|
1
|
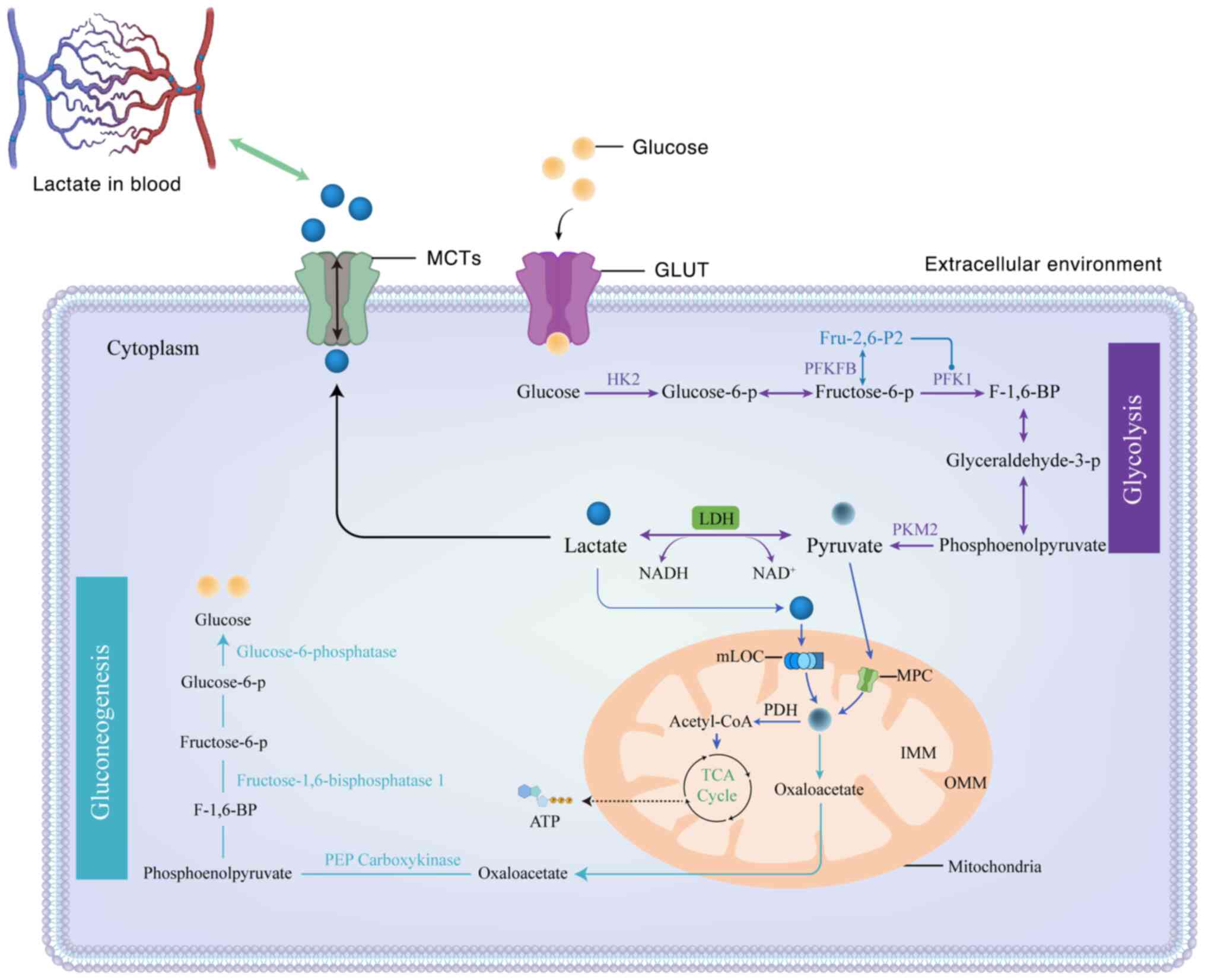
Yu XY, Sun Q, Zhang YM, Zou L and Zhao YY:
TGF-β/Smad signaling pathway in tubulointerstitial fibrosis. Front
Pharmacol. 13:8605882022. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zhao X, Kwan JYY, Yip K, Liu PP and Liu
FF: Targeting metabolic dysregulation for fibrosis therapy. Nat Rev
Drug Discovery. 19:57–75. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Vavřička J, Brož P, Follprecht D, Novák J
and Kroužecký A: Modern perspective of lactate metabolism. Physiol
Res. 73:499–514. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
4
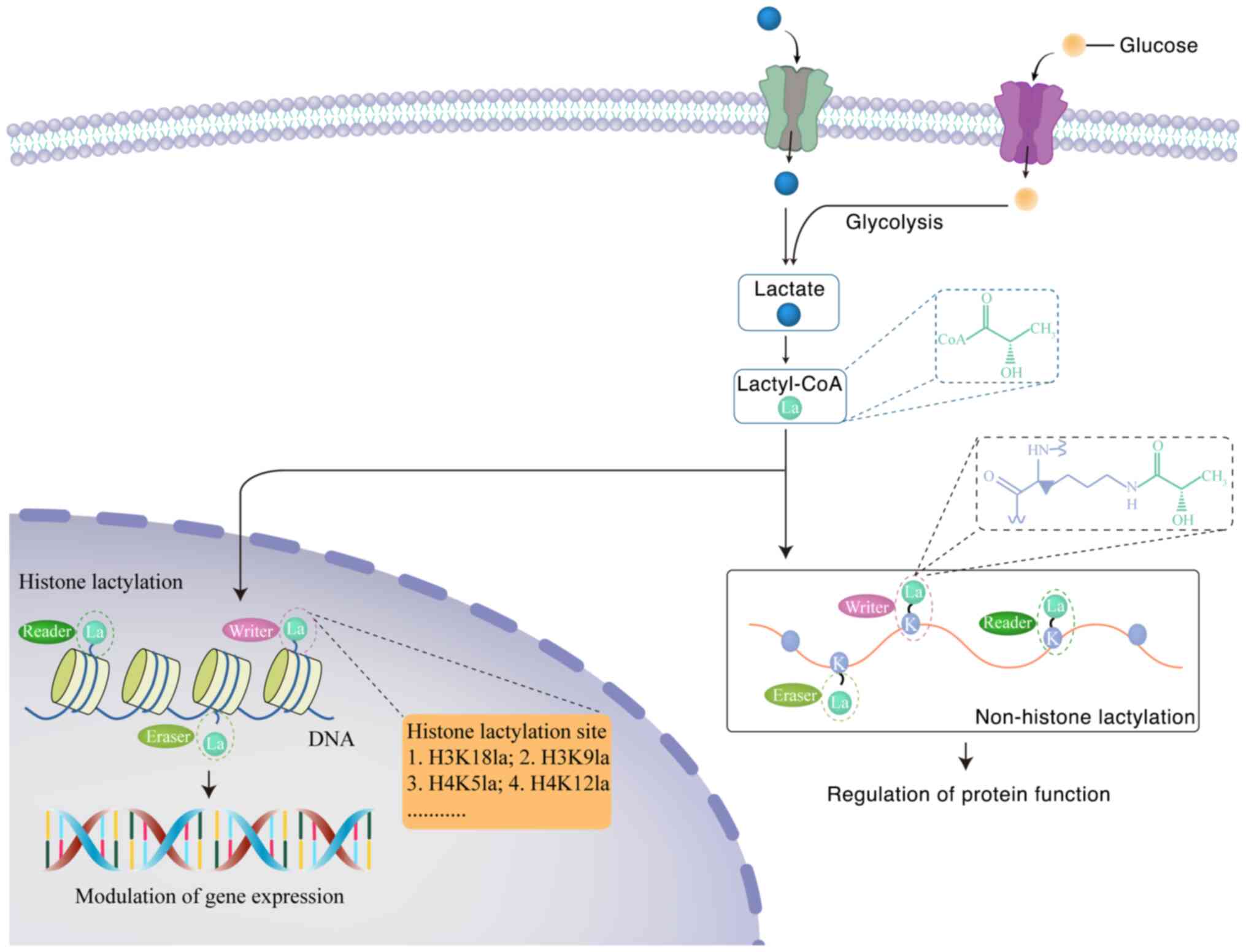
|
Rabinowitz JD and Enerbäck S: Lactate: The
ugly duckling of energy metabolism. Nat Metab. 2:566–571. 2020.
View Article : Google Scholar : PubMed/NCBI
|
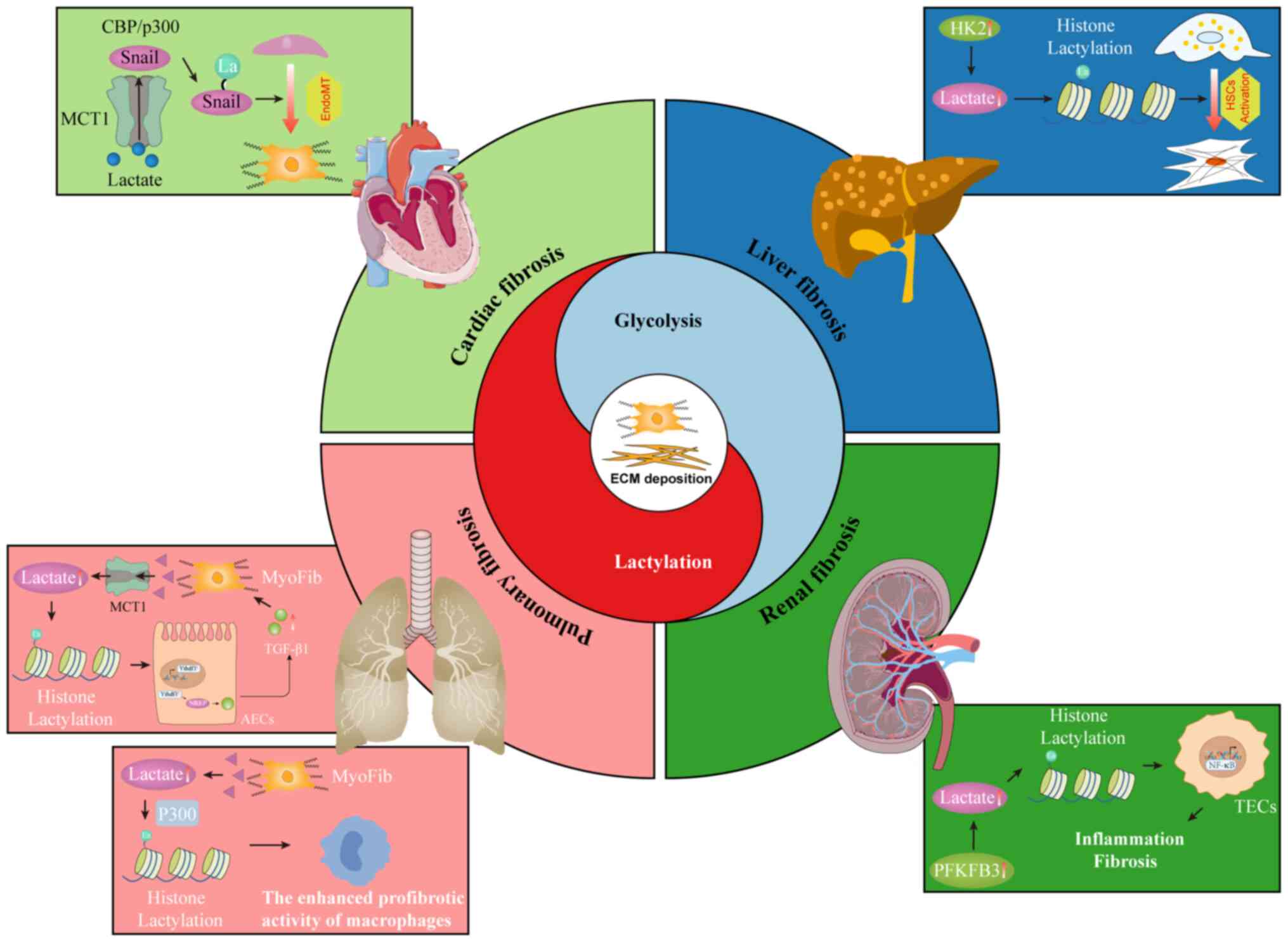
|
5
|
Ren LL, Miao H, Wang YN, Liu F, Li P and
Zhao YY: TGF-β as A master regulator of Aging-associated tissue
fibrosis. Aging Dis. 14:1633–1650. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Brooks GA: The science and translation of
lactate shuttle theory. Cell Metab. 27:757–785. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Miguel V, Alcalde-Estévez E, Sirera B,
Rodríguez-Pascual F and Lamas S: Metabolism and bioenergetics in
the pathophysiology of organ fibrosis. Free Radic Biol Med.
222:85–105. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Pucino V, Bombardieri M, Pitzalis C and
Mauro C: Lactate at the crossroads of metabolism, inflammation, and
autoimmunity. Eur J Immunol. 47:14–21. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Maciolek JA, Alex Pasternak J and Wilson
HL: Metabolism of activated T lymphocytes. Curr Opin Immunol.
27:60–74. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Li X, Yang Y, Zhang B, Lin X, Fu X, An Y,
Zou Y, Wang JX, Wang Z and Yu T: Lactate metabolism in human health
and disease. Signal Transduct Target Ther. 7:3052022. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Urbańska K and Orzechowski A:
Unappreciated role of LDHA and LDHB to control apoptosis and
autophagy in tumor cells. Int J Mol Sci. 20:20852019. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Dawson DM, Goodfriend TL and Kaplan NO and
Kaplan NO: Lactic Dehydrogenases: Functions of the two types: Rates
of synthesis of the two major forms can be correlated with
metabolic differentiation. Science. 143:929–933. 1964. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Martínez-Reyes I and Chandel NS:
Mitochondrial TCA cycle metabolites control physiology and disease.
Nat Commun. 11:1022020. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gray LR, Tompkins SC and Taylor EB:
Regulation of pyruvate metabolism and human disease. Cell Mol Life
Sci. 71:2577–2604. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Brooks GA, Arevalo JA, Osmond AD, Leija
RG, Curl CC and Tovar AP: Lactate in contemporary biology: A
phoenix Risen. J Physiol. 600:1229–1251. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Brooks GA: Lactate as a fulcrum of
metabolism. Redox Biol. 35:1014542020. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Brooks GA, Curl CC, Leija RG, Osmond AD,
Duong JJ and Arevalo JA: Tracing the lactate shuttle to the
mitochondrial reticulum. Exp Mol Med. 54:1332–1347. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Leija RG, Arevalo JA, Xing D,
Vázquez-Medina JP and Brooks GA: The mitochondrial lactate
oxidation complex: Endpoint for carbohydrate carbon disposal. Am J
Physiol Endocrinol Metab. 328:E126–E136. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zhu W, Guo S, Sun J, Zhao Y and Liu C:
Lactate and lactylation in cardiovascular diseases: Current
progress and future perspectives. Metabolis. 158:1559572024.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Stumvoll M, Meyer C, Mitrakou A, Nadkarni
V and Gerich JE: Renal glucose production and utilization: New
aspects in humans. Diabetologia. 40:749–757. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Li H, Ren Q, Shi M, Ma L and Fu P: Lactate
metabolism and acute kidney injury. Chin Med J (Engl). 138:916–924.
2025. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Jones R and Morris M: Monocarboxylate
transporters: Therapeutic targets and prognostic factors in
disease. Clin Pharmacol Ther. 100:454–463. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Zhang D, Tang Z, Huang H, Zhou G, Cui C,
Weng Y, Liu W, Kim S, Lee S, Perez-Neut M, et al: Metabolic
regulation of gene expression by histone lactylation. Nature.
574:575–580. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Xiong J, He J, Zhu J, Pan J, Liao W, Ye H,
Wang H, Song Y, Du Y, Cui B, et al: Lactylation-driven
METTL3-mediated RNA m6A modification promotes immunosuppression of
Tumor-infiltrating myeloid cells. Mol Cell. 82:1660–1677.e10. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Yang K, Fan M, Wang X, Xu J, Wang Y, Tu F,
Gill PS, Ha T, Liu L, Williams DL and Li C: Lactate promotes
macrophage HMGB1 lactylation, acetylation, and exosomal release in
polymicrobial sepsis. Cell Death Differ. 29:133–146. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Gaffney DO, Jennings EQ, Anderson CC,
Marentette JO, Shi T, Schou Oxvig AM, Streeter MD, Johannsen M,
Spiegel DA, Chapman E, et al: Non-enzymatic lysine lactoylation of
glycolytic enzymes. Cell Chem Biol. 27:206–213.e6. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Liu X, Zhang Y, Li W and Zhou X:
Lactylation, an emerging hallmark of metabolic reprogramming:
Current progress and open challenges. Front Cell Dev Biol.
10:9720202022. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Cui H, Xie N, Banerjee S, Ge J, Jiang D,
Dey T, Matthews QL, Liu RM and Liu G: Lung myofibroblasts promote
macrophage profibrotic activity through Lactate-induced histone
lactylation. Am J Respir Cell Mol Biol. 64:115–125. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Wei S, Gao Y, Dai X, Fu W, Cai S, Fang H,
Zeng Z and Chen Z: SIRT1-mediated HMGB1 deacetylation suppresses
sepsis-associated acute kidney injury. Am J Physiol Renal Physiol.
316:F20–F31. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Varner EL, Trefely S, Bartee D, von
Krusenstiern E, Izzo L, Bekeova C, O'Connor RS, Seifert EL, Wellen
KE, Meier JL and Snyder NW: Quantification of lactoyl-CoA
(lactyl-CoA) by liquid chromatography mass spectrometry in
mammalian cells and tissues. Open Biol. 10:2001872020. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Rabbani N, Xue M and Thornalley PJ:
Activity, regulation, copy number and function in the glyoxalase
system. Biochem Soc Trans. 42:419–424. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Allaman I, Bélanger M and Magistretti PJ:
Methylglyoxal, the dark side of glycolysis. Front Neurosci.
9:232015. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Trujillo MN, Jennings EQ, Hoffman EA,
Zhang H, Phoebe AM, Mastin GE, Kitamura N, Reisz JA, Megill E,
Kantner D, et al: Lactoylglutathione promotes inflammatory
signaling in macrophages through histone lactoylation. Mol Metab.
81:1018882024. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Dichtl S, Lindenthal L, Zeitler L, Behnke
K, Schlösser D, Strobl B, Scheller J, El Kasmi KC and Murray PJ:
Lactate and IL6 define separable paths of inflammatory metabolic
adaptation. Sci Adv. 7:eabg35052021. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Wang P, Xie D, Xiao T, Cheng C, Wang D,
Sun J, Wu M, Yang Y, Zhang A and Liu Q: H3K18 lactylation promotes
the progression of arsenite-related idiopathic pulmonary fibrosis
via YTHDF1/m6A/NREP. J Hazard Mater. 461:1325822024. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Aggarwal S, Wang Z, Rincon Fernandez
Pacheco D, Rinaldi A, Rajewski A, Callemeyn J, Van Loon E,
Lamarthée B, Covarrubias AE, Hou J, et al: SOX9 switch links
regeneration to fibrosis at the single-cell level in mammalian
kidneys. Science. 383:eadd63712024. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Wynn TA and Vannella KM: Macrophages in
tissue repair, regeneration, and fibrosis. Immunity. 44:450–462.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Marconi GD, Fonticoli L, Rajan TS,
Pierdomenico SD, Trubiani O, Pizzicannella J and Diomede F:
Epithelial-mesenchymal transition (EMT): The Type-2 EMT in wound
healing, tissue regeneration and organ fibrosis. Cells.
10:15872021. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Tang W and Wei Q: The metabolic pathway
regulation in kidney injury and repair. Front Physiol.
14:13442712024. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Richter K and Kietzmann T: Reactive oxygen
species and fibrosis: Further evidence of a significant liaison.
Cell Tissue Res. 365:591–605. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Feng L, Chen X, Huang Y, Zhang X, Zheng S
and Xie N: Immunometabolism changes in fibrosis: From mechanisms to
therapeutic strategies. Front Pharmacol. 14:12436752023. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Liu SS, Liu C, Lv XX, Cui B, Yan J, Li YX,
Li K, Hua F, Zhang XW, Yu JJ, et al: The chemokine CCL1 triggers an
AMFR-SPRY1 pathway that promotes differentiation of lung
fibroblasts into myofibroblasts and drives pulmonary fibrosis.
Immunity. 54:2042–2056.e8. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Chen S, Wang K, Fan Z, Zhou T, Li R, Zhang
B, Chen J, Chi J, Wei K, Liu J, et al: Modulation of anti-cardiac
fibrosis immune responses by changing M2 macrophages into M1
macrophages. Mol Med. 30:882024. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Weber KT, Sun Y, Bhattacharya SK, Ahokas
RA and Gerling IC: Myofibroblast-mediated mechanisms of
pathological remodelling of the heart. Nat Rev Cardiol. 10:15–26.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Segura AM, Frazier OH and Buja LM:
Fibrosis and heart failure. Heart Fail Rev. 19:173–185. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Li L, Zhao Q and Kong W: Extracellular
matrix remodeling and cardiac fibrosis. Matrix Biol. 68-69:490–506.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Disertori M, Masè M and Ravelli F:
Myocardial fibrosis predicts ventricular tachyarrhythmias. Trends
Cardiovasc Med. 27:363–372. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Liu M, López De Juan Abad B and Cheng K:
Cardiac fibrosis: Myofibroblast-mediated pathological regulation
and drug delivery strategies. Adv Drug Delivery Rev. 173:504–519.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Gibb AA, Lazaropoulos MP and Elrod JW:
Myofibroblasts and fibrosis: Mitochondrial and metabolic control of
cellular differentiation. Circ Res. 127:427–447. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Chen ZT, Gao QY, Wu MX, Wang M, Sun RL,
Jiang Y, Guo Q, Guo DC, Liu CY, Chen SX, et al: Glycolysis
inhibition alleviates cardiac fibrosis after myocardial infarction
by suppressing cardiac fibroblast activation. Front Cardiovasc Med.
8:7017452021. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Wang F, Yin X, Fan YM, Zhang X, Ma C, Jia
K, Zhou W, Tang Z, Qi LW and Li J: Upregulation of glycolytic
enzyme PFKFB3 by deubiquitinase OTUD4 promotes cardiac fibrosis
post myocardial infarction. J Mol Med. 101:743–756. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Zeng H, Pan T, Zhan M, Hailiwu R, Liu B,
Yang H and Li P: Suppression of PFKFB3-driven glycolysis restrains
endothelial-to-mesenchymal transition and fibrotic response. Signal
Transduct Target Ther. 7:3032022. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Wang Q, Donthi RV, Wang J, Lange AJ,
Watson LJ, Jones SP and Epstein PN: Cardiac phosphatase-deficient
6-phosphofructo-2-kinase/fructose-2,6-bisphosphatase increases
glycolysis, hypertrophy, and myocyte resistance to hypoxia. Am J
Physiol Heart Circ Physiol. 294:H2889–H2897. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Hailiwu R, Zeng H, Zhan M, Pan T, Yang H
and Li P: Salvianolic acid A diminishes LDHA-driven aerobic
glycolysis to restrain myofibroblasts activation and cardiac
fibrosis via blocking Akt/GSK-3β/HIF-1α axis. Phytother Res.
37:4540–4556. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Mao Q, Zhang X, Yang J, Kong Q, Cheng H,
Yu W, Cao X, Li Y, Li C, Liu L and Ding Z: HSPA12A acts as a
scaffolding protein to inhibit cardiac fibroblast activation and
cardiac fibrosis. J Adv Res. 67:217–229. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Chen ZT, Zhang HF, Wang M, Wang SH, Wen
ZZ, Gao QY, Wu MX, Liu WH, Xie Y, Mai JT, et al: Long non-coding
RNA Linc00092 inhibits cardiac fibroblast activation by altering
glycolysis in an ERK-dependent manner. Cell Signal. 74:1097082020.
View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Liu F, Chen Y, Qin D and Qian C:
Interleukin-22 inhibits cardiac fibrosis by regulating fibroblast
metabolic reprogramming in myocardial infarction. Pathol Res Pract.
256:1552562024. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Ji J, Qian L, Zhu Y, Jiang Y, Guo JQ, Wu
Y, Yang ZW, Yao YY and Ma GS: Kallistatin/Serpina3c inhibits
cardiac fibrosis after myocardial infarction by regulating
glycolysis via Nr4a1 activation. Biochim Biophys Acta Mol Basis
Dis. 1868:1664412022. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Yao S, Yang X, An J, Jin H, Wen G, Wang H
and Tuo B: Role of the S100 protein family in liver disease
(Review). Int J Mol Med. 48:1662021. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Roehlen N, Crouchet E and Baumert TF:
Liver fibrosis: Mechanistic concepts and therapeutic perspectives.
Cells. 9:8752020. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Dulai PS, Singh S, Patel J, Soni M, Prokop
LJ, Younossi Z, Sebastiani G, Ekstedt M, Hagstrom H, Nasr P, et al:
Increased risk of mortality by fibrosis stage in nonalcoholic fatty
liver disease: Systematic review and meta-analysis. Hepatology.
65:1557–1565. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Tan Z, Sun H, Xue T, Gan C, Liu H, Xie Y,
Yao Y and Ye T: Liver fibrosis: Therapeutic Targets and advances in
drug therapy. Front Cell Dev Biol. 9:7301762021. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Yao S, Chai H, Tao T, Zhang L, Yang X, Li
X, Yi Z, Wang Y, An J, Wen G, et al: Role of lactate and lactate
metabolism in liver diseases (Review). Int J Mol Med. 54:592024.
View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Mejias M, Gallego J, Naranjo-Suarez S,
Ramirez M, Pell N, Manzano A, Suñer C, Bartrons R, Mendez R and
Fernandez M: CPEB4 increases expression of PFKFB3 to induce
glycolysis and activate mouse and human hepatic stellate cells,
promoting liver fibrosis. Gastroenterology. 159:273–288. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Trivedi P, Wang S and Friedman SL: The
power of Plasticity-metabolic regulation of hepatic stellate cells.
Cell Metab. 33:242–257. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Chen Y, Choi SS, Michelotti GA, Chan IS,
Swiderska-Syn M, Karaca GF, Xie G, Moylan CA, Garibaldi F, Premont
R, et al: Hedgehog controls hepatic stellate cell fate by
regulating metabolism. Gastroenterology. 143:1319–1329.e11. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Zheng D, Jiang Y, Qu C, Yuan H, Hu K, He
L, Chen P, Li J, Tu M, Lin L, et al: Pyruvate kinase M2
tetramerization protects against hepatic stellate cell activation
and liver fibrosis. Am J Pathol. 190:2267–2281. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Rao J, Wang H, Ni M, Wang Z, Wang Z, Wei
S, Liu M, Wang P, Qiu J, Zhang L, et al: FSTL1 promotes liver
fibrosis by reprogramming macrophage function through modulating
the intracellular function of PKM2. Gut. 71:2539–2550. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Tu W, Ye J and Wang ZJ: Embryonic liver
fordin is involved in glucose glycolysis of hepatic stellate cell
by regulating PI3K/Akt signaling. World J Gastroenterol.
22:85192016. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Zhou MY, Cheng ML, Huang T, Hu RH, Zou GL,
Li H, Zhang BF, Zhu JJ, Liu YM, Liu Y and Zhao XK: Transforming
growth factor beta-1 upregulates glucose transporter 1 and
glycolysis through canonical and noncanonical pathways in hepatic
stellate cells. World J Gastroenterol. 27:6908–6926. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Wang F, Chen L, Kong D, Zhang X, Xia S,
Liang B, Li Y, Zhou Y, Zhang Z, Shao J, et al: Canonical Wnt
signaling promotes HSC glycolysis and liver fibrosis through an
LDH-A/HIF-1α transcriptional complex. Hepatology. 79:606–623. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Wu X, Shen Y, Meng Y, Chen J, Zhang Y,
Zeng S and Xu H: Suv39h1 contributes to activation of hepatic
stellate cells in non-alcoholic fatty liver disease by enabling
anaerobic glycolysis. Life Sci. 341:1224982024. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Huang T, Li YQ, Zhou MY, Hu RH, Zou GL, Li
JC, Feng S, Liu YM, Xin CQ and Zhao XK: Focal adhesion
kinase-related non-kinase ameliorates liver fibrosis by inhibiting
aerobic glycolysis via the FAK/Ras/c-myc/ENO1 pathway. World J
Gastroenterol. 28:123–139. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Xu L, Yang TY, Zhou YW, Wu MF, Shen J,
Cheng JL, Liu QX, Cao SY, Wang JQ and Zhang L: Bmal1 inhibits
phenotypic transformation of hepatic stellate cells in liver
fibrosis via IDH1/α-KG-mediated glycolysis. Acta Pharmacol Sin.
43:316–329. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Wan L, Xia T, Du Y, Liu J, Xie Y, Zhang Y,
Guan F, Wu J, Wang X and Shi C: Exosomes from activated hepatic
stellate cells contain GLUT1 and PKM2: A role for exosomes in
metabolic switch of liver nonparenchymal cells. FASEB J.
33:8530–8542. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Khanal S, Liu Y, Bamidele AO, Wixom AQ,
Washington AM, Jalan-Sakrikar N, Cooper SA, Vuckovic I, Zhang S,
Zhong J, et al: Glycolysis in hepatic stellate cells coordinates
fibrogenic extracellular vesicle release spatially to amplify liver
fibrosis. Sci Adv. 10:eadn52282024. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Lian N, Jin H, Zhang F, Wu L, Shao J, Lu Y
and Zheng S: Curcumin inhibits aerobic glycolysis in hepatic
stellate cells associated with activation of adenosine
monophosphate-activated protein kinase. IUBMB Life. 68:589–596.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Lian N, Jiang Y, Zhang F, Jin H, Lu C, Wu
X, Lu Y and Zheng S: Curcumin regulates cell fate and metabolism by
inhibiting hedgehog signaling in hepatic stellate cells. Lab
Invest. 95:790–803. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Wang F, Jia Y, Li M, Wang L, Shao J, Guo
Q, Tan S, Ding H, Chen A, Zhang F and Zheng S: Blockade of
glycolysis-dependent contraction by oroxylin a via inhibition of
lactate dehydrogenase-a in hepatic stellate cells. Cell Commun
Signal. 17:112019. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Ban D, Hua S, Zhang W, Shen C, Miao X and
Liu W: Costunolide reduces glycolysis-associated activation of
hepatic stellate cells via inhibition of hexokinase-2. Cell Mol
Biol Lett. 24:522019. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Gao W, Sun J, Wang F, Lu Y, Wen C, Bian Q
and Wu H: Deoxyelephantopin suppresses hepatic stellate cells
activation associated with inhibition of aerobic glycolysis via
hedgehog pathway. Biochem Biophys Res Commun. 516:1222–1228. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Bae M, Lee Y, Pham TX, Hu S, Park YK and
Lee JY: Astaxanthin inhibits the reduction of glycolysis during the
activation of hepatic stellate cells. Life Sci. 256:1179262020.
View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Bae M, Kim MB and Lee JY: Fucoxanthin
attenuates the reprogramming of energy metabolism during the
activation of hepatic stellate cells. Nutrients. 14:19022022.
View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Li Y, Zhou Y, Xia S, Chen L, Yang T, Zhao
D, Zhang Z, Shao J, Xu X, Zhang F and Zheng S: Blockade of
KLF5/LDH-A feedback loop contributes to Curcumol inhibition of
sinusoidal endothelial cell glycolysis and mitigation of liver
fibrosis. Phytomedicine. 114:1547592023. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Le CT, Nguyen G, Park SY, Dong HN, Cho YK,
Lee JH, Im SS, Choi DH and Cho EH: Phloretin ameliorates
succinate-induced liver fibrosis by regulating hepatic stellate
cells. Endocrinol Metab (Seoul). 38:395–405. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Chen X, Wang Y, Wan J, Dou X, Zhang C, Sun
M and Ye F: Quercetin alleviates liver fibrosis via regulating
glycolysis of liver sinusoidal endothelial cells and neutrophil
infiltration. Biomol Biomed. 24:1806–1815. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Rho H, Terry AR, Chronis C and Hay N:
Hexokinase 2-mediated gene expression via histone lactylation is
required for hepatic stellate cell activation and liver fibrosis.
Cell Metab. 35:1406–1423.e8. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Li J, Chen X, Song S, Jiang W, Geng T,
Wang T, Xu Y, Zhu Y, Lu J, Xia Y and Wang R: Hexokinase 2-mediated
metabolic stress and inflammation burden of liver macrophages via
histone lactylation in MASLD. Cell Rep. 44:1154652025. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Zhou Y, Yan J, Huang H, Liu L, Ren L, Hu
J, Jiang X, Zheng Y, Xu L, Zhong F and Li X: The m6A reader IGF2BP2
regulates glycolytic metabolism and mediates histone lactylation to
enhance hepatic stellate cell activation and liver fibrosis. Cell
Death Dis. 15:1892024. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Wu S, Li J and Zhan Y: H3K18 lactylation
accelerates liver fibrosis progression through facilitating SOX9
transcription. Exp Cell Res. 440:1141352024. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Tang F, Xiao D, Li X and Qiao L: The roles
of lactate and the interplay with m6A modification in diseases.
Cell Biol Toxicol. 40:1072024. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Chen W, Wang P, Xie Y, Xie D, Wang H, Bu
N, Lin J, Wu M, Xia H, Cheng C, et al: Histone
lactylation-augmented IRF4 is implicated in arsenite-induced liver
fibrosis via modulating Th17 cell differentiation. Chem Biol
Interact. 414:1115072025. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Kalantar-Zadeh K, Jafar TH, Nitsch D,
Neuen BL and Perkovic V: Chronic kidney disease. Lancet.
398:786–802. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Zhang Y, Zhang J, Feng D, Zhou H, Gui Z,
Zheng M, Hang Z, Wang Z, Wang Z, Gu M and Tan R:
IRF1/ZNF350/GPX4-mediated ferroptosis of renal tubular epithelial
cells promote chronic renal allograft interstitial fibrosis. Free
Radic Biol Med. 193:579–594. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Li J, Zou Y, Kantapan J, Su H, Wang L and
Dechsupa N: TGF-β/Smad signaling in chronic kidney disease:
Exploring post-translational regulatory perspectives (review). Mol
Med Rep. 30:1432024. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Ding H, Jiang L, Xu J, Bai F, Zhou Y, Yuan
Q, Luo J, Zen K and Yang J: Inhibiting aerobic glycolysis
suppresses renal interstitial fibroblast activation and renal
fibrosis. Am J Physiol Renal Physiol. 313:F561–F575. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Yin XN, Wang J, Cui LF and Fan WX:
Enhanced glycolysis in the process of renal fibrosis aggravated the
development of chronic kidney disease. Eur Rev Med Pharmacol Sci.
22:4243–4251. 2018.PubMed/NCBI
|
|
98
|
Wang C, Li Y, Yan S, Wang H, Shao X, Xiao
M, Yang B, Qin G, Kong R, Chen R and Zhang N: Interactome analysis
reveals that lncRNA HULC promotes aerobic glycolysis through LDHA
and PKM2. Nat Commun. 11:31622020. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Ashizawa K, Willingham MC, Liang CM and
Cheng SY: In vivo regulation of monomer-tetramer conversion. J Biol
Cem. 266:16842–16846. 1991.PubMed/NCBI
|
|
100
|
Liu H, Takagaki Y, Kumagai A, Kanasaki K
and Koya D: The PKM2 activator TEPP-46 suppresses kidney fibrosis
via inhibition of the EMT program and aberrant glycolysis
associated with suppression of HIF-1α accumulation. J Diabetes
Investig. 12:697–709. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Zhang Z, Deng X, Liu Y, Liu Y, Sun L and
Chen F: PKM2, function and expression and regulation. Cell Biosci.
9:522019. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Wang P, Sun C, Zhu T and Xu Y: Structural
insight into mechanisms for dynamic regulation of PKM2. Protein
Cell. 6:275–287. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Wei Q, Su J, Dong G, Zhang M, Huo Y and
Dong Z: Glycolysis inhibitors suppress renal interstitial fibrosis
via divergent effects on fibroblasts and tubular cells. Am J
Physiol Renal Physiol. 316:F1162–F1172. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Yu H, Zhu J, Chang L, Liang C, Li X and
Wang W: 3-Bromopyruvate decreased kidney fibrosis and fibroblast
activation by suppressing aerobic glycolysis in unilateral ureteral
obstruction mice model. Life Sci. 272:1192062021. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Lee M, Harley G, Katerelos M, Gleich K,
Sullivan MA, Laskowski A, Coughlan M, Fraser SA, Mount PF and Power
DA: Mutation of regulatory phosphorylation sites in PFKFB2 worsens
renal fibrosis. Sci Rep. 10:145312020. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Yang Q, Huo E, Cai Y, Zhang Z, Dong C,
Asara JM and Wei Q: PFKFB3-mediated glycolysis boosts fibroblast
activation and subsequent kidney fibrosis. Cells. 12:20812023.
View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Yang Q, Huo E, Cai Y, Zhang Z, Dong C,
Asara JM, Shi H and Wei Q: Myeloid PFKFB3-mediated glycolysis
promotes kidney fibrosis. Front Immunol. 14:12594342023. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Wang Y, Li H, Jiang S, Fu D, Lu X, Lu M,
Li Y, Luo D, Wu K, Xu Y, et al: The glycolytic enzyme PFKFB3 drives
kidney fibrosis through promoting histone lactylation-mediated
NF-κB family activation. Kidney Int. 106:226–240. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Srivastava SP, Li J, Kitada M, Fujita H,
Yamada Y, Goodwin JE, Kanasaki K and Koya D: SIRT3 deficiency leads
to induction of abnormal glycolysis in diabetic kidney with
fibrosis. Cell Death Dis. 9:9972018. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Zhang Y, Wen P, Luo J, Ding H, Cao H, He
W, Zen K, Zhou Y, Yang J and Jiang L: Sirtuin 3 regulates
mitochondrial protein acetylation and metabolism in tubular
epithelial cells during renal fibrosis. Cell Death Dis. 12:8472021.
View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Tang S, Huang T, Jing H, Huang Z, Chen H,
Fan Y, Zhong J and Zhou J: Aldehyde dehydrogenase-2 acts as a
potential genetic target for renal fibrosis. Life Sci.
239:1170152019. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Li SY, Tsai MT, Kuo YM, Yang HM, Tong ZJ,
Cheng HW, Lin CC and Wang HT: Aldehyde dehydrogenase 2 preserves
kidney function by countering acrolein-induced metabolic and
mitochondrial dysfunction. JCI Insight. 9:e1798712024. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Cao H, Luo J, Zhang Y, Mao X, Wen P, Ding
H, Xu J, Sun Q, He W, Dai C, et al: Tuberous sclerosis 1 (Tsc1)
mediated mTORC1 activation promotes glycolysis in tubular
epithelial cells in kidney fibrosis. Kidney Int. 98:686–698. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Li L, Galichon P, Xiao X, Figueroa-Ramirez
AC, Tamayo D, Lee JJ, Kalocsay M, Gonzalez-Sanchez D, Chancay MS,
McCracken KW, et al: Orphan nuclear receptor COUP-TFII enhances
myofibroblast glycolysis leading to kidney fibrosis. EMBO Rep.
22:e511692021. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Cui X, Shi E, Li J, Li Y, Qiao Z, Wang Z,
Liu M, Tang W, Sun Y, Zhang Y, et al: GPR87 promotes renal
tubulointerstitial fibrosis by accelerating glycolysis and
mitochondrial injury. Free Radic Biol Med. 189:58–70. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Li X, Ma TK, Wang M, Zhang XD, Liu TY, Liu
Y, Huang ZH, Zhu YH, Zhang S, Yin L, et al: YY1-induced
upregulation of LncRNA-ARAP1-AS2 and ARAP1 promotes diabetic kidney
fibrosis via aberrant glycolysis associated with EGFR/PKM2/HIF-1α
pathway. Front Pharmacol. 14:10693482023. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Yang S, Wu H, Li Y, Li L, Xiang J, Kang L,
Yang G and Liang Z: Inhibition of PFKP in renal tubular epithelial
cell restrains TGF-β induced glycolysis and renal fibrosis. Cell
Death Dis. 14:8162023. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Zhang L, Tian M, Zhang M, Li C, Wang X,
Long Y, Wang Y, Hu J, Chen C, Chen X, et al: Forkhead box Protein
K1 promotes chronic kidney disease by driving glycolysis in tubular
epithelial cells. Adv Sci. 24053252024. View Article : Google Scholar
|
|
119
|
Jiang A, Liu J, Wang Y and Zhang C:
cGAS-STING signaling pathway promotes hypoxia-induced renal
fibrosis by regulating PFKFB3-mediated glycolysis. Free Radic Biol
Med. 208:516–529. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Hu D, Wang L, Zhang Y, Liu X, Lu Z and Li
H: Sanqi oral solution ameliorates renal fibrosis by suppressing
fibroblast activation via HIF-1α/PKM2/glycolysis pathway in chronic
kidney disease. J Ethnopharmacol. 335:1186792024. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Cai T, Ke Q, Fang Y, Wen P, Chen H, Yuan
Q, Luo J, Zhang Y, Sun Q, Lv Y, et al: Sodium-glucose cotransporter
2 inhibition suppresses HIF-1α-mediated metabolic switch from lipid
oxidation to glycolysis in kidney tubule cells of diabetic mice.
Cell Death Dis. 11:3902020. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Huang X, Gao L, Deng R, Peng Y, Wu S, Lu J
and Liu X: Huangqi-Danshen decoction reshapes renal glucose
metabolism profiles that delays chronic kidney disease progression.
Biomed Pharmacother. 164:1149892023. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Wang L, Feng X, Ye C, Wang C and Wang M:
Shen Shuai II Recipe inhibits hypoxia-induced glycolysis by
preserving mitochondrial dynamics to attenuate kidney fibrosis. J
Ethnopharmacol. 308:1162712023. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Xie N, Tan Z, Banerjee S, Cui H, Ge J, Liu
RM, Bernard K, Thannickal VJ and Liu G: Glycolytic reprogramming in
myofibroblast differentiation and lung fibrosis. Am J Respir Crit
Care Med. 192:1462–1474. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Kang YP, Lee SB, Lee J, Kim HM, Hong JY,
Lee WJ, Choi CW, Shin HK, Kim DJ, Koh ES, et al: Metabolic
profiling regarding pathogenesis of idiopathic pulmonary fibrosis.
J Proteome Res. 15:1717–1724. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Zhao YD, Yin L, Archer S, Lu C, Zhao G,
Yao Y, Wu L, Hsin M, Waddell TK, Keshavjee S, et al: Metabolic
heterogeneity of idiopathic pulmonary fibrosis: A metabolomic
study. BMJ Open Respir Res. 4:e0001832017. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Cho SJ, Moon JS, Lee CM, Choi AMK and
Stout-Delgado HW: Glucose Transporter 1-Dependent glycolysis is
increased during Aging-Related lung fibrosis, and phloretin
inhibits lung fibrosis. Am J Respir Cell Mol Biol. 56:521–531.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Kim SH, Jin JA, So HJ, Lee SH, Kang TW,
Lee JU, Choi DE, Jeong JY, Chang YK, Choi H, et al: Urine-derived
stem Cell-secreted klotho plays a crucial role in the HK-2 fibrosis
model by inhibiting the TGF-β signaling pathway. Int J Mol Sci.
23:50122022. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Yin X, Choudhury M, Kang JH, Schaefbauer
KJ, Jung MY, Andrianifahanana M, Hernandez DM and Leof EB:
Hexokinase 2 couples glycolysis with the profibrotic actions of
TGF-β. Sci Signal. 12:eaax40672019. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Hu X, Xu Q, Wan H, Hu Y, Xing S, Yang H,
Gao Y and He Z: PI3K-Akt-mTOR/PFKFB3 pathway mediated lung
fibroblast aerobic glycolysis and collagen synthesis in
lipopolysaccharide-induced pulmonary fibrosis. Lab Invest.
100:801–811. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Tang CJ, Xu J, Ye HY and Wang XB:
Metformin prevents PFKFB3-related aerobic glycolysis from enhancing
collagen synthesis in lung fibroblasts by regulating AMPK/mTOR
pathway. Exp Ther Med. 21:5812021. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Chen W, Zhang J, Zhong W, Liu Y, Lu Y,
Zeng Z, Huang H, Wan X, Meng X, Zou F, et al: Anlotinib Inhibits
PFKFB3-Driven glycolysis in myofibroblasts to reverse pulmonary
fibrosis. Front Pharmacol. 12:7448262021. View Article : Google Scholar : PubMed/NCBI
|
|
133
|
O'Leary EM, Tian Y, Nigdelioglu R, Witt
LJ, Cetin-Atalay R, Meliton AY, Woods PS, Kimmig LM, Sun KA, Gökalp
GA, et al: TGF-β promotes metabolic reprogramming in lung
fibroblasts via mTORC1-dependent ATF4 activation. Am J Respir Cell
Mol Biol. 63:601–612. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Xu J, Li J, Yu Z, Rao H, Wang S and Lan H:
HMGB1 promotes HLF-1 proliferation and ECM production through
activating HIF1-α-regulated aerobic glycolysis. Pulm Pharmacol
Ther. 45:136–141. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Goodwin J, Choi H, Hsieh M, Neugent ML,
Ahn JM, Hayenga HN, Singh PK, Shackelford DB, Lee IK, Shulaev V, et
al: Targeting Hypoxia-Inducible Factor-1α/Pyruvate Dehydrogenase
Kinase 1 Axis by dichloroacetate suppresses bleomycin-induced
pulmonary fibrosis. Am J Respir Cell Mol Biol. 58:216–231. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Sun Z, Ji Z, He W, Duan R, Qu J and Yu G:
Lactate accumulation induced by Akt2-PDK1 signaling promotes
pulmonary fibrosis. FASEB J. 38:e234262024. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Schruf E, Schroeder V, Kuttruff CA, Weigle
S, Krell M, Benz M, Bretschneider T, Holweg A, Schuler M, Frick M,
et al: Human lung fibroblast-to-myofibroblast transformation is not
driven by an LDH5-dependent metabolic shift towards aerobic
glycolysis. Respir Res. 20:872019. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Mei S, Xu Q, Hu Y, Tang R, Feng J, Zhou Y,
Xing S, Gao Y and He Z: Integrin β3-PKM2 pathway-mediated aerobic
glycolysis contributes to mechanical ventilation-induced pulmonary
fibrosis. Theranostics. 12:6057–6068. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Wang L, Xu K, Wang N, Ding L, Zhao W, Wan
R, Zhao W, Guo X, Pan X, Yang J, et al: Fenbendazole attenuates
Bleomycin-induced pulmonary fibrosis in mice via suppression of
Fibroblast-to-myofibroblast differentiation. Int J Mol Sci.
23:140882022. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Wang W, Zhang Y, Huang W, Yuan Y, Hong Q,
Xie Z, Li L, Chen Y, Li X and Meng Y: Alamandine/MrgD axis prevents
TGF-β1-mediated fibroblast activation via regulation of aerobic
glycolysis and mitophagy. J Transl Med. 21:242023. View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Lai X, Huang S, Lin Y, Qiu Y, Pu L, Lin S,
Zeng Q, Huang W and Wang Z: DACT2 protects against pulmonary
fibrosis via suppressing glycolysis in lung myofibroblasts. Int J
Biol Macromol. 226:291–300. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
142
|
Li J, Zeng G, Zhang Z, Wang Y, Shao M, Li
C, Lu Z, Zhao Y, Zhang F and Ding W: Urban airborne PM2.5 induces
pulmonary fibrosis through triggering glycolysis and subsequent
modification of histone lactylation in macrophages. Ecotoxicol
Environ Saf. 273:1161622024. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Feng J, Zhong H, Mei S, Tang R, Zhou Y,
Xing S, Gao Y, Xu Q and He Z: LPS-induced monocarboxylate
transporter-1 inhibition facilitates lactate accumulation
triggering epithelial-mesenchymal transformation and pulmonary
fibrosis. Cell Mol Life Sci. 81:2062024. View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Gopu V, Fan L, Shetty RS, Nagaraja MR and
Shetty S: Caveolin-1 scaffolding domain peptide regulates glucose
metabolism in lung fibrosis. JCI Insight. 5:e1379692020. View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Trivlidis J, Aloufi N, Al-Habeeb F, Nair
P, Azuelos I, Eidelman DH and Baglole CJ: HuR drives lung
fibroblast differentiation but not metabolic reprogramming in
response to TGF-β and hypoxia. Respir Res. 22:3232021. View Article : Google Scholar : PubMed/NCBI
|
|
146
|
Xia Y, Wang Y, Xiong Q, He J, Wang H,
Islam M, Zhou X, Kim A, Zhang H, Huang H and Tsung A: Neutrophil
extracellular traps promote MASH fibrosis by metabolic
reprogramming of HSC. Hepatology. 81:947–961. 2025. View Article : Google Scholar : PubMed/NCBI
|