|
1
|
GBD 2015 Chronic Respiratory Disease
Collaborators, . Global, regional, and national deaths, prevalence,
disability-adjusted life years, and years lived with disability for
chronic obstructive pulmonary disease and asthma, 1990–2015: A
systematic analysis for the global burden of disease study 2015.
Lancet Respir Med. 5:691–706. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
World Health Organization (WHO), . Global
Health Estimates 2016: Deaths by cause, age, sex, by country and by
region, 2000–2016. WHO; Geneva: 2018
|
|
3
|
Ogal M, Johnston SL, Klein P and Schoop R:
Echinacea reduces antibiotic usage in children through respiratory
tract infection prevention: A randomized, blinded, controlled
clinical trial. Eur J Med Res. 26:332021. View Article : Google Scholar : PubMed/NCBI
|
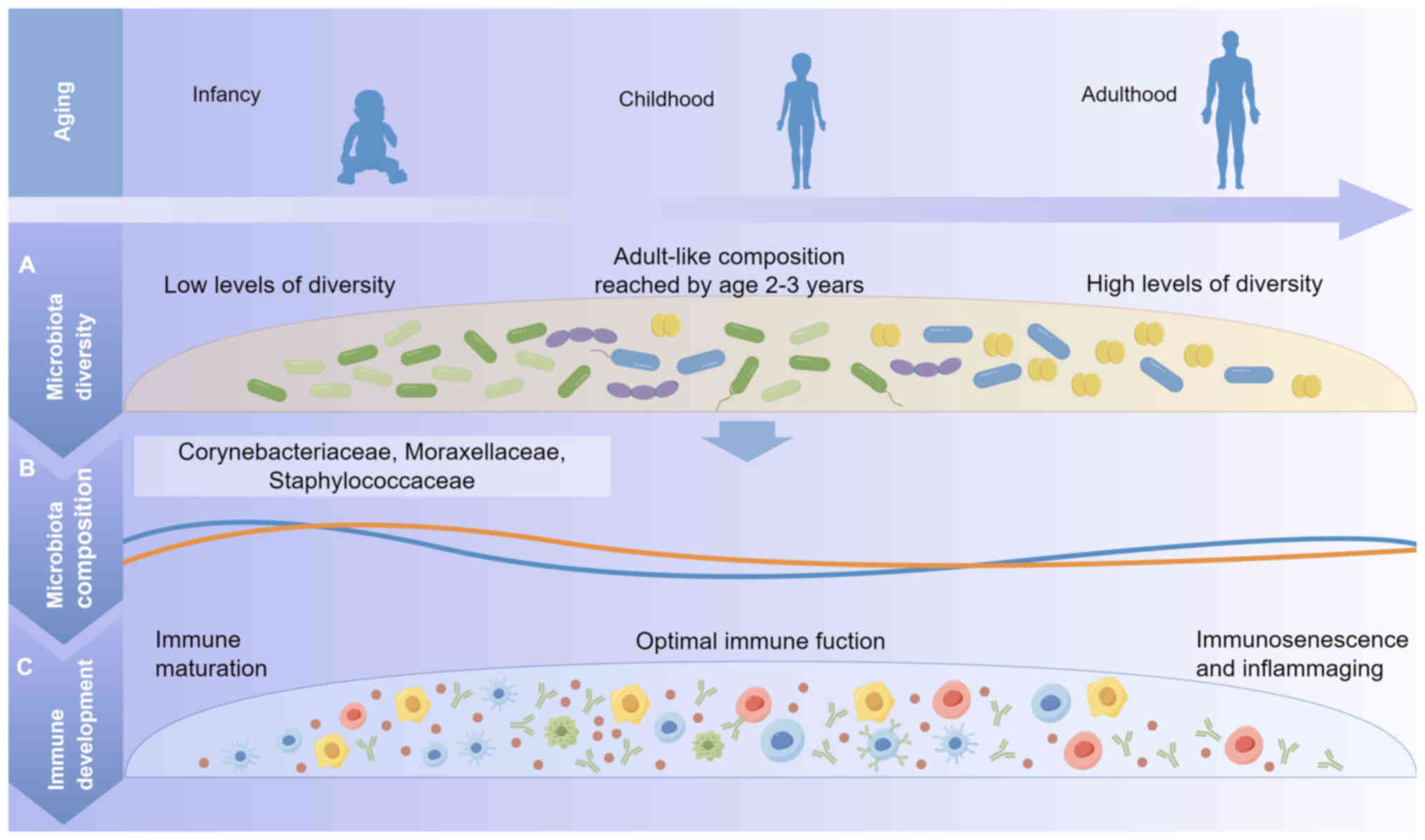
|
4
|
Aitken M and Taylor JA: Prevalence of
clinical sinusitis in young children followed up by primary care
pediatricians. Arch Pediatr Adolesc Med. 152:244–248. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tian J, Wang XY, Zhang LL, Liu MJ, Ai JH,
Feng GS, Zeng YP, Wang R and Xie ZD: Clinical epidemiology and
disease burden of bronchiolitis in hospitalized children in China:
A national cross-sectional study. World J Pediatr. 19:851–863.
2023. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chatterjee A, Mavunda K and Krilov LR:
Current state of respiratory syncytial virus disease and
management. Infect Dis Ther. 10 (Suppl 1):S5–S16. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Keulers L, Dehghani A, Knippels L, Garssen
J, Papadopoulos N, Folkerts G, Braber S and van Bergenhenegouwen J:
Probiotics, prebiotics, and synbiotics to prevent or combat air
pollution consequences: The gut-lung axis. Environ Pollut.
302:1190662022. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Asadi A, Shadab Mehr N, Mohamadi MH,
Shokri F, Heidary M, Sadeghifard N and Khoshnood S: Obesity and
gut-microbiota-brain axis: A narrative review. J Clin Lab Anal.
36:e244202022. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mancin L, Wu GD and Paoli A: Gut
microbiota-bile acid-skeletal muscle axis. Trends Microbiol.
31:254–269. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ahlawat S and Asha Sharma KK: Gut-organ
axis: A microbial outreach and networking. Lett Appl Microbiol.
72:636–668. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Akshay A, Gasim R, Ali TE, Kumar YS and
Hassan A: Unlocking the gut-cardiac axis: A paradigm shift in
cardiovascular health. Cureus. 15:e510392023.PubMed/NCBI
|
|
12
|
Wong CC and Yu J: Gut microbiota in
colorectal cancer development and therapy. Nat Rev Clin Oncol.
20:429–452. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yang Z, Wang Q, Liu Y, Wang L, Ge Z, Li Z,
Feng S and Wu C: Gut microbiota and hypertension: Association,
mechanisms and treatment. Clin Exp Hypertens. 45:21951352023.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wilkins AT and Reimer RA: Obesity, early
life gut microbiota, and antibiotics. Microorganisms. 9:4132021.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zhu W, Wu Y, Liu H, Jiang C and Huo L:
Gut-lung axis: Microbial crosstalk in pediatric respiratory tract
infections. Front Immunol. 12:7412332021. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Walker AW and Hoyles L: Human microbiome
myths and misconceptions. Nat Microbiol. 8:1392–1396. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Eribo OA, du Plessis N and Chegou NN: The
intestinal commensal, bacteroides fragilis, modulates host
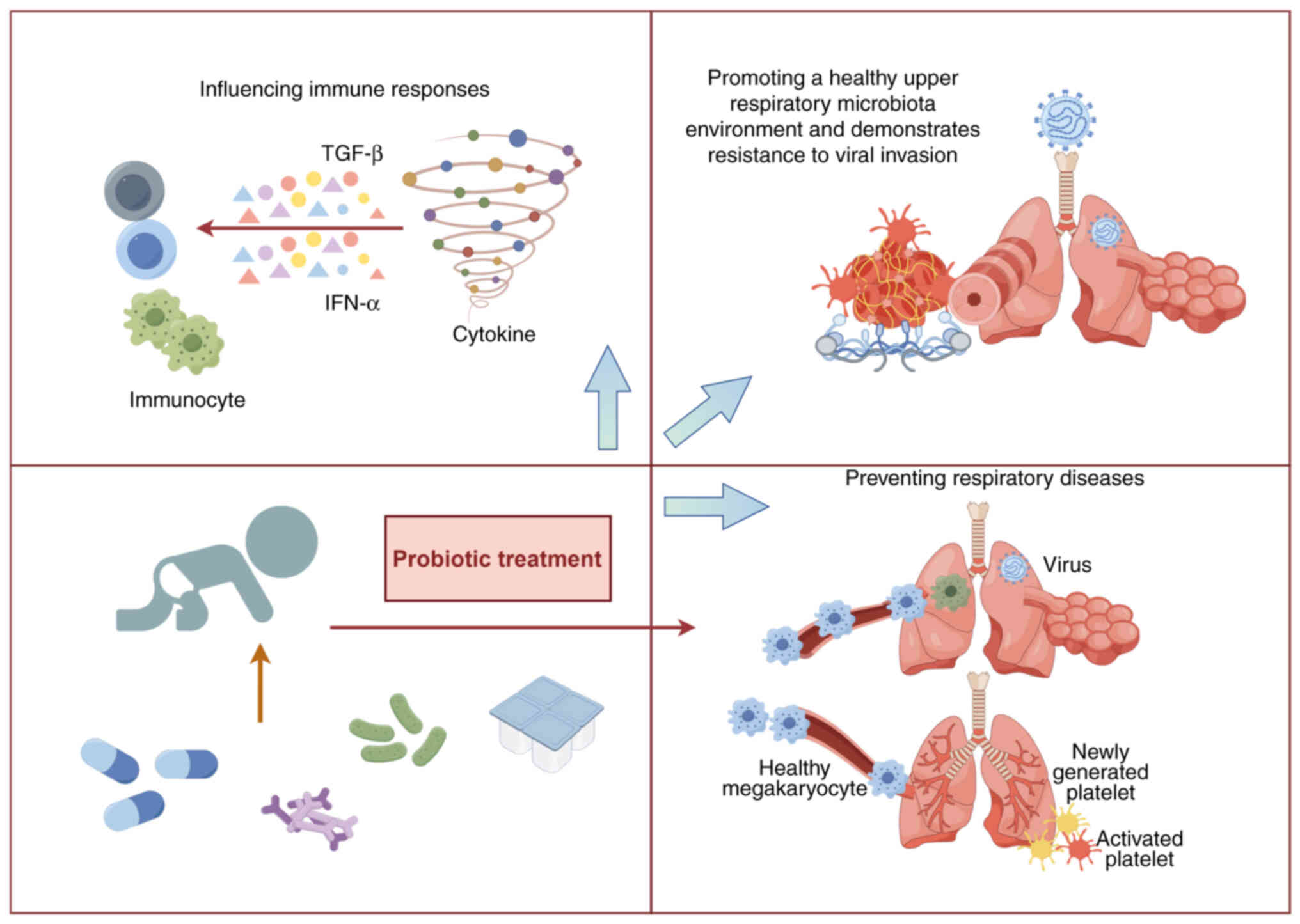
responses to viral infection and therapy: Lessons for exploration
during mycobacterium tuberculosis infection. Infect Immun.
90:e00321212022. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Alcazar CG, Paes VM, Shao Y, Oesser C,
Miltz A, Lawley TD, Brocklehurst P, Rodger A and Field N: The
association between early-life gut microbiota and childhood
respiratory diseases: A systematic review. Lancet Microbe.
3:e867–e880. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zheng D, Liwinski T and Elinav E:
Interaction between microbiota and immunity in health and disease.
Cell Res. 30:492–506. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
van den Elsen LWJ, Garssen J, Burcelin R
and Verhasselt V: Shaping the gut microbiota by breastfeeding: The
gateway to allergy prevention? Front Pediatr. 7:472019. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Shao Y, Forster SC, Tsaliki E, Vervier K,
Strang A, Simpson N, Kumar N, Stares MD, Rodger A, Brocklehurst P,
et al: Stunted microbiota and opportunistic pathogen colonization
in caesarean-section birth. Nature. 574:117–121. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Munyaka PM, Khafipour E and Ghia JE:
External influence of early childhood establishment of gut
microbiota and subsequent health implications. Front Pediatr.
2:1092014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Dominguez-Bello MG, Costello EK, Contreras
M, Magris M, Hidalgo G, Fierer N and Knight R: Delivery mode shapes
the acquisition and structure of the initial microbiota across
multiple body habitats in newborns. Proc Natl Acad Sci USA.
107:11971–11975. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Bokulich NA, Chung J, Battaglia T,
Henderson N, Jay M, Li H, D Lieber A, Wu F, Perez-Perez GI, Chen Y,
et al: Antibiotics, birth mode, and diet shape microbiome
maturation during early life. Sci Transl Med. 8:343ra3822016.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Rodríguez JM, Murphy K, Stanton C, Ross
RP, Kober OI, Juge N, Avershina E, Rudi K, Narbad A, Jenmalm MC, et
al: The composition of the gut microbiota throughout life, with an
emphasis on early life. Microb Ecol Health Dis.
26:260502015.PubMed/NCBI
|
|
26
|
Jakobsson HE, Abrahamsson TR, Jenmalm MC,
Harris K, Quince C, Jernberg C, Björkstén B, Engstrand L and
Andersson AF: Decreased gut microbiota diversity, delayed
Bacteroidetes colonisation and reduced Th1 responses in infants
delivered by caesarean section. Gut. 63:559–566. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Chu DM, Ma J, Prince AL, Antony KM,
Seferovic MD and Aagaard KM: Maturation of the infant microbiome
community structure and function across multiple body sites and in
relation to mode of delivery. Nat Med. 23:314–326. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Fouhy F, Watkins C, Hill CJ, O'Shea CA,
Nagle B, Dempsey EM, O'Toole PW, Ross RP, Ryan CA and Stanton C:
Perinatal factors affect the gut microbiota up to four years after
birth. Nat Commun. 10:15172019. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Stupak A and Kwaśniewski W: Evaluating
current molecular techniques and evidence in assessing microbiome
in placenta-related health and disorders in pregnancy.
Biomolecules. 13:9112023. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Le Huërou-Luron I, Blat S and Boudry G:
Breast- v. formula-feeding: Impacts on the digestive tract and
immediate and long-term health effects. Nutr Res Rev. 23:23–36.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Korpela K, Blakstad EW, Moltu SJ, Strømmen
K, Nakstad B, Rønnestad AE, Brække K, Iversen PO, Drevon CA and de
Vos W: Intestinal microbiota development and gestational age in
preterm neonates. Sci Rep. 8:24532018. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Milani C, Duranti S, Bottacini F, Casey E,
Turroni F, Mahony J, Belzer C, Delgado Palacio S, Arboleya Montes
S, Mancabelli L, et al: The first microbial colonizers of the human
gut: Composition, activities, and health implications of the infant
gut microbiota. Microbiol Mol Biol Rev. 81:e00036–17. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Arboleya S, Sánchez B, Milani C, Duranti
S, Solís G, Fernández N, de los Reyes-Gavilán CG, Ventura M,
Margolles A and Gueimonde M: Intestinal microbiota development in
preterm neonates and effect of perinatal antibiotics. J Pediatr.
166:538–544. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Cong X, Xu W, Janton S, Henderson WA,
Matson A, McGrath JM, Maas K and Graf J: Gut microbiome
developmental patterns in early life of preterm infants: Impacts of
feeding and gender. PLoS One. 11:e01527512016. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Binns C, Lee M and Low WY: The long-term
public health benefits of breastfeeding. Asia Pac J Public Health.
28:7–14. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Perrella S, Gridneva Z, Lai CT, Stinson L,
George A, Bilston-John S and Geddes D: Human milk composition
promotes optimal infant growth, development and health. Semin
Perinatol. 45:1513802021. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Berger B, Porta N, Foata F, Grathwohl D,
Delley M, Moine D, Charpagne A, Siegwald L, Descombes P, Alliet P,
et al: Linking human milk oligosaccharides, infant fecal community
types, and later risk to require antibiotics. mBio. 11:e03196–19.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Zuurveld M, van Witzenburg NP, Garssen J,
Folkerts G, Stahl B, Van't Land B and Willemsen LEM:
Immunomodulation by human milk oligosaccharides: The potential role
in prevention of allergic diseases. Front Immunol. 11:8012020.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Bogaert D, van Beveren GJ, de Koff EM,
Lusarreta Parga P, Balcazar Lopez CE, Koppensteiner L, Clerc M,
Hasrat R, Arp K, Chu MLJN, et al: Mother-to-infant microbiota
transmission and infant microbiota development across multiple body
sites. Cell Host Microbe. 31:447–460.e6. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Yagi K, Asai N, Huffnagle GB, Lukacs NW
and Fonseca W: Early-life lung and gut microbiota development and
respiratory syncytial virus infection. Front Immunol.
13:8777712022. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Borewicz K, Suarez-Diez M, Hechler C,
Beijers R, de Weerth C, Arts I, Penders J, Thijs C, Nauta A,
Lindner C, et al: The effect of prebiotic fortified infant formulas
on microbiota composition and dynamics in early life. Sci Rep.
9:24342019. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Zhu B, Zheng S, Lin K, Xu X, Lv L, Zhao Z
and Shao J: Effects of infant formula supplemented with prebiotics
and OPO on infancy fecal microbiota: A pilot Randomized clinical
trial. Front Cell Infect Microbiol. 11:6504072021. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Ratsika A, Codagnone MC, O'Mahony S,
Stanton C and Cryan JF: Priming for Life: Early life nutrition and
the microbiota-gut-brain axis. Nutrients. 13:4232021. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Ianiro G, Tilg H and Gasbarrini A:
Antibiotics as deep modulators of gut microbiota: Between good and
evil. Gut. 65:1906–1915. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Dierikx TH, Visser DH, Benninga MA, van
Kaam AHLC, de Boer NKH, de Vries R, van Limbergen J and de Meij
TGJ: The influence of prenatal and intrapartum antibiotics on
intestinal microbiota colonisation in infants: A systematic review.
J Infect. 81:190–204. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Panda S, El khader I, Casellas F, López
Vivancos J, García Cors M, Santiago A, Cuenca S, Guarner F and
Manichanh C: Short-term effect of antibiotics on human gut
microbiota. PLoS One. 9:e954762014. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Blaser MJ and Dominguez-Bello MG: The
human microbiome before birth. Cell Host Microbe. 20:558–560. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Azad MB, Konya T, Persaud RR, Guttman DS,
Chari RS, Field CJ, Sears MR, Mandhane PJ, Turvey SE, Subbarao P,
et al: Impact of maternal intrapartum antibiotics, method of birth
and breastfeeding on gut microbiota during the first year of life:
A prospective cohort study. BJOG. 123:983–993. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Hermansson H, Kumar H, Collado MC,
Salminen S, Isolauri E and Rautava S: Breast milk microbiota is
shaped by mode of delivery and intrapartum antibiotic exposure.
Front Nutr. 6:42019. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Subramanian S, Huq S, Yatsunenko T, Haque
R, Mahfuz M, Alam MA, Benezra A, DeStefano J, Meier MF, Muegge BD,
et al: Persistent gut microbiota immaturity in malnourished
Bangladeshi children. Nature. 510:417–421. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Blanton LV, Barratt MJ, Charbonneau MR,
Ahmed T and Gordon JI: Childhood undernutrition, the gut
microbiota, and microbiota-directed therapeutics. Science.
352:15332016. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Kane AV, Dinh DM and Ward HD: Childhood
malnutrition and the intestinal microbiome. Pediatr Res.
77:256–262. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Moles L, Gómez M, Heilig H, Bustos G,
Fuentes S, de Vos W, Fernández L, Rodríguez JM and Jiménez E:
Bacterial diversity in meconium of preterm neonates and evolution
of their fecal microbiota during the first month of life. PLoS One.
8:e669862013. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Fernández L, Langa S, Martín V, Maldonado
A, Jiménez E, Martín R and Rodríguez JM: The human milk microbiota:
Origin and potential roles in health and disease. Pharmacol Res.
69:1–10. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Mountzouris KC, McCartney AL and Gibson
GR: Intestinal microflora of human infants and current trends for
its nutritional modulation. Br J Nutr. 87:405–420. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Barrett E, Kerr C, Murphy K, O'Sullivan O,
Ryan CA, Dempsey EM, Murphy BP, O'Toole PW, Cotter PD, Fitzgerald
GF, et al: The individual-specific and diverse nature of the
preterm infant microbiota. Arch Dis Child Fetal Neonatal Ed.
98:F334–F340. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Fouhy F, Guinane CM, Hussey S, Wall R,
Ryan CA, Dempsey EM, Murphy B, Ross RP, Fitzgerald GF, Stanton C
and Cotter PD: High-throughput sequencing reveals the incomplete,
short-term recovery of infant gut microbiota following parenteral
antibiotic treatment with ampicillin and gentamicin. Antimicrob
Agents Chemother. 56:5811–5820. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Fallani M, Young D, Scott J, Norin E,
Amarri S, Adam R, Aguilera M, Khanna S, Gil A, Edwards CA, et al:
Intestinal microbiota of 6-week-old infants across Europe:
Geographic influence beyond delivery mode, breast-feeding, and
antibiotics. J Pediatr Gastroenterol Nutr. 51:77–84. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Budden KF, Gellatly SL, Wood DL, Cooper
MA, Morrison M, Hugenholtz P and Hansbro PM: Emerging pathogenic
links between microbiota and the gut-lung axis. Nat Rev Microbiol.
15:55–63. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Espírito Santo C, Caseiro C, Martins MJ,
Monteiro R and Brandão I: Gut microbiota, in the halfway between
nutrition and lung function. Nutrients. 13:17162021. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Chistiakov DA, Bobryshev YV, Kozarov E,
Sobenin IA and Orekhov AN: Intestinal mucosal tolerance and impact
of gut microbiota to mucosal tolerance. Front Microbiol. 5:7812015.
View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Ratajczak W, Rył A, Mizerski A,
Walczakiewicz K, Sipak O and Laszczyńska M: Immunomodulatory
potential of gut microbiome-derived short-chain fatty acids
(SCFAs). Acta Biochim Pol. 66:1–12. 2019.PubMed/NCBI
|
|
63
|
Li M, van Esch BCAM, Wagenaar GTM, Garssen
J, Folkerts G and Henricks PAJ: Pro- and anti-inflammatory effects
of short chain fatty acids on immune and endothelial cells. Eur J
Pharmacol. 831:52–59. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Lee SH, Yun Y, Kim SJ, Lee EJ, Chang Y,
Ryu S, Shin H, Kim HL, Kim HN and Lee JH: Association between
cigarette smoking status and composition of gut microbiota:
Population-based cross-sectional study. J Clin Med. 7:2822018.
View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Bowerman KL, Rehman SF, Vaughan A, Lachner
N, Budden KF, Kim RY, Wood DLA, Gellatly SL, Shukla SD, Wood LG, et
al: Disease-associated gut microbiome and metabolome changes in
patients with chronic obstructive pulmonary disease. Nat Commun.
11:58862020. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Gray J, Oehrle K, Worthen G, Alenghat T,
Whitsett J and Deshmukh H: Intestinal commensal bacteria mediate
lung mucosal immunity and promote resistance of newborn mice to
infection. Sci Transl Med. 9:eaaf94122017. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Olszak T, An D, Zeissig S, Vera MP,
Richter J, Franke A, Glickman JN, Siebert R, Baron RM, Kasper DL
and Blumberg RS: Microbial exposure during early life has
persistent effects on natural killer T cell function. Science.
336:489–493. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Brown RL, Sequeira RP and Clarke TB: The
microbiota protects against respiratory infection via GM-CSF
signaling. Nat Commun. 8:15122017. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Luoto R, Ruuskanen O, Waris M, Kalliomäki
M, Salminen S and Isolauri E: Prebiotic and probiotic
supplementation prevents rhinovirus infections in preterm infants:
a randomized, placebo-controlled trial. J Allergy Clin Immunol.
133:405–413. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Maldonado J, Cañabate F, Sempere L, Vela
F, Sánchez AR, Narbona E, López-Huertas E, Geerlings A, Valero AD,
Olivares M and Lara-Villoslada F: Human milk probiotic
Lactobacillus fermentum CECT5716 reduces the incidence of
gastrointestinal and upper respiratory tract infections in infants.
J Pediatr Gastroenterol Nutr. 54:55–61. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Wang Y, Li X, Ge T, Xiao Y, Liao Y, Cui Y,
Zhang Y, Ho W, Yu G and Zhang T: Probiotics for prevention and
treatment of respiratory tract infections in children: A systematic
review and meta-analysis of randomized controlled trials. Medicine
(Baltimore). 95:e45092016. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Redd WD, Zhou JC, Hathorn KE, McCarty TR,
Bazarbashi AN, Thompson CC, Shen L and Chan WW: Prevalence and
characteristics of gastrointestinal symptoms in patients with
severe acute respiratory syndrome coronavirus 2 infection in the
United States: A multicenter cohort study. Gastroenterology.
159:765–767.e2. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Zuo T, Zhang F, Lui GCY, Yeoh YK, Li AYL,
Zhan H, Wan Y, Chung ACK, Cheung CP, Chen N, et al: Alterations in
gut microbiota of patients with COVID-19 during time of
hospitalization. Gastroenterology. 159:944–955.e8. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Yeoh YK, Zuo T, Lui GC, Zhang F, Liu Q, Li
AY, Chung AC, Cheung CP, Tso EY, Fung KS, et al: Gut microbiota
composition reflects disease severity and dysfunctional immune
responses in patients with COVID-19. Gut. 70:698–706. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Liu Y, Ni F, Huang J, Hu Y, Wang J, Wang
X, Du X and Jiang H: PPAR-α inhibits DHEA-induced ferroptosis in
granulosa cells through upregulation of FADS2. Biochem Biophys Res
Commun. 715:1500052024. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Mazur NI, Higgins D, Nunes MC, Melero JA,
Langedijk AC, Horsley N, Buchholz UJ, Openshaw PJ, McLellan JS,
Englund JA, et al: The respiratory syncytial virus vaccine
landscape: Lessons from the graveyard and promising candidates.
Lancet Infect Dis. 18:e295–e311. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Janet S, Broad J and Snape MD: Respiratory
syncytial virus seasonality and its implications on prevention
strategies. Hum Vaccin Immunother. 14:234–244. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Russell CD, Unger SA, Walton M and
Schwarze J: The human immune response to respiratory syncytial
virus infection. Clin Microbiol Rev. 30:481–502. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Bénet T, Sánchez Picot V, Messaoudi M,
Chou M, Eap T, Wang J, Shen K, Pape JW, Rouzier V, Awasthi S, et
al: Microorganisms associated with pneumonia in children <5
years of age in developing and emerging countries: The GABRIEL
pneumonia multicenter, prospective, case-control study. Clin Infect
Dis. 65:604–612. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Pneumonia Etiology Research for Child
Health (PERCH) Study Group, : Causes of severe pneumonia requiring
hospital admission in children without HIV infection from Africa
and Asia: the PERCH multi-country case-control study. Lancet.
394:757–779. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Lozano R, Naghavi M, Foreman K, Lim S,
Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, et
al: Global and regional mortality from 235 causes of death for 20
age groups in 1990 and 2010: A systematic analysis for the Global
Burden of Disease Study 2010. Lancet. 380:2095–2128. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Harding JN, Siefker D, Vu L, You D,
DeVincenzo J, Pierre JF and Cormier SA: Altered gut microbiota in
infants is associated with respiratory syncytial virus disease
severity. BMC Microbiol. 20:1402020. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Jang MJ, Kim YJ, Hong S, Na J, Hwang JH,
Shin SM and Ahn YM: Positive association of breastfeeding on
respiratory syncytial virus infection in hospitalized infants: A
multicenter retrospective study. Clin Exp Pediatr. 63:135–140.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Hasegawa K, Linnemann RW, Mansbach JM,
Ajami NJ, Espinola JA, Petrosino JF, Piedra PA, Stevenson MD,
Sullivan AF, Thompson AD and Camargo CA Jr: The fecal microbiota
profile and bronchiolitis in infants. Pediatrics.
138:e201602182016. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Nishimura T, Suzue J and Kaji H:
Breastfeeding reduces the severity of respiratory syncytial virus
infection among young infants: A multi-center prospective study.
Pediatr Int. 51:812–816. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Kristensen K, Fisker N, Haerskjold A, Ravn
H, Simões EA and Stensballe L: Caesarean section and
hospitalization for respiratory syncytial virus infection: A
population-based study. Pediatr Infect Dis J. 34:145–148. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Lee HC, Headley MB, Loo YM, Berlin A, Gale
M Jr, Debley JS, Lukacs NW and Ziegler SF: Thymic stromal
lymphopoietin is induced by respiratory syncytial virus-infected
airway epithelial cells and promotes a type 2 response to
infection. J Allergy Clin Immunol. 130:1187–1196.e1185. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Ptaschinski C, Mukherjee S, Moore ML,
Albert M, Helin K, Kunkel SL and Lukacs NW: RSV–Induced H3K4
demethylase KDM5B leads to regulation of dendritic cell-derived
innate cytokines and exacerbates pathogenesis in vivo. PLoS Pathog.
11:e10049782015. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Lu S, Hartert TV, Everard ML, Giezek H,
Nelsen L, Mehta A, Patel H, Knorr B and Reiss TF: Predictors of
asthma following severe respiratory syncytial virus (RSV)
bronchiolitis in early childhood. Pediatr Pulmonol. 51:1382–1392.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Malinczak CA, Fonseca W, Rasky AJ,
Ptaschinski C, Morris S, Ziegler SF and Lukacs NW: Sex-associated
TSLP-induced immune alterations following early-life RSV infection
leads to enhanced allergic disease. Mucosal Immunol. 12:969–979.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Yagi K, Lukacs NW, Huffnagle GB, Kato H
and Asai N: Respiratory and gut microbiome modification during
respiratory syncytial virus infection: A systematic review.
Viruses. 16:2202024. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Fonseca W, Malinczak CA, Fujimura K, Li D,
McCauley K, Li J, Best SKK, Zhu D, Rasky AJ, Johnson CC, et al:
Maternal gut microbiome regulates immunity to RSV infection in
offspring. J Exp Med. 218:e202102352021. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Ballarini S, Ardusso L, Ortega Martell JA,
Sacco O, Feleszko W and Rossi GA: Can bacterial lysates be useful
in prevention of viral respiratory infections in childhood? The
results of experimental OM-85 studies. Front Pediatr.
10:10510792022. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
National Institute for Health and Care
Excellence (NICE), . Asthma: Diagnosis, monitoring and chronic
asthma management. NICE Guideline, No. 80. NICE; London: 2021
|
|
95
|
Asher MI, Rutter CE, Bissell K, Chiang CY,
El Sony A, Ellwood E, Ellwood P, García-Marcos L, Marks GB, Morales
E, et al: Worldwide trends in the burden of asthma symptoms in
school-aged children: Global asthma network phase I cross-sectional
study. Lancet. 398:1569–1580. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Fainardi V, Esposito S, Chetta A and Pisi
G: Asthma phenotypes and endotypes in childhood. Minerva Med.
113:94–105. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Martinez FD and Vercelli D: Asthma.
Lancet. 382:1360–1372. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Ntontsi P, Photiades A, Zervas E, Xanthou
G and Samitas K: Genetics and epigenetics in asthma. Int J Mol Sci.
22:24122021. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Stokholm J, Blaser MJ, Thorsen J,
Rasmussen MA, Waage J, Vinding RK, Schoos AM, Kunøe A, Fink NR,
Chawes BL, et al: Maturation of the gut microbiome and risk of
asthma in childhood. Nat Commun. 9:1412018. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Fujimura KE, Sitarik AR, Havstad S, Lin
DL, Levan S, Fadrosh D, Panzer AR, LaMere B, Rackaityte E, Lukacs
NW, et al: Neonatal gut microbiota associates with childhood
multisensitized atopy and T cell differentiation. Nat Med.
22:1187–1191. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Abreo A, Gebretsadik T, Stone CA and
Hartert TV: The impact of modifiable risk factor reduction on
childhood asthma development. Clin Transl Med. 7:152018. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Rosas-Salazar C, Shilts MH, Tang ZZ, Hong
Q, Turi KN, Snyder BM, Wiggins DA, Lynch CE, Gebretsadik T, Peebles
RS Jr, et al: Exclusive breast-feeding, the early-life microbiome
and immune response, and common childhood respiratory illnesses. J
Allergy Clin Immunol. 150:612–621. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Saeed NK, Al-Beltagi M, Bediwy AS,
El-Sawaf Y and Toema O: Gut microbiota in various childhood
disorders: Implication and indications. World J Gastroenterol.
28:1875–1901. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Patrick DM, Sbihi H, Dai DLY, Al Mamun A,
Rasali D, Rose C, Marra F, Boutin RCT, Petersen C, Stiemsma LT, et
al: Decreasing antibiotic use, the gut microbiota, and asthma
incidence in children: Evidence from population-based and
prospective cohort studies. Lancet Respir Med. 8:1094–1105. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Kloepfer KM and Kennedy JL: Childhood
respiratory viral infections and the microbiome. J Allergy Clin
Immunol. 152:827–834. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Gensollen T, Iyer SS, Kasper DL and
Blumberg RS: How colonization by microbiota in early life shapes
the immune system. Science. 352:539–544. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Renz H and Skevaki C: Early life microbial
exposures and allergy risks: Opportunities for prevention. Nat Rev
Immunol. 21:177–191. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Fahy JV and Dickey BF: Airway mucus
function and dysfunction. N Engl J Med. 363:2233–2247. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Scotet V, L'Hostis C and Férec C: The
changing epidemiology of cystic fibrosis: Incidence, Survival and
impact of the CFTR gene discovery. Genes (Basel). 11:5892020.
View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Elborn JS: Cystic fibrosis. Lancet.
388:2519–2531. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Rafeeq MM and Murad HAS: Cystic fibrosis:
Current therapeutic targets and future approaches. J Transl Med.
15:842017. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Bassis CM, Erb-Downward JR, Dickson RP,
Freeman CM, Schmidt TM, Young VB, Beck JM, Curtis JL and Huffnagle
GB: Analysis of the upper respiratory tract microbiotas as the
source of the lung and gastric microbiotas in healthy individuals.
mBio. 6:e000372015. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Rogers GB, Carroll MP, Hoffman LR, Walker
AW, Fine DA and Bruce KD: Comparing the microbiota of the cystic
fibrosis lung and human gut. Gut Microbes. 1:85–93. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Dayama G, Priya S, Niccum DE, Khoruts A
and Blekhman R: Interactions between the gut microbiome and host
gene regulation in cystic fibrosis. Genome Med. 12:122020.
View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Kristensen M, Prevaes SMPJ, Kalkman G,
Tramper-Stranders GA, Hasrat R, de Winter-de Groot KM, Janssens HM,
Tiddens HA, van Westreenen M, Sanders EAM, et al: Development of
the gut microbiota in early life: The impact of cystic fibrosis and
antibiotic treatment. J Cyst Fibros. 19:553–561. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Vernocchi P, Del Chierico F, Russo A, Majo
F, Rossitto M, Valerio M, Casadei L, La Storia A, De Filippis F,
Rizzo C, et al: Gut microbiota signatures in cystic fibrosis: Loss
of host CFTR function drives the microbiota enterophenotype. PLoS
One. 13:e02081712018. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Burke DG, Fouhy F, Harrison MJ, Rea MC,
Cotter PD, O'Sullivan O, Stanton C, Hill C, Shanahan F, Plant BJ
and Ross RP: The altered gut microbiota in adults with cystic
fibrosis. BMC Microbiol. 17:582017. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Miragoli F, Federici S, Ferrari S, Minuti
A, Rebecchi A, Bruzzese E, Buccigrossi V, Guarino A and Callegari
ML: Impact of cystic fibrosis disease on archaea and bacteria
composition of gut microbiota. FEMS Microbiol Ecol. 93:fiw2302017.
View Article : Google Scholar : PubMed/NCBI
|
|
119
|
de Freitas MB, Moreira EAM, Tomio C,
Moreno YMF, Daltoe FP, Barbosa E, Ludwig Neto N, Buccigrossi V and
Guarino A: Altered intestinal microbiota composition, antibiotic
therapy and intestinal inflammation in children and adolescents
with cystic fibrosis. PLoS One. 13:e01984572018. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Matamouros S, Hayden HS, Hager KR,
Brittnacher MJ, Lachance K, Weiss EJ, Pope CE, Imhaus AF, McNally
CP, Borenstein E, et al: Adaptation of commensal proliferating
Escherichia coli to the intestinal tract of young children with
cystic fibrosis. Proc Natl Acad Sci USA. 115:1605–1610. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Nielsen S, Needham B, Leach ST, Day AS,
Jaffe A, Thomas T and Ooi CY: Disrupted progression of the
intestinal microbiota with age in children with cystic fibrosis.
Sci Rep. 6:248572016. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Coffey MJ, Nielsen S, Wemheuer B, Kaakoush
NO, Garg M, Needham B, Pickford R, Jaffe A, Thomas T and Ooi CY:
Gut microbiota in children with cystic fibrosis: A taxonomic and
functional dysbiosis. Sci Rep. 9:185932019. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Manor O, Levy R, Pope CE, Hayden HS,
Brittnacher MJ, Carr R, Radey MC, Hager KR, Heltshe SL, Ramsey BW,
et al: Metagenomic evidence for taxonomic dysbiosis and functional
imbalance in the gastrointestinal tracts of children with cystic
fibrosis. Sci Rep. 6:224932016. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Wang Y, Leong LEX, Keating RL, Kanno T,
Abell GCJ, Mobegi FM, Choo JM, Wesselingh SL, Mason AJ, Burr LD and
Rogers GB: Opportunistic bacteria confer the ability to ferment
prebiotic starch in the adult cystic fibrosis gut. Gut Microbes.
10:367–381. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Vaezi A, Healy T, Ebrahimi G, Rezvankhah
S, Hashemi Shahraki A and Mirsaeidi M: Phage therapy: breathing new
tactics into lower respiratory tract infection treatments. Eur
Respir Rev. 33:2400292024. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Hong Y and Luo T: The potential protective
effects of probiotics, prebiotics, or yogurt on chronic obstructive
pulmonary disease: Results from NHANES 2007–2012. Food Sci Nutr.
12:7233–7241. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Depoorter L and Vandenplas Y: Probiotics
in pediatrics. A review and practical guide. Nutrients.
13:21762021. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Zhang Y, Xu Y, Hu L and Wang X:
Advancements related to probiotics for preventing and treating
recurrent respiratory tract infections in children. Front Pediatr.
13:15086132025. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
O'Donnell A, Murray A, Nguyen A, Salmon T,
Taylor S, Morton JP and Close GL: Nutrition and golf performance: A
systematic scoping review. Sports Med. 54:3081–3095. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Wang Q, Lin X, Xiang X, Liu W, Fang Y,
Chen H, Tang F, Guo H, Chen D, Hu X, et al: Oropharyngeal probiotic
ENT-K12 prevents respiratory tract infections among frontline
medical staff fighting against COVID-19: A pilot study. Front
Bioeng Biotechnol. 9:6461842021. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Samuelson DR, Charles TP, de la Rua NM,
Taylor CM, Blanchard EE, Luo M, Shellito JE and Welsh DA: Analysis
of the intestinal microbial community and inferred functional
capacities during the host response to Pneumocystis pneumonia. Exp
Lung Res. 42:425–439. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Dong Y, Li M and Yue X: Current research
on probiotics and fermented products. Foods. 13:14062024.
View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Mazziotta C, Tognon M, Martini F,
Torreggiani E and Rotondo JC: Probiotics mechanism of action on
immune cells and beneficial effects on human health. Cells.
12:1842023. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Suissa R, Oved R, Jankelowitz G, Turjeman
S, Koren O and Kolodkin-Gal I: Molecular genetics for probiotic
engineering: Dissecting lactic acid bacteria. Trends Microbiol.
30:293–306. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Chiappini E, Santamaria F, Marseglia GL,
Marchisio P, Galli L, Cutrera R, de Martino M, Antonini S,
Becherucci P, Biasci P, et al: Prevention of recurrent respiratory
infections : Inter-society Consensus. Ital J Pediatr. 47:2112021.
View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Yamanishi S and Pawankar R: Current
advances on the microbiome and role of probiotics in upper airways
disease. Curr Opin Allergy Clin Immunol. 20:30–35. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Lopes SA, Roque-Borda CA, Duarte JL, Di
Filippo LD, Borges Cardoso VM, Pavan FR, Chorilli M and Meneguin
AB: delivery strategies of probiotics from nano- and
microparticles: Trends in the treatment of inflammatory bowel
disease-an overview. Pharmaceutics. 15:26002023. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Sun W, Zhou T, Ding P, Guo L, Zhou X and
Long K: Bibliometric analysis of intestinal microbiota and lung
diseases. Front Cell Infect Microbiol. 14:13471102024. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Chakradhar S: A curious connection:
Teasing apart the link between gut microbes and lung disease. Nat
Med. 23:402–404. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Han X, Hu X, Jin W and Liu G: Dietary
nutrition, intestinal microbiota dysbiosis and post-weaning
diarrhea in piglets. Anim Nutr. 17:188–207. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Zhang T, Wei X, Li Y, Huang S, Wu Y, Cai
S, Aipire A and Li J: Dendritic cell-based vaccine prepared with
recombinant Lactococcus lactis enhances antigen cross-presentation
and antitumor efficacy through ROS production. Front Immunol.
14:12083492023. View Article : Google Scholar : PubMed/NCBI
|
|
142
|
Ni C, Li X, Wang L, Li X, Zhao J, Zhang H,
Wang G and Chen W: Lactic acid bacteria strains relieve
hyperuricaemia by suppressing xanthine oxidase activity via a
short-chain fatty acid-dependent mechanism. Food Funct.
12:7054–7067. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Zhao H, Chen X, Zhang L, Meng F, Zhou L,
Pang X, Lu Z and Lu Y: Lacticaseibacillus rhamnosus Fmb14 prevents
purine induced hyperuricemia and alleviate renal fibrosis through
gut-kidney axis. Pharmacol Res. 182:1063502022. View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Ren D, Ding M, Su J, Ye J, He X, Zhang Y
and Shang X: Stachyose in combination with L. rhamnosus GG
ameliorates acute hypobaric hypoxia-induced intestinal barrier
dysfunction through alleviating inflammatory response and oxidative
stress. Free Radic Biol Med. 212:505–519. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Hojsak I, Snovak N, Abdović S, Szajewska
H, Misak Z and Kolacek S: Lactobacillus GG in the prevention of
gastrointestinal and respiratory tract infections in children who
attend day care centers: A randomized, double-blind,
placebo-controlled trial. Clin Nutr. 29:312–316. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
146
|
Liu S, Hu P, Du X, Zhou T and Pei X:
Lactobacillus rhamnosus GG supplementation for preventing
respiratory infections in children: A meta-analysis of randomized,
placebo-controlled trials. Indian Pediatr. 50:377–381. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
147
|
Laursen RP and Hojsak I: Probiotics for
respiratory tract infections in children attending day care
centers-a systematic review. Eur J Pediatr. 177:979–994. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
148
|
Kumpu M, Lehtoranta L, Roivainen M, Rönkkö
E, Ziegler T, Söderlund-Venermo M, Kautiainen H, Järvenpää S,
Kekkonen R, Hatakka K, et al: The use of the probiotic
Lactobacillus rhamnosus GG and viral findings in the nasopharynx of
children attending day care. J Med Virol. 85:1632–1638. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
149
|
Damholt A, Keller MK, Baranowski K, Brown
B, Wichmann A, Melsaether C, Eskesen D, Westphal V, Arltoft D,
Habicht A, et al: Lacticaseibacillus rhamnosus GG DSM 33156 effects
on pathogen defence in the upper respiratory tract: A randomised,
double-blind, placebo-controlled paediatric trial. Benef Microbes.
13:13–23. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
150
|
Sibanda T, Marole TA, Thomashoff UL,
Thantsha MS and Buys EM: Bifidobacterium species viability in
dairy-based probiotic foods: Challenges and innovative approaches
for accurate viability determination and monitoring of probiotic
functionality. Front Microbiol. 15:13270102024. View Article : Google Scholar : PubMed/NCBI
|
|
151
|
Li M, Ding J, Stanton C, Ross RP, Zhao J,
Yang B and Chen W: Bifidobacterium longum subsp. infantis FJSYZ1M3
ameliorates DSS-induced colitis by maintaining the intestinal
barrier, regulating inflammatory cytokines, and modifying gut
microbiota. Food Funct. 14:354–368. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
152
|
Lau AS, Yanagisawa N, Hor YY, Lew LC, Ong
JS, Chuah LO, Lee YY, Choi SB, Rashid F, Wahid N, et al:
Bifidobacterium longum BB536 alleviated upper respiratory illnesses
and modulated gut microbiota profiles in Malaysian pre-school
children. Benef Microbes. 9:61–70. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
153
|
Taipale TJ, Pienihäkkinen K, Isolauri E,
Jokela JT and Söderling EM: Bifidobacterium animalis subsp. lactis
BB-12 in reducing the risk of infections in early childhood.
Pediatr Res. 79:65–69. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
154
|
Li W, Zhang S, Wang Y, Bian H, Yu S, Huang
L and Ma W: Complex probiotics alleviate ampicillin-induced
antibiotic-associated diarrhea in mice. Front Microbiol.
14:11560582023. View Article : Google Scholar : PubMed/NCBI
|
|
155
|
Li KL, Wang BZ, Li ZP, Li YL and Liang JJ:
Alterations of intestinal flora and the effects of probiotics in
children with recurrent respiratory tract infection. World J
Pediatr. 15:255–261. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
156
|
DI Pierro F, Lo Russo P, Danza ML, Basile
I, Soardo S, Capocasale G, Paparone SB, Paletta V, Lanza C,
Schiavone E, et al: Use of a probiotic mixture containing
Bifidobacterium animalis subsp. lactis BB-12 and Enterococcus
faecium L3 as prophylaxis to reduce the incidence of acute
gastroenteritis and upper respiratory tract infections in children.
Minerva Pediatr (Torino). 73:222–229. 2021.PubMed/NCBI
|
|
157
|
Manti S, Parisi GF, Papale M, Licari A,
Salpietro C, Miraglia Del Giudice M, Marseglia GL and Leonardi S:
Bacteriotherapy with Streptococcus salivarius 24SMB and
Streptococcus oralis 89a nasal spray for treatment of upper
respiratory tract infections in children: A pilot study on
short-term efficacy. Ital J Pediatr. 46:422020. View Article : Google Scholar : PubMed/NCBI
|
|
158
|
Campanella V, Syed J, Santacroce L, Saini
R, Ballini A and Inchingolo F: Oral probiotics influence oral and
respiratory tract infections in pediatric population: A randomized
double-blinded placebo-controlled pilot study. Eur Rev Med
Pharmacol Sci. 22:8034–8041. 2018.PubMed/NCBI
|
|
159
|
Plaza-Diaz J, Ruiz-Ojeda FJ, Gil-Campos M
and Gil A: Mechanisms of action of probiotics. Adv Nutr. 10
(Suppl_1):S49–s66. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
160
|
Liu R and Sun B: Lactic acid bacteria and
aging: Unraveling the interplay for healthy longevity. Aging Dis.
15:1487–1498. 2023.PubMed/NCBI
|
|
161
|
Crits-Christoph A, Hallowell HA,
Koutouvalis K and Suez J: Good microbes, bad genes? The
dissemination of antimicrobial resistance in the human microbiome.
Gut Microbes. 14:20559442022. View Article : Google Scholar : PubMed/NCBI
|
|
162
|
Merenstein D, Pot B, Leyer G, Ouwehand AC,
Preidis GA, Elkins CA, Hill C, Lewis ZT, Shane AL, Zmora N, et al:
Emerging issues in probiotic safety: 2023 perspectives. Gut
Microbes. 15:21850342023. View Article : Google Scholar : PubMed/NCBI
|
|
163
|
Boumis E, Capone A, Galati V, Venditti C
and Petrosillo N: Probiotics and infective endocarditis in patients
with hereditary hemorrhagic telangiectasia: A clinical case and a
review of the literature. BMC Infect Dis. 18:652018. View Article : Google Scholar : PubMed/NCBI
|
|
164
|
Doern CD, Nguyen ST, Afolabi F and Burnham
CA: Probiotic-associated aspiration pneumonia due to Lactobacillus
rhamnosus. J Clin Microbiol. 52:3124–3126. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
165
|
Zbinden A, Zbinden R, Berger C and
Arlettaz R: Case series of Bifidobacterium longum bacteremia in
three preterm infants on probiotic therapy. Neonatology. 107:56–59.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
166
|
Rizzatti G, Lopetuso LR, Gibiino G, Binda
C and Gasbarrini A: Proteobacteria: A common factor in human
diseases. Biomed Res Int. 2017:93515072017. View Article : Google Scholar : PubMed/NCBI
|
|
167
|
Zhu M, Liu X, Ye Y, Yan X, Cheng Y, Zhao
L, Chen F and Ling Z: Gut microbiota: A novel therapeutic target
for Parkinson's disease. Front Immunol. 13:9375552022. View Article : Google Scholar : PubMed/NCBI
|
|
168
|
Gentle SJ and Lal CV: Predicting BPD:
Lessons learned from the airway microbiome of preterm infants.
Front Pediatr. 7:5642020. View Article : Google Scholar : PubMed/NCBI
|
|
169
|
Carvalho JL, Miranda M, Fialho AK,
Castro-Faria-Neto H, Anatriello E, Keller AC and Aimbire F: Oral
feeding with probiotic Lactobacillus rhamnosus attenuates cigarette
smoke-induced COPD in C57Bl/6 mice: Relevance to inflammatory
markers in human bronchial epithelial cells. PLoS One.
15:e02255602020. View Article : Google Scholar : PubMed/NCBI
|
|
170
|
Fangous MS, Alexandre Y, Hymery N, Gouriou
S, Arzur D, Blay GL and Berre RL: Lactobacilli intra-tracheal
administration protects from Pseudomonas aeruginosa pulmonary
infection in mice - a proof of concept. Benef Microbes. 10:893–900.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
171
|
Zelaya H, Villena J, Lopez AG, Alvarez S
and Agüero G: Modulation of the inflammation-coagulation
interaction during pneumococcal pneumonia by immunobiotic
Lactobacillus rhamnosus CRL1505: Role of Toll-like receptor 2.
Microbiol Immunol. 58:416–426. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
172
|
Fangous MS, Gosset P, Galakhoff N, Gouriou
S, Guilloux CA, Payan C, Vallet S, Héry-Arnaud G and Le Berre R:
Priming with intranasal lactobacilli prevents Pseudomonas
aeruginosa acute pneumonia in mice. BMC Microbiol. 21:1952021.
View Article : Google Scholar : PubMed/NCBI
|
|
173
|
Wallace C, Gordon M, Sinopoulou V and
Akobeng AK: Probiotics for management of functional abdominal pain
disorders in children. Cochrane Database Syst Rev.
2:Cd0128492023.PubMed/NCBI
|
|
174
|
Su Z, Ma C, Ru X, Zhang S, Wu C, Huang Y,
Cen H, Yin Z and Zhang J: Effects of probiotic treatment on
patients and animals with chronic obstructive pulmonary disease: A
systematic review and meta-analysis of randomized control trials.
Front Cell Infect Microbiol. 14:14112222024. View Article : Google Scholar : PubMed/NCBI
|
|
175
|
Li P, Uma Mageswary M, Taib F, Koo TH,
Yusof A, Hamid IJA, Jiang H, Liong MT, Ali A and Zhang Y: Safety
and tolerance of bifidobacterium longum subsp. Infantis YLGB-1496
in toddlers with respiratory symptoms. Nutrients. 17:21272025.
View Article : Google Scholar : PubMed/NCBI
|
|
176
|
Zeng L, Yang K, He Q, Zhu X, Long Z, Wu Y,
Chen J, Li Y, Zeng J, Cui G, et al: Efficacy and safety of gut
microbiota-based therapies in autoimmune and rheumatic diseases: A
systematic review and meta-analysis of 80 randomized controlled
trials. BMC Med. 22:1102024. View Article : Google Scholar : PubMed/NCBI
|
|
177
|
Bettocchi S, Comotti A, Elli M, De Cosmi
V, Berti C, Alberti I, Mazzocchi A, Rosazza C, Agostoni C and
Milani GP: Probiotics and fever duration in children with upper
respiratory tract infections: A Randomized clinical trial. JAMA
Netw Open. 8:e2506692025. View Article : Google Scholar : PubMed/NCBI
|
|
178
|
Hiraku A, Nakata S, Murata M, Xu C, Mutoh
N, Arai S, Odamaki T, Iwabuchi N, Tanaka M, Tsuno T and Nakamura M:
Early probiotic supplementation of healthy term infants with
bifidobacterium longum subsp. infantis M-63 is safe and leads to
the development of bifidobacterium-predominant gut microbiota: A
double-blind, placebo-controlled trial. Nutrients. 15:14022023.
View Article : Google Scholar : PubMed/NCBI
|