PubMed/NCBI
|
|
152
|
Carlos R, Contreras-Vidaurre E, Almeida
OP, Silva KR, Abrahão PG, Miranda AM and Pires FR: Regional
odontodysplasia: morphological, ultrastructural, and
immunohistochemical features of the affected teeth, connective
tissue, and odontogenic remnants. J Dent Child (Chic). 75:144–150.
2008.PubMed/NCBI
|
|
153
|
Kerebel B, Kerebel LM, Heron D and Le
Cabellec MT: Regional odontodysplasia: New histopathological data.
J Biol Buccale. 17:121–128. 1989.PubMed/NCBI
|
|
154
|
Kerebel LM and Kerebel B: Soft-tissue
calcifications of the dental follicle in regional odontodysplasia:
A structural and ultrastructural study. Oral Surg Oral Med Oral
Pathol. 56:396–404. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
155
|
Barbería E, Sanz Coarasa A, Hernández A
and Cardoso-Silva C: Regional odontodysplasia. A literature review
and three case reports. Eur J Paediatr Dent. 13:161–166.
2012.PubMed/NCBI
|
|
156
|
Mathew A, Dauravu LM, Reddy SN, Kumar KR
and Venkataramana V: Ghost teeth: Regional odontodysplasia of
maxillary first molar associated with eruption disorders in a
10-year-old girl. J Pharm Bioallied Sci. 7 (Suppl 2):S800–S803.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
157
|
Sapp JP and Gardner DG: Regional
odontodysplasia: An ultrastructural and histochemical study of the
soft-tissue calcifications. Oral Surg Oral Med Oral Pathol.
36:383–392. 1973. View Article : Google Scholar : PubMed/NCBI
|
|
158
|
Gomez RS, Silva EC, Silva-Filho EC and
Castro WH: Multiple calcifying hyperplastic dental follicles. J
Oral Pathol Med. 27:333–334. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
159
|
Gardner DG and Radden B: Multiple
calcifying hyperplastic dental follicles. Oral Surg Oral Med Oral
Pathol Oral Radiol Endod. 79:603–606. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
160
|
Jamshidi S, Zargaran M and Mohtasham N:
Multiple calcifying hyperplastic dental follicle (MCHDF): A case
report. J Dent Res Dent Clin Dent Prospects. 7:174–176.
2013.PubMed/NCBI
|
|
161
|
Rodrigues LG, da Silva VB, Carmelo JC,
Khouri MS, Mendes PA and Manzi FR: An imaging perspective to
multiple calcifying hyperplastic dental follicles-a report of three
cases. Ann Maxillofac Surg. 12:227–230. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
162
|
Ulutürk H, Yücel E, Akinci HO, Calisan EB,
Yildirim B and Gizli A: Multiple calcifying hyperplastic dental
follicles. J Stomatol Oral Maxillofac Surg. 120:77–79. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
163
|
Davari D, Arzhang E and Soltani P:
Multiple calcifying hyperplastic dental follicles: A case report. J
Oral Maxillofac Surg. 77:757–761. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
164
|
Fukuta Y, Totsuka M, Takeda Y and Yamamoto
H: Pathological study of the hyperplastic dental follicle. J Nihon
Univ Sch Dent. 33:166–173. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
165
|
Cho YA, Yoon HJ, Hong SP, Lee JI and Hong
SD: Multiple calcifying hyperplastic dental follicles: Comparison
with hyperplastic dental follicles. J Oral Pathol Med. 40:243–249.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
166
|
Hemeryck L, Hermans F, Chappell J,
Kobayashi H, Lambrechts D, Lambrichts I, Bronckaers A and
Vankelecom H: Organoids from human tooth showing epithelial
stemness phenotype and differentiation potential. Cell Mol Life
Sci. 79:1532022. View Article : Google Scholar : PubMed/NCBI
|
|
167
|
Hemeryck L, Lambrichts I, Bronckaers A and
Vankelecom H: Establishing organoids from human tooth as a powerful
tool toward mechanistic research and regenerative therapy. J Vis
Exp. 182:e636712022.PubMed/NCBI
|