|
1
|
Barbhaiya M, Zuily S, Naden R, Hendry A,
Manneville F, Amigo MC, Amoura Z, Andrade D, Andreoli L, Artim-Esen
B, et al: 2023 ACR/EULAR antiphospholipid syndrome classification
criteria. Ann Rheum Dis. 82:1258–1270. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Radic M and Pattanaik D: Cellular and
molecular mechanisms of anti-phospholipid syndrome. Front Immunol.
9:9692018. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Knight JS and Kanthi Y: Mechanisms of
immunothrombosis and vasculopathy in antiphospholipid syndrome.
Semin Immunopathol. 44:347–362. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hernández-Molina G, González-Pérez I,
Pacheco-Molina C and Cabral AR: Quality of life in patients with
antiphospholipid syndrome is related to disease burden and
anticoagulant therapy. Int J Rheum Dis. 20:755–759. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chighizola CB, Crisafulli F, Hoxha A,
Carubbi F, Bellan M, Monti S, Costa L, Baldi C, Radin M, Praino E,
et al: Psychosocial burden in young patients with primary
anti-phospholipid syndrome: An Italian nationwide survey (The
AQUEOUS study). Clin Exp Rheumatol. 39:938–946. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Velásquez M, Peláez LF, Rojas M,
Narváez-Sánchez R, Velásquez JA, Escudero C, San Martín S and
Cadavid ÁP: Differences in endothelial activation and dysfunction
induced by antiphospholipid antibodies among groups of patients
with thrombotic, refractory, and non-refractory antiphospholipid
syndrome. Front Physiol. 12:7647022021. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Redecha P, Tilley R, Tencati M, Salmon JE,
Kirchhofer D, Mackman N and Girardi G: Tissue factor: A link
between C5a and neutrophil activation in antiphospholipid antibody
induced fetal injury. Blood. 110:2423–2431. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Salmon JE and Girardi G: Antiphospholipid
antibodies and pregnancy loss: A disorder of inflammation. J Reprod
Immunol. 77:51–56. 2008. View Article : Google Scholar : PubMed/NCBI
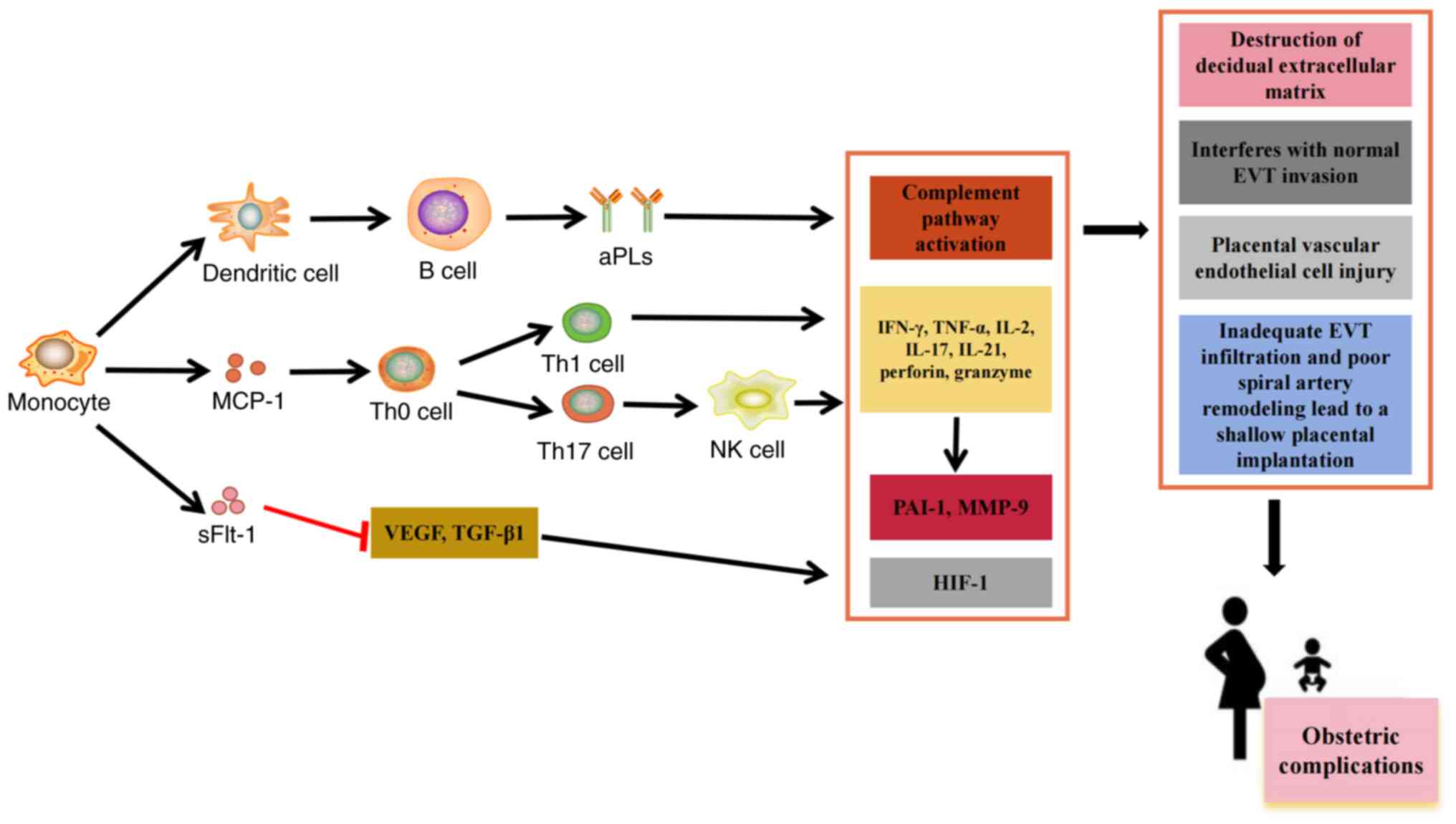
|
|
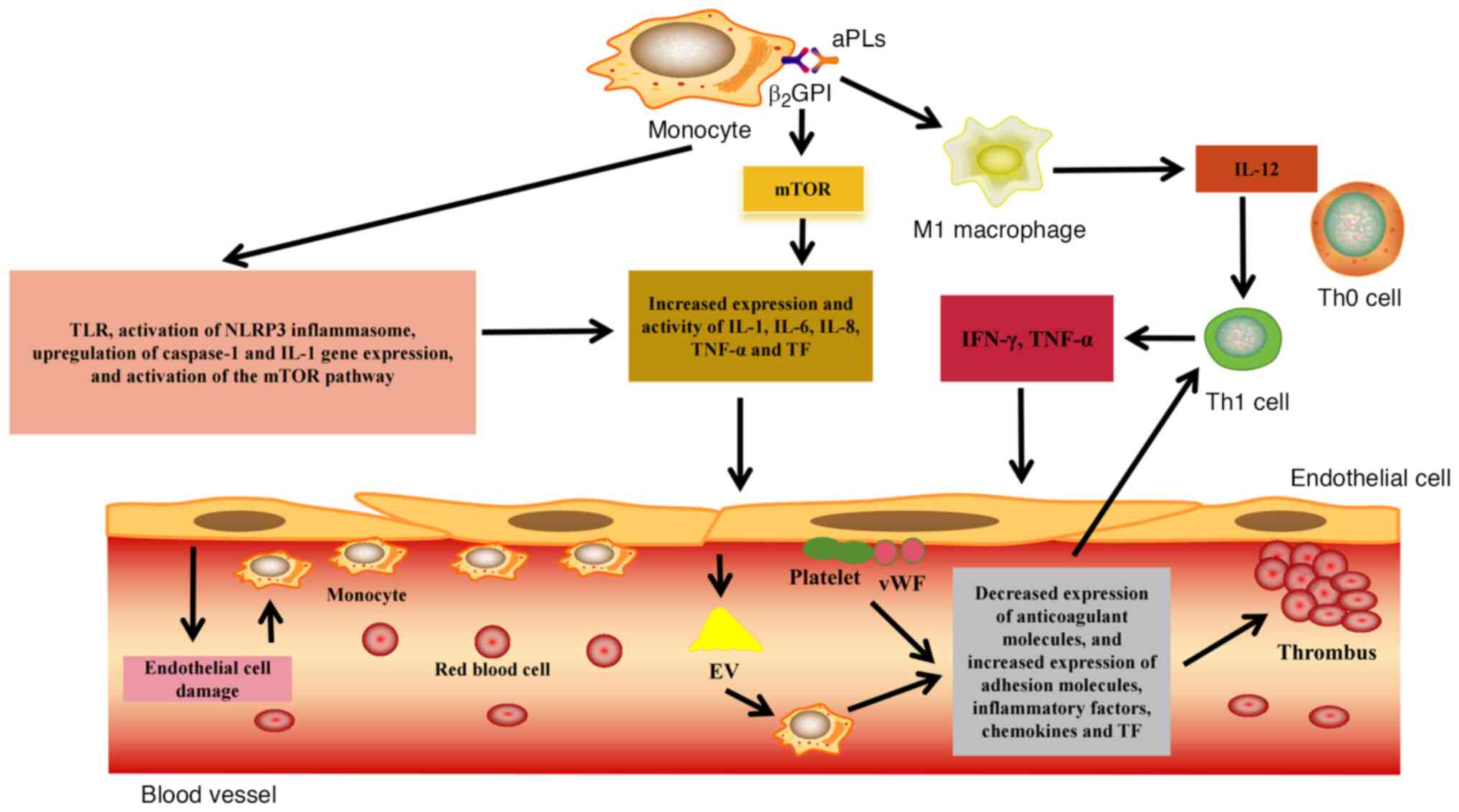
9
|
Proulle V, Furie RA, Merrill-Skoloff G,
Furie BC and Furie B: Platelets are required for enhanced
activation of the endothelium and fibrinogen in a mouse thrombosis
model of APS. Blood. 124:611–622. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wahl D, Membre A, Perret-Guillaume C,
Regnault V and Lecompte T: Mechanisms of antiphospholipid-induced
thrombosis: Effects on the protein C system. Curr Rheumatol Rep.
11:77–81. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bu C, Gao L, Xie W, Zhang J, He Y, Cai G
and McCrae KR: beta2-glycoprotein i is a cofactor for tissue
plasminogen activator-mediated plasminogen activation. Arthritis
Rheum. 60:559–568. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Yalavarthi S, Gould TJ, Rao AN, Mazza LF,
Morris AE, Núñez-Álvarez C, Hernández-Ramírez D, Bockenstedt PL,
Liaw PC, Cabral AR and Knight JS: Release of neutrophil
extracellular traps by neutrophils stimulated with antiphospholipid
antibodies: A newly identified mechanism of thrombosis in the
antiphospholipid syndrome. Arthritis Rheumatol. 67:2990–3003. 2015.
View Article : Google Scholar : PubMed/NCBI
|
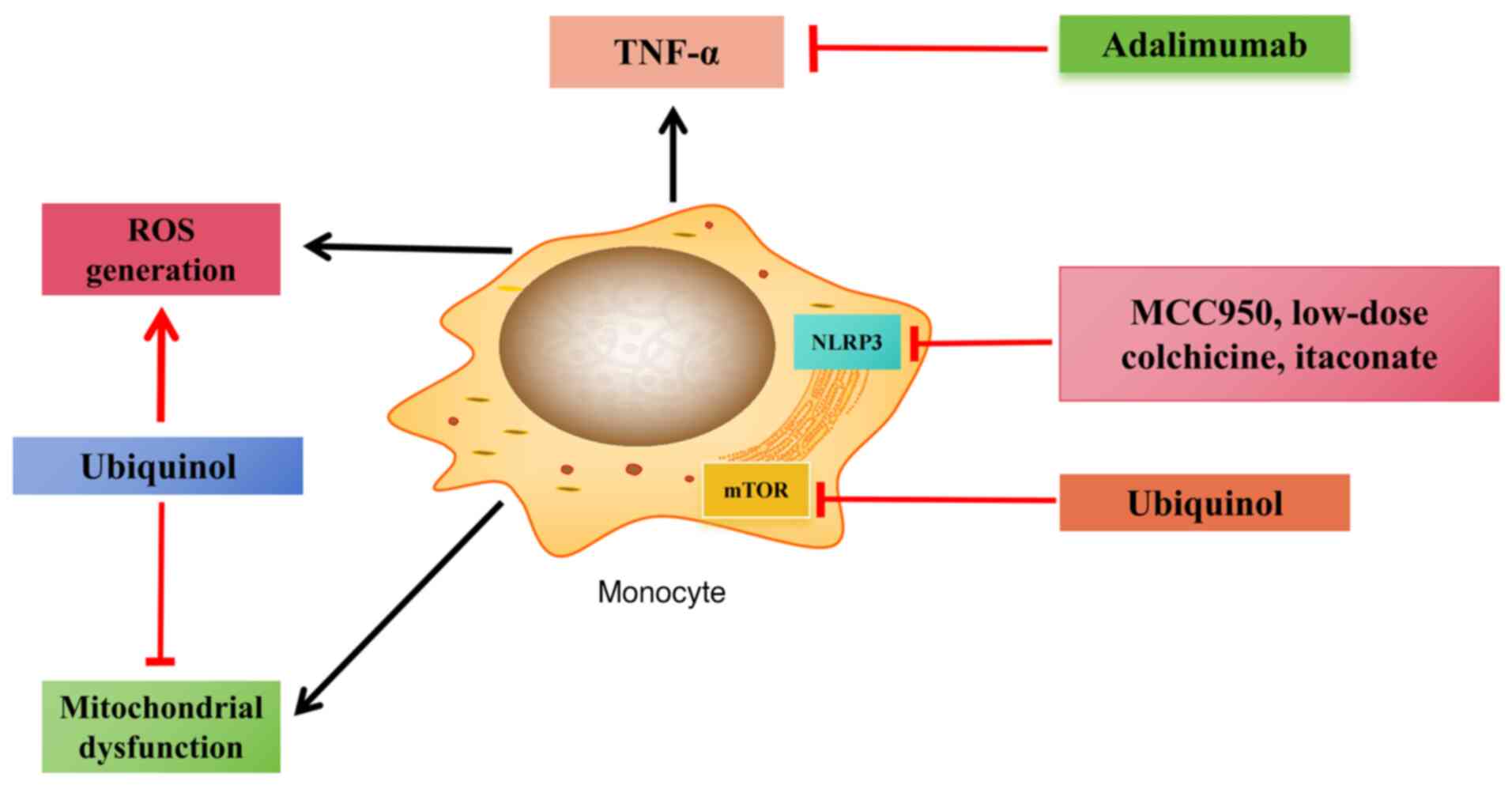
|
13
|
Kuwana M: Beta2-glycoprotein I:
Antiphospholipid syndrome and T-cell reactivity. Thromb Res.
114:347–355. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chaturvedi S, Alluri R and McCrae KR:
Extracellular vesicles in the antiphospholipid syndrome. Semin
Thromb Hemost. 44:493–504. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Rand JH, Wu XX, Guller S, Gil J, Guha A,
Scher J and Lockwood CJ: Reduction of annexin-V (placental
anticoagulant protein-I) on placental villi of women with
antiphospholipid antibodies and recurrent spontaneous abortion. Am
J Obstet Gynecol. 171:1566–1572. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Doğan Z, Bektaşoğlu G, Dümür Ş, Uzun H,
Erden İ and Yurtdaş M: Evaluation of the relationship between
monocyte to high-density lipoprotein cholesterol ratio and thrombus
burden in patients with deep vein thrombosis. Rev Assoc Med Bras
(1992). 69:e202212112023. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Chen P, Zhou L, Chen J, Lu Y, Cao C, Lv S,
Wei Z, Wang L, Chen J, Hu X, et al: The immune atlas of human
deciduas with unexplained recurrent pregnancy loss. Front Immunol.
12:6890192021. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Oku K, Amengual O and Atsumi T:
Pathophysiology of thrombosis and pregnancy morbidity in the
antiphospholipid syndrome. Eur J Clin Invest. 42:1126–1135. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Xourgia E and Tektonidou MG: An update on
antiphospholipid syndrome. Curr Rheumatol Rep. 23:842022.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Dabit JY, Valenzuela-Almada MO,
Vallejo-Ramos S and Duarte-García A: Epidemiology of
antiphospholipid syndrome in the general population. Curr Rheumatol
Rep. 23:852022. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hwang JJ, Shin SH, Kim YJ, Oh YM, Lee SD,
Kim YH, Choi CW and Lee JS: Epidemiology of antiphospholipid
syndrome in Korea: A nationwide population-based study. J Korean
Med Sci. 35:e352020. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Radin M, Sciascia S, Bazzan M, Bertero T,
Carignola R, Montabone E, Montaruli B, Vaccarino A, Cecchi I,
Rubini E, et al: Antiphospholipid syndrome is still a rare
disease-estimated prevalence in the piedmont and aosta valley
regions of northwest Italy: Comment on the article by Duarte-García
et al. Arthritis Rheumatol. 72:1774–1776. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Duarte-García A, Pham MM, Crowson CS, Amin
S, Moder KG, Pruthi RK, Warrington KJ and Matteson EL: The
epidemiology of antiphospholipid syndrome: A population-based
study. Arthritis Rheumatol. 71:1545–1552. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Petri M: Antiphospholipid syndrome. Transl
Res. 225:70–81. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Cervera R, Serrano R, Pons-Estel GJ,
Ceberio-Hualde L, Shoenfeld Y, de Ramón E, Buonaiuto V, Jacobsen S,
Zeher MM, Tarr T, et al: Morbidity and mortality in the
antiphospholipid syndrome during a 10-year period: A multicentre
prospective study of 1000 patients. Ann Rheum Dis. 74:1011–1018.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
D'Ippolito S, Barbaro G, Paciullo C,
Tersigni C, Scambia G and Di Simone N: Antiphospholipid syndrome in
pregnancy: New and old pathogenetic mechanisms. Int J Mol Sci.
24:31952023. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Turrent-Carriles A, Herrera-Félix JP and
Amigo MC: Renal involvement in antiphospholipid syndrome. Front
Immunol. 9:10082018. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Abreu MM, Danowski A, Wahl DG, Amigo MC,
Tektonidou M, Pacheco MS, Fleming N, Domingues V, Sciascia S, Lyra
JO, et al: The relevance of ‘non-criteria’ clinical manifestations
of antiphospholipid syndrome: 14th international congress on
antiphospholipid antibodies technical task force report on
antiphospholipid syndrome clinical features. Autoimmun Rev.
14:401–414. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Pignatelli P, Ettorre E, Menichelli D,
Pani A, Violi F and Pastori D: Seronegative antiphospholipid
syndrome: Refining the value of ‘non-criteria’ antibodies for
diagnosis and clinical management. Haematologica. 105:562–572.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Miyakis S, Lockshin MD, Atsumi T, Branch
DW, Brey RL, Cervera R, Derksen RH, DE Groot PG, Koike T, Meroni
PL, et al: International consensus statement on an update of the
classification criteria for definite antiphospholipid syndrome
(APS). J Thromb Haemost. 4:295–306. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Asherson RA, Cervera R, de Groot PG, Erkan
D, Boffa MC, Piette JC, Khamashta MA and Shoenfeld Y; Catastrophic
Antiphospholipid Syndrome Registry Project Group, : Catastrophic
antiphospholipid syndrome: International consensus statement on
classification criteria and treatment guidelines. Lupus.
12:530–534. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Auffray C, Sieweke MH and Geissmann F:
Blood monocytes: Development, heterogeneity, and relationship with
dendritic cells. Annu Rev Immunol. 27:669–692. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Ziegler-Heitbrock L: Blood monocytes and
their subsets: Established features and open questions. Front
Immunol. 6:4232015. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Kzhyshkowska J, Gudima A, Moganti K,
Gratchev A and Orekhov A: Perspectives for
monocyte/macrophage-based diagnostics of chronic inflammation.
Transfus Med Hemother. 43:66–77. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Geissmann F, Manz MG, Jung S, Sieweke MH,
Merad M and Ley K: Development of monocytes, macrophages, and
dendritic cells. Science. 327:656–561. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Dash SP, Gupta S and Sarangi PP: Monocytes
and macrophages: Origin, homing, differentiation, and functionality
during inflammation. Heliyon. 10:e296862024. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Cormican S and Griffin MD: Human monocyte
subset distinctions and function: Insights from gene expression
analysis. Front Immunol. 11:10702020. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Ziegler-Heitbrock L, Ancuta P, Crowe S,
Dalod M, Grau V, Hart DN, Leenen PJ, Liu YJ, MacPherson G, Randolph
GJ, et al: Nomenclature of monocytes and dendritic cells in blood.
Blood. 116:e74–e80. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Wong KL, Yeap WH, Tai JJ, Ong SM, Dang TM
and Wong SC: The three human monocyte subsets: Implications for
health and disease. Immunol Res. 53:41–57. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Medrano-Bosch M, Simón-Codina B, Jiménez
W, Edelman ER and Melgar-Lesmes P: Monocyte-endothelial cell
interactions in vascular and tissue remodeling. Front Immunol.
14:11960332023. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Wong KL, Tai JJ, Wong WC, Han H, Sem X,
Yeap WH, Kourilsky P and Wong SC: Gene expression profiling reveals
the defining features of the classical, intermediate, and
nonclassical human monocyte subsets. Blood. 118:e16–e31. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Cros J, Cagnard N, Woollard K, Patey N,
Zhang SY, Senechal B, Puel A, Biswas SK, Moshous D, Picard C, et
al: Human CD14dim monocytes patrol and sense nucleic acids and
viruses via TLR7 and TLR8 receptors. Immunity. 33:375–386. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Štok U, Štucin N, Blokar E, Ambrožič A,
Sodin-Šemrl S, Čučnik S and Žigon P: Antiphospholipid antibody
syndrome-associated increased surface expression of VLA4 integrin
on human monocytes. Biomedicines. 10:23412022. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Mandel J, Casari M, Stepanyan M, Martyanov
A and Deppermann C: Beyond hemostasis: Platelet innate immune
interactions and thromboinflammation. Int J Mol Sci. 23:38682022.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Hui H, Fuller KA, Erber WN and Linden MD:
Imaging flow cytometry in the assessment of leukocyte-platelet
aggregates. Methods. 112:46–54. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Gawaz MP, Loftus JC, Bajt ML, Frojmovic
MM, Plow EF and Ginsberg MH: Ligand bridging mediates integrin
alpha IIb beta 3 (platelet GPIIB-IIIA) dependent homotypic and
heterotypic cell-cell interactions. J Clin Invest. 88:1128–1134.
1991. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Silverstein RL, Asch AS and Nachman RL:
Glycoprotein IV mediates thrombospondin-dependent platelet-monocyte
and platelet-U937 cell adhesion. J Clin Invest. 84:546–552. 1989.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Han Z, Liu Q, Li H, Zhang M, You L, Lin Y,
Wang K, Gou Q, Wang Z, Zhou S, et al: The role of monocytes in
thrombotic diseases: A review. Front Cardiovasc Med.
10:11138272023. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
von Hundelshausen P, Weber KS, Huo Y,
Proudfoot AE, Nelson PJ, Ley K and Weber C: RANTES deposition by
platelets triggers monocyte arrest on inflamed and atherosclerotic
endothelium. Circulation. 103:1772–1777. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Moore KL, Stults NL, Diaz S, Smith DF,
Cummings RD, Varki A and McEver RP: Identification of a specific
glycoprotein ligand for P-selectin (CD62) on myeloid cells. J Cell
Biol. 118:445–456. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Ivanov II, Apta BHR, Bonna AM and Harper
MT: Platelet P-selectin triggers rapid surface exposure of tissue
factor in monocytes. Sci Rep. 9:133972019. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Purdy M, Obi A, Myers D and Wakefield T:
P- and E-selectin in venous thrombosis and non-venous pathologies.
J Thromb Haemost. 20:1056–1066. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Maugeri N, Brambilla M, Camera M, Carbone
A, Tremoli E, Donati MB, de Gaetano G and Cerletti C: Human
polymorphonuclear leukocytes produce and express functional tissue
factor upon stimulation. J Thromb Haemost. 4:1323–1330. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Hottz ED, Martins-Gonçalves R, Palhinha L,
Azevedo-Quintanilha IG, de Campos MM, Sacramento CQ, Temerozo JR,
Soares VC, Dias SSG, Teixeira L, et al: Platelet-monocyte
interaction amplifies thromboinflammation through tissue factor
signaling in COVID-19. Blood Adv. 6:5085–5099. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Melgert BN, Spaans F, Borghuis T, Klok PA,
Groen B, Bolt A, de Vos P, van Pampus MG, Wong TY, van Goor H, et
al: Pregnancy and preeclampsia affect monocyte subsets in humans
and rats. PLoS One. 7:e452292012. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Torchinsky A, Shepshelovich J, Orenstein
H, Zaslavsky Z, Savion S, Carp H, Fain A and Toder V: TNF-alpha
protects embryos exposed to developmental toxicants. Am J Reprod
Immunol. 49:159–168. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Piccinni MP, Raghupathy R, Saito S and
Szekeres-Bartho J: Cytokines, hormones and cellular regulatory
mechanisms favoring successful reproduction. Front Immunol.
12:7178082021. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Casazza RL, Lazear HM and Miner JJ:
Protective and pathogenic effects of interferon signaling during
pregnancy. Viral Immunol. 33:3–11. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Yang X, Tian Y, Zheng L, Luu T and
Kwak-Kim J: The update immune-regulatory role of pro- and
anti-inflammatory cytokines in recurrent pregnancy losses. Int J
Mol Sci. 24:1322022. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Michimata T, Tsuda H, Sakai M, Fujimura M,
Nagata K, Nakamura M and Saito S: Accumulation of CRTH2-positive
T-helper 2 and T-cytotoxic 2 cells at implantation sites of human
decidua in a prostaglandin D(2)-mediated manner. Mol Hum Reprod.
8:181–187. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Mitchell RE, Hassan M, Burton BR, Britton
G, Hill EV, Verhagen J and Wraith DC: IL-4 enhances IL-10
production in Th1 cells: implications for Th1 and Th2 regulation.
Sci Rep. 7:113152017. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Shi JW, Yang HL, Fan DX, Yang SL, Qiu XM,
Wang Y, Lai ZZ, Ha SY, Ruan LY, Shen HH, et al: The role of CXC
chemokine ligand 16 in physiological and pathological pregnancies.
Am J Reprod Immunol. 83:e132232020. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Shao Q, Liu X, Huang Y, Chen X and Wang H:
Human decidual stromal cells in early pregnancy induce functional
re-programming of monocyte-derived dendritic cells via crosstalk
between G-CSF and IL-1β. Front Immunol. 11:5742702020. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Álvarez D, Morales-Prieto DM and Cadavid
ÁP: Interaction between endothelial cell-derived extracellular
vesicles and monocytes: A potential link between vascular
thrombosis and pregnancy-related morbidity in antiphospholipid
syndrome. Autoimmun Rev. 22:1032742023. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Erez O, Romero R, Jung E, Chaemsaithong P,
Bosco M, Suksai M, Gallo DM and Gotsch F: Preeclampsia and
eclampsia: The conceptual evolution of a syndrome. Am J Obstet
Gynecol. 226((2S)): S786–S803. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Xie H, Zhou H, Wang H, Chen D, Xia L, Wang
T and Yan J: Anti-β(2)GPI/β(2)GPI induced TF and TNF-α expression
in monocytes involving both TLR4/MyD88 and TLR4/TRIF signaling
pathways. Mol Immunol. 53:246–254. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Colasanti T, Alessandri C, Capozzi A,
Sorice M, Delunardo F, Longo A, Pierdominici M, Conti F, Truglia S,
Siracusano A, et al: Autoantibodies specific to a peptide of
β2-glycoprotein I cross-react with TLR4, inducing a proinflammatory
phenotype in endothelial cells and monocytes. Blood. 120:3360–3370.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Raschi E, Chighizola CB, Grossi C, Ronda
N, Gatti R, Meroni PL and Borghi MO: β2-glycoprotein I,
lipopolysaccharide and endothelial TLR4: Three players in the two
hit theory for anti-phospholipid-mediated thrombosis. J Autoimmun.
55:42–50. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Brandt KJ, Fickentscher C, Boehlen F,
Kruithof EKO and de Moerloose P: NF-κB is activated from endosomal
compartments in antiphospholipid antibodies-treated human
monocytes. J Thromb Haemost. 12:779–791. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Müller-Calleja N, Köhler A, Siebald B,
Canisius A, Orning C, Radsak M, Stein P, Mönnikes R and Lackner KJ:
Cofactor-independent antiphospholipid antibodies activate the
NLRP3-inflammasome via endosomal NADPH-oxidase: Implications for
the antiphospholipid syndrome. Thromb Haemost. 113:1071–1083. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Hurst J, Prinz N, Lorenz M, Bauer S,
Chapman J, Lackner KJ and von Landenberg P: TLR7 and TLR8 ligands
and antiphospholipid antibodies show synergistic effects on the
induction of IL-1beta and caspase-1 in monocytes and dendritic
cells. Immunobiology. 214:683–691. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Tektonidou MG: Cardiovascular disease risk
in antiphospholipid syndrome: Thrombo-inflammation and
atherothrombosis. J Autoimmun. 128:1028132022. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Benagiano M, Borghi MO, Romagnoli J,
Mahler M, Bella CD, Grassi A, Capitani N, Emmi G, Troilo A,
Silvestri E, et al: Interleukin-17/Interleukin-21 and Interferon-γ
producing T cells specific for β2 Glycoprotein I in atherosclerosis
inflammation of systemic lupus erythematosus patients with
antiphospholipid syndrome. Haematologica. 104:2519–2527. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Xia L, Zhou H, Wang T, Xie Y, Wang T, Wang
X and Yan J: Activation of mTOR is involved in
anti-β2GPI/β2GPI-induced expression of tissue
factor and IL-8 in monocytes. Thromb Res. 157:103–110. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Niyonzima N, Rahman J, Kunz N, West EE,
Freiwald T, Desai JV, Merle NS, Gidon A, Sporsheim B, Lionakis MS,
et al: Mitochondrial C5aR1 activity in macrophages controls IL-1β
production underlying sterile inflammation. Sci Immunol.
6:eabf24892021. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Khoy K, Mariotte D, Defer G, Petit G,
Toutirais O and Le Mauff B: Natalizumab in multiple sclerosis
treatment: from biological effects to immune monitoring. Front
Immunol. 11:5498422020. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Cheng S, Wang H and Zhou H: The role of
TLR4 on B cell activation and anti-β2GPI antibody
production in the antiphospholipid syndrome. J Immunol Res.
2016:17197202016. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Chaturvedi S, Brodsky RA and McCrae KR:
Complement in the pathophysiology of the antiphospholipid syndrome.
Front Immunol. 10:4492019. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Kiss MG, Papac-Miličević N, Porsch F,
Tsiantoulas D, Hendrikx T, Takaoka M, Dinh HQ, Narzt MS, Göderle L,
Ozsvár-Kozma M, et al: Cell-autonomous regulation of complement C3
by factor H limits macrophage efferocytosis and exacerbates
atherosclerosis. Immunity. 56:1809–1824.e10. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Girardi G, Yarilin D, Thurman JM, Holers
VM and Salmon JE: Complement activation induces dysregulation of
angiogenic factors and causes fetal rejection and growth
restriction. J Exp Med. 203:2165–2175. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Lin Z, Shi JL, Chen M, Zheng ZM, Li MQ and
Shao J: CCL2: An important cytokine in normal and pathological
pregnancies: A review. Front Immunol. 13:10534572023. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Shields CA, McCalmon M, Ibrahim T, White
DL, Williams JM, LaMarca B and Cornelius DC: Placental
ischemia-stimulated T-helper 17 cells induce
preeclampsia-associated cytolytic natural killer cells during
pregnancy. Am J Physiol Regul Integr Comp Physiol. 315:R336–R343.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Wang W, Sung N, Gilman-Sachs A and
Kwak-Kim J: T helper (Th) cell profiles in pregnancy and recurrent
pregnancy losses: Th1/Th2/Th9/Th17/Th22/Tfh cells. Front Immunol.
11:20252020. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Wu Z, Wang M, Liang G, Jin P, Wang P, Xu
Y, Qian Y, Jiang X, Qian J and Dong M: Pro-inflammatory signature
in decidua of recurrent pregnancy loss regardless of embryonic
chromosomal abnormalities. Front Immunol. 12:7727292021. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Vishnyakova P, Elchaninov A, Fatkhudinov T
and Sukhikh G: Role of the monocyte-macrophage system in normal
pregnancy and preeclampsia. Int J Mol Sci. 20:36952019. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Huang SJ, Schatz F, Masch R, Rahman M,
Buchwalder L, Niven-Fairchild T, Tang C, Abrahams VM, Krikun G and
Lockwood CJ: Regulation of chemokine production in response to
pro-inflammatory cytokines in first trimester decidual cells. J
Reprod Immunol. 72:60–73. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Gowhari Shabgah A, Jadidi-Niaragh F,
Mohammadi H, Ebrahimzadeh F, Oveisee M, Jahanara A and Gholizadeh
Navashenaq J: The role of atypical chemokine receptor D6 (ACKR2) in
physiological and pathological conditions; friend, foe, or both?
Front Immunol. 13:8619312022. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Yan S, Cui S, Zhang L, Yang B, Yuan Y, Lv
X, Fu H, Li Y, Huang C and Wang P: Expression of ACKR2 in placentas
from different types of preeclampsia. Placenta. 90:121–127. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Rybak-Krzyszkowska M, Staniczek J,
Kondracka A, Bogusławska J, Kwiatkowski S, Góra T, Strus M and
Górczewski W: From biomarkers to the molecular mechanism of
preeclampsia-A comprehensive literature review. Int J Mol Sci.
24:132522023. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Jena MK, Sharma NR, Petitt M, Maulik D and
Nayak NR: Pathogenesis of preeclampsia and therapeutic approaches
targeting the placenta. Biomolecules. 10:9532020. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Knight JS, Branch DW and Ortel TL:
Antiphospholipid syndrome: Advances in diagnosis, pathogenesis, and
management. BMJ. 380:e0697172023. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Alvarez AM, Mulla MJ, Chamley LW, Cadavid
AP and Abrahams VM: Aspirin-triggered lipoxin prevents
antiphospholipid antibody effects on human trophoblast migration
and endothelial cell interactions. Arthritis Rheumatol. 67:488–497.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Bruno V, Svensson-Arvelund J, Rubér M,
Berg G, Piccione E, Jenmalm MC and Ernerudh J: Effects of low
molecular weight heparin on the polarization and cytokine profile
of macrophages and T helper cells in vitro. Sci Rep. 8:41662018.
View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Saraiva-Mangolin S, Vaz CDO, Ruiz T,
Mazetto BM and Orsi FA: Use of hydroxychloroquine to control immune
response and hypercoagulability in patients with primary
antiphospholipid syndrome. Eur J Intern Med. 90:114–115. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Tishler M, Yaron I, Shirazi I and Yaron M:
Hydroxychloroquine treatment for primary Sjögren's syndrome: Its
effect on salivary and serum inflammatory markers. Ann Rheum Dis.
58:253–256. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Miranda S, Billoir P, Damian L, Thiebaut
PA, Schapman D, Le Besnerais M, Jouen F, Galas L, Levesque H, Le
Cam-Duchez V, et al: Hydroxychloroquine reverses the prothrombotic
state in a mouse model of antiphospholipid syndrome: Role of
reduced inflammation and endothelial dysfunction. PLoS One.
14:e02126142019. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Arachchillage DJ, Laffan M and Pericleous
C: Hydroxy-chloroquine as an immunomodulatory and antithrombotic
treatment in antiphospholipid syndrome. Int J Mol Sci. 24:13312023.
View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Müller-Calleja N, Hollerbach A, Häuser F,
Canisius A, Orning C and Lackner KJ: Antiphospholipid
antibody-induced cellular responses depend on epitope specificity:
Implications for treatment of antiphospholipid syndrome. J Thromb
Haemost. 15:2367–2376. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Hollerbach A, Müller-Calleja N, Canisius
A, Orning C and Lackner KJ: Induction of tissue factor expression
by anti-β2-glycoprotein I is mediated by tumor necrosis factor α. J
Thromb Thrombolysis. 49:228–234. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Canaud G, Bienaimé F, Tabarin F, Bataillon
G, Seilhean D, Noël LH, Dragon-Durey MA, Snanoudj R, Friedlander G,
Halbwachs-Mecarelli L, et al: Inhibition of the mTORC pathway in
the antiphospholipid syndrome. N Engl J Med. 371:303–312. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Cornelius DC, Travis OK, Tramel RW,
Borges-Rodriguez M, Baik CH, Greer M, Giachelli CA, Tardo GA and
Williams JM: NLRP3 inflammasome inhibition attenuates
sepsis-induced platelet activation and prevents multi-organ injury
in cecal-ligation puncture. PLoS One. 15:e02340392020. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Hooftman A, Angiari S, Hester S, Corcoran
SE, Runtsch MC, Ling C, Ruzek MC, Slivka PF, McGettrick AF, Banahan
K, et al: The immunomodulatory metabolite itaconate modifies NLRP3
and inhibits inflammasome activation. Cell Metab. 32:468–478.e7.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Li Y, Chen X, Zhang H, Xiao J, Yang C,
Chen W, Wei Z, Chen X and Liu J: 4-Octyl itaconate alleviates
lipopolysaccharide-induced acute lung injury in mice by inhibiting
oxidative stress and inflammation. Drug Des Devel Ther.
14:5547–5558. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Tardif JC, Kouz S, Waters DD, Bertrand OF,
Diaz R, Maggioni AP, Pinto FJ, Ibrahim R, Gamra H, Kiwan GS, et al:
Efficacy and safety of low-dose colchicine after myocardial
infarction. N Engl J Med. 381:2497–2505. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Perez-Sanchez C, Ruiz-Limon P, Aguirre MA,
Bertolaccini ML, Khamashta MA, Rodriguez-Ariza A, Segui P,
Collantes-Estevez E, Barbarroja N, Khraiwesh H, et al:
Mitochondrial dysfunction in antiphospholipid syndrome:
Implications in the pathogenesis of the disease and effects of
coenzyme Q(10) treatment. Blood. 119:5859–5870. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Pérez-Sánchez C, Aguirre MÁ, Ruiz-Limón P,
Ábalos-Aguilera MC, Jiménez-Gómez Y, Arias-de la Rosa I,
Rodriguez-Ariza A, Fernández-Del Río L, González-Reyes JA, Segui P,
et al: Ubiquinol effects on antiphospholipid syndrome prothrombotic
profile: A randomized, placebo-controlled trial. Arterioscler
Thromb Vasc Biol. 37:1923–1932. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Alijotas-Reig J, Esteve-Valverde E, Llurba
E and Gris JM: Treatment of refractory poor aPL-related obstetric
outcomes with TNF-alpha blockers: Maternal-fetal outcomes in a
series of 18 cases. Semin Arthritis Rheum. 49:314–318. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Sachetto ATA, Archibald SJ, Perkins M,
Zhang G, Zhang Y, Ye D, Grover SP, Wu C, Li Z and Mackman N:
Pathways regulating the levels of tissue factor-positive
extracellular vesicles and activation of coagulation in endotoxemic
mice. J Thromb Haemost. 23:2422–2435. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Mantle D and Hargreaves IP: Coenzyme Q10
and autoimmune disorders: An overview. Int J Mol Sci. 25:45762024.
View Article : Google Scholar : PubMed/NCBI
|